Appendix
Ophthalmic History and Examination
AAO Suggested Routine Eye Examination Guidelines
Differential Diagnosis of Common Ocular Symptoms
Color Codes for Topical Ocular Medication Caps
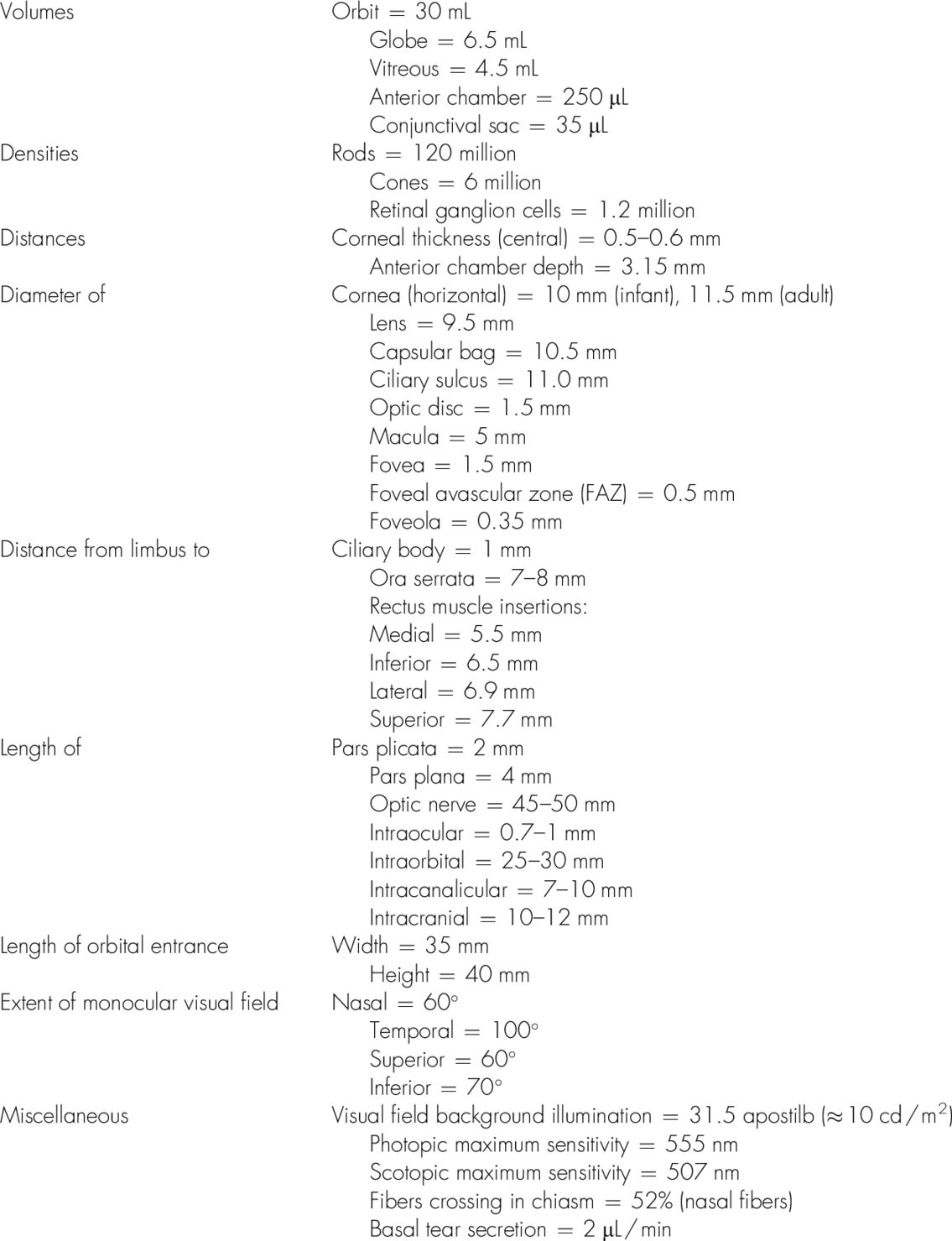
List of Important Ocular Measurements
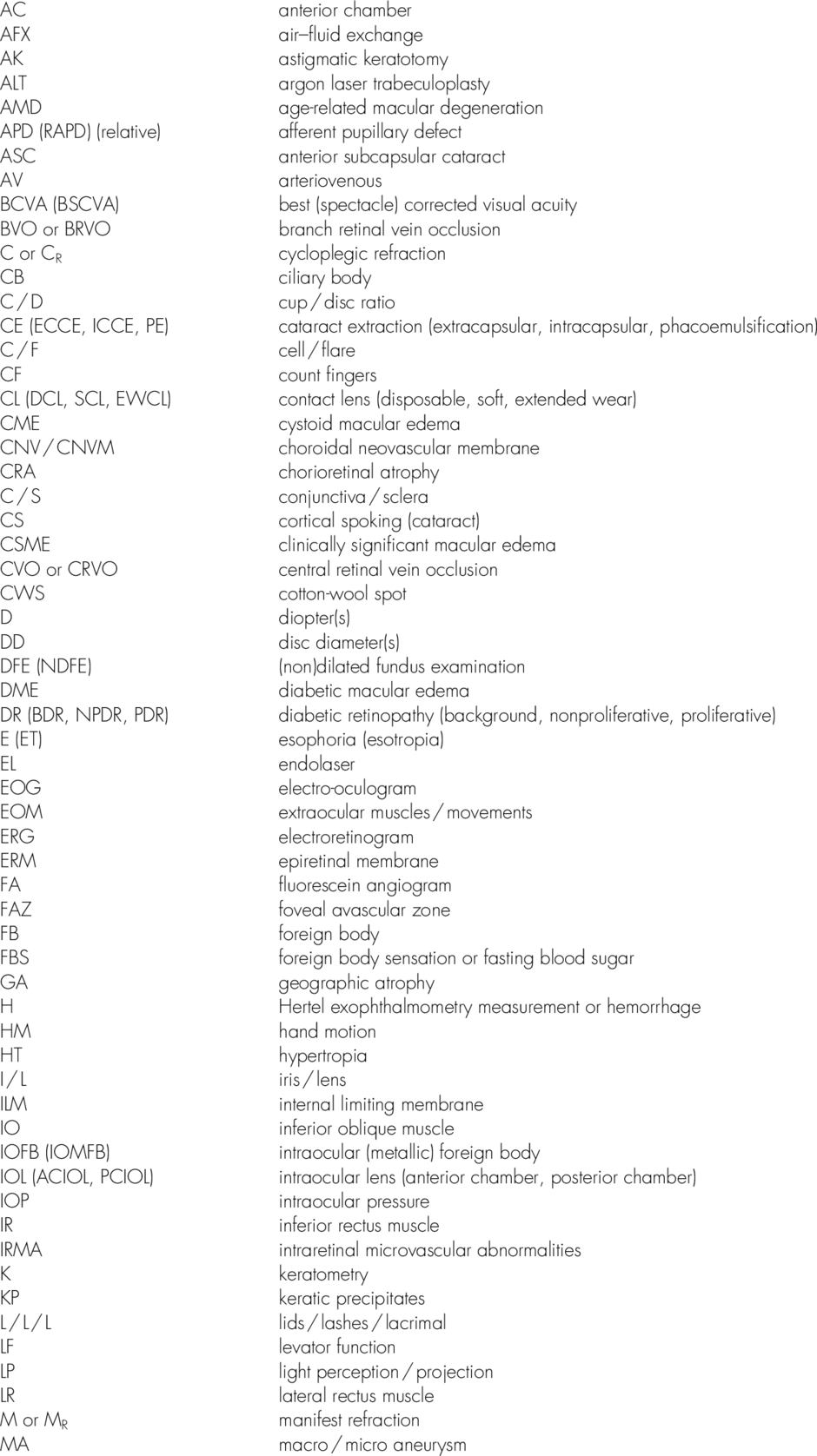
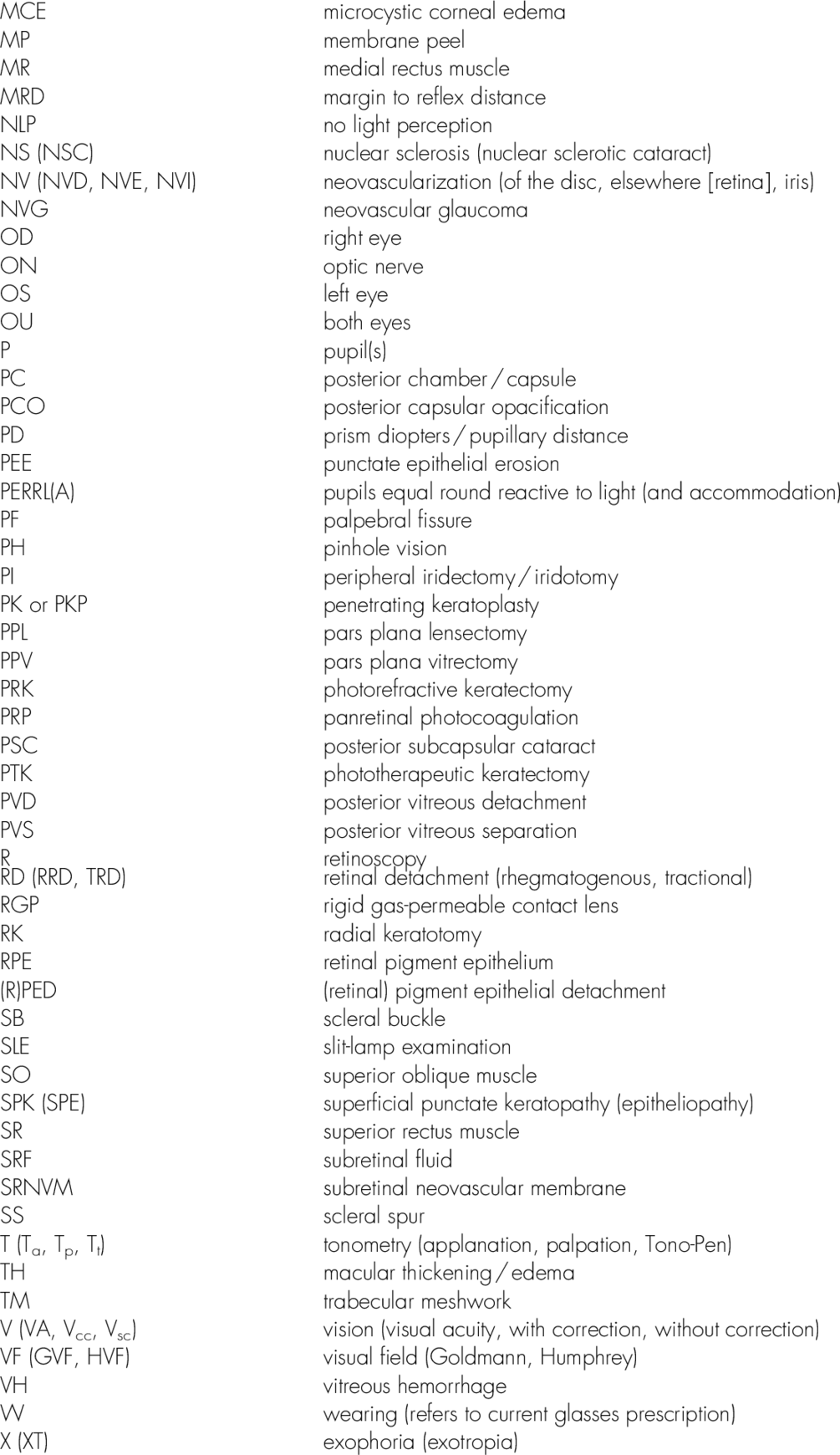
Common Ophthalmic Abbreviations (How to Read an Ophthalmology Chart)
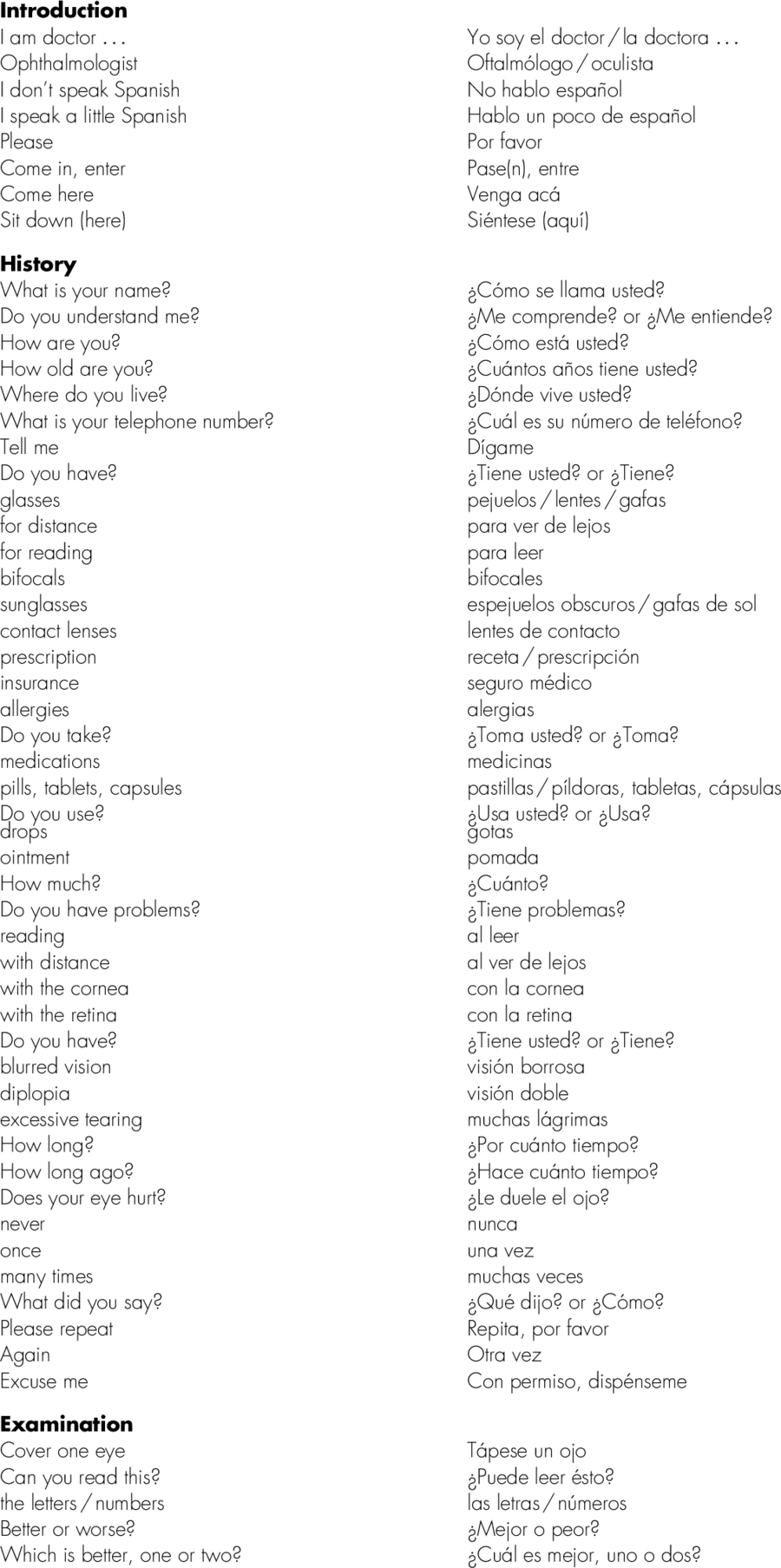
Ophthalmic History and Examination
History
As with any medical encounter, the initial part of the evaluation begins with a thorough history. The components of the history are similar to a general medical history but focus on the visual system:
• History of present illness (HPI)
• Past ocular history (POH)
• Eye medications
• Past medical and surgical histories (PMH / PSH)
• Systemic medications
• Allergies
• Family history (FH)
• Social history (SH)
• Review of systems (ROS).
