Arterial Blood Gases
An arterial blood gas is a physiological assessment tool that measures a patient’s acid-base balance, alveolar ventilation, and oxygenation status.1 It is a valuable resource for obtaining information from respiratory monitoring in the intensive care unit, for conducting follow-up of outpatients, and for evaluating the treatment and the progress of their diseases. There has been a trend toward finding more noninvasive techniques to serve these purposes. This trend has been motivated by the desire to spare patients from being “stuck” so frequently and to avoid the risk for infection posed by indwelling cannulas in patients who already are ill and have weakened immune systems. Physical therapists frequently use oxygen saturation for assessment, but this is insufficient in many patients. When a patient has been thoroughly examined and it is determined that the arterial blood gas values are relatively stable, the physical therapist should compare those values to subsequent readings on the oximeter. Therapists need to consider the blood gas trends, acid/base status, and alveolar ventilation and then correlate those findings to the patient’s signs and symptoms, the physiological monitoring of HR, BP, and RR, and the perceived exertion with exercise. In many cases we need to consider a multisystem approach without examination and evaluation. Oximetry readings are important but must be evaluated in light of all body systems, not just the oximetry readings.
Noninvasive Monitoring
Noninvasive monitoring has become more readily available and is used to measure expired carbon dioxide (Pet CO2) and transcutaneous CO2 (T CO2) in neonatal and pediatric patients. New studies are showing that a universal pulse oximetry screening of all neonates before they are discharged would improve the detection rate of congenital heart disease. In a survey conducted in the United Kingdom by Kang and colleagues, it was found that 209 (93%) of the 224 units contacted did not use pulse oximetry routinely. In the neonatal units that did use pulse oximetry, if the saturation was abnormal, they also did echocardiography. Two other units obtained not only echocardiogram, but also x-rays and ECG. The conclusion was that this should be used with national guidelines to supplement the postnatal examination.2
A similar study was conducted by Arlettaz and colleagues to determine whether pulse oximetry could detect congenital heart disease in newborns. It was noted that about half of all newborns who had congenital heart disease were asymptomatic in the first few days of their life. However, early detection of this condition is important because treatment outcomes are related to the time of the diagnosis, and early identification leads to best outcomes. The authors studied the effectiveness of oximetry on the first day of life for early detection of congenital heart disease in neonates who appeared normal. They also examined whether pulse oximeter screening in addition to the clinical examination of the patient would yield more results in the diagnosis of congenital heart disease than would examination alone. If pulse oximetry was less than 95%, echocardiography was done. Of the 3262 newborns screened, 24 infants had repeated oxygen saturations of less than 95%. Of these neonates, 17 had congenital heart disease and the other 5 had persistent pulmonary hypertension. Arlettaz and colleagues concluded that pulse oximetry screening in the first few days of life is an effective tool to identify cyanotic congenital heart disease in otherwise healthy newborns.3
Partial Pressure of Gases
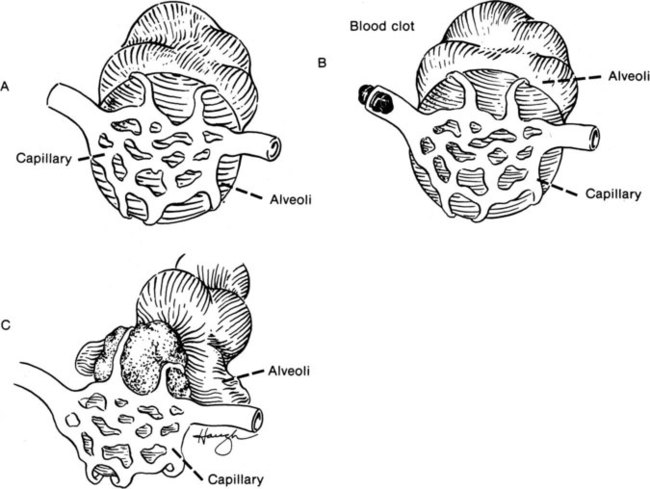
Normally, alveolar units ventilate and capillary units bring oxygenated blood to the tissues, excreting CO2 back into the alveoli to be removed through the lungs. Some abnormal situations may occur, however, such as shunts and dead-space units. In a shunt unit, the alveoli have collapsed, but blood flow continues and is unable to pick up oxygen. An example of this is atelectasis, in which a lung segment or part of a segment has retained secretions and lung tissue distal to the mucous plug collapses. Circulation continues but oxygenation does not occur, and the PO2 decreases. On the other hand, a dead-space unit can have ventilation but not perfusion. This occurs with pulmonary embolism, when a blood clot obstructs the circulation. The oxygen is available in the ventilated alveoli, but with no circulation, a dead unit is credited. Figure 10-1 demonstrates the regional differences seen in respiratory units.
