Chapter 213 Anterior Cervical Corpectomy and Fusion
To Plate or Not to Plate
Not to Plate
Anterior cervical corpectomy, with or without plating, has been reported to achieve high fusion rates, improvement in myelopathy, and good to excellent outcomes.1–13 However, complications increase as the number of levels increases.2,3 Postoperative dislodgement of a long strut graft is one of the most feared complications of this procedure. Pseudarthrosis, graft migration, graft fracture, segmental kyphosis, and graft displacement also have been reported2,5-10 as potential complications of corpectomy and fusion without ventral plating. With the advent and evolution of ventral cervical plating, it was assumed that the addition of a plate would reduce the complications associated with the procedure. In the current age of spinal instrumentation, it seems obvious that this technology must be used to improve fusion rates, allow for faster mobilization, prevent complications related to graft displacement, and improve clinical outcomes. Data are lacking to support this theory, however, especially in the case of multilevel cervical corpectomy.
Many studies have reported a paradoxical increase in complications when ventral plating alone was used for internal fixation. Plates added the complications of plate failure, screw back-out or breakage, and reported esophageal or pharyngeal injury. With graft subsidence, the plate or caudal screws often damaged the adjacent level. Plate dislodgement with airway compromise and death has been reported.14 Catastrophic graft and plate dislocations occurred despite postoperative use of hard cervical spine collars and even halos.1,3,4 Thus, ventral plating does not convincingly reduce the need for postoperative orthosis after multilevel strut grafting. Clinical series also show an increased rate of reoperation with the use of a ventral plate over the historical rates without plating. Graft migration or subsidence in multilevel corpectomy without a plate was largely managed nonoperatively without clinical sequelae.2 In plated constructs, incomplete graft migration or excessive subsidence was associated with instrumentation failure, which generally cannot be managed without hardware revision. In addition, higher rates of complete graft dislodgement are found in plated multilevel cervical corpectomy.1,3,15
With three-level corpectomy, the addition of dorsal instrumentation provides optimal results.1,3,4 Biomechanical studies have not shown that any additional stability results from adding a ventral plate once dorsal instrumentation has been performed.16,17 Situations such as postlaminectomy kyphosis, osteoporosis, oncologic reconstructions, and severe deformity still may be indications for ventral cervical plating after corpectomy.4 However, maintaining that ventral plate placement after anterior cervical corpectomy is standard overstates the benefits of plating and ignores multiple clinical studies and biomechanical data to the contrary. Given the absence of class I evidence or comparative series for ventral cervical plating following multilevel cervical corpectomy, this chapter reviews the evidence for not plating reconstructions following anterior cervical corpectomy.
Historical Review
Cervical corpectomy including multilevel strut graft techniques has been reported since the early 1980s.13 Caspar introduced ventral cervical plates in 1991.18 Plating systems evolved over time, and the technology was extended to include cervical corpectomy. Cervical corpectomy with the addition of plating, however, revealed a paradoxical increase in the complications of both graft failure and hardware failure, most notably in multilevel corpectomy and reconstruction. Graft failure in these patients often was an early postoperative event. The grafts frequently failed by inferior and ventral displacement of the graft or by pull-out of the screw and plate from the inferior vertebrae of the construct.1,3,15
Plates evolved from nonlocking plates that used bicortical screws to unicortical locking plate systems and, most recently, dynamic plates. Constrained plates with unicortical locking screws were reported to loosen and pull away from the ventral cervical spine despite successful fusion of the graft.1 Also, as the graft subsided, the caudal screws of the plate had the potential to cut into the adjacent disc, necessitating reoperation.4 Dynamic plates have been promoted due to improved load sharing across the plate and resultant fusion rates.19 Graft subsidence and loss of lordosis, however, have been shown to be higher with dynamic plating systems.20 Excessive graft subsidence adversely affects the caudal screws of a dynamic plate in the same as it affects a constrained plate.
Biomechanical Studies
DiAngelo and Foley described reversal of the load transfer with plated multilevel strut grafts. With plating, the graft is unloaded in flexion and excessively loaded with extension. After plating, even a small degree of extension (7.5 degrees) caused the strut graft to fail at the caudal vertebra with fracture of the lower vertebra, excessive graft subsidence, graft dislodgement, or plate failure.21,22 These same patterns of graft failure are found in clinical series.1,3,4,15 The stand-alone graft in comparison is loaded in flexion and unloaded in extension.21,22
Brodke et al. showed biomechanical superiority of dynamic plates after simulated subsidence in a single-level corpectomy model due to the load sharing across the graft.23 Clinical studies have confirmed that dynamic plates increase fusion rates.19 It is important to remember, however, that graft dislodgement is generally an early postoperative event prior to the anticipated failure from lack of fusion.1,3 Furthermore, both dynamic plates and constrained plates would be expected to provide a tensile force during extension.
