Ankle and Foot
Terminology Used to Describe Movements
Structure and Function of the Joints Associated with the Ankle
Structure and Function of the Joints Associated with the Foot
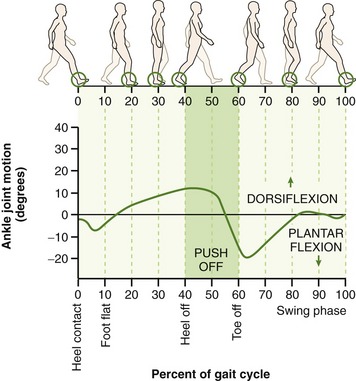
This chapter sets forth a firm basis for an understanding of the evaluation and treatment of several disorders that affect the ankle and foot, many of which are kinesiologically related to the movement of the entire lower extremity. Several of the kinesiologic issues addressed in this chapter are related specifically to the process of walking, or gait, a topic covered in detail in Chapter 15. Figure 15-12 should be consulted as a reference to the terminology used throughout Chapter 14 to describe the different phases of the gait cycle.
OSTEOLOGY
NAMING THE JOINTS AND REGIONS
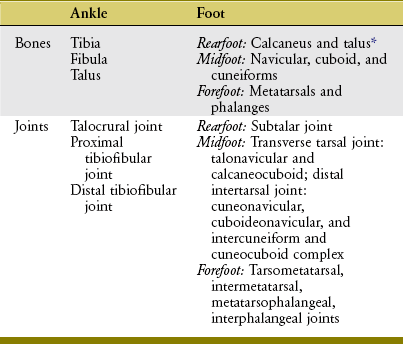
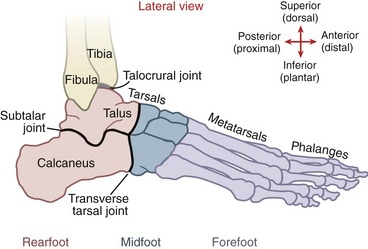
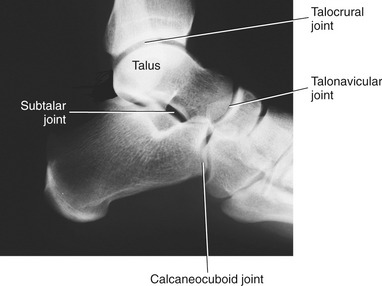
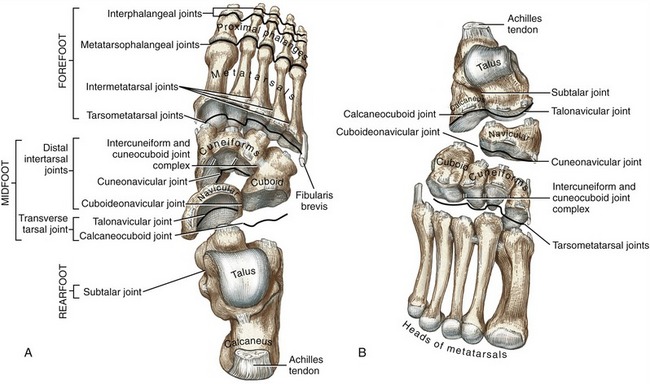
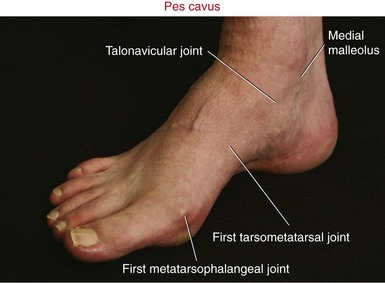
Figure 14-1 depicts an overview of the terminology that describes the regions of the ankle and foot. The term ankle refers primarily to the talocrural joint: the articulation among the tibia, fibula, and talus. The term foot refers to all the tarsal bones, and the joints distal to the ankle. Within the foot are three regions, each consisting of a set of bones and one or more joints. The rearfoot (hindfoot) consists of the talus, calcaneus, and subtalar joint; the midfoot consists of the remaining tarsal bones, including the transverse tarsal joint and the smaller distal intertarsal joints; and the forefoot consists of the metatarsals and phalanges, including all joints distal to and including the tarsometatarsal joints. Table 14-1 provides a summary of the organization of the bones and joints of the ankle and foot.
OSTEOLOGIC SIMILARITIES BETWEEN THE DISTAL LEG AND THE DISTAL ARM
As described in Chapter 12, the entire lower extremity progressively internally or medially rotates during embryologic development. As a result, the great toe is positioned on the medial side of the foot, and the top of the foot is actually its dorsal surface. This orientation is similar to that of the hand when the forearm is fully pronated (Figure 14-2). This plantigrade position of the foot is necessary for walking and standing. With the forearm pronated, flexion and extension of the wrist are similar to plantar flexion and dorsiflexion of the ankle, respectively.