Normal Blood Gas Values
Arterial oxygen is measured as PO2, the partial pressure of oxygen. Normal values are 80 to 100 mm Hg. If the PO2 is below 80 mm Hg in someone younger than 60 years of age, the patient is hypoxemic. A value of 60 to 80 mm Hg is considered mild hypoxemia; 40 to 60 mm Hg is considered moderate hypoxemia, and less than 40 mm Hg is severe hypoxemia.1
Hemoglobin
There is a predictable relationship between the arterial oxygen saturation of the Hgb and the PO2. It is represented in the oxyhemoglobin dissociation curve as follows. When oxygen saturation is monitored during exercise, saturation is kept at or above 90%. As the curve denotes at a level of approximately 60 mm Hg, the saturation is about 90%. As the PO2 drops at the sharp part of the curve, there is a marked decrease in oxygen saturation for every mm Hg PO2.4
Acid-Base Balance
Normal body metabolism consists of the consumption of nutrients and the excretion of acid metabolites. Acid metabolites must be kept from accumulating in large amounts because the body’s cardiovascular and nervous systems operate in a relatively narrow free hydrogen ion (H+) range (narrow pH). Free H+ concentration is discussed as pH (−log [H+]). The maintenance of body systems requires an appropriate acid-base balance.5
< ?xml:namespace prefix = "mml" />

Chemoreceptor Response to Hypoxemia
The peripheral chemoreceptors, the carotid bodies, and the aortic bodies are located at the bifurcation of the internal and external carotid arteries and the arch of the aorta. These receptors are nervous tissue with a high metabolic rate and an abundant oxygen supply. When tissue PO2 decreases, the response of these receptors to the brain is to increase ventilation and cardiac output. When that is not sufficient to effect a normal PO2, supplemental oxygen or increased mechanical assistance such as continuous positive airway pressure (CPAP) is administered.6
Blood Gas Interpretation
1. Look at the PCO2 to determine whether there is normal alveolar ventilation.
2. Look at the pH to see whether there is a normal acid-base balance or whether it is acute or chronic.
3. Look at the PO2 to see whether there is normal oxygenation or whether there is hypoxemia and to what degree.
Acceptable Ranges of Arterial Blood Gases
 For every 20 mm Hg increase in PCO2, the pH decreases by 0.10 (PCO2 60, pH 7.25)
For every 20 mm Hg increase in PCO2, the pH decreases by 0.10 (PCO2 60, pH 7.25)
 For every 10 mm Hg decrease in PCO2, the pH increases by 0.10 (PCO2 25, pH 7.50)
For every 10 mm Hg decrease in PCO2, the pH increases by 0.10 (PCO2 25, pH 7.50)
There is also a relationship between the PCO2 and the plasma bicarbonate.
 For every increase of 10 mm Hg in the PCO2, there is a decrease of 1 mmol/L of plasma bicarbonate
For every increase of 10 mm Hg in the PCO2, there is a decrease of 1 mmol/L of plasma bicarbonate
 For every 10 mm Hg PCO2, there is a decrease in plasma bicarbonate of 2 mmol/L
For every 10 mm Hg PCO2, there is a decrease in plasma bicarbonate of 2 mmol/L
By knowing these guidelines, the therapist can determine whether the changes in the arterial blood gases are in line with respiratory problems as opposed to metabolic problems such as acidosis due to diabetic ketoacidosis, in which the base deficit can be very low and the pH can be low (acidemic), but the PCO2 can be within normal limits.5,7
Potential Causes of Error in Arterial Blood Gas Sampling
The accuracy of arterial blood gas results depends on many factors: proper collection of the arterial sample, the handling of the sample from the patient to the laboratory, and the method by which the sample was analyzed. Possibilities for error exist all along the pathway. Great care must be taken to create proper protocol for all steps, and laboratories need to remain vigilant to decrease errors. Some of the common problems are nonarterial samples (venous blood versus arterial blood), air bubbles in the syringe, inadequate anticoagulant in the sample, and delayed analysis of a noncooled sample.8
Factors Affecting Arterial Blood Gases
Exercise or any increase in activity above rest may result in significantly increased oxygen consumption in patients with cardiopulmonary dysfunction. In the normal population, the human body compensates by increasing oxygen consumption to meet the workload. Usually, a plateau is reached and a constant oxygen consumption for that activity is achieved. In patients with cardiopulmonary dysfunction, oxygen consumption continues to increase, even at the same workload in untrained patients. It is important to monitor oxygen saturation to prevent desaturation in these patients.4 During pregnancy, hormonal and mechanical factors may have negative effects on cardiopulmonary function. In the last trimester, women commonly observe shortness of breath and difficulty in taking a deep breath because of hormonal issues and diaphragmatic encroachment.