Kirkpatrick et al. studied the biomechanics of three-level corpectomies. Intact specimens, graft alone, ventral plating alone, and dorsal instrumentation alone were compared. Dorsal instrumentation was found to have a greater strength and stiffness in both flexion and extension than a ventral plate. Dorsal fixation provides segmental instrumentation at the level of the corpectomy, as well as above and below, thereby applying three-point bending forces that cannot be achieved with ventral plating.24
Koh et al. compared ventral, dorsal, or ventral-dorsal stabilization of three-column injuries in the cervical spine. Dorsal instrumentation was superior to ventral plating, and the addition of a ventral plate did not significantly increase stability compared with dorsal plating and interbody grafting.16
Singh et al. studied a two-level corpectomy with ventral plating, dorsal lateral mass screw-rod construct, and combined ventral and dorsal instrumentation. In all pure moments tested, the specimens with dorsal instrumentation outperformed those with ventral plating. No difference was found in any between the dorsal alone and combined ventral-dorsal instrumentation. Furthermore, the authors noted that ventral plating sometimes limited compression of the graft, with the net result being a less biomechanically rigid construct when coupled with dorsal instrumentation.17
Surgical Techniques
Multilevel anterior cervical corpectomy and strut grafting have a steep learning curve. The incidence of early graft dislodgement has been reported to decrease with experience. One critical test for strut graft security is resistance to displacement under flexion and extension under direct visualization prior to wound closure.25 Placement of a plate compounds rather than corrects poor intraoperative strut graft sizing.26 Optimal graft placement and sizing are especially important in the reconstruction following multilevel corpectomy.
The procedure often is performed with intraoperative neuromonitoring. Somatosensory-evoked potentials, motor-evoked potentials, and free running electromyography of C5-T1 all can be used for intraoperative monitoring. In conjunction with total intravenous anesthesia, the integrity of the descending motor tracts, nerve roots, and peripheral nerves can be ensured using these modalities.27 The patient is positioned supine with Gardner-Wells tongs, and cervical traction of 5 to 10 pounds is used initially.
The approach is typically via a transverse incision in the skin on the right or left based on surgeon preference with undermining of the skin above the platysma muscle. The platysma is then divided in line with the muscle fibers, and placement of stay suture at either end can facilitate exposure and obviate the need for a retractor placed superior to inferior. A vertical incision along the ventral border of the sternocleidomastoid has been described25 but is not a requirement for anterior cervical corpectomy even in the multilevel reconstruction.28 Ventral plating over a long segment is aided by the additional exposure and visualization of the plate at both ends simultaneously. Ventral plating also requires additional soft tissue retraction to triangulate the screws at either end and for plate placement. Cervical corpectomy without plating typically does not require this additional exposure or retraction.
Discetomies at each level are performed initially. The corpectomy trough is made in the central two thirds of the vertebral bodies. Generally the trough is between 14 and 18 mm wide. Some authors have advocated preservation of the posterior longitudinal ligament if no instrumentation is planned.28 With removal of the posterior longitudinal ligament, however, graft displacement rates without plate usage were not found to be increased in one series.29 Careful review of preoperative films for rotational deformity or vertebral artery anomalies should minimize the small risk of a catastrophic intraoperative vertebral artery injury. Small curets can be utilized to safely free osteophytes causing spinal cord compression within a kyphotic deformity. Intentional preservation of the posterior longitudinal ligament, when appropriate from the spinal cord decompression standpoint, will add stability to the strut graft if no supplemental instrumentation is planned.28 Bracing to prevent excessive cervical extension should be utilized if no posterior instrumentation is planned.
Prior to placement of the strut graft, skeletal traction is increased to 30 to 40 pounds, reducing any preoperative kyphosis and facilitating a snug graft placement. Depending on the type of graft to be used, the end plates are prepared to accept the allograft, autograft, or cage. With autogenous fibular or iliac crest autograft, the ends of the graft are rounded, and the end plates are fashioned with seating holes, providing a peg-in-hole design.28 Excessive traction has been associated with oversizing of the strut graft, and similar graft failure rates have been found without the use of intraoperative traction.29 Autograft is associated with additional morbidity from the graft harvest site, reportedly as high as 34%.30
Multiple techniques have been employed to limit the morbidity of autograft with and without plating. Fibular allograft also has been used with good results without plating.25,26,29 Titanium mesh cages (TMCs) allow lordotic contouring and can be packed with autograft taken from the corpectomy defect. In this case, the sharp footprint off the titanium mesh will subside into the bony end plate, providing a secure fit.11 End caps should be used at the end of the implant to increase the contact area to minimize subsidence.31 Unfortunately, the end caps usually do not allow variation of orientation relative to the end plate, and cage subsidence is problematic. Daubs reported a high early failure rate of TMC with ventral plating due to subsidence and distal plate extrusion.15
Expandable titanium cages that allow for easy insertion also have been designed. Spikes or contouring at either end allow for fixation to the end plates. The broader surface at each end of this implant decreases subsidence.32 Limits of this implant, however, include decreased space for autograft packing, decreased contact of the autograft at the ends of the graft, inability to contour the implant into lordosis, and limitation of postoperative imaging. Titanium prevents accurate assessment of fusion postoperatively with CT and causes significant interaction with MR imaging of the neural elements in the event of neurologic decline. Finally, the force created by an expandable cage can be large, and adjacent-level fracture in the coronal plane has been reported with expandable cages.33
Lastly, polyetheretherketone (PEEK) now is available in a stackable implant for use in the cervical spine. PEEK grafts are stronger than allograft but softer than titanium and less likely to cause the adjacent bone to collapse. The footprint is significantly wider than TMC, allowing force distribution along the end plate. In addition, the polymer does not interfere with CT scans or MRI, allowing for easier postoperative film interpretation and fusion assessment.34 Clinical studies for efficacy in multilevel cervical corpectomy reconstruction are currently unavailable.
