Chapter 24 Anterior Approaches to the Thoracic Spine and Thoracolumbar Junction
INTRODUCTION
The transthoracic approach to the mid-thoracic level is indicated in cases in which the anterior column is involved with the tumor mass. This approach enables surgeons to accomplish complete ventral decompression of the spinal cord and simultaneous anterior reconstruction.1 Depending on the intactness of the pleura, two kinds of approaches might be taken: transpleural and extrapleural. Patients should possess competent lung function to perform one-lung ventilation. If preoperative evaluation shows a pO2 <60; pCO2 >45; O2 saturation <90%; FVC <1.5 L; FEV1 <1 L; and FEV1/FVC <35%, then the transthoracic approach is contraindicated.2
TRANSTHORACIC APPROACH TO THE MID-THORACIC LEVEL
POSITIONING AND INCISION
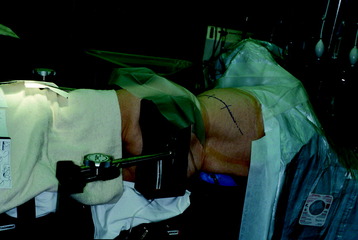
The operation is performed with the patient in a lateral decubitus position with an axillary roll under the dependent axilla (Fig. 24-1). The patient should be extended with the kidney rest and by tilting the operating table. The side of approach is decided based on the location of the pathology. When possible, a right-sided approach is preferred in the middle and upper thoracic spine because more working space is available over the spinal surface behind the azygos vein compared with that behind the aorta. The left side is preferred for the lower thoracic spine because at this level the liver causes the right diaphragm to rise and partially obstruct the working space. The skin incision starts from four finger breadths lateral to the spinous process, running along the selected rib, and reaches anteriorly to the costochondral junction.
MUSCLE DISSECTION
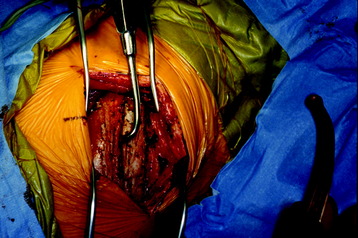
The latissimus dorsi muscle is then divided in a direction transverse to that of the fibers (Fig. 24-2). In the anterior region of the opening, the anterior serratus muscle is exposed. Posteriorly, the trapezius muscle can be exposed. When severing this muscle, the incision line should be as far caudal as possible to save the long thoracic nerve.
After the superficial muscle layer is divided, the second layer of muscles is exposed. According to the level of the lesion, the rhomboids (superiorly), serratus anterior (anterior), and serratus posterior inferior (posterior) can be severed (Fig. 24-3). In cases of the upper thoracic level, mobilization of the scapula is required.
RIB REMOVAL
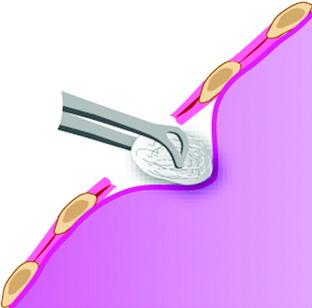
The outer periosteum of the selected rib is incised sharply and stripped with a periosteal elevator (Fig. 24-4). When preparing the outer and superior surfaces of the rib, a small dissector is used to free the inner periosteum from the underlying pleura. A Doyen elevator is introduced, elevating the inner periosteum anteriorly from the costal junction to the angle of the rib posteriorly (Fig. 24-5). A rib cutter is used to remove the rib. To gain additional exposure of the rib posteriorly, a longitudinal incision is made along the anterior border of the paraspinal muscles, allowing them to be retracted posteriorly past the rib angle.
EXPOSURE OF VERTEBRAL BODY (TRANSPLEURAL)
The thoracic cavity is opened in the bed of the resected rib. The spine is exposed by a longitudinal incision of the pleura 5 mm anterior to the rib heads.2 The lung is retracted anteriorly and the VB is exposed with the parietal pleura covered. Underneath the parietal pleura, the rib head is seen to be in contact with the intervertebral disc. On palpation, the intervertebral disc spaces are prominent, and the segmental vessels generally cross the middle portion of the body.