Ocular Examination
The ocular examination is unique in medicine since most of the pathology is directly visible to the examiner; however, specialized equipment and instruments are necessary to perform a comprehensive examination. As with the general medical examination, there are multiple components to the eye examination, and they should be performed systematically.
Vision
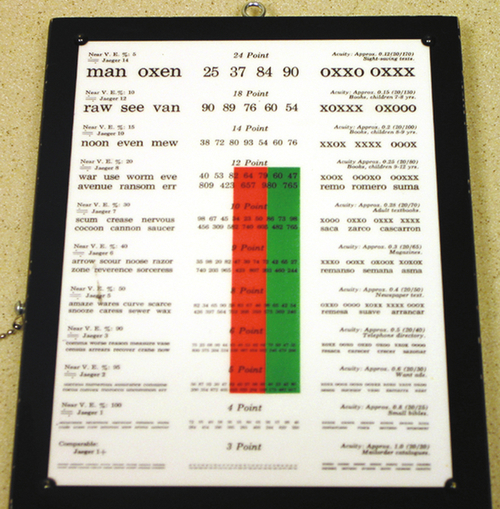
Visual acuity
Visual acuity measures the ability to see an object at a certain distance. It is measured one eye at a time, with correction if the patient wears glasses or contact lenses, and usually recorded as a ratio comparing an individual’s results with a standard.
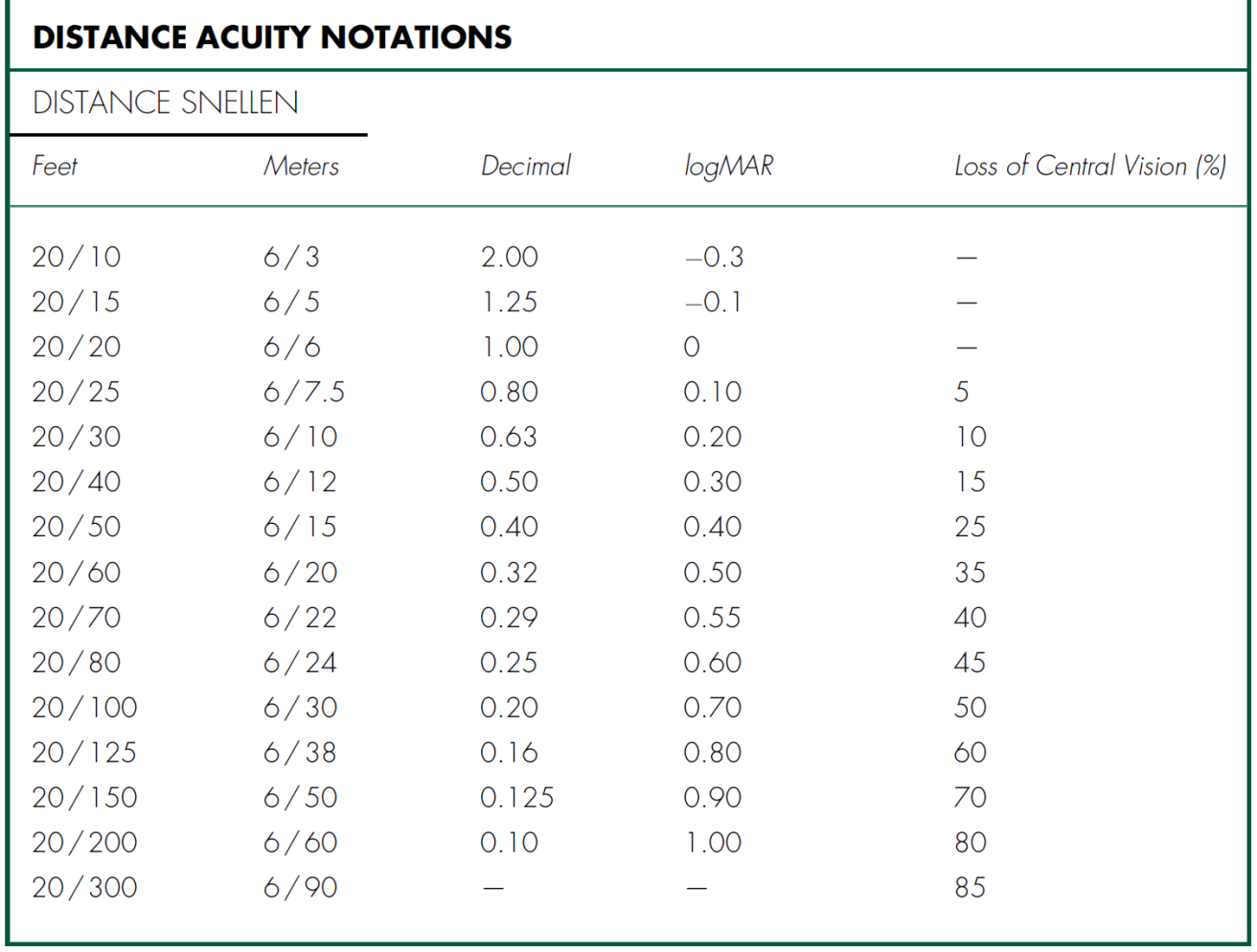
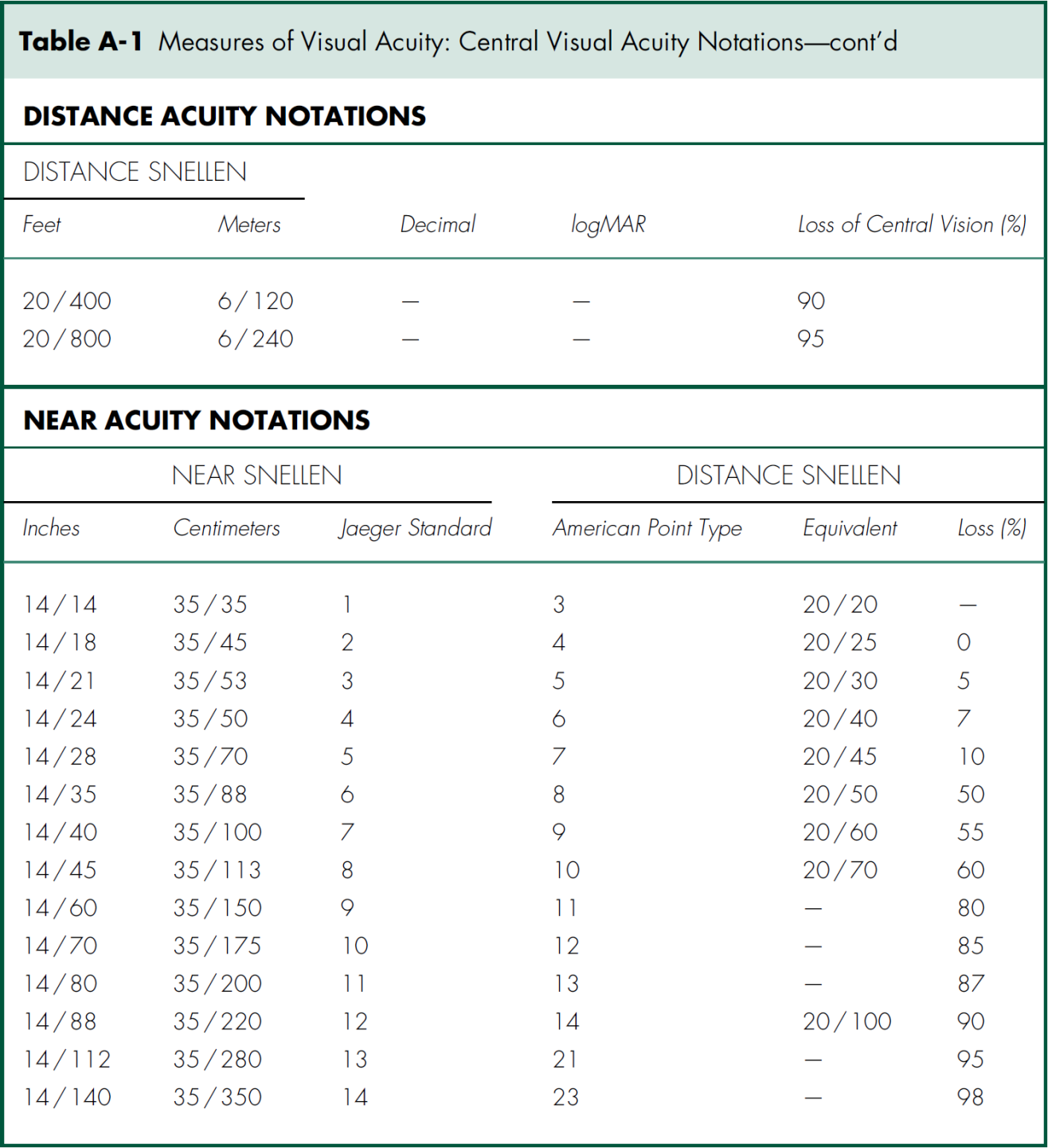
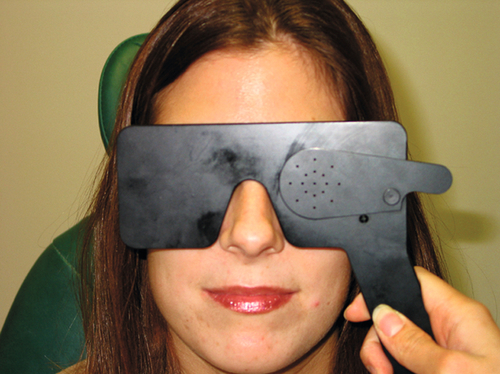
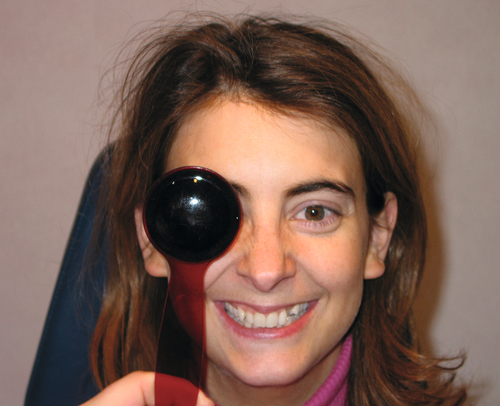
Distance vision using a Snellen chart at 20 feet (or 6 meters) is the most common method for recording visual acuity (Table A-1), and is denoted with VA, Va, or V and subscript of cc or sc (i.e., Vcc or Vsc) depending whether the acuity is measured with (cc) or without (sc) correction, respectively. An ocular occluder with pinholes (PH) can be used in an attempt to improve vision and estimate the eye’s best potential vision. If pinhole testing improves vision, an uncorrected refractive error or cataract is typically present. Visual acuity worse than 20 / 400 is recorded either as counting fingers (CF at the test distance; e.g., CF at 6 inches) if the patient can identify the number of fingers the examiner holds up; hand motion (HM) if the patient can identify the movement of the examiner’s hand; light perception with projection (LP and the quadrants) if the patient can identify the direction from which a light is shined into the eye; light perception without projection (LP) if the patient can determine only when a bright light is shone into the eye and not the direction the light is coming from; or no light perception (NLP) if the patient cannot perceive light from even the brightest light source. Near vision is similarly measured (monocularly with or without correction) and is denoted with N.