Graft Displacement
In the largest clinical series of anterior cervical corpectomies, which included 249 patients, no plates were used. The rate of graft migration was measured over an average follow-up of 4.7 years. In the 16 graft migrations, only 5 required revision. These five failures requiring revision were described as complete dislocations (>10 mm); all were ventral, and none were associated with neurologic deterioration or respiratory compromise. Eleven patients had incomplete graft displacements measured between 3 and 8 mm but did not require revision. Overall, graft displacement by any amount occurred in 8% of the multilevel (≥2) corpectomy cases, and most were managed nonoperatively. Only 2% of anterior cervical corpectomies in this large series required surgical revision for graft dislodgement without plating.2
In the extreme case of multilevel anterior cervical corpectomy and fusion without plating, Saunders et al. reported 31 cases with four-level anterior cervical corpectomy without plating and long-term follow-up. Three graft displacements occurred in the early postoperative period, and two (6.2%) required reoperation.29
In contrast, graft displacement and reoperation in multilevel corpectomy has been reported to range from 33% to 75% with the use of a plate.1,3,15 Vaccaro et al. reported the largest multicenter study of 45 patients with ventral plating: 33 with two-level corpectomies and 12 with three-level corpectomies. Of these, 24 (73%) of the two-level corpectomies and 10 (83%) of the three-level corpectomies were managed with a postoperative halo. Despite the aggressive postoperative bracing program, 3 of the 33 two-level corpectomies (9%) and 6 of the 12 three-level corpectomies (50%) developed early graft failure. Younger age, halo use, and optimal hardware placement did not prevent early graft failure with the use of a plate. The graft displaced or failed at the inferior vertebral body in 78% of patients. All failures required reoperation. One reoperation to combine ventral and dorsal instrumentation subsequently failed again less than 1 week postoperatively.1
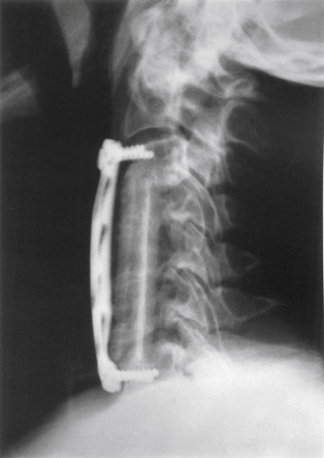
Sasso et al. reported on 40 patients with more than 2 years’ follow-up after multilevel anterior cervical corpectomy with ventral plating. All patients had iliac crest autograft and placement of a constrained plate, and all were kept in a Philadelphia collar for 6 weeks. Two of the 33 patients (6%) undergoing a two-level corpectomy developed a pseudarthrosis, and 5 of 7 patients (71%) with three-level corpectomy had catastrophic graft/plate dislodgement, with the graft excessively subsiding into the inferior vertebral body, kicking the plate out ventrally (Fig. 213-1). All failures required reoperation, and three patients had dorsal instrumentation added. Sasso et al. recommend the addition of dorsal instrumentation with three-level corpectomies.3
Daubs reported a 75% failure rate of multilevel corpectomy reconstructed with a TMC and ventral plating. The report included 15 one-level, 6 two-level, and 2 three-level corpectomies. Two three-level corpectomies and four two-level corpectomies failed in the early postoperative course, for a 75% failure rate. Failure occurred in less than 6 weeks on average (range, 2–10 weeks) postoperatively. Halo and Aspen collars did not prevent failure in this series. At reoperation, the failures were successfully revised to fibular allograft with dorsal instrumentation.15
Patients undergoing cervical corpectomy after laminectomy represent a special situation due to the increased instability of the spine. A corpectomy will disrupt the ventral portion of the vertebral ring, whereas a laminectomy disrupts the dorsal portion of the ring, producing left and right halves of the spine connected only by soft tissue. With only ventral reconstruction, this procedure resulted in early graft complications in 11 of 18 patients (61%) in a study by Riew et al. The authors concluded that with a corpectomy of more than one level in a postlaminectomy patient, a concomitant dorsal instrumented fusion would be required. Again, halo immobilization did not prevent graft-related complications.4
Buttress Plating
Although initially considered useful with dorsal cervical fixation, the addition of a buttress plate on the inferior end of the construct is of questionable value. In an initial report of this technique, 11 patients had stabilization of a multilevel anterior cervical corpectomy with dorsal instrumentation as well as a ventral buttress plate. Although the authors in this initial report concluded that a buttress plate may decrease the incidence of graft and dislodgement, one reoperation was required due to fracture of a fibula autograft caused by a locking screw placed into the graft itself.35
