Chapter 20 Anterior Approaches to the Cervicothoracic Junction
TRANSCLAVICULAR–TRANSMANUBRIAL APPROACH
Radiological studies of the upper thoracic spine have indicated that at least the T3 vertebra can be visualized in the majority of patients in whom a suprasternal approach is undertaken after the splitting and mobilization of the manubrium.1
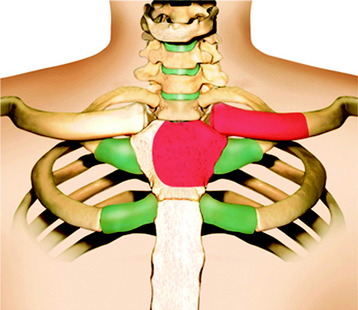
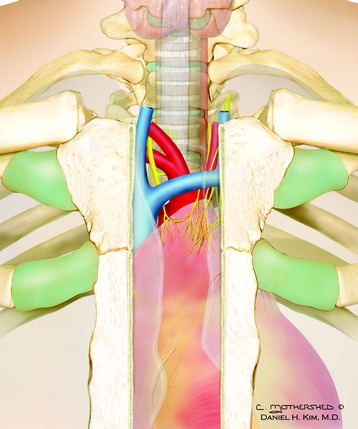
The external landmarks for level identification are T2–3 at the suprasternal notch and T4–5 at the sternal angle (Fig. 20-1). Before adopting this approach, it is important preoperatively to confirm the extent of the lesion and the position of the upper margin of the sternum on lateral radiographs. It also is essential to assess the affected spinal cord level and its relation to the level of the upper margin of the sternal manubrium because this relationship varies among individuals.
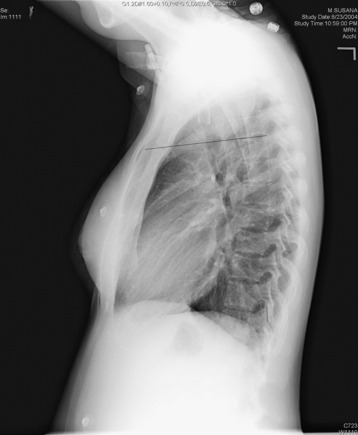
Fig. 20-1 In this patient, the sternomanubrial junction corresponds to the T2–3 intervertebral disc level.
BONE REMOVAL
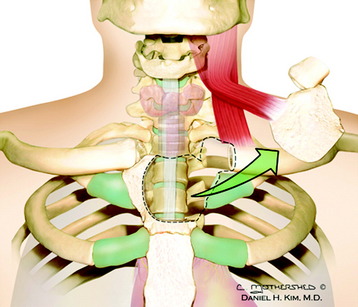
The medial third of the clavicle and manubrium is dissected periosteally. The clavicle is divided at the junction of the medial and middle thirds (Fig. 20-2). All procedures are safe when the periosteum is separated from the bone by using a raspatory. While excising the sternum, the sternum lining is carefully separated using the raspatory to avoid possible damage to the internal mammary artery (Fig. 20-3).2
The left side of the manubrium can be removed piecemeal along its posterior periosteum.
Alternatively, the manubrium and sternoclavicular joint can be left intact and reflected with the sternal head of the sternocleidomastoid muscle (Fig. 20-4).
VASCULAR DISSECTION
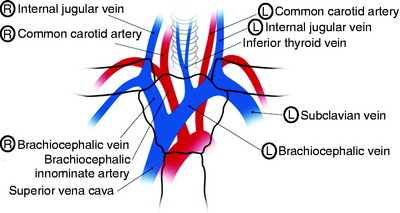
Dissection is carried deeper until the great vessels are identified. Inferior thyroid vessels can be ligated. If the cranial part, approximately 50% of the sternal manubrium, is removed, the surgeons do not need to retract the left innominate vein. A bilateral retraction of the brachiocephalic trunk can expose the T1 and T2 vertebral body (Fig. 20-5).
TRANS-STERNAL–TRANSTHORACIC APPROACH
SKIN INCISION AND CERVICAL DISSECTION
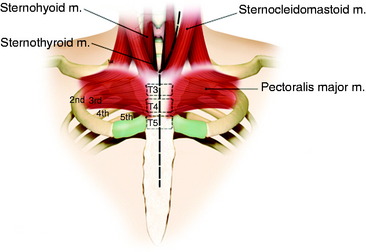
The supine position is set with the neck hyperextended. A linear vertical incision starts from the mid-cervical spine along the anterior border of the sternocleidomastoid muscle and continues through the middle of the sternum down to the tip of the xiphoid process (Fig. 20-6).