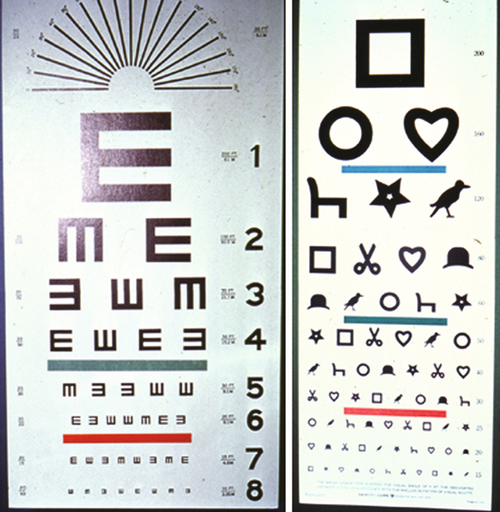
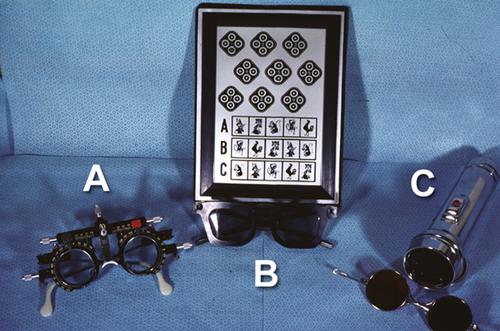
Other types of eye charts used to measure vision include the Bailie–Lovie or Early Treatment Diabetic Retinopathy Study (ETDRS) charts used in clinical trials (vision is measured at 2 and 4 meters). On ETDRS charts, halving of the visual angle occurs every three lines as there are equal (0.1) logarithmic intervals between lines as well as consistent spacing between letters and rows, proportional to letter size. Unlike Snellen charts, the score is recorded by letter, not line. For preschool children and illiterate adults, other tests including the tumbling “E” chart, Landolt “C” chart, HOTV match test, and Allen card pictures can be used to assess visual acuity. For infants, vision is commonly evaluated by the ability to fix and follow (F&F) objects of interest or the presence of central steady maintained fixation (CSM).
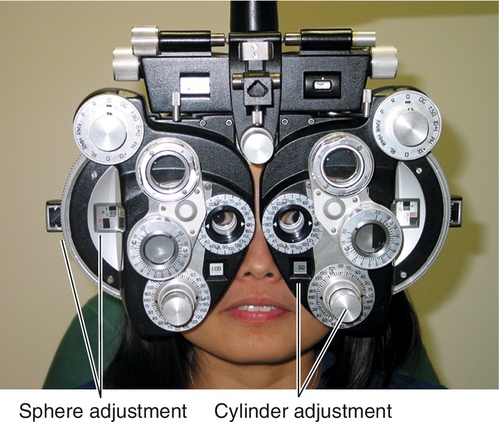
Refraction
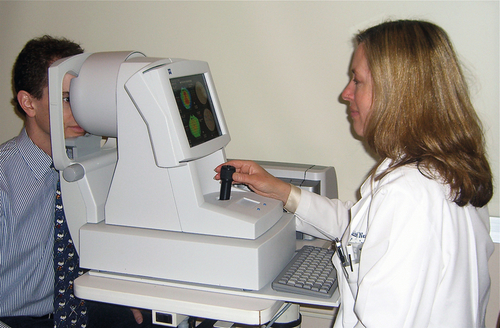
A subjective measurement of the refractive error is performed with a phoropter or trial frame that allows the patient to decide which lens power gives the sharpest image. This test is used to determine the best spectacle-corrected visual acuity (BSCVA) and prescription for glasses. A manifest refraction is done before dilating the eyes and is denoted with MR or M. A cycloplegic refraction is done after dilating the eyes with cycloplegic drops to prevent accommodation and is denoted with CR or C. A cycloplegic refraction is particularly important when refracting children, hyperopes, and refractive surgery candidates, in whom a manifest refraction may not be accurate. The duochrome (red–green) test is a useful method to check the refraction for overcorrection or undercorrection. An autorefractor is an instrument that performs automated retinoscopy and measures refractive error; however, the values should be confirmed with a subjective refraction before prescribing lenses.
Retinoscopy
An objective measurement of the refractive error performed with a retinoscope; it is denoted with R.
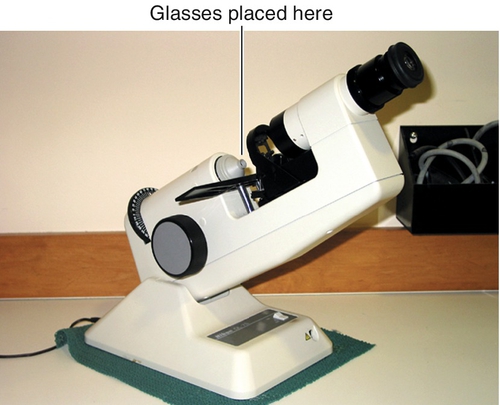
Lensometer
A manual or automated instrument that measures the power of a spectacle or lens; the prescription the patient is wearing is denoted with W.
Potential acuity meter (PAM)
An instrument that measures the visual potential of the retina by projecting the eye chart onto the retina through corneal and /or lens opacities. This test is most commonly used to assess visual potential before cataract surgery when there is coexisting retinal pathology.
Contrast sensitivity
Tested monocularly, usually with special charts (i.e., Pelli–Robson) having bar patterns on backgrounds with varying contrast. Reading can be plotted on a curve for different spatial frequencies.
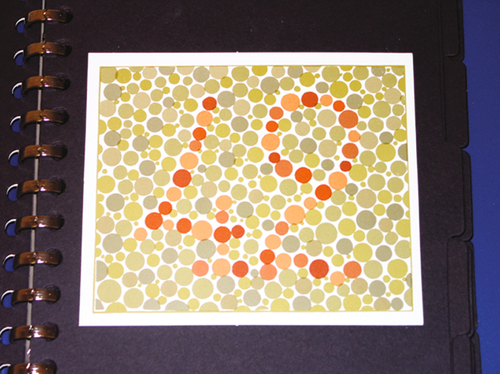
Color vision
Tested monocularly and most commonly with Ishihara pseudoisochromatic (red–green only) or Hardy–Rand–Ritter plates. More extensive evaluation is done using Farnsworth test. Gross macular or optic nerve function can be assessed by asking the patient to identify the color of a red object such as an eyedrop bottle cap (all dilating drops have red caps). Red saturation can also be tested with the red cap by asking the patient whether the cap appears to be the same degree of brightness of red when the eyes are alternately tested.
Stereopsis
Stereo acuity is tested binocularly and is commonly done with titmus or randot tests. The titmus test uses polarized images of a fly (patient is asked to grasp or touch the wings), animals (three rows of five cartoon animals each are pictured, and the patient is asked to touch the animal that is popping up), and circles (nine groups of four circles each are pictured, and the patient is asked to touch the circle that is popping up) of increasing difficulty to quantitate the degree of stereopsis (40 seconds of arc is normal).
4-Diopter base-out prism test
This test is useful for detecting fusion or suppression in what appear to be “straight” eyes. It is an objective test that can be used on a cooperative young child who may not understand the stereo acuity test. It is also useful for the patient suspected of “faking” a negative stereo test. A 4-diopter base-out prism is placed over one eye, as the patient fixes on a distant target. A normal response is a small convergence movement by each eye. If the prism is placed over a suppressing eye, that eye will not move. A fusing eye will move toward the nose.
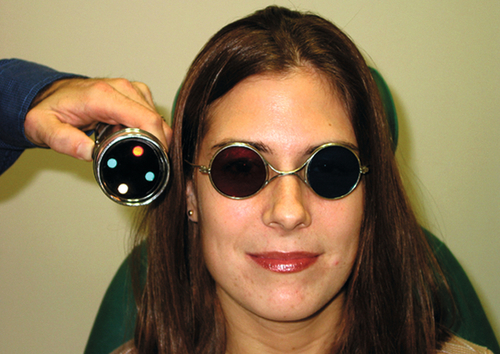
Worth 4-dot test
Assesses binocularity in cases of strabismus. The patient views 4 lights (1 red, 2 green, and 1 white) at distance and near while wearing special glasses with a red lens over the right eye and a green lens over the left eye. The size and location of a suppression scotoma can be determined depending on the number and pattern of lights perceived.
Ocular Motility
The alignment of the eyes in primary gaze is observed, and the movement of the eyes is assessed as the patient looks in all directions of gaze by following an object that the examiner moves. Normal motility (extraocular movements) is often recorded as intact (EOMI) or full. If misalignment, gaze restriction, or nystagmus is present, then other tests are performed. Several methods are used to distinguish and measure ocular misalignment.
Cover tests
Assess ocular alignment by occluding an eye while the patient fixates on a target. Measurements are made for both distance and near with and without glasses.
Cover–uncover test
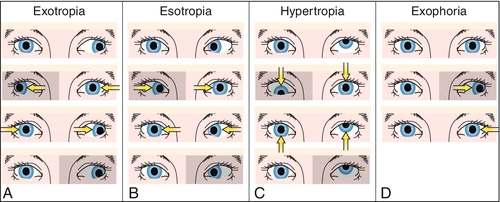
Distinguishes between a tropia and a phoria. One eye is covered and then uncovered. If the unoccluded eye moves when the cover is in place, a tropia is present. If the covered eye moves when the cover is removed, a phoria is present.
Alternate cover test (prism and cover test)
Measures the total ocular deviation (tropia and phoria). The occluder is alternately placed in front of each eye until dissociation occurs, and then hand-held prisms are held in front of an eye until no movement occurs.
Corneal light reflex tests
Assess ocular alignment by observing the relative position of the corneal light reflections from a light source directed into the patient’s eyes; can be used in patients who cannot cooperate for cover tests. The position of the corneal light reflexes can be used to measure the ocular deviation.
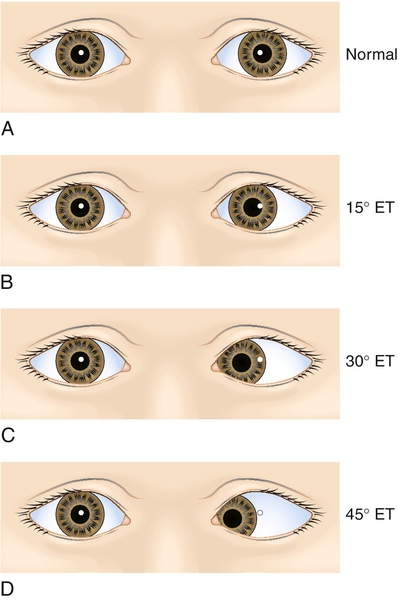
Hirschberg’s method
The amount of decentration of the light reflex is used to estimate ocular deviation (1 mm of decentration corresponds to 7° or 15 prism diopters [PD]). Light reflections at the pupillary margin (2 mm decentration), mid-iris (4 mm decentration), and limbus (6 mm decentration) correspond to deviations of approximately 15° or 30PD, 30° or 45PD, and 45° or 60PD, respectively.