Individual Bones
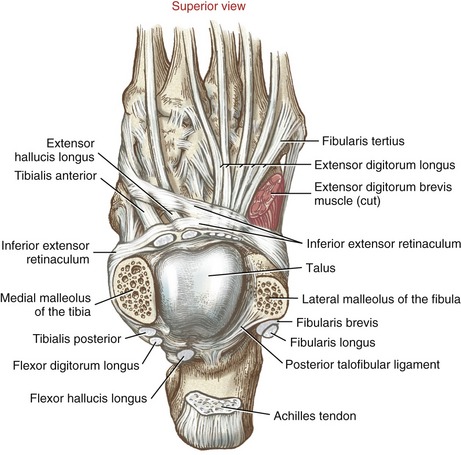
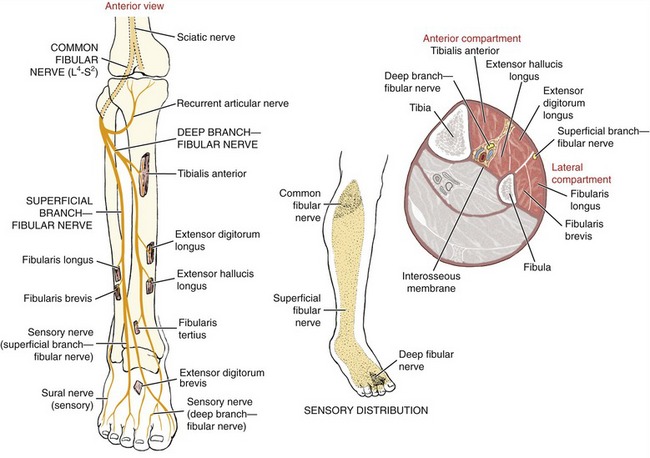
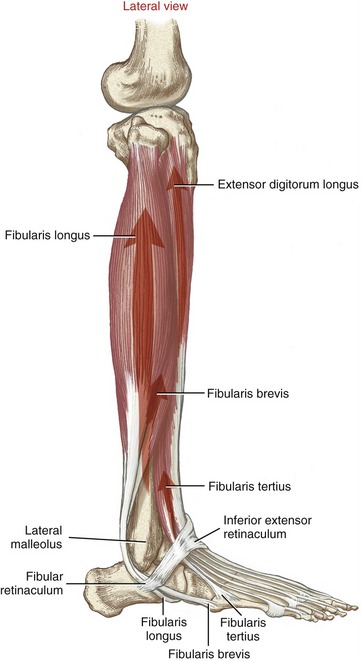
The long and thin fibula is located lateral and parallel to the tibia (Figure 13-3). The fibular head can be palpated just lateral to the lateral condyle of the tibia. The slender shaft of the fibula transfers only about 10% of body weight through the leg; most of the weight is transferred through the thicker tibia. The shaft of the fibula continues distally to form the sharp and easily palpable lateral malleolus (from the Latin root malleus, hammer). The lateral malleolus functions as a pulley for the tendons of the fibularis (peroneus) longus and brevis. On the medial surface of the lateral malleolus is the articular facet for the talus (see ahead Figure 14-11). In the articulated ankle, this facet forms part of the talocrural joint (Figure 14-3).
DISTAL TIBIA
The distal end of the tibia expands to accommodate loads transferred across the ankle. On its medial side is the prominent medial malleolus. On the lateral surface of the medial malleolus is the articular facet for the talus (see ahead Figure 14-11). In the articulated ankle, this facet forms a small part of the talocrural joint. On the lateral side of the distal tibia is the fibular notch, a triangular concavity that accepts the distal end of the fibula at the distal tibiofibular joint (see ahead Figure 14-11).
In the adult the distal end of the tibia is twisted externally around its long axis approximately 20 or 30 degrees relative to its proximal end.141 This natural torsion is evidenced by the slight externally rotated position of the foot during standing. This twist of the lower leg is referred to as lateral tibial torsion, based on the orientation of the bone’s distal end relative to its proximal end.