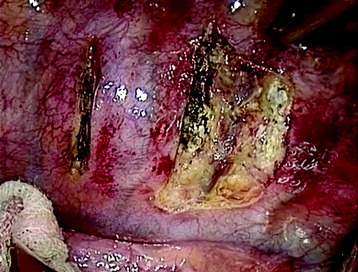
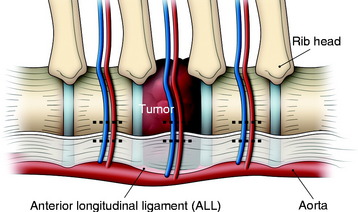
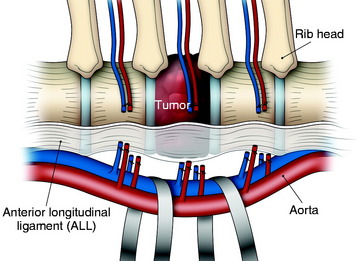
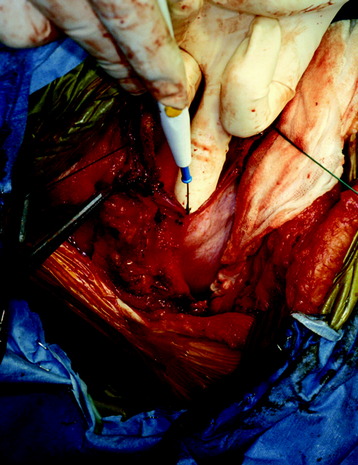
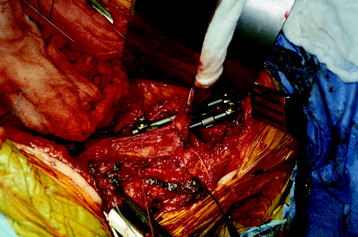
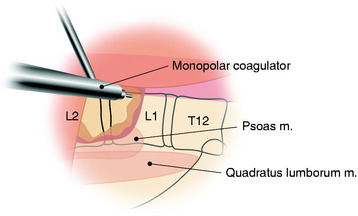
A transverse incision of parietal pleura is made along the rib head and disc space to expose segmental vessels. In cases of a T8 body lesion, dissection starts from adjacent levels (T7 and T9). The parietal pleurae overlying the segmental vessels are swept away with a monopolar coagulator (Fig. 24-6).
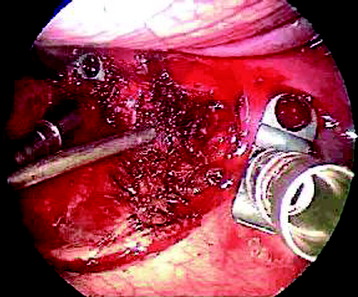
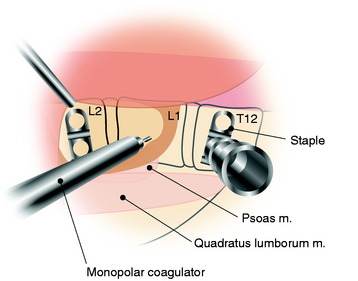
The segmental vessels are coagulated and divided (Fig. 24-7). The segmental vessels are dissected from the underlying VB with a right angle dissector. The hemoclips are applied to two sites, proximal and distal. The proximal side is controlled first, and later the distal side. After the hemoclips are applied to both sides, the vessel is cut and retracted. The sympathetic ganglion is removed to expose the rib head. For further exposure of the anterior portion of the VB, the great vessels should be dissected. The space between the anterior longitudinal ligaments (ALLs) and great vessels is easily created by blunt dissection after the segmental vessels are disconnected. The removal of the rib head is mandatory to gain exposure of the intervertebral foramen and posterior margin of the VB. The rib head is drilled away and the shell is removed with a curette. After rib head removal is completed, the costovertebral joint is exposed.
VERTEBRAL BODY RESECTION
After the parietal pleura is reflected and segmental vessels are controlled, the corpectomy begins. Adjacent disc removal is completed with an osteotome and pituitary forceps. The tumor-infiltrated VB is slightly soft and friable. The resection boundary is confined with an osteotome, and internal debulking is performed with pituitary forceps (Fig. 24-8). For exposure of the ventral surface of the spinal cord, the posterior cortical shell of the VB should be removed. When the posterior cortex is removed, great care should be taken not to injure the spinal cord.