The sternohyoid muscle originates from the ventrocaudal hyoid bone to the dorsal surface of the manubrium and attaches to the sternoclavicular joint capsule. The sternothyroid muscle attaches along the dorsal midline of the manubrium (Fig. 20-7). The sternocleidomastoid muscle arises on the mastoid process and superior nuchal line and attaches to the manubrioclavicular joint. The nervous supply of these three muscles is from the accessory nerve. Their arterial supply branches from the superior thyroid artery.
STERNOTOMY
The sternum is exposed subperiosteally and divided in the middle with a sternal saw. After the sternotomy, visceral fascia is seen to circumscribe the trachea and esophagus (Fig. 20-8). The visceral fascia continues down to the bronchi, where the fascia fuses with the parietal and visceral pleurae.
VASCULAR DISSECTION
In the superior mediastinum, the vascular compartment is not circumscribed by its own well-defined fascial sheath but is defined secondarily by independent surrounding fasciae: ventrally by the prevertebral fascial extension (the transthoracic fascia), caudally by the visceral fascia, laterally by the parietal pleura, and inferiorly by the pericardium.3
Inferior thyroid vessels can be ligated. For the exposure of prevertebral fascia, the esophagus, trachea, and brachiocephalic trunk are retracted gently to the right side, while the thoracic duct, the cupola of the pleura, and left common carotid artery are retracted to the left side and the left innominate vein is retracted caudally (or ligated if necessary) (Fig. 20-9). If the vertebral body mass protrudes to the ventral side, the bilateral carotid artery is displaced laterally and the mass is found to be between the common carotid arteries (Fig. 20-10).
Venous structures lie on the arterial structures. The right brachiocephalic vein is formed just posterior to the medial end of the right clavicle and descends vertically into the superior mediastinum. The left brachiocephalic vein is formed just posterior to the medial end of the left clavicle and descends diagonally to join the right brachiocephalic vein just posterior to the right first costal cartilage to form the superior vena cava. In the superior mediastinum, the left brachiocephalic vein runs obliquely from left inferior to right superior (see Fig. 20-5). Internal thoracic, thymic, and inferior thyroid veins in the superior mediastinum drain into the brachiocephalic vein. On the left, the superior intercostal vein, which drains the second and third intercostal spaces, also drains into the left brachiocephalic vein. The aortic arch initially ascends posteriorly to the superior vena cava but also turns diagonally posterior, then inferior just anterior and to the left of the vertebral column. A second concave turn occurs as the arch curves around the anterolateral visceral compartment to reach the vertebral column.
The brachiocephalic artery is the first branch off the aortic arch and ascends vertically and slightly rightward to branch into the right common carotid and subclavian arteries posterior to the right sternoclavicular joint. The left common carotid artery arises next off the arch and ascends essentially vertically into the carotid sheath without branching in the superior mediastinum (Fig. 20-11).
The left subclavian artery is the third branch and ascends superiorly and leftward to curve around the thoracic inlet and into the axillary sheath without branches in the superior mediastinum (see Fig. 20-11). From the right brachiocephalic innominate artery, the right subclavian artery originates just from the medial side of the right claviculo-manubrial joint and runs under the clavicle (Fig. 20-12).

Fig. 20-12 Sagittal section showing the right brachiocephalic innominate artery and right subclavian artery.
The prevertebral fascia is identified and incised to expose the vertebral bodies (Fig. 20-13). Autonomic branches to the cardiopulmonary plexuses may be seen in this region and can be sacrificed if necessary. The left recurrent laryngeal nerve loops around the ligamentum arteriosum and ascends within the visceral fascia between the esophagus and trachea. Closure should be performed with standard wiring. A chest tube is not necessary unless there is pleural violation.