TARSAL BONES
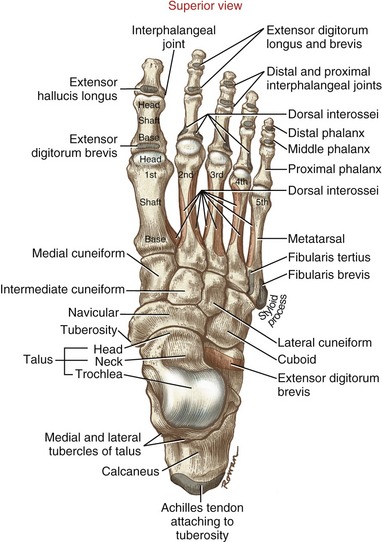
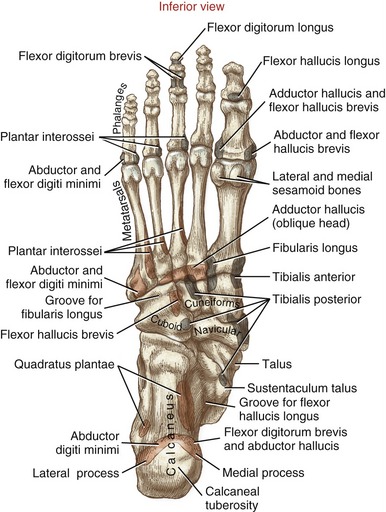
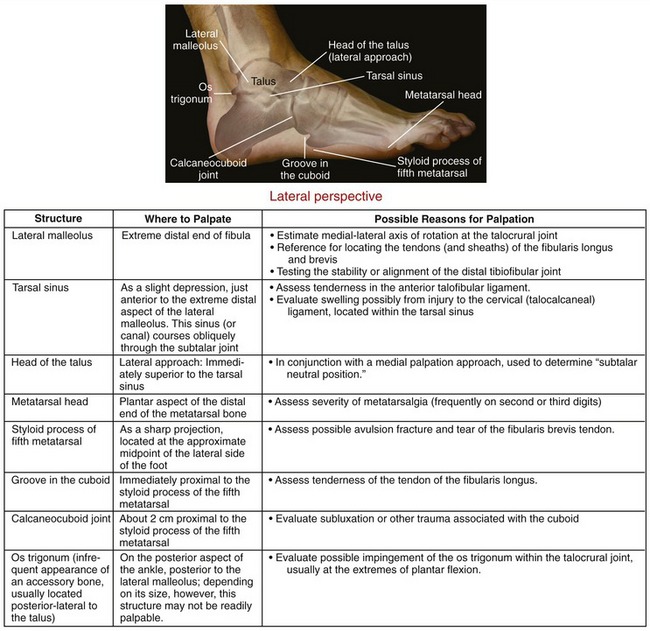
The seven tarsal bones are shown in four different perspectives in Figures 14-4 through 14-7.
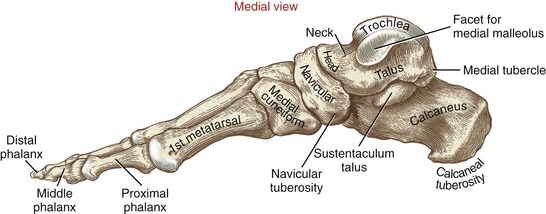
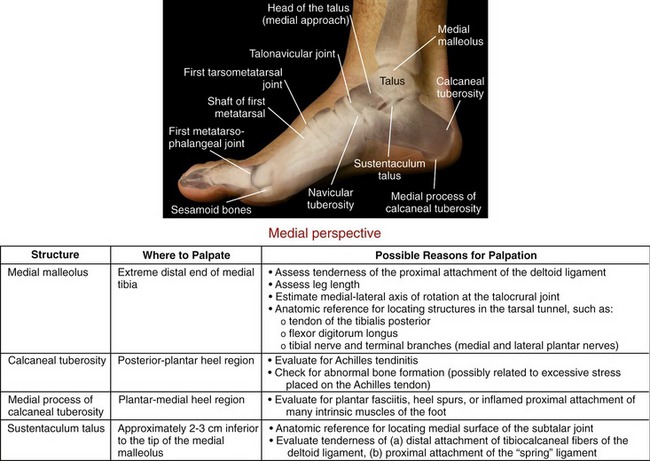
FIGURE 14-6. A medial view of the bones of the right foot.
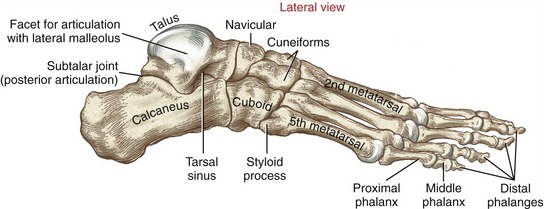
FIGURE 14-7. A lateral view of the bones of the right foot.
Talus: The talus is the most superiorly located bone of the foot. Its dorsal or trochlear surface is a rounded dome: convex anterior-posteriorly and slightly concave medial-laterally (see Figures 14-4 and 14-6). Cartilage covers the trochlear surface and its adjacent sides, providing smooth articular surfaces for the talocrural joint.120 The prominent head of the talus projects forward and slightly medially toward the navicular. In the adult the long axis of the neck of the talus positions the head of this bone about 30 degrees medial to the sagittal plane. In small children the head is projected medially about 40 to 50 degrees, partially accounting for the often inverted appearance of their feet.