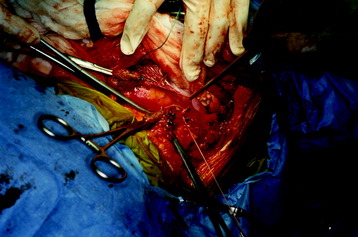
EXPOSURE OF THE VERTEBRAL BODY (EXTRAPLEURAL)
When a patient’s pulmonary function is not sustainable for one-lung ventilation, an extrapleural approach can be considered. Although this approach provides limited exposure compared with the transpleural approach, one advantage is that it can be performed with lung retraction without lung collapse. After rib removal, the endothoracic fascia is incised. The parietal pleura is kept intact. The dissection is performed between the endothoracic fascia and the parietal pleura (Fig. 24-9). This dissection provides the way to the VB (Fig. 24-10).
BILATERAL SEGMENTAL VESSEL LIGATION
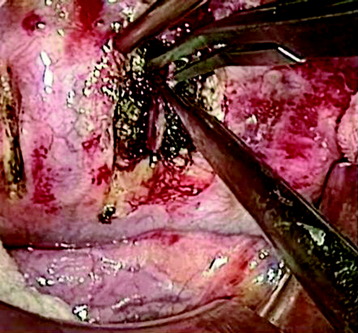
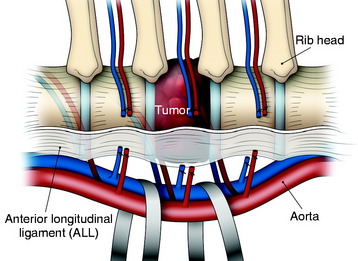
In the thoracic region, parietal pleural incisions are made on each VB level and corresponding rib head. After the dissection of the parietal pleura, the segmental vessels are seen on the midpoint of the VBs. First, the segmental vessels on the approach side are ligated (Fig. 24-11). Great care should be taken to dissect the vessel from the tumor-infiltrated cortical surface. After vessel ligation, the interface between the aorta and VB anterior surface is dissected. With traction applied to the proximal portion of the ligated segmental vessels, great vessels are moved to the anterior side to form potential space with reference to the ALL (Fig. 24-12).
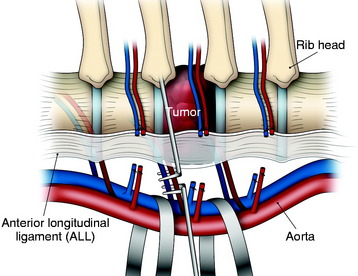
An adhesion may exist between the tumor-infiltrated VB and the great vessels. However, the dissection is relatively easy because the ALL blocks ventral expansion of the tumor mass. When the great vessels are moved forward, the segmental vessels on the contralateral side are seen to wind the lateral surface of the VBs. The exposed field is very deep. A surgical instrument such as the right angle dissector is applied to the contralateral segmental vessels, which are cut and tied (Figs. 24-13 and 24-14). Great care should be taken not to stretch these vessels. Neurological deficit after unilateral left-sided ligation of the T10–12 segmental vessels occurs in 0.75% of patients.3,4 There would appear to be virtually no risk to segmental vessel ligation provided the following: (1) vessel ligation is unilateral, (2) ligation is performed on the convexity of a scoliosis, (3) vessels are ligated at the mid-VB level, and (4) hypotensive anesthesia is avoided.