Riew et al. reported an asymptomatic ventral buttress plate dislodgement that occurred following subsidence of fibular allograft despite dorsal instrumentation. Again, an intraoperative allograft fracture from a graft screw occurred. Moreover, the authors reported that without the addition of dorsal instrumentation, buttress plating alone is associated with potentially catastrophic consequences. One patient died from airway compromise on postoperative day 3 caused by graft dislodgement and subsequent plate failure. Because the inferior buttress plate kicked out from the spine at a 45-degree angle, the ventral soft tissues were more impinged upon than would have been the case had only the graft displaced. After this complication, the use of ventral buttress plating was abandoned at Riew’s center.14
Pseudarthrosis
Proponents of ventral instrumentation often refer to a decreased rate of pseudarthrosis with the use of ventral cervical plating. While this argument may be true for multilevel interbody fusion, fusion rates of anterior cervical corpectomy without plating have been reported as 100% by multiple clinical studies with significant follow up.2,5–8 Nothing is 100% successful; however, painful pseudarthrosis following anterior cervical corpectomy is a rare event.25 Pseudarthrosis improvement with only ventral plating following cervical corpectomy becomes a moot point altogether if one considers increased graft displacement postoperatively in multilevel procedures requiring surgical revision. Graft failure typically takes place before fusion would be expected. Only by excluding the significant number of early graft displacements in multilevel cervical corpectomy with ventral plates alone could an improvement in the already high rate of fusion expect to be seen by the addition of a plate.
Esophageal Injury
Dysphagia is a well-recognized complication after ventral cervical plating, with rates as high as 21% at 2-year follow-up by a longitudinal cohort study of 450 patients within the Cervical Spine Research Society. The dysphagia increased according to the number of vertebral levels operated, with rates of 20% for one level, 33% for two levels, and 39% for three or more levels at the 3-month follow-up. Pharyngoesophageal diverticulum following anterior cervical corpectomy with plating was reported by Joanes and Belinchon.36 The authors believed that scar tissue and traction from hardware were the causes of the complication. Newhouse et al. compiled a group of 22 patients with esophageal perforation following ventral cervical spine surgery. Hardware was suspected to be the underlying cause in 25% of the delayed cases.37
Summary
Despite the widespread use of ventral plating in general, no level 1 data support its use over anterior cervical corpectomy without a plate. A randomized prospective comparison between these two procedures has been proposed previously.9 Clinical series have shown a higher rate of reoperation and failure with ventral plating despite the use of extensive bracing in the case of multilevel anterior cervical corpectomy and plating. Biomechanical studies have offered a plausible mechanism by which failure rates are increased by ventral plating. Ventral plating in the setting of multilevel cervical corpectomy has been associated with more catastrophic clinical complications, including neurologic deficits, esophageal injury, and asphyxia.
DiAngelo D., Foley K., Vossel K., et al. Anterior cervical plating reverses load transfer through multilevel strut-grafts. Spine (Phila Pa 1976). 2000;25:783-795.
Foley K., DiAngelo D., Rampersaud Y., et al. The in vitro effects of instrumentation on multilevel cervical strut-graft mechanics. Spine (Phila Pa 1976). 1999;24:2366-2376.
Riew D.K., Hilibrand A.S., Palumbo M.A., Bohlman H.H. Anterior cervical corpectomy in patients previously managed with a laminectomy: short-term complications. J Bone Joint Surg [Am]. 1999;81(7):950-957.
Sasso R.C., Ruggiero R.A.Jr., Reilly T.M., Hall P.V. Early reconstruction failures after multilevel cervical corpectomy. Spine (Phila Pa 1976). 2003;28(2):140-142.
Vaccaro A.R., Falatyn S.P., Scuderi G.J., et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11(5):410-415.
Wang J.C., Hart R.A., Emery S.E., Bohlman H.H. Graft migration or displacement after multilevel cervical corpectomy and strut grafting. Spine (Phila Pa 1976). 2003;28(10):1016-1021.
1. Vaccaro A.R., Falatyn S.P., Scuderi G.J., et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11(5):410-415.
2. Wang J.C., Hart R.A., Emery S.E., Bohlman H.H. Graft migration or displacement after multilevel cervical corpectomy and strut grafting. Spine (Phila Pa 1976). 2003;28(10):1016-1021.
3. Sasso R.C., Ruggiero R.A.Jr, Reilly T.M., Hall P.V. Early reconstruction failures after multilevel cervical corpectomy. Spine (Phila Pa 1976). 2003;28(2):140-142.
4. Riew D.K., Hilibrand A.S., Palumbo M.A., Bohlman H.H. Anterior cervical corpectomy in patients previously managed with a laminectomy: short-term complications. J Bone Joint Surg [Am]. 1999;81(7):950-957.