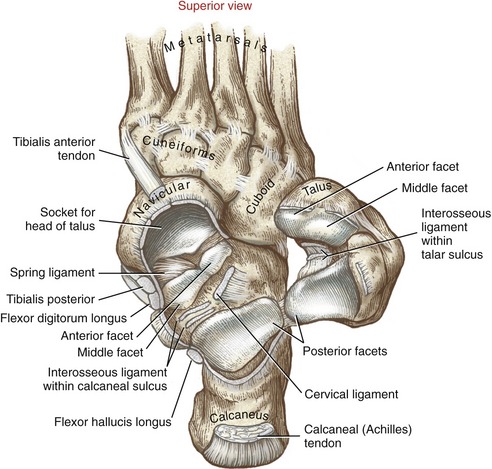
Figure 14-8 shows three articular facets on the plantar (inferior) surface of the talus. The anterior and middle facets are slightly curved and often continuous with each other. The articular cartilage that covers these facets also covers part of the adjacent head of the talus. The oval, concave posterior facet is the largest facet. As a functional set, the three facets articulate with the three facets on the dorsal (superior) surface of the calcaneus, forming the subtalar joint. The talar sulcus is an obliquely running groove between the anterior-middle and posterior facets.
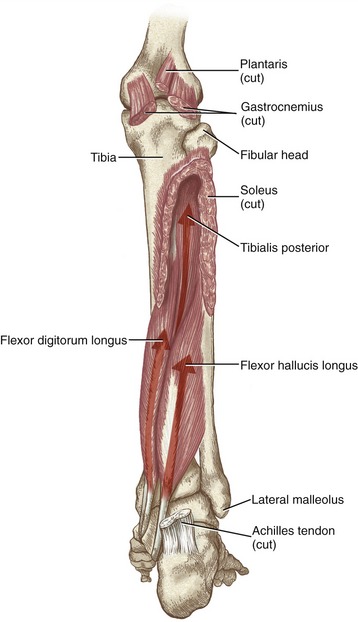
Lateral and medial tubercles are located on the posterior-medial surface of the talus (see Figure 14-4). A groove formed between these tubercles serves as a pulley for the tendon of the flexor hallucis longus (see ahead Figure 14-12).
Calcaneus: The calcaneus, the largest of the tarsal bones, is well suited to accept the impact of the heel striking the ground during walking. The large and rough calcaneal tuberosity receives the attachment of the Achilles tendon. The plantar surface of the tuberosity has lateral and medial processes that serve as attachments for many of the intrinsic muscles and the deep plantar fascia of the foot (see Figure 14-5).
The calcaneus articulates with other tarsal bones on its anterior and dorsal surfaces. The relatively small, curved anterior surface of the calcaneus joins the cuboid at the calcaneocuboid joint (see Figure 14-7). The more extensive dorsal surface contains three facets that join the matching facets on the talus (see Figure 14-8). The anterior and middle facets are relatively small and nearly flat. The posterior facet is large and convex, conforming to the concave shape of the equally large posterior facet on the talus. Between the posterior and medial facets is a wide oblique groove called the calcaneal sulcus. Located within this sulcus are the attachments of several strong ligaments that bind the subtalar joint. With the subtalar joint articulated, the sulci of the calcaneus and talus form a canal within the subtalar joint, known as the tarsal sinus (see Figure 14-7).
The sustentaculum talus projects medially as a horizontal shelf from the dorsal surface of the calcaneus (see Figure 14-6). The sustentaculum talus lies under and supports the middle facet of the talus. (Sustentaculum talus literally means a “shelf for the talus.”)
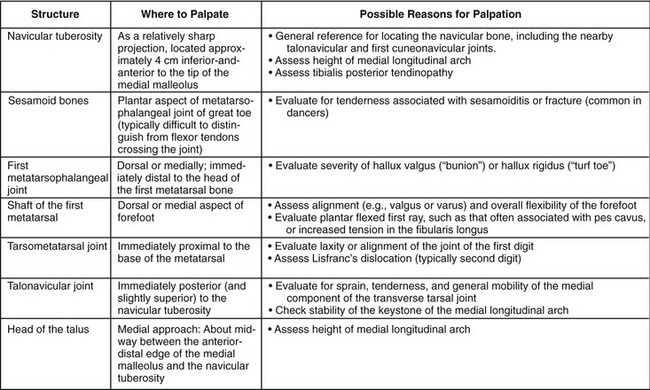
Navicular: The navicular is named for its resemblance to a ship (i.e., referring to “navy”). Its proximal (concave) surface accepts the head of the talus at the talonavicular joint (see Figure 14-4). The distal surface of the navicular bone contains three relatively flat facets that articulate with the three cuneiform bones.