ANTERIOR APPROACH TO THORACOLUMBAR JUNCTION (TRANSPLEURAL-TRANSDIAPHRAGMATIC APPROACH WITH 10TH RIB RESECTION)
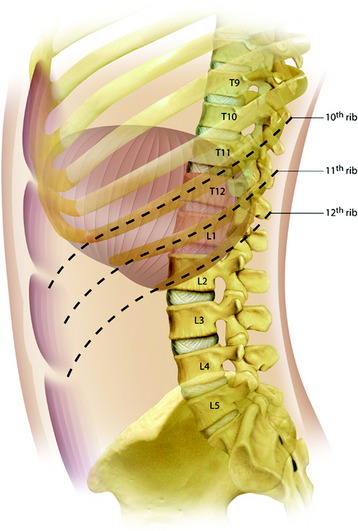
Exposure of the thoracolumbar junction can be approached through either side, but a left-sided approach is often selected. For the left-sided approach, the patient is placed in the true lateral decubitus position with a beanbag under the flank. For the exposure of T11–12, the resection of the ninth rib is usually best, and at T12–L1, a 10th rib thoracoabdominal approach is preferred. In this approach, long exposure of the thoracic and lumbar spine is possible from the T10 VB down to the L3 level. This approach involves detaching the diaphragm at its circumference.5,6
POSITIONING AND INCISION
The patient is placed in the lateral decubitus position. The skin incision begins posteriorly near the midline, follows the course of the 10th rib as far as the costal cartilage, and then continues obliquely downward on the upper abdomen, following the direction of the segmental nerves (Fig. 24-15). The procedures are performed to expose the thoracic cavity first, followed by exposure of the abdomen, and then the two parts are joined.
SOFT TISSUE DISSECTION
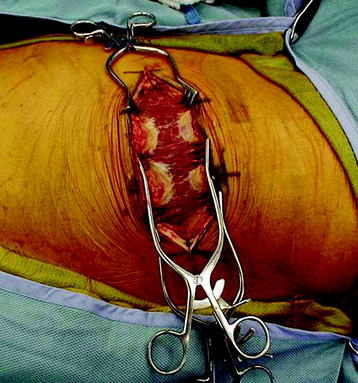
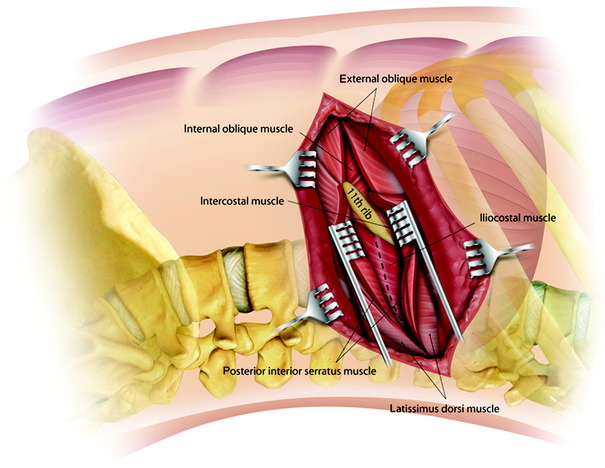
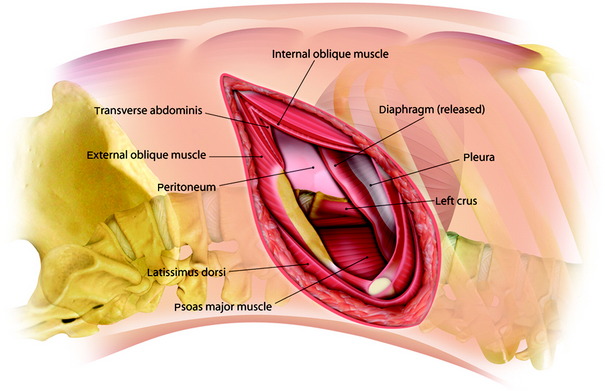
Using cautery, the incision is deepened down through the thoracic muscles, and the latissimus dorsi and serratus anterior muscles are transected posteriorly (Fig. 24-16). The deep abdominal muscle layers (internal oblique and transverse muscles of the abdomen) are bluntly split and retracted. This allows exposure of the upper lumbar spine retroperitoneally.
RIB REMOVAL
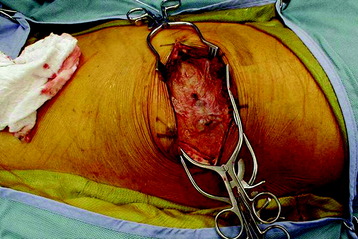
The rib is removed using a rib cutter from the angle of the rib posteriorly to the costal cartilage anteriorly (Fig. 24-17). The pleural cavity extends over the majority of the 11th rib and the medial portion of the 12th rib. The endothoracic fascia and the pleura are carefully stripped from the inner surface of the rib.