5. Boni M., Cehrubino P., Denaro V., et al. Multiple subtotal somatectomy. Technique and evaluation of a series of 39 cases. Spine (Phila Pa 1976). 1984;9:358-362.
6. Bernard T.N.Jr, Whitecloud T.S.III. Cervical spondylotic myelopathy and myeloradiculopathy. Anterior decompression and stabilization with autogenous fibula strut grafting. Clin Orthop Relat Res. 1987;221:149-160.
7. Kojima T., Waga S., Kubo Y., et al. Anterior cervical vertebrectomy and interbody fusion for multilevel spondylosis and ossification of the posterior longitudinal ligament. Neurosurgery. 1989;24:864-872.
8. Okada K., Shirasaki N., Hayash H., et al. Treatment of cervical spondylotic myelopathy by enlargement of the spinal canal anteriorly followed by arthrodesis. J Bone Joint Surg [Am]. 1991;73:352-364.
9. Hilibrand A.S., Fey M.A., Emery S.E., et al. Increased rate of arthrodesis with strut grafting after multilevel anterior cervical decompression. Spine (Phila Pa 1976). 2002;27(2):146-151.
10. Cheng N.S., Lau P.Y., Sun L.K., Wong N.M. Fusion rate of anterior cervical plating after corpectomy. J Orthop Surg. 2005;13(3):223-227.
11. Acosta F.L.Jr, Aryan H.E., Chou D., Ames C.P. Long-term biomechanical stability and clinical improvement after extended multilevel corpectomy and circumferential reconstruction of the cervical spine using titanium mesh cages. J Spinal Disord Tech. 2008;21(3):165-174.
12. McAfee P.C., Bohlman H.H., Ducker T.B., et al. One-stage anterior cervical decompression and posterior stabilization. A study of one hundred patients with a minimum of two years of follow-up. J Bone Joint Surg [Am]. 1995;77:1791-1800.
13. Hanai K., Inouye Y., Kwai K., et al. Anterior decompression for myelopathy resulting from ossification of the posterior longitudinal ligment. J Bone Joint Surg [Br]. 1982;64:561-564.
14. Riew K.D., Sethi N.S., Devney J., et al. Complications of buttress plate stabilization of cervical corpectomy. Spine (Phila Pa 1976). 1999;24:2404-2410.
15. Daubs M.D. Early failures following cervical corpectomy reconstruction with titanium mesh cages and anterior plating. Spine (Phila Pa 1976). 2005;30(12):1402-1406.
16. Koh Y.D., Lim T.H., You J.W., et al. A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine (Phila Pa 1976). 2001;26(1):15-21.
17. Singh K., Vaccaro A.R., Kim J., et al. An HS enhancement of stability following anterior cervical corpectomy: a biomechanical study. Spine (Phila Pa 1976). 2004;29(8):845-849.
18. Caspar W. Anterior cervical fusion and interbody stabilization with the trapezial osteosynthetic plate technique. Aesculap Sci Info. 1993;12:3.
19. Nunley P.D., Jawahar A., Kerr E.J., et al. Choice of plate may affect outcomes for single versus multilevel ACDF: results of a prospective randomized single blind trial. Spine J. 2009;9:121-127.
20. Gharhreman, Prashanth J.V., Ferch R.D. Dynamic plates in anterior cervical fusion surgery: graft settling and cervical alignment. Spine (Phila Pa 1976). 2009;34(15):1567-1571.
21. DiAngelo D., Foley K., Vossel K., et al. Anterior cervical plating reverses load transfer through multilevel strut-grafts. Spine (Phila Pa 1976). 2000;25:783-795.
22. Foley K., DiAngelo D., Rampersaud Y., et al. The in vitro effects of instrumentation on multilevel cervical strut-graft mechanics. Spine (Phila Pa 1976). 1999;24:2366-2376.
23. Brodke D.S., Klimo P., Bachas K.N., et al. Anterior cervical fixation: analysis of load sharing and stability with use of static and dynamic plates. J Bone Joint Surg [Am]. 2006;88(7):1566-1573.
24. Kirkpatrick J.S., Levy J.A., Carillo J., Moeini S.R. Reconstruction after multilevel corpectomy in the cervical spine. Spine (Phila Pa 1976). 1999;24(12):1186-1191.
25. Saunders R.L., Berninin P.M., Serreffis T.G. Central corpectomy for cervical spondylotic myelopathy a consequetive series with long term follow up. J Neurosurg. 1992;74:163-170.
26. McDonald R.L., Fehlings M.G., Tator C.H., et al. Multilevel anterior cervical corpectomy and fibular allograft fusion for cervical myelopathy. J Neurosurg. 1997;86:990-997.
27. Gonzalez A.A., Jeyanandarajan D., Hansen C., et al. Intraoperative neurophysiological monitoring during spine surgery: a review. Neurosurg Focus. 2009;27(4):E6.
28. Zdeblick T., Bohlman H. Cervical kyphosis and myelopathy treatment by anterior corpectomy and strut grafting. J Bone Joint Surg [Am]. 1989;71:170-182.