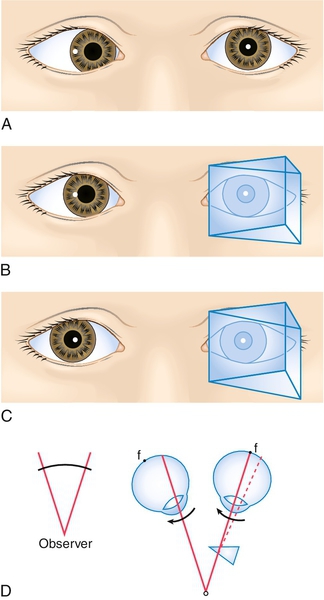
Modified Krimsky’s method
Prisms are placed in front of the fixating eye to center the light reflection in the deviated eye.
Forced ductions
Determine whether limited ocular motility is due to a restrictive etiology. Under topical anesthesia the eye is grasped at the limbus with forceps and rotated into the deficient direction of gaze. Resistance to movement indicates restriction. The forceps should be placed on the same side of the limbus in which the eye is being moved to avoid an inadvertent corneal abrasion should the forceps slip.
Optokinetic nystagmus (OKN) testing
Assesses patients with nystagmus and other eye movement disorders. A rotating drum (or strip) with alternating black and white lines is slowly moved both horizontally and vertically in front of the patient and the resultant eye movements are observed.
Pupils
The size, shape, and reactivity of the pupils are assessed while the patient fixates on a distant target. Both the direct and consensual responses are observed. The swinging flashlight test is done to identify a relative afferent pupillary defect (see RAPD in Chapter 7), particularly if anisocoria or poor reaction to light is present. If the pupils react to light, then they will react to accommodation, so this does not need to be tested; however, if one or both pupils do not react to light, then the reaction to accommodation should be assessed since some conditions may cause light-near dissociation.
The reactivity of each pupil is graded on a scale of 1 + (sluggish) to 4 + (brisk). Normal pupils should be equal, round, and briskly reactive to light. The most common abbreviation for denoting this pupillary response is “pupils equal round and reactive to light” (PERRL or PERRLA if accommodation is also tested). A preferred method that provides more information is to note the size of the pupils before and after the light stimulus is applied (i.e., P 4 → 2 OU). If anisocoria is present, the pupils should be measured in both normal lighting conditions and dim conditions (mesopic or scotopic).
Visual Fields
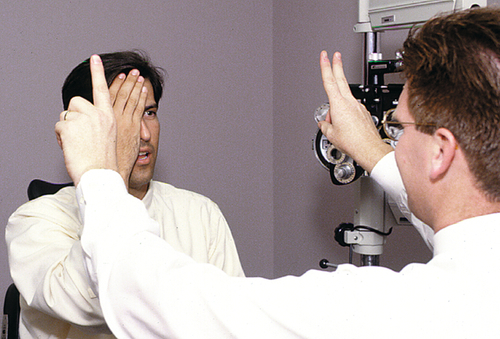
Confrontation visual fields are evaluated monocularly with the patient and examiner sitting opposite one another and looking into the examiner’s opposite eye (used as a control) while being asked to identify the number of fingers presented or the movement of a finger in each quadrant. Normal fields are recorded as visual fields full to confrontation (VFFC or VF full).
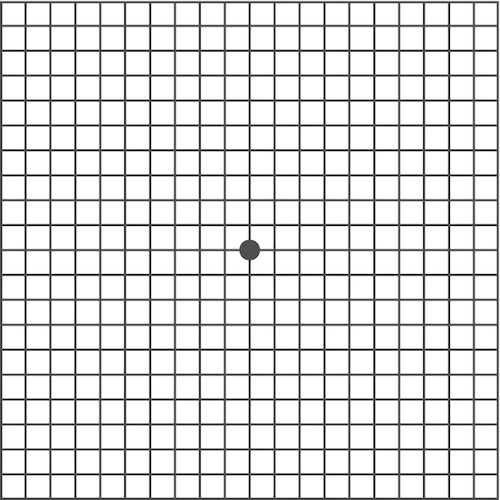
Amsler grid
A 10 cm × 10 cm grid composed of 5 mm squares that evaluates the central 10° of the visual field. This test is most commonly used to assess central visual distortion in patients with age-related macular degeneration and other macular pathology.
Tangent screen
A manual test that is performed with the patient seated 1 m in front of a 2 m × 2 m square black cloth over which the examiner presents test objects (spheres of various size and color).
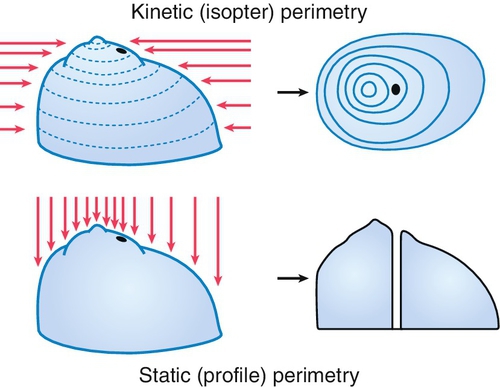
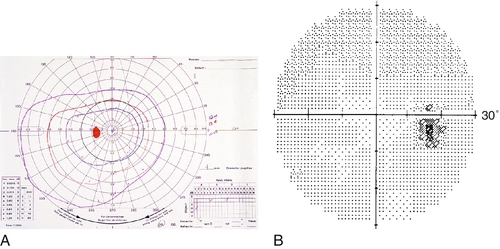
Goldmann visual field
A manually operated machine used to perform static and kinetic perimetry centrally and peripherally.
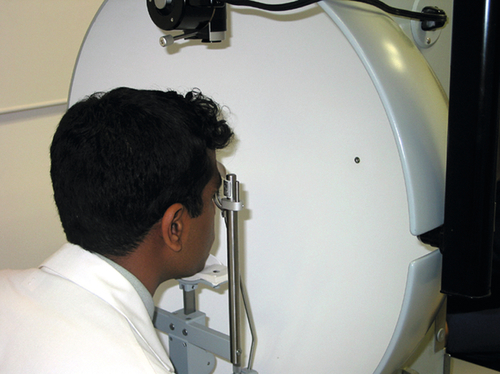
Humphrey visual field
A computerized static perimetry test with various programs to screen for and evaluate glaucomatous, neurologic, and lid-induced visual field defects.
External Examination
Orbit, eyelid, and lacrimal structures are evaluated for symmetry, position, and any abnormalities. Palpation and auscultation are performed when indicated.
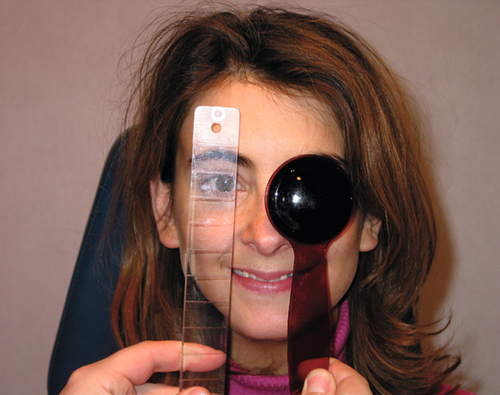
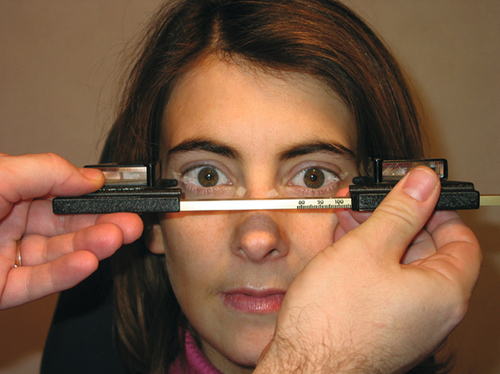
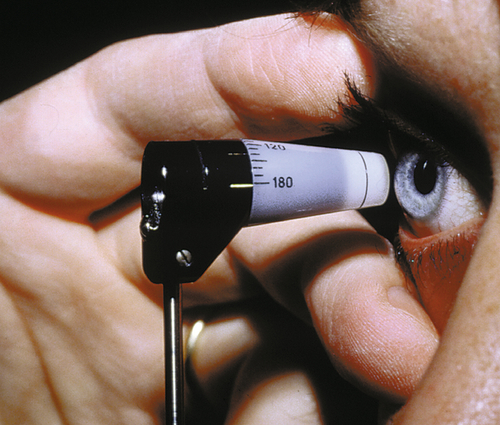
Exophthalmometry
Measurement of the distance the corneal apex protrudes from the lateral orbital rim to assess for proptosis or enophthalmos. The exophthalmometer is adjusted to rest against the lateral orbital rims, and with the patient looking in primary gaze, the level of each corneal apex is viewed in the exophthalmometer mirrors; these measurements are recorded along with the base number (width of the orbital rims).
Schirmer’s test
Special strips of 5 × 35 mm Whatman #41 filter paper are placed in the lower eyelids to absorb tears and measure tear production to evaluate dry eyes (see Dry Eye Disease in Chapter 4).
Jones’ dye tests
Two tests that evaluate lacrimal drainage obstruction (see Nasolacrimal Duct Obstruction in Chapter 3).
Other cranial nerve examination
CN5 is tested to assess facial and corneal sensation, and CN7 is tested to assess facial movement including eyelid closure, when warranted.
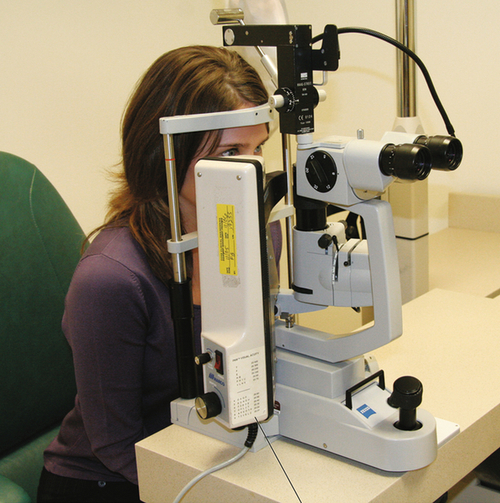
Slit-Lamp Examination (SLE)
This specialized biomicroscope allows detailed examination of the eye. The height, width, and angle of the light beam can all be controlled, and various filters can be changed to enhance visualization. A thin beam directed through the clear ocular media (cornea, anterior chamber, lens, and vitreous) acts as a scalpel of light illuminating a cross-sectional slice of optical tissue. This property of the slit-lamp allows precise localization of pathology. The technique of retroillumination (coaxial alignment of the light beam with the oculars) uses the red reflex from the retina to backlight the cornea and lens, making some abnormalities more easily visible. Furthermore, anterior segment lesions can be accurately measured by recording the height of the slit-beam from the millimeter scale on the control knob. Although the posterior segment can be evaluated with the aid of additional lenses, the SLE typically focuses on the anterior segment.
Portable, hand-held, slit-lamp devices facilitate examination at the bedside. If a slit-lamp instrument is not available, a penlight examination can be done with a magnifying lens to briefly assess the anterior segment. Similarly, a direct ophthalmoscope or indirect ophthalmoscope and lens can also be focused on the anterior segment structures for examination.
Components of the slit-lamp examination
Lids, lashes, and lacrimal glands
The lids, lashes, puncta, and Meibomian gland orifices are inspected. The medial canthus or lid margin can be palpated to express discharge or secretions from the inferior punctum or Meibomian glands, respectively. The lacrimal gland can also be inspected and palpated.
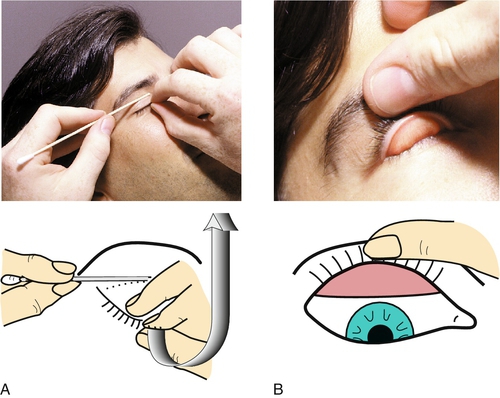
Conjunctiva and sclera
The patient is asked to look in the horizontal and vertical directions to observe the entire bulbar conjunctiva, and the lids are everted to observe the tarsal conjunctival surface. The caruncle and plica semilunaris are also inspected. The upper eyelid can be double everted to evaluate the superior fornix, and a moistened cotton-tipped applicator can be used to sweep the fornix to remove suspected foreign bodies.