In a small study by Sunyal and colleagues assessing oxygen saturation in pregnant women to try to evaluate the lung function in pregnancy, 32 women (25 to 35 years old) without any recent respiratory disease were monitored during each trimester. The study compared eight healthy nonpregnant women as an age-matched control group. In the pregnant women, the oxygen saturation levels increased progressively each trimester: first trimester (97.73% ± 0.30), second trimester (98.05% ± 0.54), and third trimester (98.40% ± .30). The oxygen saturation readings were higher in the pregnant women than in the nonpregnant women. The study conclusion was that the increased oxygen saturation during pregnancy was related to increased ventilation and a rising progesterone level, which reaches a peak in the later phases of pregnancy.9
Other Factors That Can Influence the Arterial Blood Gas
If the patient is on supplemental oxygen and the PO2 is only 55 mm Hg, the PO2 is still inadequate because of the additional O2.10–12 Any patient on oxygen at rest should be evaluated for appropriate oxygenation with exercise. Most patients’ blood gases are drawn at rest, not with exercise. Similarly, if a patient is on mechanical ventilation, the blood gases should be within or near normal limits.
Noninvasive Monitoring
Pulse Oximetry
Pulse oximetry provides estimates of arterial oxyhemoglobin saturation (SaO2) by utilizing selected wavelengths of light to noninvasively determine the saturation of oxyhemoglobin (SpO2).13
Precautions for Pulse Oximetry
If a patient needs ongoing measurement of pH, PCO2, and total Hgb, the presence of abnormal Hgb may be a “relative” contraindication for pulse oximetry.13 If the Hgb is low (i.e., 7-8, or virtually half the normal Hgb), the oxygen saturation may be above 90% at rest but as soon as exercise begins, the patient will usually desaturate very quickly. Thus pulse oximeter reading needs to be monitored before, during, and after exercise/activity to have a better overall view of the physiological response to the intervention. The other vital signs need to be evaluated as well.
Situations exist in which pulse oximetry may not yield accurate results: abnormal Hgb, jaundice, anemia, low perfusion (i.e., diabetes), the use of intravascular dye such as methylene blue, deeply pigmented skin, and dark nail polish.15 In addition, movement artifacts and highly lit fluorescent lights can have an effect on the readings. These concerns must be appreciated by therapists, especially during exercise, to ensure proper readings and correct evaluation of responses to exercise.
Transcutaneous Carbon Dioxide
A study by Sandberg and colleagues performed in the neonatal intensive care unit (NICU) evaluated the accuracy of transcutaneous (Tc) blood gas monitoring in newborn infants, including infants with extremely low birth weights. The measurements were taken under “stable conditions.” Some differences were found in arterial measurements versus Tc measurements, related to body weight, postnatal age, and the amount of oxygen each neonate required. Overall, Sandberg and colleagues concluded that there was good agreement between the two methods and that it was clinically acceptable to use Tc in their NICU. They added that although it would not replace the need for doing arterial blood gases, Tc monitoring would be a good supplement to use in assessing neonates.16
End Tidal Carbon Dioxide
The end tidal CO2 readings help monitor changes in the ventilatory status and assist in determining the need for changes in the ventilator settings to improve alveolar ventilation.17 Most notable is the ability to see trends in these readings and maintain an ongoing monitoring system that can allow for early detection of complications, such as pneumothorax, hypoventilation, pulmonary embolism, or fat embolism (any increase in dead space). The end tidal CO2 readings have also been used to determine the proper positioning of feeding tubes and endotracheal tubes.18,19
Summary
Noninvasive monitoring has been a great advance; it is now possible to see ongoing trends in a patient and assess complications early so that patients can be moved forward more safely and efficiently. Noninvasive monitoring can also be an adjunct to exercise, as will be discussed in Chapter 43.