The medial surface of the navicular has a prominent tuberosity, palpable in the adult at about 2.5 cm inferior and distal (anterior) to the tip of the medial malleolus (see Figure 14-6). This tuberosity serves as one of several distal attachments of the tibialis posterior muscle.
Medial, Intermediate, and Lateral Cuneiforms: The cuneiform bones (from the Latin root meaning “wedge”) act as a spacer between the navicular and bases of the three medial metatarsal bones (see Figure 14-4). The cuneiforms contribute to the transverse arch of the foot, accounting, in part, for the transverse convexity of the dorsal aspect of the midfoot.
Cuboid: As its name indicates, the cuboid has six surfaces, three of which articulate with adjacent tarsal bones (see Figures 14-4, 14-5, and 14-7). The distal surface articulates with the bases of both the fourth and fifth metatarsals. The cuboid is therefore homologous to the hamate bone in the wrist.
The entire, curved proximal surface of the cuboid articulates with the calcaneus (see Figure 14-4). The medial surface has an oval facet for articulation with the lateral cuneiform and a small facet for articulation with the navicular. A distinct groove runs across the plantar surface of the cuboid, which in life is occupied by the tendon of the fibularis longus muscle (see Figure 14-5).
RAYS OF THE FOOT
A ray of the forefoot is functionally defined as one metatarsal and its associated set of phalanges.
Metatarsals: The five metatarsal bones link the distal row of tarsal bones with the proximal phalanges (see Figure 14-4). Metatarsals are numbered 1 through 5, starting on the medial side. The first metatarsal is the shortest and thickest, and the second is usually the longest. The second and usually the third metatarsals are the most rigidly attached to the distal row of tarsal bones. These morphologic characteristics generally reflect the larger forces that pass through this region of the forefoot during the push off phase of gait. Each metatarsal has a base at its proximal end, a shaft, and a convex head at its distal end (see Figure 14-4, first metatarsal). The bases of the metatarsals have small articular facets that mark the site of articulation with the bases of the adjacent metatarsals.
Longitudinally, the shafts of the metatarsals are slightly concave on their plantar side (see Figure 14-6). This arched shape enhances the load-supporting ability of the metatarsals, and provides space for muscles and tendons. The plantar surface of the first metatarsal head has two small facets for articulation with two sesamoid bones that are imbedded within the tendon of the flexor hallucis brevis (see Figure 14-5). The fifth metatarsal has a prominent styloid process just lateral to its base, marking the attachment of the fibularis brevis muscle (see Figure 14-7).
Phalanges: As in the hand, the foot has 14 phalanges. Each of the four lateral toes contains a proximal, middle, and distal phalanx (see Figure 14-4). The first toe—more commonly called the great toe or hallux—has two phalanges, designated as proximal and distal. In general, each phalanx has a concave base at its proximal end, a shaft, and a convex head at its distal end.
ARTHROLOGY
The major joints of the ankle and foot are the talocrural, subtalar, and transverse tarsal joints (Figure 14-9). As will be described, the talus is mechanically involved with all three of these joints. The multiple articulations made by the talus help to explain the bone’s complex shape, with nearly 70% of its surface covered with articular cartilage. An understanding of the shape of the talus is crucial to an understanding of the kinesiology of the ankle and foot.