Cornea
All five layers of the cornea are inspected. The tear film is evaluated for break-up time and height of the meniscus. The cobalt-blue filter allows better visualization of corneal iron lines.
Anterior chamber
The anterior chamber is evaluated for depth – graded on a scale from 1 + (shallow) to 4 + (deep) – and the presence of cells and flare (see Chapter 6). Normally, the AC is deep and quiet (D&Q).
Iris and lens
The iris and lens are inspected. The lens is better evaluated after pupillary dilation. If the eye is pseudophakic, the position and stability of the intraocular lens implant are noted, and the condition of the posterior capsule is assessed. The anterior vitreous (AV) can also be observed without the use of additional lenses. For aphakic eyes, the integrity of the anterior hyaloid face is evaluated, and any vitreous prolapse into the AC or strands to anterior structures is noted.
Dyes
Fluorescein, rose bengal, and lissamine green can be used to evaluate the health and integrity of the conjunctival and corneal epithelium. The integrity of wounds is assessed with the Seidel test (see Laceration in Chapter 5).
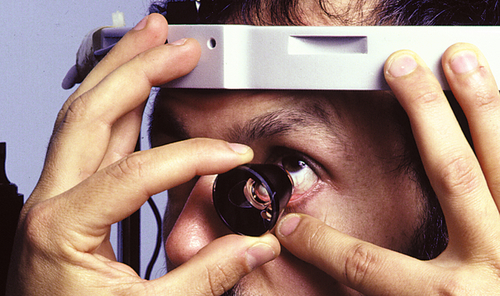
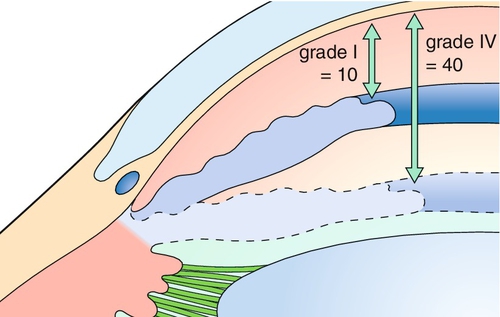
Gonioscopy
Evaluation of the anterior chamber angle structures with special mirrored contact lenses that are placed on the cornea. Various grading systems exist to specify the degree to which the angle is open. Indentation gonioscopy is used to determine whether angle closure is due to apposition (opens with indentation of the central cornea, which pushes aqueous peripherally) or synechiae (does not open with indentation).
Fundus contact and noncontact lenses
Numerous lenses can be used to examine the retina and optic nerve. Although performed with a slit-lamp, these findings are recorded as part of the fundus examination (see below).
Tonometry
Various instruments can be used to measure the intraocular pressure (IOP). Most commonly, IOP is measured as part of the slit-lamp examination (SLE) with the Goldmann applanation tonometer (a biprism that creates optical doubling), which is attached to the slit-lamp. Topical anesthetic drops and fluorescein drops (either individually or in a combination drop) are instilled into the eye, the tonometer head is illuminated with a broad beam and cobalt-blue filter, the tip contacts the cornea, the dial is adjusted until the mirror-image semicircular mires slightly overlap so that their inner margins just touch each other, and the pressure measurement in mmHg is obtained by multiplying the dial reading by 10 (i.e., “2” equals 20 mmHg). If marked corneal astigmatism exists, to obtain an accurate reading the tonometer tip must be rotated so that the graduation marking corresponding to the flattest corneal meridian is aligned with the red mark on the tip holder. Central corneal thickness also affects pressure readings. It is important to record the time when the pressure is measured. If a slit-lamp is not available, portable hand-held devices such as the Tono-Pen, Perkins, or Shiotz tonometers can be used. Estimating IOP by digital palpation (finger tension) is highly inaccurate.
Specialized Tests
Pachymetry
Measurement of corneal thickness by an optical or ultrasound pachymeter. Ultrasound instruments are used to measure central corneal thickness by applanation and therefore require topical anesthesia. This is most commonly performed in order to adjust IOP measured by applanation tonometry and to screen refractive surgery candidates. Optical devices are computerized to generate a thickness map of the entire cornea, which can be helpful in evaluating corneal ectasia and edema.
Keratometry
Measurement of corneal curvature and power using a keratometer, which evaluates two paracentral points on the anterior corneal surface. Mires are projected onto the cornea and, by turning the instrument knobs to align the reflected images, a direct reading is obtained. Automated machines often combine keratometry with other measurements such as refractive error or biometry.
Corneal topography / tomography
Computerized videokeratography (CVK) measures the curvature or elevation of the entire corneal surface, providing more information than keratometry. These instruments produce topographic maps, and some can measure the posterior corneal surface as well as corneal thickness. Many contain software to help identify early corneal irregularities.
Wavefront aberrometry
Measurement of the total aberrations of the eye (cornea and lens) including the higher-order aberrations (HOAs). Zernicke or Fourier analysis is used to determine the aberrations and generate a map. This technology is utilized in wavefront refractive surgical procedures.
Specular microscopy
Evaluation of the corneal endothelial cells by specular light reflection. The instrument measures cell count and morphology.
Confocal microscopy
Evaluation of corneal cellular structure. This non-invasive technique for evaluation of the cornea provides images delineating corneal epithelium, Bowman’s layer, stroma, Descemet’s membrane and the corneal endothelium.
Anterior segment–ocular coherence tomography (AS-OCT)
Evaluation of the anterior segment with cross-sectional scans of the cornea, anterior chamber angle, iris, and lens. AS-OCT utilizes near-infrared light waves to measure distances of anatomical structures. Requires a specialized lens or scan pattern as compared with posterior segment OCT.
Fundus Examination
The optic nerve and retina can be examined with or without pupillary dilation and with a variety of instruments and lenses. Direct ophthalmoscopy (DO) and indirect ophthalmoscopy (IO) are performed with a direct or indirect ophthalmoscope, respectively. The direct ophthalmoscope provides monocular high magnification (15 ×) with a narrow field of view, whereas the indirect ophthalmoscope produces a wide binocular field of view at lower magnification (2–3 ×). The images obtained through the indirect lenses used for IO and slit-lamp examination are flipped and inverted, and this must be taken into account when drawing retinal diagrams. An easy way to correct for this image reversal is to turn the retinal diagram upside-down and then draw the pathology as it is seen through the lens; when the diagram is viewed right side up, the picture will then be correct. A dilated fundus examination is often denoted as DFE, and the appearances of the disc, vessels, macula, and periphery are noted. A normal retinal examination is commonly abbreviated as d / v/ m / p wnl. The dimensions and location of lesions are compared with the size of the disc; thus measurements are recorded as multiples of disc diameters (DD) or areas (DA).
Components of the fundus examination
The optic nerve is inspected with particular attention to the cup-to-disc ratio (C / D), appearance of the neural rim (normally sharp and flat), and color (orange–yellow). The presence/absence of disc edema is also important.
Vessels
The retinal vessels are observed as they emerge from the optic cup and followed as they branch toward the periphery. Spontaneous venous pulsations can sometimes be seen at the nerve head. Any anomalous pattern or abnormality of the vasculature is recorded. This includes color (important for diseases such as hypertension where the vessels can take on an appearance of copper wires), tortuosity, caliber, and any changes where arteries and veins cross (i.e., AV nicking).
Macula
The macula, especially the fovea, is evaluated. Usually a bright light reflex is seen at the center of the fovea, especially in younger patients. In eyes with a suspected macular hole or cyst, the Watzke–Allen test can be performed by shining a thin vertical slit-beam over the center of the fovea and asking the patient if the light beam appears discontinuous or narrower in the middle (see Macular Hole in Chapter 10).
Peripheral retina
The retinal periphery is most easily examined through a widely dilated pupil. The patient is asked to look in all directions of gaze so that the entire retina (360°) can be viewed with indirect ophthalmoscopy. Visualization and differentiation of pathology near the ora serrata and far retinal periphery are aided with scleral depression.
Specialized Tests
Ultrasonography
Measurement of the acoustic reflectivity of ocular interfaces. Two modes:
A-scan (amplitude)
Produces a one-dimensional display that is primarily used to determine axial length measurement (biometry) for IOL calculations, but it can also be helpful to differentiate the internal structure of ocular masses. Methods include immersion (more accurate) or contact (less accurate due to corneal indentation and misalignment errors). Biometry measurement is based upon reflectivity from the internal limiting membrane.
B-scan (brightness)
Produces a two-dimensional image of the posterior segment, and is obtained when the fundus cannot be directly visualized.
Partial coherence laser interferometry (IOLMaster) and optical low coherence reflectometry (Lenstar)
Measurement of the optical reflectivity from the retinal pigment epithelium to determine axial length. Both are noncontact modalities with better resolution than immersion A-scan. They also perform keratometry, anterior chamber depth, and white-to-white measurements as well as IOL calculations. In addition, the Lenstar instrument measures pachymetry, lens thickness, pupillometry, eccentricity of the visual axis, and retinal thickness.
Optical coherence tomography
A noninvasive, noncontact imaging modality that provides high-resolution, cross-sectional images of the eye by measurement of the optical reflectivity of ocular structures. Optical coherence tomography (OCT) is useful for diagnosing and following anterior segment, macular and optic nerve pathology. Time domain OCT (TDOCT) relies on movement of a reference mirror and thus requires a longer period of time to acquire images. Spectral (SDOCT) or Fourier domain OCT offers dramatically increased speed as no movement of the mirror is required. In addition, SDOCT offers improved resolution especially when image averaging is used. By moving the scanner closer to the patient or by using image averaging, evaluation of deeper structures such as choroid and sclera can be performed (enhanced depth imaging). By using OCT perpendicular to the cornea, anterior segment structures can also be imaged with excellent detail (see above). Broader wavelength light sources (e.g., 1050 nm) allow deeper penetration. Next-generation swept source OCT using a swept wavelength tunable laser instead of a narrow bandwidth laser offers increased signal-to-noise ratio and dramatically faster scan rates (100,000 A scans/second) leading to better image quality.
Reference
FM Wilson, JE Gurland, 2005 Practical Ophthalmology: A manual for beginning residents, ed 5. American Academy of Ophthalmology: San Francisco.
AAO Suggested Routine Eye Examination Guidelines
Differential Diagnosis of Common Ocular Symptoms
Decreased Vision
There are many causes of decreased or blurred vision, so to narrow the differential diagnosis, it is important to characterize the visual loss in terms of rapidity of onset, duration, central versus peripheral vision, distance versus near vision, monocular versus binocular, and other associated symptoms (i.e., none, pain, red eye, tearing, flashes of light, headache, other neurologic symptoms):
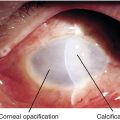
• Gradual loss of vision: Optic neuropathy (compressive, hereditary, infectious, infiltrative, nutritional, toxic), glaucoma, dry macular degeneration, macular edema, diabetic retinopathy, central serous retinopathy (CSR), chronic retinal detachment, uveitis (mild pain/ photophobia), cataract (may cause glare from bright lights), corneal edema, corneal dystrophy, corneal ectasia, change in refractive error.
• Transient loss of vision (< 24 hours): Amaurosis fugax (transient ischemic attack; monocular), vertebrobasilar insufficiency (binocular), migraine, papilledema, presyncopal episode.
• Visual field defect: Stroke, optic neuropathy, branch retinal vascular occlusion, chronic glaucoma, retinal detachment.
Visual Distortion
Macular pathology (i.e., AMD, epiretinal membrane, macular hole, CSR, etc.), uncorrected refractive error, irregular astigmatism, migraine, pharmacologic, CNS pathology, visual hallucination.
Glare / Halos
Due to corneal, iris, or lens pathology: dry eye disease, corneal edema, corneal scar, uveitis, angle-closure glaucoma, cataract, posterior capsular opacification, intraocular lens implant, after corneal refractive surgery, uncorrected refractive error, mydriasis, iris hole.
Photophobia
Corneal abrasion, edema, or scar, keratitis, uveitis, scleritis, angle-closure glaucoma, mydriasis, migraine, albinism, aniridia, congenital glaucoma, meningitis, optic neuritis.
Diplopia
Double vision may be binocular or monocular, horizontal or vertical, intermittent or constant. The patient must be asked about the characteristics of the diplopia to narrow the differential diagnosis:
• Monocular: Uncorrected refractive error, corneal opacity, irregular astigmatism, iris hole, iridodialysis, cataract, dislocated lens/decentered lens implant, posterior capsular opacification, epiretinal membrane.