29. Saunders R.L., Pikus H.J., Ball P. Four level cervical corpectomy. Spine (Phila Pa 1976). 1998;23(22):2455-2461.
30. Heary R.F., Schlenk R.P., Sacchieri T.A., et al. Persistent ilac crest donor site pain: independent outcome assessment. Neurosurgery. 2002;50(3):510-516.
31. Chen Y., Chen D., Guo Y., et al. Subsidence of titanium mesh cage: a study based on 300 cases. J Spinal Disord Tech. 2008;21(7):489-492.
32. Ibrahim O., Bekelis K., Gregory A., et al. The use of expandable cages in patients undergoing multilevel corpectomies for metastatic tumors in the cervical spine. Orthopedics. 2010;33:87.
33. Chou D., Lu D.C., Weinstein P., Ames C.P. Adjacent-level vertebral body fractures after expandable cage reconstruction. J Neurosurg Spine. 2008;8(6):584-588.
34. Kulkarni A.G., Hee H.T., Wong H.K. Solis cage (PEEK) for anterior cervical fusion: preliminary radiological results with emphasis on fusion and subsidence. Spine J. 2007;7(2):205-209.
35. Vanichkachorn J.S., Vaccaro A.R., Sivlveri C.P., et al. Anterior junctional plate in the cervical spine. Spine (Phila Pa 1976). 1998;23:2462-2467.
36. Joanes V., Belinchon J. Pharyngoesophageal diverticulum following cervical corpectomy and plating. J Neurosurg Spine. 2008;9(3):258-260.
37. Newhouse K.E., Lindsey R.W., Clark C.R., et al. Esophageal perforation following anterior cervical spine surgery. Spine (Phila Pa 1976). 1989;14(10):1051-1053.
To Plate
The ventral approach for cervical spine surgery has been used for numerous conditions of the cervical spine, including traumatic, degenerative, neoplastic, and infectious lesions. The ventral approach is particularly useful for the treatment of cervical spondylotic myelopathy caused by ventral compression of the spinal cord. Single-level or multilevel cervical corpectomy can be used to decompress the spinal cord and nerve roots. After a corpectomy, an appropriate bone graft (autogenous or allograft) can be placed in the defect to restore structural integrity and to maintain the cervical lordosis. A review of the literature shows that the likelihood of complications after ventral cervical surgery varies according to the number of levels fused, the type of bone graft, and whether the ventral grafting is supplemented with instrumentation.1–18 Although the reported results of single-level corpectomies with strut graft are uniformly good, the rates of pseudarthrosis formation and graft migration are higher with multilevel corpectomies.5,16–18
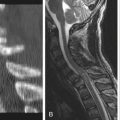
After multilevel corpectomy, the addition of instrumentation to the construct has provided significant advantages.19–22 In most series reporting on treatment without instrumentation, there is a higher incidence of graft-related problems, including pseudarthrosis, graft resorption, and graft migration.4,6,16–18 All of these complications can lead to serious neurologic and biomechanical problems (Fig. 213-2). These problems may necessitate the use of additional methods for stabilization and immobilization of the cervical spine.
Numerous studies have shown the biomechanical advantages of ventral cervical plate fixation.14,23,24 Therefore, in a case of multilevel corpectomy, to prevent postoperative graft-related problems, instrumentation should be added to the construct. The advantages of adding internal fixation in cases of multilevel corpectomy include biomechanical improvements, improved immediate stability, improved fusion rates with acceleration of the fusion process, prevention of graft migration, and, in some instances, obviation of the need for external fixation.
Biomechanical Aspects
A corpectomy effectively diminishes the structural support of the ventral and middle columns of the spine. A ventral cervical fusion without internal fixation may result in tenuous bone graft stability. A bone graft alone, used in the cervical spine, will be subjected to rotational and translational forces in three dimensions.20 When multiple levels are fused, the strut graft creates a lengthy moment arm that is manipulated during spinal movements.4 This results in motion across the graft–vertebral body junction, which is a hindrance to successful fusion. Ventral cervical instrumentation helps to restrict motion at those junctions19,21,22,25 and, therefore, theoretically promotes fusion.
When bony cortex dorsal to the plate is held in contact under load, the plate becomes part of the load-bearing, cross-sectional area.14 Therefore, after plating, the operated segment will more effectively approximate the elastic modulus (Young modulus) of the plate, which is more than the elastic modulus of the graft alone.
Dryer et al.23 compared the effect of the strut graft alone, strut graft plus plate, and plate alone in an experimental C5 corpectomy model of the human cadaver. They reported that the most rigid construct was the plate construct with tricortical iliac crest strut graft. The least rigid construct was the ventral strut graft alone. This study also showed that the plate alone can provide more rigid fixation than graft alone after C5 corpectomy. They concluded that the ventral plate and bone graft construct acts as a reverse tension band, putting the dorsal elements under tension.23 The biomechanical effectiveness of plating after three-level corpectomy also has been shown by DiAngelo et al.,19 Foley et al.,20 and Kirkpatrick et al.22 According to Kirkpatrick et al.,22 the application of plates to the cervical spine as an adjunct to bone graft may improve the surgeon’s ability to stabilize the spine after multilevel corpectomy.