DIAPHRAGM INCISION
For exposure of the T12–L1 VB, diaphragmatic detachment is required.
Anatomically, the diaphragmatic muscle fibers originate from three locations: the sternal, costal, and lumbar parts. The lumbar part arises from both the right and left crura and from the medial and lateral arcuate ligaments. The sternal part originates from two muscular slips from the dorsum of the xiphoid process.7 The costal part arises from the inner surfaces of the costal cartilages and adjacent portions of the bone of the last six ribs on either side. The right crus begins from the sides of the L1–3 bodies and the left crus from the sides of the L1 and L2 bodies. The medial arcuate ligament covers the upper part of the psoas major muscle, attaching from the sides of the first and second lumbar vertebrae to the tip of the L1 and L2 transverse processes. The lateral arcuate ligament covers the quadratus lumborum and attaches from the tip of the L1 transverse process and laterally to the lower border of the 12th rib. Thus, both the crura and arcuate ligaments of the diaphragm are inserted below the T12–L1 disc space, so lesions located above the T12–L1 disc can be approached from above without dividing the diaphragm. Below the T12–L1 disc space, the spine is surrounded by the diaphragmatic crura, psoas muscles, and arcuate ligaments, so injuries here require diaphragmatic detachment for adequate exposure.
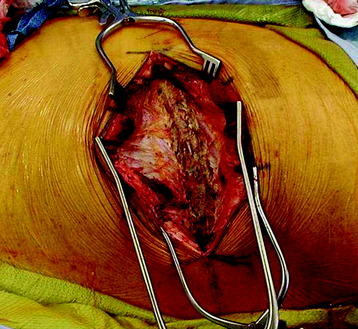
The diaphragmatic incision is made from inside the chest with clear visualization under the diaphragm in the retroperitoneal space (Fig. 24-18). The incision may be extended circumferentially 1 inch from its peripheral attachment to the chest wall. For an accurate reapproximation, marker clips should be used throughout the takedown of the diaphragm (Fig. 24-19).
EXPOSURE OF EACH VERTEBRAL BODY
After the longitudinal incision of the parietal pleura, the dissection is performed over the intervertebral disc space until the base of the transverse processes is reached. The sympathetic trunk is retracted laterally (Fig. 24-20). The origins of the psoas muscles are stripped from the VB. The intercostal arteries and veins are tied and ligated to allow for mobilization of the major vascular trunk (Fig. 24-21). The 12th intercostal vessels and first lumbar artery and vein may be covered by the muscular crus of the diaphragm.
CLOSURE
The diaphragm is reattached starting with approximation of the divided crus and a continuous suture or interrupted suture is done along the periphery of the divided diaphragm to the site of the division of the costal arch.6 (Figs. 24-22 and 24-23). If the instrument is left on the VB, the crus connection may be incomplete. The diaphragm repair is done over the implant applied to the VB. The divided costal cartilage serves as a good landmark for closure and should be reapproximated with two 0 or 1 braided polyester sutures, used in a figure 8 pattern. Then, closure of the diaphragm is completed by additional stitches.
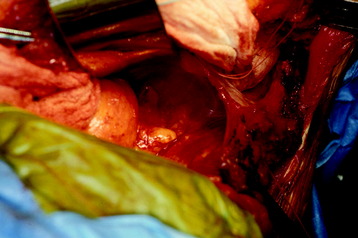
CASE ILLUSTRATION
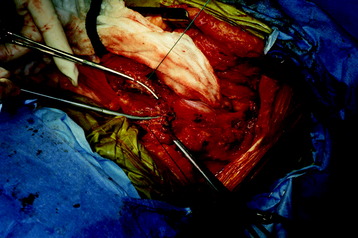
A 53-year-old patient was diagnosed with breast cancer with L1 metastasis. Preoperative magnetic resonance imaging (MRI) showed an L1 VB collapse with severe dural sac compression (Fig. 24-24). Surgical treatment was done with a left-sided transpleural-transdiaphragmatic approach. The diaphragm was detached, and an L1 corpectomy and dural sac decompression were completed. Then a titanium mesh graft was inserted, and an anterior screw-rod system was used for anterior stabilization (Fig. 24-25).
