Antiemetic agents
Nausea and vomiting represent an extremely distressing and financially costly problem, the risk of which has increased as the fields of anesthesia, surgery, and cancer chemotherapy have advanced. Many drugs are now available to treat and provide prophylaxis against the myriad of situations that give rise to nausea and vomiting (Figures 98-1 and 98-2).
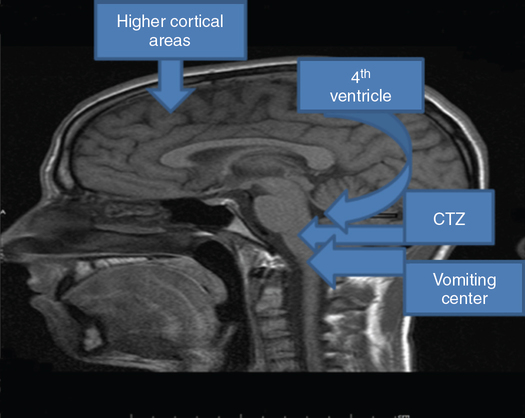
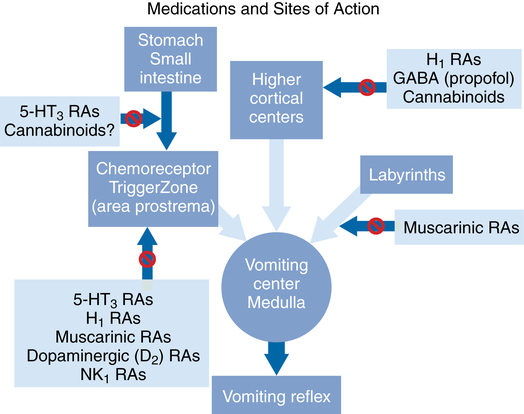
From studies in the 1950s, a model of the emetic reflex emerged (which has been subsequently validated), consisting of a chemoreceptor trigger zone (CTZ) in the area postrema and a vomiting center in the brainstem. Nausea and vomiting result from chemical or neural stimulation of the vomiting center. Chemical activation is mediated via the CTZ, which is sensitive to the presence of toxins and poisons in the bloodstream (see Figure 98-1). Neural activation occurs as a result of information coming directly from the frontal lobes of the brain, the digestive tract, and the balancing mechanism of the inner ear.
The CTZ is susceptible to stimulation from the release of dopamine and serotonin (5-HT) in the blood and cerebrospinal fluid and may also be activated by opioids and certain anesthetic agents. In addition, the release of 5-HT from the gastrointestinal tract can stimulate the CTZ. The vestibular system sends input to the vomiting center in response to changes in motion and pressure. The reflex afferent pathway from the cerebral cortex stimulates the vomiting center in response to such factors as pain, anxiety, and visual, sensory, or cognitive overload (see Figure 98-2).