Immediate Stability
An optimal environment for fracture healing necessitates anatomic alignment, absolute immobilization, bone-to-bone contact, and compression of fracture segments. By means of a rigid internal fixation, immediate stability is improved without external bracing.14 On the other hand, while the stand-alone strut graft is loaded in flexion, it is unloaded in extension. The lack of plate leads to instability during each motion, particularly during flexion and extension.20
Improvement of the Rate of Fusion
The incidence of successful incorporation of a strut graft depends on the type of graft used. An iliac strut graft has a higher union rate than a fibular strut graft. The reported rates of union after single-level corpectomy are similar in cases fused with allograft or autologous graft. However, the rate of nonunion has been reported to range from 0% to 70% after multilevel corpectomy without plating. Nonunion rates tend to be especially high in cases undergoing fusion with allograft.3–5,8,16–18,25 Yonenobu et al.,17 using autograft, reported nonunion rates of 5% and 45% after one- and three-level corpectomies, respectively. Fernyhough et al.4 reported a total autograft nonunion rate of 27%, and a total allograft nonunion rate of 41% for ventral cervical fusion in cases with cervical spondylosis. In Fernyhough’s series, the rates of nonunion using autograft and allograft, respectively, were 25% and 18% after two-motion segment fusion, 22% and 43% after three-motion segment fusion, and as high as 41% and 70% after four-motion segment fusion. Using allograft, Zdeblick and Ducker18 reported 5% and 63% nonunion after one- and two-level fusion, respectively. The rate of successful fusion in most published series of patients fused with graft plus plate, however, is greater than 90%.1–3,8–13,14,16
Further support for the use of ventral cervical plating was reported by Lowery et al.9 In a series of 86 patients, Lowery reported 92% and 90% rates of fusion after autograft and allograft, respectively. They concluded that plating made allograft fusion rates comparable with those of autograft.9
Connolly et al.3 compared their results in ventral cervical fusions with and without ventral cervical plating. They reported that the overall graft complication rate (i.e., pseudarthrosis, delayed union, and graft collapse) was decreased with ventral cervical plate fixation. The rate of nonunion was significantly less in plated cases versus nonplated cases in the study of Yablon et al.16 as well. They reported nonunion in 9 of 60 cases undergoing fusion alone, whereas nonunion was seen in only 2 of 111 cases undergoing fusion plus plating. Furthermore, they reported complete relief of symptoms in 39% of the nonfixation group and in 63% of the fixation group.16
Acceleration of the Fusion Process
The rate of delayed union is higher in cases undergoing fusion alone. The use of plating can decrease the time of fusion. Caspar2 reported that fusion occurred, on average, in half or less of the time in instrumented cases, compared with nonplated fixation. The rate of delayed fusion has been reported to be as high as 75% in cases undergoing fusion alone.18
Prevention of Graft Migration and Collapse
The rate of graft collapse has been reported to be as high as 30%.18 Connolly et al.3 reported graft collapse in one of 18 cases operated without plating, and in none of 25 cases operated with plating. Yablon16 reported graft collapse in 8 of 60 cases operated without plating. Isaza et al.6 reported 100% fusion and no graft collapse after fusion and plating. The other serious complication following grafting without plating is graft migration. Graft intrusion and extrusion can be observed despite external immobilization. Yablon et al.16 reported graft migration in 7 of 60 cases (5 cases of extrusion and 2 cases of intrusion). They further reported 20% and 1% reoperation rates after grafting without and with plating, respectively.
Fernyhough J.C., White J.I., LaRocca H. Fusion rates in multilevel spondolysis comparing allograft fibula with autograft fibula in 126 patients. Spine (Phila Pa 1976). 1991;15(Suppl 10):S561-S564.
Isomi T., Panjabi M.M., Wang J.L., et al. Stabilizing potential of anterior cervical plates in multilevel corpectomies. Spine (Phila Pa 1976). 1999;24:2219-2223.
Naderi S., Alberstone C.D., Rupp F.W., et al. Cervical spondylotic myelopathy treated with corpectomy: technique and results in 44 patients. Neurosurg Focus. 1996;1(6):e5.
Wang J.C., Hart R.A., Emery S.E., Bohlman H.H. Graft migration or displacement after multilevel cervical corpectomy and strut grafting. Spine (Phila Pa 1976). 2003;28:1016-1021.
Yonenobu K., Fuji T., Ono K., et al. Choice of surgical treatment for multisegmental cervical spondylotic myelopathy. Spine (Phila Pa 1976). 1985;10:710-716.
1. Apfelbaum R.I. Ventral and upper cervical spine fixation techniques. In: Benzel E.C., editor. Spinal instrumentation: neurosurgical topics. Park Ridge, IL: American Association of Neurological Surgeons; 1994:63-96.