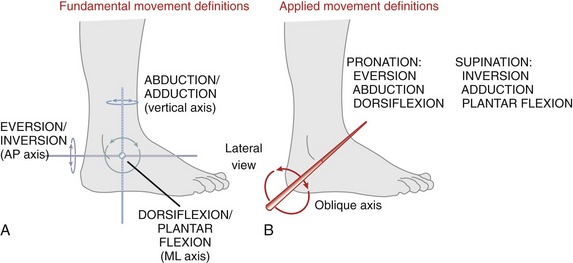
Terminology Used to Describe Movements
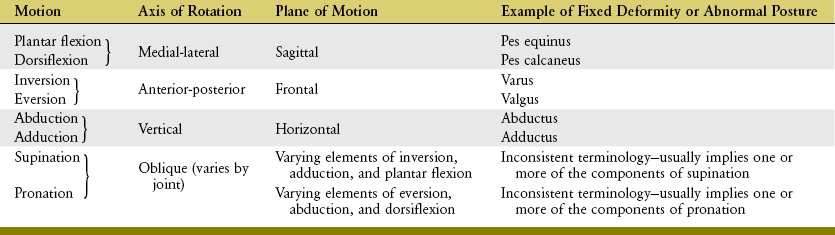
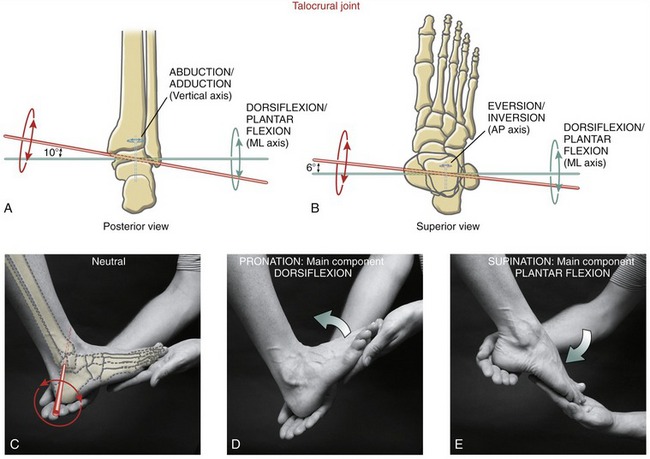
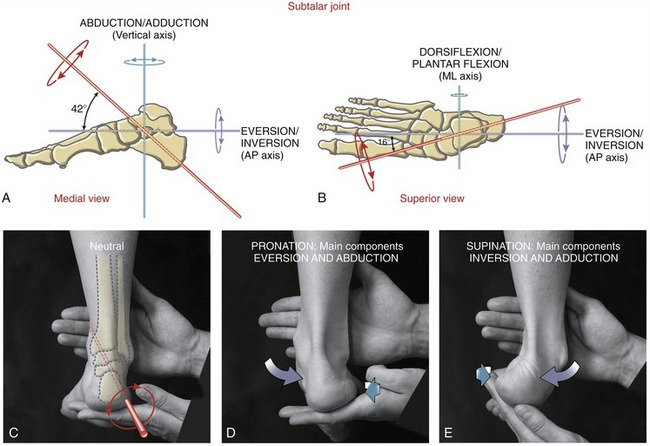
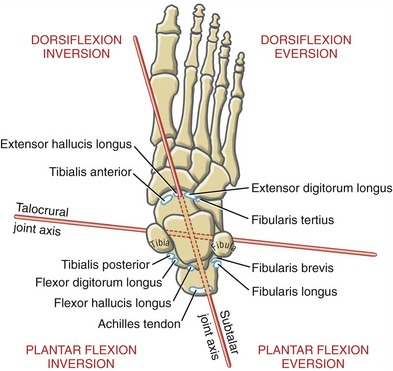
The terminology used to describe movements of the ankle and foot incorporates two sets of definitions: a fundamental set and an applied set. The fundamental terminology defines movement of the foot or ankle as occurring at right angles to the three standard axes of rotation (Figure 14-10, A). Dorsiflexion (extension) and plantar flexion describe motion that is parallel to the sagittal plane, around a medial-lateral axis of rotation. Eversion and inversion describe motion that is parallel to the frontal plane, around an anterior-posterior axis of rotation. Abduction and adduction describe motion that is parallel to the horizontal (transverse) plane, around a vertical (superior-inferior) axis of rotation. For at least the three major joints of the ankle and foot, these fundamental definitions are inadequate because most movements at these joints occur about an oblique axis rather than about the three standard, orthogonal axes of rotation depicted in Figure 14-10, A.
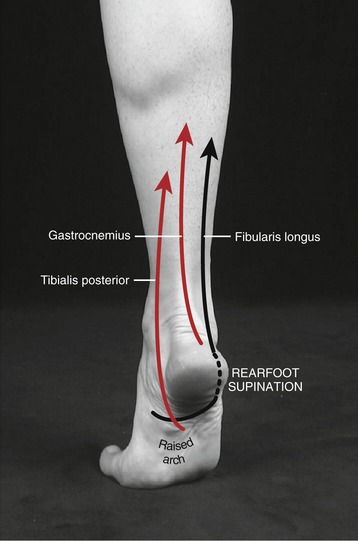
A second and more applied terminology has therefore evolved in the attempt to define the movements that occur perpendicular to the prevailing oblique axes of rotation at the ankle and foot (see Figure 14-10, B). Pronation is defined as a motion that has elements of eversion, abduction, and dorsiflexion. Supination, in contrast, is defined as a motion that has elements of inversion, adduction, and plantar flexion. The orientation of the oblique axis of rotation depicted in Figure 14-10, B varies across the major joints but, in general, has a pitch that is similar to that illustrated. The exact pitch of each major joint’s axis of rotation is described in subsequent sections.