CASE ILLUSTRATION
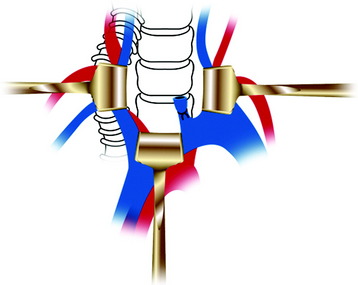
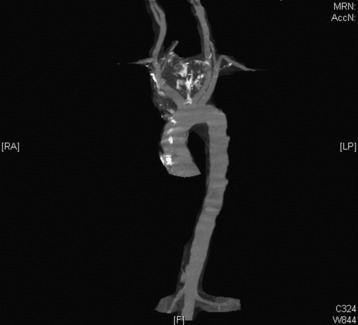
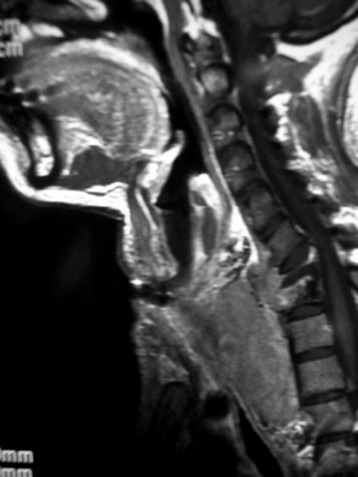
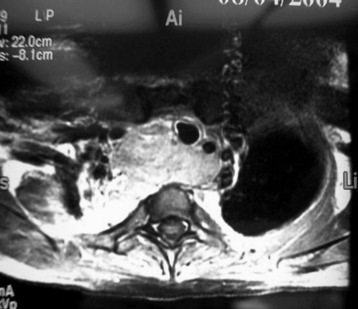
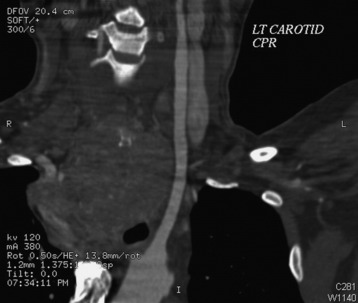
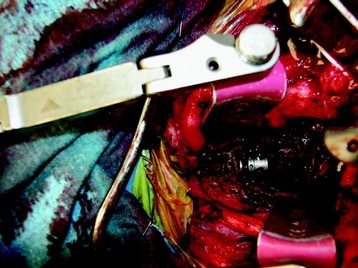
Preoperative evaluation included simple radiography, magnetic resonance imaging (MRI), and computed tomography (CT) angiography. On x-ray, the vertebral body destruction was found at the C7–T1 levels. On MRI, the destructive lesion from the C7–T1 body grew into the superior mediastinal space and showed downward extension along the anterior surface of the upper thoracic spine (Fig. 20-14). On axial view, the mass displaced all the visceral and vascular structures (Fig. 20-15). Angiography was necessary because the vascular encasement should be excluded. The right side brachiocephalic innominate artery was displaced to the anterior side (Fig. 20-16). The left side brachiocephalic trunk was displaced to the left side (Fig. 20-17). The patency of the vessels was maintained and tumor-vessel interface seemed to be intact.
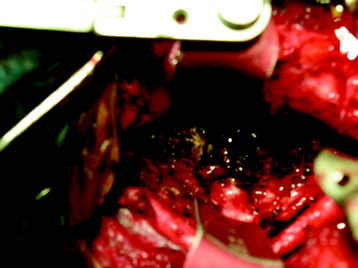
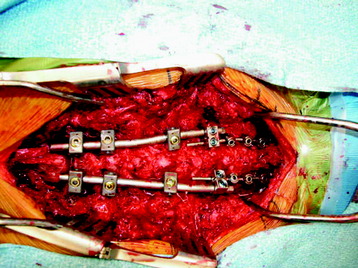
After the sternotomy opening, vascular structures were seen. The right brachiocephalic innominate artery was running underneath the left brachiocephalic vein (Fig. 20-18). With the caudal retraction of the left brachiocephalic vein, the T4 vertebral body could be reached. The right brachiocephalic artery and left common carotid artery were retracted bilaterally. A superior mediastinal mass was removed with forceps and a monopolar dissector. The superior mediastinal mass was removed piecemeal. The ventral body surface was exposed from the C6 to T4 vertebral body. Corpectomy was performed for the C7 and T1 vertebral body, and a vertebral body replacement (VBR) cage was inserted (Fig. 20-19). An anterior cervical plate was applied from C6 to T2. After the screw angle was adjusted with the consideration of the disc plane inclination, then posterior stabilization was performed with cervical lateral mass screws and thoracic pedicle screws (Fig. 20-20). Postoperative chest x-ray should be taken to ensure that pneumothorax does not develop (Fig. 20-21).