Night Blindness
Retinal dystrophy (i.e., retinitis pigmentosa, congenital stationary night blindness, gyrate atrophy, choroideremia) or toxicity, following panretinal photocoagulation, vitamin A deficiency, optic atrophy, advanced glaucoma, uncorrected refractive error, dense cataracts, small pupils.
Eye Pain
Patients with ocular discomfort must be asked about the character and severity of their pain:
• Deep (ache/ pain): Large corneal abrasion, recurrent erosion, chemical burn or ulcer, uveitis, endophthalmitis, angle closure, scleritis, myositis, optic neuritis.
• Orbital/ periorbital: Nonocular pain including trauma, lid /adnexa pathology (i.e., hordeolum, preseptal cellulitis, dermatitis, dacryocystitis, dacryoadenitis), referred pain (sinus, dental, nasal), cranial nerve palsy, trigeminal neuralgia, cavernous sinus abnormality, orbital lesion (i.e., idiopathic orbital inflammation, orbital cellulitis, mass), headache (migraine, cluster).
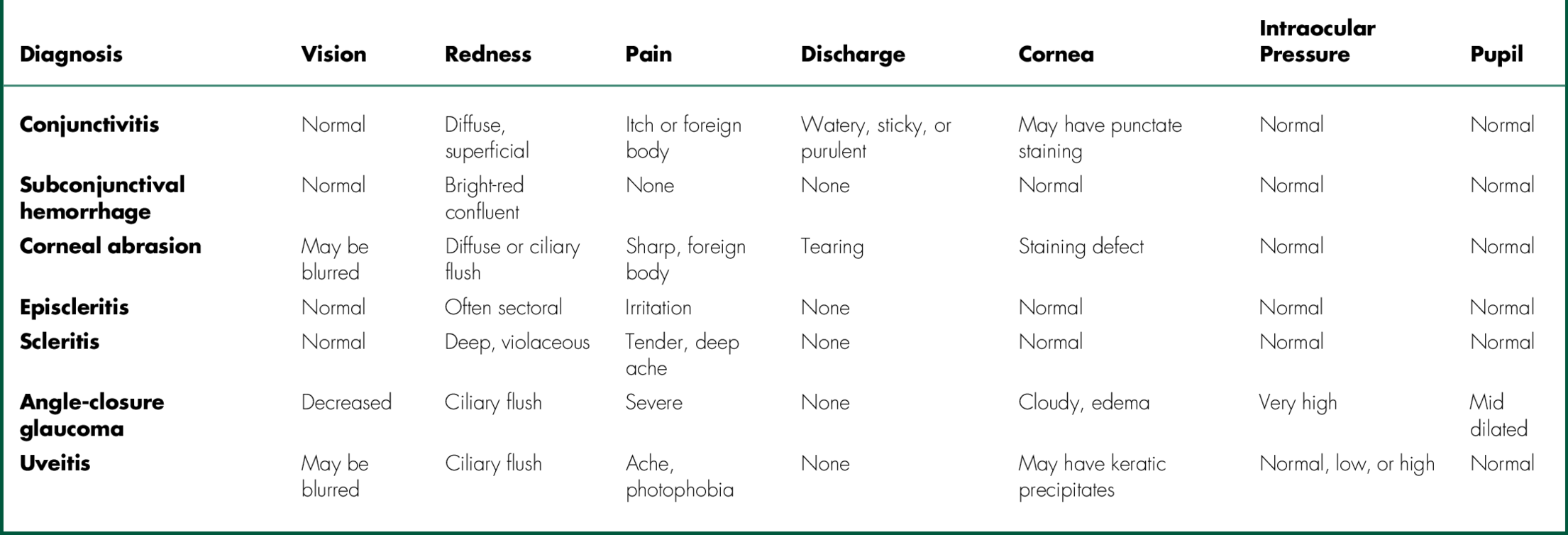
Red Eye
The common causes and associated findings of a red eye are listed in Table A-2.
Tearing
Dry eye disease, blepharitis, trichiasis, entropion, ectropion, conjunctivitis, punctual stenosis or occlusion, nasolacrimal duct obstruction, canaliculitis, dacryocystitis, keratitis, corneal abrasion, corneal or conjunctival foreign body, uveitis, congenital glaucoma.
Discharge
Conjunctivitis, nasolacrimal duct obstruction, hordeolum, dacryocystitis, canaliculitis, corneal ulcer, blepharitis.
Lid Swelling
Chalazion / hordeolum, cellulitis, dermatitis (contact or infectious), allergy (angioedema), blepharitis, dermatochalasis, conjunctivitis, trauma, foreign body, insect bite, orbital fat prolapse, blepharochalasis, dacryoadenitis, lid or lacrimal gland mass.
Lid Twitch
Eyelid myokymia, conjunctival or corneal irritation, blepharospasm, hemifacial spasm, trigeminal neuralgia, Tourette’s syndrome.
Flashes of Light
Retinal tear/ detachment, posterior vitreous detachment, rapid eye movements, eye rubbing, migraine, retinitis, optic neuritis, occipital lobe disorders, vertebrobasilar insufficiency, visual hallucinations.
Floaters
Vitreous syneresis, posterior vitreous detachment, vitritis, vitreous hemorrhage, retinal tear/ detachment, hyphema, large cell lymphoma.
Common Ophthalmic Medications
Anti-Infectives
Antibiotics
Aminoglycosides
amikacin (Amikin) 10 mg / mL up to q1h
amikacin 25 mg / 0.5 mL subconjunctival
amikacin 0.4 mg / 0.1 mL intravitreal
amikacin 15 mg / kg / day IV in 2–3 divided doses
gentamicin (Genoptic, Gent-AK, Gentacidin, Garamycin) 0.3% qid
neomycin–polymyxin B–gramicidin 0.025 (Neosporin, AK-Spore) qid to q1h
tobramycin (Tobrex, AK-Tob, Tobralcon, Tobrasol) 0.3% qid to q1h
fortified tobramycin 13.6 mg / mL up to q1h
Fluoroquinolones
besifloxacin (Besivance) 0.6% tid to q1h
ciprofloxacin (Ciloxan) 0.3% solution or ointment qid to q1h
ciprofloxacin (Cipro) 500–750 mg PO bid
gatifloxacin (Zymar) 0.3%, (Zymaxid) 0.5% qid to q1h
levofloxacin (Quixin) 0.5%, (Iquix) 1.5% qid to q1h
levofloxacin (Levaquin) 500 mg PO qd
moxifloxacin (Vigamox, Moxeza) 0.5% tid to q1h
norfloxacin (Chibroxin, Noroxin) 0.3% qid to q1h
ofloxacin (Ocuflox) 0.3% qid to q1h
ofloxacin (Floxin) 200–400 mg PO q12h
Penicillins
amoxicillin /clavulanate (Augmentin) 250 mg PO q8h, or 500 mg PO bid
ampicillin 500 μg / 0.1 mL intravitreal
ampicillin 50–150 mg / 0.5 mL subconjunctival
ampicillin (Polycillin) 4–12 g / day IV in 4 divided doses
methicillin 200–300 mg / kg / day IV in 4 divided doses
penicillin G 12–24 million / units / day IV in 4 divided doses
ticarcillin (Ticar) 200–300 mg / kg / day IV in 3 divided doses
Cephalosporins
cefazolin 100 mg / 0.5 mL subconjunctival
cefazolin 2.25 mg / 0.1 mL intravitreal
cefazolin (Ancef) 50–100 mg / kg / day IV in 3–4 divided doses
fortified cefazolin 50–100 mg / mL up to q1h
cefotaxime (Claforan) 25 mg / kg IV q8–12 h
ceftazidime 2.25 mg / 0.1 mL intravitreal
ceftazidime 100 mg / 0.5 mL subconjunctival
ceftazidime (Fortaz) 2 g IV q8h
fortified ceftazidime 50–100 mg / mL up to q1h
ceftriaxone 100 mg / 0.5 mL subconjunctival
ceftriaxone (Rocephin) 2 gm IV q12h
cephalexin (Keflex) 500 mg PO bid
Macrolides
azithromycin (Azasite) 1% bid for 2 days then qd for 5 days
azithromycin (Zithromax) 250–600 mg PO Z-Pak
erythromycin (Ilotycin, AK-Mycin, Romycin) 0.5% qd to qid
erythromycin 0.5 mg / 0.1 mL intravitreal
erythromycin 100 mg / 0.5 mL subconjunctival
Peptides
bacitracin (AK-Tracin) qd to qid
neomycin–polymyxin B–bacitracin (AK-Spore, Neosporin, Ocutricin) qid to q2h
polymyxin B–bacitracin (Polysporin, AK-Poly Bac, Polycin B) qid to q4h
polymyxin B–oxytetracycline (Terak, Terramycin) qid to q4h
trimethoprim–polymyxin B (Polytrim) qid to q1h
vancomycin 1 mg / 0.1 mL intravitreal
vancomycin 25 mg / 0.5 mL subconjunctival
vancomycin 1 g IV q12h
fortified vancomycin 25–50 mg / mL up to q1h
Sulfonamides
trimethoprim / sulfamethoxazole (Bactrim) 1 double-strength tablet PO bid
Tetracyclines
minocycline 25–100 mg PO qd
tetracycline 250–500 mg PO qd
tetracycline (Achromycin) 1% qid to q2h
Miscellaneous antibiotics
clindamycin (Cleocin) 200 μg / 0.1 mL intravitreal
clindamycin (Cleocin) 50 mg / mL up to q1h
clindamycin (Cleocin) 15–50 mg / 0.5 mL subconjunctival
clindamycin (Cleocin) 300 mg PO qid
clindamycin (Cleocin) 600–900 mg IV q8h
Antibiotic / steroid combinations
gentamicin–prednisolone acetate 0.6% (Pred-G) solution or ointment qid to q2h
neomycin–dexamethasone 0.05% (NeoDecadron) qid to q2h
neomycin–polymyxin B–dexamethasone (AK-Trol, Maxitrol, Dexacidin, Dexasporin) qid to q2h
neomycin–polymyxin B–hydrocortisone (AK-Spore HC, Cortisporin) qid to q2h
neomycin–polymyxin B–prednisolone acetate (Poly-Pred Liquifilm) qid to q2h
oxytetracycline–hydrocortisone acetate (Terra-Cortril) qid
sulfacetamide sodium 10%–flurometholone 1% (FML-S) qid to q4h
sulfacetamide sodium 10%–prednisolone acetate 0.2% (Blephamide) solution or ointment qid to q4h
sulfacetamide sodium 10%–prednisolone acetate 0.5% (Ak-Cide, Metimyd) solution or ointment qid to q4h
sulfacetamide sodium 10%–prednisolone phosphate 0.25% (Isopto Cetapred, Vasocidin) qid to q4h
sulfacetamide sodium 10%–prednisolone phosphate 0.25% (Cetapred) ointment qid to q4h
tobramycin 0.3%–dexamethasone 0.05% (Tobradex ST) solution qid to q2h
tobramycin 0.3%–dexamethasone 0.1% (Tobradex) solution or ointment qid to q2h
tobramycin 0.3%–loteprednol etabonate 0.5% (Zylet) qid to q2h
Antiamoebics
hexamidine (Desomedine) 0.1% up to q1h
paromomycin (Humatin) 10 mg / mL up to q1h
polyhexamethylene biguanide (PHBG, Baquacil) 0.02% up to q1h
propamidine isethionate (Brolene) 0.1% up to q1h
Antifungals
amphotericin B 0.1–0.5% up to q1h
amphotericin B 0.25–1.0 mg / kg IV over 6 hours
amphotericin B 5 mg / 0.1 mL intravitreal
clotrimazole 1% up to q1h
fluconazole (Diflucan) 800 mg PO loading dose, 400 mg / day maintenance
fluconazole (Diflucan) 0.2% up to q1h
flucytosine (Ancobon) 50–150 mg / kg / day IV in 4 divided doses
ketoconazole 1–2% up to q1h
ketoconazole (Nizoral) 200–400 mg PO qd to tid
metronidazole 0.75% ointment qd
miconazole 1% up to q1h
miconazole 25 μg / 0.1 mL intravitreal
miconazole 30 mg / kg / day IV
natamycin (Natacyn) 5% up to q1h
voriconazole 1% up to q 1 h
Antivirals
famciclovir (Famvir) 250–500 mg; for herpes simplex virus: 250–500 mg PO qd to tid; for herpes zoster virus: 500 mg PO tid for 7 days.