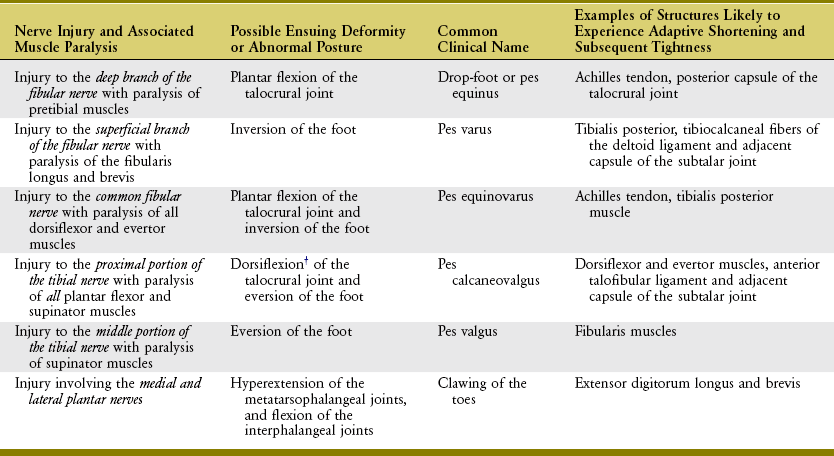
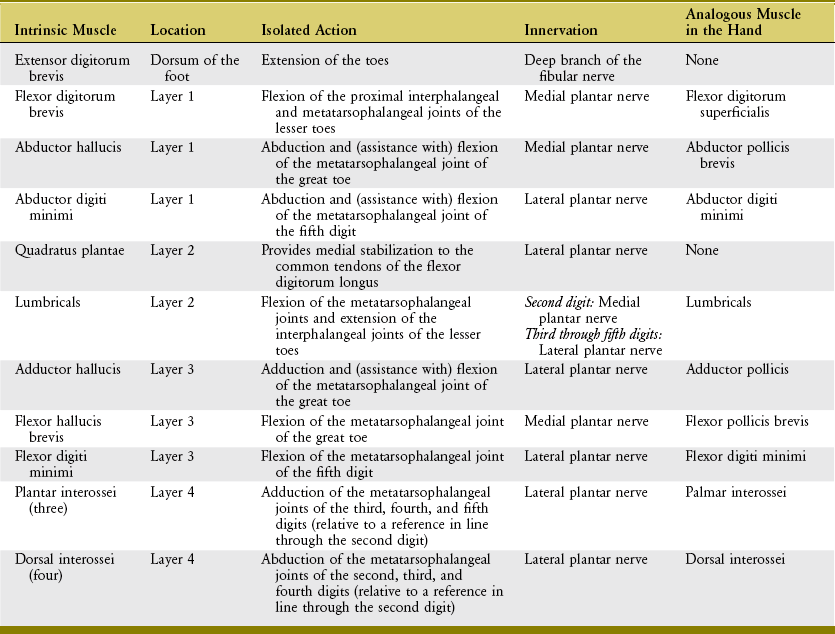
Pronation and supination motions have been called “triplanar” motions. Unfortunately, this description is misleading. The term triplanar implies only that the movements “cut through” each of the three cardinal planes, not that the joint exhibiting this movement possesses three degrees of freedom. Pronation and supination occur in one plane. Table 14-2 summarizes the terminology used to describe the movements of the ankle and foot, including the terminology that describes abnormal posture or deformity.
Structure and Function of the Joints Associated with the Ankle
From an anatomic perspective, the ankle includes one articulation: the talocrural joint. An important structural component of this joint is the articulation formed between the tibia and fibula—an articulation reinforced by the proximal and distal tibiofibular joints and the interosseous membrane of the leg (see Figure 13-3). Because of this functional association, the proximal and distal tibiofibular joints are included under the topic of the “ankle.”
PROXIMAL TIBIOFIBULAR JOINT
The proximal tibiofibular joint is a synovial joint located lateral to and immediately inferior to the knee. The joint is formed between the head of the fibula and the posterior-lateral aspect of the lateral condyle of the tibia (see Figure 13-4). The joint surfaces are generally flat or slightly oval, covered by articular cartilage.120
A capsule strengthened by anterior and posterior ligaments encloses the proximal tibiofibular joint (see Figures 13-7 and 13-9). The tendon of the popliteus muscle provides additional stabilization as it crosses the joint posteriorly. Very little gliding motion occurs at this joint; a firm articulation is needed to ensure that forces within the biceps femoris and lateral collateral ligament of the knee are transferred effectively from the fibula to the tibia.
DISTAL TIBIOFIBULAR JOINT
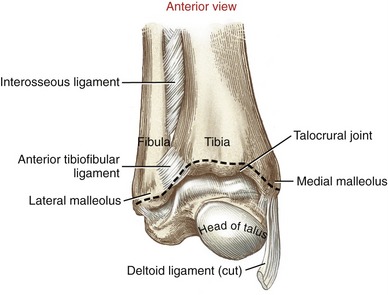
The distal tibiofibular joint is formed by the articulation between the medial surface of the distal fibula and the fibular notch of the tibia (Figure 14-11).6 Anatomists frequently refer to the distal tibiofibular joint as a syndesmosis, which is a type of fibrous synarthrodial joint that is closely bound by an interosseous membrane.120 Relatively little movement is permitted between the distal tibia and distal fibula.