TRANSPLEURAL-RETROPERITONEAL APPROACH (DIAPHRAGM-DETACH) TO THE THORACOLUMBAR JUNCTION
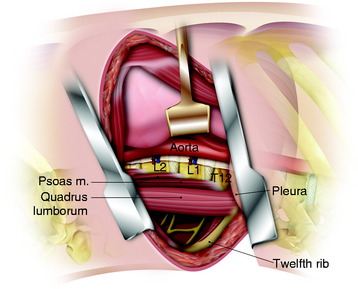
IDENTIFICATION OF THE INSERTION POINT OF THE CRUS
The skin incision and rib removal procedure are the same as for the transdiaphragmatic approach.
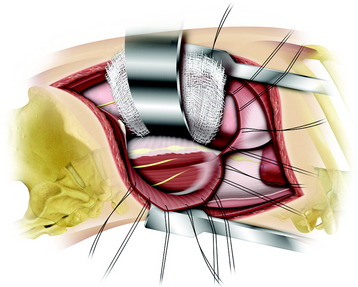
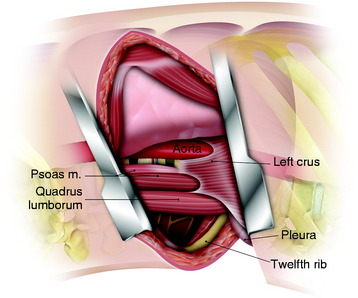
The pleural cavity is entered through the rib bed. The lung is retracted cranially.
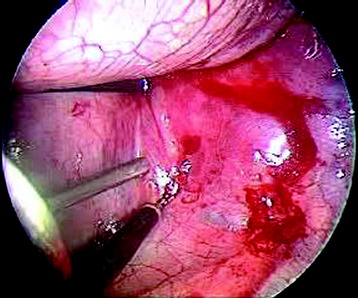
After a thoracotomy, the diaphragm is identified and gradually retracted caudally to expose the crus of the diaphragm. The key is to enter the pleural cavity and then identify the posterior insertion and crus of the diaphragm. The retractor holds down the diaphragm and exposes the insertion of the diaphragm on the spine (Figs. 24-26 and 24-27). Both the crural muscle and the arcuate ligament of the diaphragm are inserted below the T12–L1 disc space. With a blunt probe, the anterior aspect of the spine along with its diaphragmatic insertion and course of the aorta are identified.
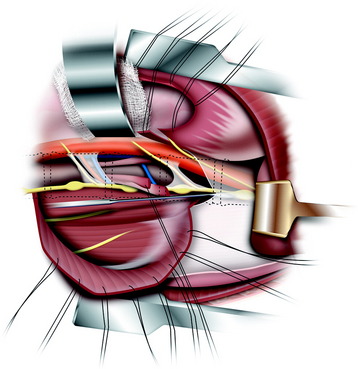
INCISION OF THE DIAPHRAGM INSERTION
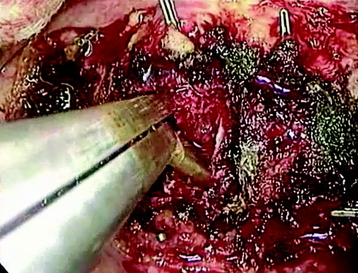
The line of incision for diaphragmatic detachment is identified and marked with monopolar cautery. A semicircular incision is preferred to radial incision because the latter is commonly associated with increased risk of diaphragmatic hernia (Figs. 24-28 and 24-29).
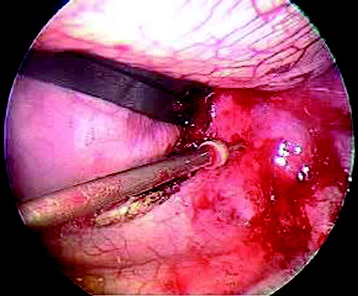
The incision for the diaphragm should run along the VB and the ribs, parallel to the diaphragmatic insertion and 1–2 cm away from it.8,9 With a diaphragmatic opening of about 6–10 cm, the L2 VB can be exposed. A rim of 1 cm is left on the spine to facilitate closure of the diaphragm at the end of the procedure. After the diaphragm is split, the retractors are applied into the diaphragmatic opening. The retroperitoneal fat tissue is then exposed and mobilized in an anterior-to-posterior direction along the anterior surface of the psoas muscle. The fat tissue should be separated from the peritoneum to create a plane leading down to the anterior aspect of the psoas and VBs.