foscarnet (Foscavir) induction: 90–120 mg / kg IV bid for 14–21 days; maintenance: 90–120 mg / kg IV qd
ganciclovir (Cytovene) induction: 5 mg / kg IV bid for 14–21 days; maintenance: 5 mg / kg IV qd
ganciclovir (Zirgan) 0.15% gel tid to 5 times a day
idoxuridine (Herplex, Stoxil) 0.1% solution, 0.5% ointment qd to 5 times a day
trifluridine (Viroptic) 1% qd to 9 times a day
valacyclovir (Valtrex) 500–1000 mg; for herpes simplex virus: 500–1000 mg PO qd to tid; for herpes zoster virus: 1 g PO tid for 7 days
vidarabine (Vira-A) 3% qd to 5 times a day
Anti-inflammatory medications
NSAIDs
bromfenac (Bromday) 0.09% (Prolensa) 0.07% qd
celecoxib (Celebrex) 100 mg PO bid
diclofenac sodium (Voltaren) 0.1% qd to qid
diclofenac sodium (Voltaren) 75 mg PO bid
diflunisal (Dolobid) 250–500 mg PO bid
flurbiprofen sodium (Ocufen) 0.03% for prevention of intraoperative miosis
indomethacin (Indocin) 50 mg PO bid to tid
ketorolac tromethamine (Acular) 0.5% (Acuvail) 0.45% (Acular LS) 0.4% qd to qid
naproxen (Naprosyn) 250 mg PO bid
nepafenac (Nevanac) 0.1% tid (Ilevro) 0.3% qd
suprofen (Profenal) 1% for prevention of intraoperative miosis
Immunomodulator
cyclosporine (ciclosporin) (Restasis) 0.05% bid
Steroids
dexamethasone alcohol (Maxidex) 0.1% qd to q1h
dexamethasone sodium phosphate (Decadron, AK-Dex) 0.05–0.1% qd to q1h
difluprednate (Durezol) 0.05% qd to q1h
fluorometholone acetate (Flarex, Eflone) 0.1% qd to q1h
fluorometholone alcohol (Fluor-Op, FML) 0.1% (FML Forte) 0.25% qd to q1h
fluorometholone alcohol (FML S.O.P.) 0.1% ointment qd to q1h
loteprednol etabonate (Lotemax [suspension, gel, ointment]) 0.5% (Alrex) 0.2% qd to q1h
medrysone (HMS) 1% qd to q1h
prednisolone acetate (Pred Mild) 0.12% (Econopred) 0.125% (AK-Tate, Pred Forte, Econopred Plus) 1% qd to q1h
prednisolone sodium phosphate (Inflamase Mild, AK-Pred) 0.125% (Inflamase Forte, AK-Pred) 1% qd to q1h
prednisone 60–100 mg PO qd followed by taper; co-therapy (to prevent peptic ulcer disease) with famotidine (Pepcid), lansoprazole (Prevacid), omeprazole (Prilosec), or ranitidine (Zantac)
rimexolone (Vexol) 1% qd to q1h
Ocular Hypotensive (Glaucoma) Medications
Alpha-Adrenergic Receptor Agonists (Purple Cap)
Mechanism of action: Inhibit aqueous production, may enhance uveoscleral outflow.
apraclonidine (Iopidine) 0.5% tid or 1.0% bid
brimonidine (Alphagan-P) 0.15% 0.1% (Alphagan) 0.2% tid
Side effects: Superior lid retraction, miosis, blanching of conjunctival vessels, dry mouth, dry nose, tachyphylaxis, lethargy, headache, allergic reactions
dipivefrin (Propine) 0.1% bid
epinephrine (Glaucon, Epifrin, Epitrate) 0.25%, 0.5%, 1%, 2% bid
Side effects: Cystoid macular edema in aphakic eyes, hypertension, tachycardia, adrenochrome deposits in conjunctiva (epinephrine)
Beta-Blockers (Yellow or Blue Cap)
betaxolol (Betoptic S) 0.25% (Betoptic) 0.5% bid
carteolol (Ocupress) 1.5%, 3% bid
levobetaxolol (Betaxon) 0.5% bid
levobunolol (Betagan) 0.25–0.5% qd or bid
metipranolol (OptiPranolol) 0.3% bid
timolol (Timoptic, Betimol, Ocudose [preservative free]) 0.25%, 0.5% bid or (Istalol) 0.5% qd,
timolol gel (Timoptic-XE) 0.25%, 0.5% qd
Side effects: Bradycardia, bronchospasm (contraindicated in asthmatics), hypotension, depression, lethargy, decreased libido, impotence, decreased serum HDL levels (except carteolol)
Cholinergic Agonists (Miotics; Green Cap)
Mechanism of action: Enhance trabecular outflow, may enhance uveoscleral outflow.
carbachol (Isopto Carbachol, Miostat [intraocular 0.01%]) 0.75%, 1.5%, 2.25%, 3% tid
echothiophate (Phospholine iodide) 0.03%, 0.0625%, 0.125%, 0.25% bid
pilocarpine (Pilocar, Ocusert, Isopto Carpine, Pilopine HS gel) 0.5%, 1%, 2%, 3%, 4%, 6% qid (qhs for gel)
Side effects: Miosis, induced myopia, accommodative spasm, brow ache, pupillary block, angle closure
Carbonic Anhydrase Inhibitors (Orange Cap)
Mechanism of action: Inhibit aqueous production.
acetazolamide (Diamox; 125 to 250 mg tablets, 500 mg Sequels) up to 1 g PO qd in divided doses
brinzolamide (Azopt) 1% tid
dorzolamide (Trusopt) 2% tid
methazolamide (Neptazane) 25–50 mg PO bid to tid
Side effects: Lethargy, depression, aplastic anemia, thrombocytopenia, agranulocytosis, Stevens–Johnson syndrome, paresthesias, renal stones, diarrhea, nausea (especially for oral medications), transient myopia, loss of libido, metallic taste. Remember that these agents are sulfonamide derivatives; beware in sulfa-allergic patients
Prostaglandin Analogues (Turquoise / Teal Cap)
Mechanism of action: Enhance uveoscleral outflow.
bimatoprost (Lumigan) 0.01% qd
latanoprost (Xalatan) 0.005% qd
tafluprost (Zioptan) 0.0015% qd
travoprost (Travatan) 0.004% qd
unoprostone isopropyl (Rescula) 0.15% bid (docosanoid compound related to prostaglandin analogues)
Side effects: Iris and eyelid pigmentation, iritis, conjunctival hyperemia, cystoid macular edema, hypertrichosis, reactivation of HSV keratitis, flu-like symptoms, prostaglandin-associated periorbitopathy (PAP: upper lid ptosis, deepening of upper lid sulcus, involution of dermatochalasis, periorbital fat atrophy, mild enophthalmos, inferior scleral show, increased prominence of lid vessels, tight eyelids)
Hyperosmotics
Mechanism of action: Shrink vitreous by creating osmotic gradient.
glycerin (Osmoglyn) 50% 8 oz PO
mannitol (Osmitrol) up to 2 g / kg IV of 20% solution over 30–60 minutes
isosorbide (Ismotic) up to 2 g / kg PO of 45% solution
Side effects: Backache, headache, mental confusion, heart failure, ketoacidosis (glycerin in diabetic patients), nausea, emesis
Combinations
brimonidine 0.2%–timolol 0.5% (Combigan) bid
brinzolamide 1%–brimonidine 0.2% (Simbrinza) tid
dorzolamide 2%–timolol 0.5% (Cosopt) bid
Allergy Medications
alcaftadine (Lastacaft) 0.25% qd
azelastine hydrochloride (Optivar) 0.05% bid
bepotastine besilate (Bepreve) 1.5% bid
cetirizine (Zyrtec) 5–10 mg PO qd
cromolyn sodium (Crolom, Opticrom) 4% qd to q4h
desloratadine (Clarinex) 5 mg PO qd
emedastine (Emadine) 0.05% qid
epinastine hydrochloride (Elestat) 0.05% bid
fexofenadine (Allegra) 60 mg PO bid; 180 mg PO qd
ketorolac tromethamine (Acular) 0.5% qid
ketotifen fumarate (Zaditor, Alaway) 0.025% bid
levocabastine (Livostin) 0.05% qid
lodoxamide tromethamine (Alomide) 0.1% qd to qid
loratadine (Claritin) 10 mg PO qd
loteprednol etabonate (Alrex) 0.2% qid
naphazoline (Naphcon, Vasocon) qd to qid
naphazoline–antazoline (Vasocon A) qd to qid
naphazoline–pheniramine (Naphcon-A, Opcon-A, Ocuhist) qid
nedocromil sodium (Alocril) 2% bid
olopatadine hydrochloride (Patanol) 0.1% bid or (Pataday) 0.2% qd
pemirolast potassium (Alamast) 0.1% bid
Mydriatics / Cycloplegics
atropine sulfate (Atropisol, Isopto Atropine) 0.5%, 1%, 2% qd to qid
cyclopentolate (Cyclogyl) 0.5%, 1%, 2% qd to qid
eucatropine 5–10% qd to qid
homatropine (Isopto Homatropine) 2%, 5% qd to qid
hydroxyamphetamine hydrobromide 1% / tropicamide 0.25% (Paremyd) qd to qid (onset within 15 minutes, recovery begins within 90 minutes)
phenylephrine (Neo-Synephrine, Mydfrin) 2.5%, 5%, 10% for pupillary dilation
scopolamine (Isopto Hyoscine) 0.25% qd to qid
tropicamide (Mydriacyl) 0.5%, 1% for pupillary dilation
Anesthetics
bupivacaine (Marcaine) 0.25–0.75% for peribulbar / retrobulbar injection
chloroprocaine (Nesacaine) 1–2% solution
cocaine 1–10% for topical anesthesia, pupil testing (Horner’s syndrome)
fluorescein (Fluress [with benoxinate 0.4% anesthetic]) 0.25–2% for examination of conjunctiva, cornea, and intraocular pressure
lidocaine (Xylocaine) 0.5–4% for topical anesthesia (preservative free for intracameral anesthesia)
mepivacaine (Carbocaine) 1–2% solution
proparacaine (Ophthaine) 0.5% for topical anesthesia
procaine (Novocain) 0.5–2% solution
tetracaine (Pontocaine) 0.5% for topical anesthesia
Miscellaneous
acetylcholine (Miochol; 1:100 [20 mg]) 0.5–2 mL intracameral for miosis during surgery
acetylcysteine (Mucomyst) 10–20% up to q4h
aminocaproic acid (Amicar) 50–100 mg / kg PO q4h up to 30 g / day
cysteamine (Cystaran) 0.44% for corneal cysteine crystals
dapiprazole (Rev-Eyes) 0.5% for reversing pupillary dilation
edrophonium (Tensilon) 10 mg IV
hydroxyamphetamine (Paredrine) 1% for pupil testing (Horner’s syndrome)
methacholine (Mecholyl) 2.5% for pupil testing (Adie’s pupil)
ocriplasmin (Jetrea) 0.125 mg intravitreal injection
sodium chloride (Adsorbonac, Muro 128) 2.5%, 5% solution or ointment qd to qid
Color Codes for Topical Ocular Medication Caps
(Based on the American Academy of Ophthalmology recommendations to the FDA to aid patients in distinguishing among drops and thus minimize the chance of using an incorrect medication.)