2. Caspar W. Anterior stabilization with trapezoid osteosynthetic plate technique in cervical spine injuries. In: Kehr P., Weidner A., editors. Cervical spine. vol I, New York: Springer-Verlag; 1987:198-202.
3. Connolly P.J., Esses S.I., Kostuik J.P. Anterior cervical fusion: outcome analysis of patients fused with and without anterior cervical plates. J Spinal Disord. 1996;9:202-206.
4. Fernyhough J.C., White J.I., LaRocca H. Fusion rates in multilevel spondolysis comparing allograft fibula with autograft fibula in 126 patients. Spine (Phila Pa 1976). 1991;15(Suppl 10):S561-S564.
5. Herkowitz H.N. Internal fixation for degenerative cervical spine disorders. Semin Spine Surg. 1995;7(1):57-60.
6. Isaza J., Munn B.G., Williams J.I., Whitecloud T.S. Instrumented anterior cervical fusion in the degenerative cervical spine. Presented at 12th annual meeting of Cervical Spine Research Society, European section. June 5-7, 1996.Nice, France
7. Jones J., Yoo J., Hart R. Delayed fracture of fibular strut allograft following multilevel anterior cervical spine corpectomy and fusion. Spine (Phila Pa 1976). 2006;31:E595-E599.
8. Law M.D., Bernhardt M., White A.A. Cervical spondylotic myelopathy: a review of surgical indications and decision making. Yale J Biol Med. 1993;66:165-177.
9. Lowery G.L., Reuter M.W., Sutterlin C.E. Anterior cervical interbody arthrodesis with plate stabilization for degenerative disc disease. Presented at 20th annual meeting for Cervical Spine Research Society. 1992. Palm Desert, CA
10. Naderi S., Alberstone C.D., Rupp F.W., et al. Cervical spondylotic myelopathy treated with corpectomy: technique and results in 44 patients. Neurosurg Focus. 1996;1(6):e5.
11. O’Shea J.F., Sundaresan N. Use of instrumentation in degenerative disease of the cervical spine. M Sinai J Med. 1994;61:248-256.
12. Sasso R.C., Ruggiero R.A.Jr, Reilly T.M., Hall P.V. Early reconstruction failures after multilevel cervical corpectomy. Spine (Phila Pa 1976). 2003;28:140-142.
13. Seifert V., Stolke D. Multisegmental cervical spondylosis: treatment by spondylectomy, microsurgical decompression, and osteosynthesis. Neurosurgery. 1991;29:498-503.
14. Tippets R.H., Apfelbaum R.I. Anterior cervical fusion with the Caspar instrumentation system. Neurosurgery. 1988;22:1008-1013.
15. Wang J.C., Hart R.A., Emery S.E., Bohlman H.H. Graft migration or displacement after multilevel cervical corpectomy and strut grafting. Spine. 2003;28:1016-1021.
16. Yablon I.G., Spatz E., Ordia J., et al. Cervical spine fusion with and without internal fixation. Presented at 23rd Annual Meeting of Cervical Spine Research Society. Nov 30-Dec 2, 1995. Santa Fe, NM
17. Yonenobu K., Fuji T., Ono K., et al. Choice of surgical treatment for multisegmental cervical spondylotic myelopathy. Spine (Phila Pa 1976). 1985;10:710-716.
18. Zdeblick T.A., Ducker T.B. The use of freeze-dried allograft bone for anterior cervical fusions. Spine (Phila Pa 1976). 1991;16:726-729.
19. DiAngelo D.J., Foley K.T., Vossel K.A., et al. Anterior cervical plating reverses load transfer through multilevel strut-grafts. Spine (Phila Pa 1976). 2000;25:783-795.
20. Foley K.T., DiAngelo D.J., Rampersaud R., et al. The in vitro effects of instrumentation on multilevel cervical strut-graft mechanics. Spine (Phila Pa 1976). 1999;24:2366-2376.
21. Isomi T., Panjabi M.M., Wang J.L., et al. Stabilizing potential of anterior cervical plates in multilevel corpectomies. Spine (Phila Pa 1976). 1999;24:2219-2223.
22. Kirkpatrick J.S., Levy J.A., Carillo J., Moeini S.R. Reconstruction after multilevel corpectomy in the cervical spine. A sagittal plane biomechanical study. Spine (Phila Pa 1976). 1999;24:1186-1191.
23. Dryer J., Nucci R., Gorup J., et al. Two-level cervical discectomy and fusion with anterior and posterior plating: a biomechanical study. Presented at 9th Annual Meeting of North American Spine Surgery. Oct 19-22, 1994. Minneapolis, MN
24. Smith S.A., Lindsey R.W., Doherty B.J., et al. An in-vitro biomechanical comparison of the orosco and AO locking plates for anterior cervical spine fixation. J Spinal Disord. 1995;8:220-223.
25. Smith G., Goldwhite N., White A., et al. Complications of anterior cervical fusion. Presented at 9th Annual Meeting of North American Spine Surgery. Oct 19-22, 1994. Minneapolis, MN