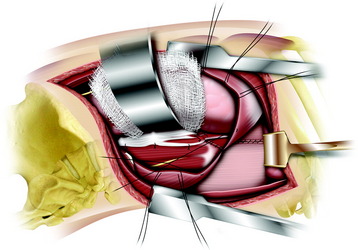
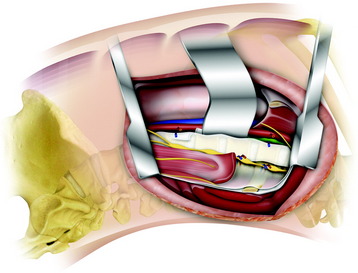
PSOAS MUSCLE DISSECTION
The psoas muscle with its tendinous insertions is dissected very carefully from the VBs to prevent damaging the segmental blood vessels hidden underneath. The segmental vessels are then identified over the center of the VB, ligated using a hemoclip or suture tie, and then divided. Compared with extensive thoracolumbar exposure with total dissection of the diaphragm in the transdiaphragmatic approach, this approach requires only minimal detachment of the diaphragm and holds the detached diaphragm down7 (Figs. 24-30 and 24-31).
EXTRAPLEURAL-RETROPERITONEAL APPROACH TO THORACOLUMBAR JUNCTION WITH 11TH RIB RESECTION
The extrapleural approach is indicated if only one or two spinal segments at the thoracolumbar junction need to be accessed.10
POSITIONING AND INCISION
The position is similar in the 10th rib approach. The skin incision line runs over the 11th rib course and curves downward at the costal cartilage to the edge of the rectus sheath at the level of the umbilicus (see Fig. 24-15).
MUSCLE INCISION AND RIB REMOVAL
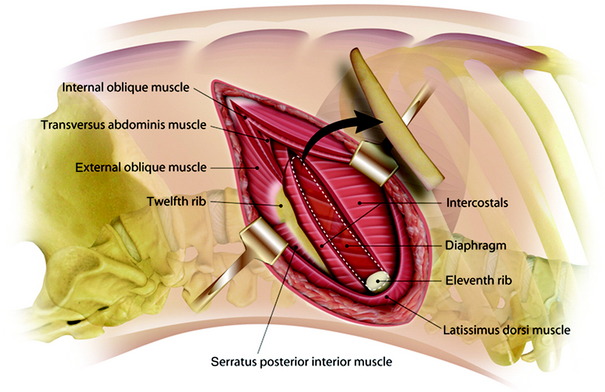
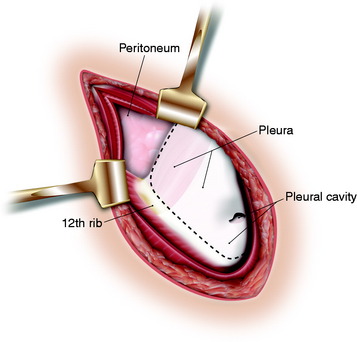
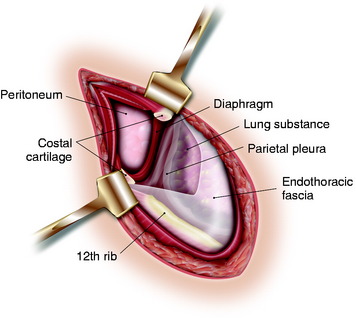
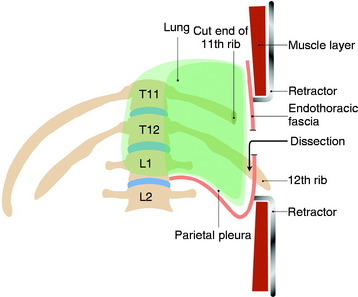
Under the rib, the endothoracic fascia layer is dissected. The anterior two-thirds of the 11th rib is removed. The pleura and the pleural cavity are under the rib bed. The rib bed has three layers: periosteum, endothoracic fascia, and parietal pleura (Fig. 24-32). The pleural cavity extends over the majority of the 11th rib and the medial portion of the 12th rib.