| Class | Color |
| Anti-infectives | Tan |
| Steroids | Pink, White |
| Nonsteroidal anti-inflammatories | Gray |
| Mydriatics / cycloplegics | Red |
| Miotics | Green |
| β-Blockers | Yellow or blue |
| α-Adrenergic agonists | Purple |
| Carbonic anhydrase inhibitors | Orange |
| Prostaglandin analogues | Turquoise |
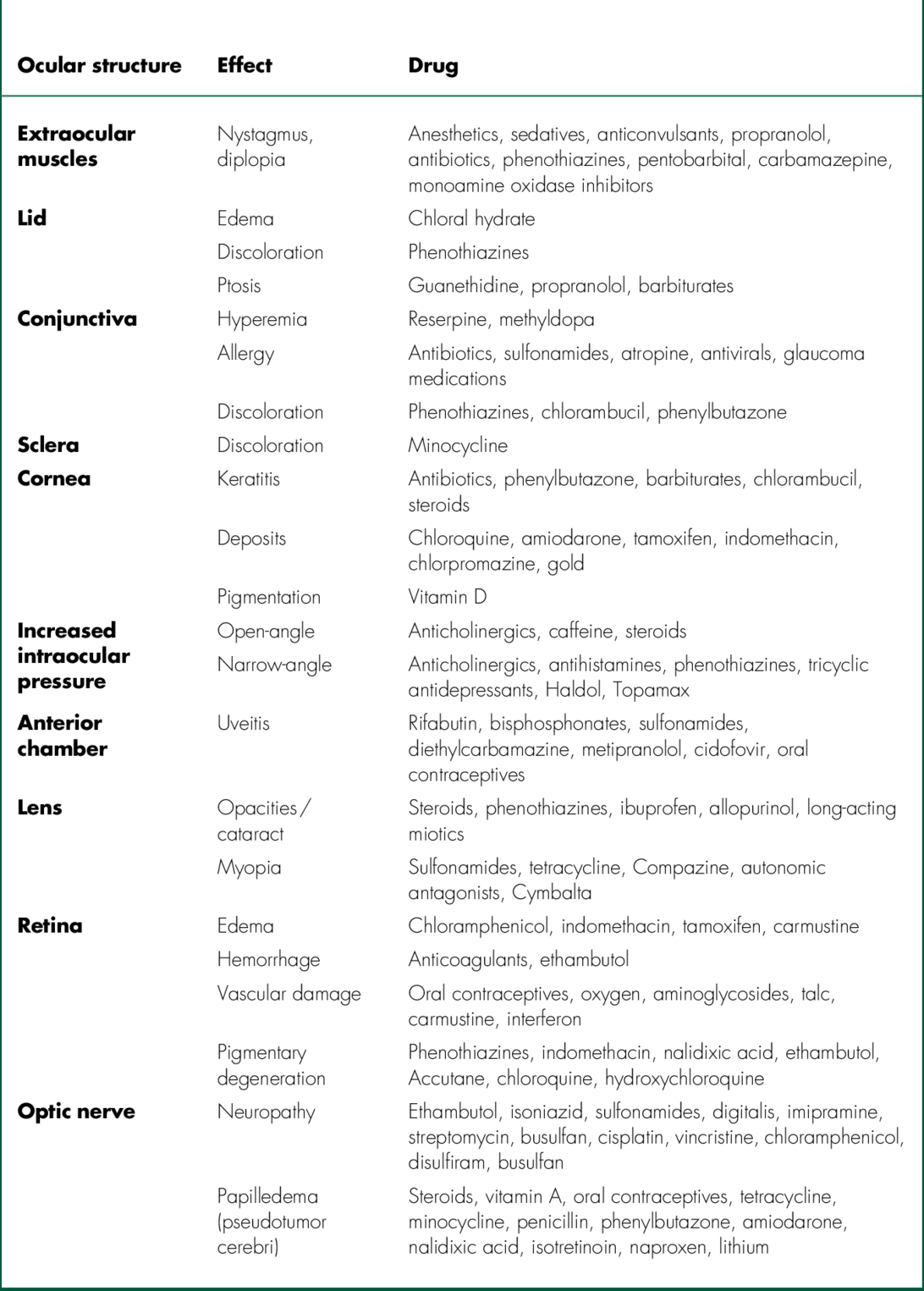
Ocular Toxicology
List of Important Ocular Measurements
List of Eponyms
Adie’s pupil: Tonic pupil that demonstrates cholinergic supersensitivity
Alexander’s law: Jerk nystagmus, usually increases in amplitude with gaze in direction of the fast phase
Argyll Robertson pupil: Small, irregular pupils that do not react to light but do respond to accommodation; occurs in syphilis
Arlt’s line: Horizontal palpebral conjunctival scar in trachoma
Arlt’s triangle: (Ehrlich–Türck line) base-down triangle of central keratic precipitates in uveitis
Amsler sign: (Amsler–Verrey sign) bleeding of abnormal anterior chamber angle vessels when IOP is rapidly lowered surgically (i.e., with paracentesis) in patients with Fuchs’ heterochromic iridocyclitis
Bergmeister’s papilla: Remnant of fetal glial tissue at optic disc
Berlin nodules: Clumps of inflammatory cells in anterior chamber angle in granulomatous uveitis
Berlin’s edema: (Commotio retinae) whitening of retina in the posterior pole from disruption of photoreceptors after blunt trauma
Bielschowsky phenomenon: Downdrift of occluded eye as increasing neutral-density filters are placed over fixating eye in dissociated vertical deviation (DVD)
Bitot’s spot: White, foamy-appearing area of keratinizing squamous metaplasia of bulbar conjunctiva in vitamin A deficiency
Bonnet’s sign: Hemorrhage at arteriovenous crossing in branch retinal vein occlusion
Boston’s sign: Lid lag on downgaze in thyroid disease
Brushfield spots: White-gray spots on peripheral iris in Down’s syndrome
Busacca nodules: Clumps of inflammatory cells on front surface of iris in granulomatous uveitis
Coats’ ring: White granular corneal stromal opacity containing iron from previous metallic foreign body
Cogan’s sign: Upper eyelid twitch when patient with ptosis refixates from downgaze to primary position; nonspecific finding in myasthenia gravis; also refers to venous engorgement over lateral rectus muscle in thyroid disease
Collier’s sign: Bilateral eyelid retraction associated with midbrain lesions
Czarnecki’s sign: Segmental pupillary constriction with eye movements due to aberrant regeneration of cranial nerve III
Dalen–Fuchs nodules: Small, deep, yellow retinal lesions composed of inflammatory cells seen histologically between retinal pigment epithelium and Bruch’s membrane in sympathetic ophthalmia (also in sarcoidosis, Vogt–Koyanagi–Harada syndrome)
Dalrymple’s sign: Widened palpebral fissure secondary to upper eyelid retraction in thyroid disease
Depression sign of Goldberg: Focal loss of nerve fiber layer after resolution of cotton-wool spot
Ehrlich–Türck line: (See Arlt’s triangle)
Elschnig pearls: Cystic proliferation of residual lens epithelial cells on capsule after cataract extraction
Elschnig spot: Yellow patches (early) of retinal pigment epithelium overlying area of choroidal infarction in hypertension, eventually becomes hyperpigmented scar with halo
Enroth’s sign: Eyelid edema in thyroid disease
Ferry’s line: Corneal epithelial iron line at edge of filtering bleb
Fischer–Khunt spot: (Senile scleral plaque) blue-gray area of hyalinized sclera anterior to horizontal rectus muscle insertions in elderly individuals
Fleischer ring: Corneal basal epithelial iron ring at base of cone in keratoconus
Fuchs’ spots: Pigmented macular lesions (retinal pigment epithelial hyperplasia) in pathologic myopia
Globe’s sign: Lid lag on upgaze in thyroid disease
Guiat’s sign: Tortuosity of retinal veins in arteriosclerosis
Gunn’s dots: Light reflections from internal limiting membrane around disc and macula
Gunn’s sign: Arteriovenous nicking in hypertensive retinopathy
Haab’s striae: Breaks in Descemet’s membrane (horizontal or concentric with limbus) in congenital glaucoma (versus vertical tears associated with birth trauma)
Hassall–Henle bodies: Peripheral hyaline excrescences on Descemet’s membrane due to normal aging
Henle’s layer: Obliquely oriented cone fibers in fovea
Herbert’s pits: Scarred limbal follicles in trachoma
Hering’s law: Equal and simultaneous innervation to yoke muscles during conjugate eye movements
Hirschberg’s sign: Pale, round spots (Koplik spots) on conjunctiva and caruncle in measles
Hollenhorst plaque: Cholesterol embolus usually seen at vessel bifurcations, associated with amaurosis fugax and retinal artery occlusions
Horner–Trantas dots: Collections of eosinophils at limbus in vernal conjunctivitis
Hudson–Stahli line: Horizontal corneal epithelial iron line at inferior one-third of cornea due to normal aging
Hutchinson’s pupil: Fixed, dilated pupil in comatose patient due to uncal herniation and compression of cranial nerve III
Hutchinson’s sign: Involvement of tip of nose in herpes zoster ophthalmicus (nasociliary nerve involvement)
Hutchinson’s triad: Three signs of congenital syphilis – interstitial keratitis, notched teeth, and deafness
Kayes’ dots: Subepithelial infiltrates in corneal allograft rejection
Kayser–Fleischer ring: Limbal copper deposition in Descemet’s membrane that occurs in Wilson’s disease
Khodadoust line: Corneal graft endothelial rejection line composed of inflammatory cells
Klein’s tags: Yellow spots at base of macular hole
Koeppe nodules: Clumps of inflammatory cells at pupillary border in granulomatous uveitis
Krukenbergspindle: Bilateral, central, vertical corneal endothelial pigment deposits in pigment dispersion syndrome
Kunkmann–Wolffian bodies: Small white peripheral iris spots that resemble Brushfield spots but occur in normal individuals
Kyreileis’ plaques: White–yellow vascular plaques in toxoplasmosis
Lander’s sign: Inferior preretinal nodules in sarcoidosis
Lisch nodules: Iris melanocytic hamartomas in neurofibromatosis
Loops of Axenfeld: Dark limbal spots representing scleral nerve loops
Mittendorf’s dot: White spot (remnant of hyaloid artery) at posterior lens surface
Mizuo–Nakamura phenomenon: Loss of abnormal macular sheen with dark adaptation in Oguchi’s disease
Morgagnian cataract: Hypermature cortical cataract in which liquified cortex allows nucleus to sink inferiorly
Munson’s sign: Protrusion of lower lid with downgaze in keratoconus
Panum’s area: Zone of single binocular vision around horopter
Parry’s sign: Exophthalmos in thyroid disease
Paton’s lines: Circumferential peripapillary retinal folds due to optic nerve edema
Paton’s sign: Conjunctival microaneurysms in sickle cell disease
Pseudo–von Graefe sign: Lid elevation on adduction or downgaze due to aberrant regeneration of cranial nerve III
Pulfrich phenomenon: Perception of stereopsis (elliptical motion of a pendulum) due to difference in nerve conduction times between eyes and cortex, seen in multiple sclerosis
Purkinje images: Reflected images from front and back surfaces of cornea and lens
Purkinje shift: Shift in peak spectral sensitivity from photopic (555 nm, cones) to scotopic (507 nm, rods) conditions
Riddoch phenomenon: Visual field anomaly in which a moving object can be seen whereas a static one cannot
Rizutti’s sign: Triangle of light on iris from oblique penlight beam focused by cone in keratoconus
Roth spots: Intraretinal hemorrhages with white center in subacute bacterial endocarditis, leukemia, severe anemia, collagen vascular diseases, diabetes mellitus, and multiple myeloma
Salus’ sign: Retinal vein angulation (90°) at arteriovenous crossing in hypertension and arteriosclerosis
Sampaoelesi’s line: Increased pigmentation anterior to Schwalbe’s line in pseudoexfoliation syndrome
Sattler’s veil: Superficial corneal edema (bedewing) caused by hypoxia (contact lens)
Scheie’s line: Pigment on lens equator and posterior capsule in pigment dispersion syndrome
Schwalbe’s line: Angle structure representing peripheral edge of Descemet’s membrane
Schwalbe’s ring: Posterior embryotoxon (anteriorly displaced Schwalbe’s line)
Seidel test: Method of detecting wound leak by observing aqueous dilute concentrated fluorescein placed over the suspected leakage site
Shafer’s sign: Anterior vitreous pigment cells (tobacco-dust) associated with retinal tear
Sherrington’s law: Contraction of muscle causes relaxation of antagonist (reciprocal innervation)
Siegrist streak: Linear chain of hyperpigmented spots over sclerosed choroidal vessel in chronic hypertension or choroiditis
Soemmering’s ring cataract: Residual peripheral cataractous lens material following capsular rupture and central lens resorption from trauma or surgery
Spiral of Tillaux: Imaginary line connecting insertions of rectus muscles
Stocker’s line: Corneal epithelial iron line at edge of pterygium
Sugiura’s sign: Perilimbal vitiligo associated with Vogt–Koyanagi–Harada syndrome
Tenon’s capsule: Fascial covering of eye
Uhthoff’s symptom: Decreased vision / diplopia secondary to increased body temperature (e.g., exercise or hot shower); occurs after recovery in optic neuritis
van Trigt’s sign: Venous pulsations on optic disc (normal finding)
Vogt’s sign: White anterior lens opacities (glaukomflecken) caused by ischemia of lens epithelial cells from previous attacks of angle closure
Vogt’s striae: Deep stromal vertical stress lines at apex of cone in keratoconus
Von Graefe’s sign: Lid lag on downgaze in thyroid disease
Vossius ring: Ring of iris pigment from pupillary ruff deposited onto anterior lens capsule after blunt trauma
Watzke–Allen sign: Patient with macular hole perceives break in light when a slit-beam is focused on the fovea
Weiss ring: Ring of adherent peripapillary glial tissue on posterior vitreous surface after posterior vitreous detachment
Wessely ring: Corneal stromal infiltrate of antigen–antibody complexes
White lines of Vogt: Sheathed or sclerosed vessels seen in lattice degeneration
Wieger’s ligament: Attachment of hyaloid face to back of lens
Willebrandt’s knee: Inferonasal optic nerve fibers that decussate in chiasm and loop into contralateral optic nerve before traveling back to optic tract