COSTAL CARTILAGE SPLITTING
When the extrapleural and retroperitoneal spaces are to be communicated, the costal cartilage should be split (Fig. 24-33). The insertion of the diaphragm is into the cephalad edge of costal cartilage and adjacent rib bed; the insertion of the transverses abdominis muscle and transversalis fascia is made into the caudad portion (Fig. 24-34).
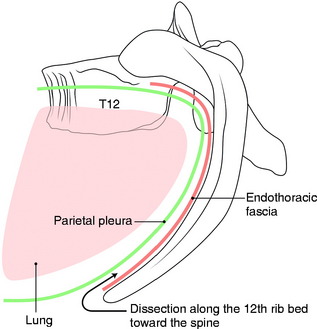
EXTRAPLEURAL SPACE DISSECTION
Careful dissection should be performed under the rib bed to create extrapleural space. The endothoracic fascia is first incised, and then the parietal pleura is seen (Fig. 24-35). Blunt dissection with a cotton ball is performed between the endothoracic fascia and the parietal pleura. The dissection is begun under the proximal end of the exposed segment of the 12th rib and then continued down to the costal cartilage and toward the VB (Figs. 24-36 to 24-38). Endothoracic fascia is firmly adhered to the bony structures.11 Gentle dissection can easily reveal the extrapleural space. If the pleural membrane is torn, an immediate suture should be placed.
DIAPHRAGM RELEASE FROM THE INSERTION TO THE 12TH RIB
The parietal pleura is mobilized from the superior aspect of the left diaphragm and posteriorly from under the surface of the 10th and 12th ribs and the 11th rib stump. Posteriorly a 4- to 5-cm margin of diaphragm along the rib cage is now exposed. The diaphragm is attached to the tip of the 12th rib. When the pleura is sufficiently pushed away from the rib, the insertion point of the diaphragm to the 12th rib is cut off (Fig. 24-39). The diaphragm is then released from the insertion site to the rib. This maneuver makes it easier to retract the diaphragm to the cephalad direction (Fig. 24-40).
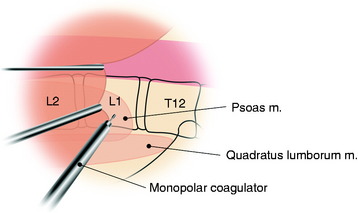
VERTEBRAL BODY EXPOSURE
For T12–L1 exposure, the approach can be possible from under the diaphragm. After the diaphragm is released from the tip of the 12th rib, the next tethered site is the L1 transverse process (Fig. 24-41). At the L1 transverse process, the medial and lateral lumbocostal arches of the diaphragm meet.12 This attachment is cut. The next anchored point of the diaphragm is on the left side of the L1–2 VBs, where the left crus is attached. The crus is divided and elevated from the VBs, leaving a portion for reattachment at closure. When the crus is detached, the diaphragm is fully freed from the bony structures. With the diaphragm retracted cephalad, the psoas muscle and quadratus lumborum muscle are shown on their proximal origin. The psoas muscle originates from the lateral surface of the T12–L1 VB. The quadratus lumborum muscle is attached to the proximal end of the 12th rib.13 The psoas muscle is peeled off the origin portion of the VB and taken down to expose the L1–2 VB and pedicles (Fig. 24-42).
This approach is taken from under the diaphragm. The upper limit of the exposure is usually the T10–11 disc space. Additional rostral exposure is limited because of the overhang of the rib cage. The lower lumbar exposure can be varied by making the initial incision more oblique below the umbilicus or by making more of a paramedian incision.14
WIDENING OF VERTEBRAL BODY EXPOSURE
For extensive exposure of the lower thoracic spine, the diaphragm should be transected (Fig. 24-43). When the pleura and the peritoneum have been freed, the diaphragm is transected above the medial arcuate ligament in such a way as to permit re-suture later.
The medial arcuate ligament—the diaphragm attachment to L1 transverse process—should be left intact.