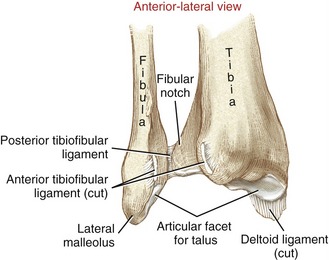
FIGURE 14-11. An anterior-lateral view of the right distal tibiofibular joint with the fibula reflected to show the articular surfaces.
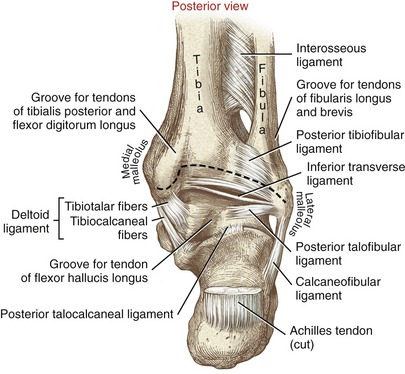
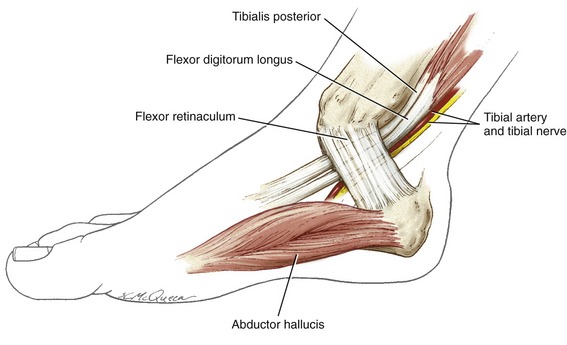
The interosseous ligament provides the strongest bond between the distal end of the tibia and fibula (see Figure 14-3).120 This ligament is an extension of the interosseous membrane between the tibia and fibula. The anterior and posterior (distal) tibiofibular ligaments also stabilize the joint (Figures 14-11 and 14-12). A stable union between the distal tibia and fibula is essential to the stability and function of the talocrural joint.
TALOCRURAL JOINT
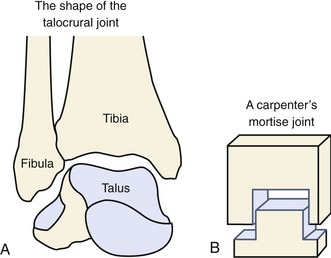
Articular Structure: The talocrural joint is the articulation of the trochlea (dome) and sides of the talus with the rectangular cavity formed by the distal end of the tibia and both malleoli (see Figures 14-3 and 14-9). The talocrural joint is often referred to as the “mortise,” owing to its resemblance to the wood joint used by carpenters (Figure 14-13). The concave shape of the proximal side of the mortise is maintained by connective tissues that bind the tibia with the fibula. The confining shape of the talocrural joint provides a major source of natural stability to the ankle.128
The structure of the mortise must be sufficiently stable to accept the forces that pass between the leg and foot. Although variable, approximately 90% to 95% of the compressive forces pass through the talus and tibia; the remaining 5% to 10% pass through the lateral region of the talus and the fibula.18 The talocrural joint is lined with about 3 mm of articular cartilage, which can be compressed by 30% to 40% in response to peak physiologic loads.135 This load-absorption mechanism protects the subchondral bone from damaging stress.
Ligaments: A thin capsule surrounds the talocrural joint. Externally, the capsule is reinforced by collateral ligaments that help maintain the stability between the talus and the rectangular “socket” of the mortise.
The medial collateral ligament of the talocrural joint is called the deltoid ligament, based on its triangular shape. This ligament is broad and expansive (Figure 14-14). Its apex is attached to the medial malleolus, with its base fanning into three sets of superficial fibers (see box). Deeper tibiotalar fibers blend with and strengthen the medial capsule of the talocrural joint.
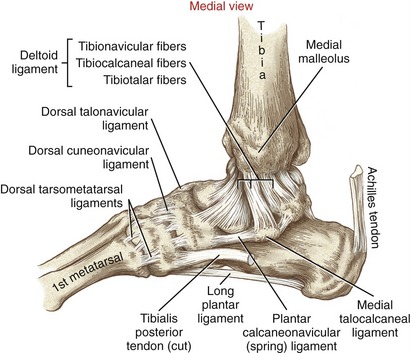
FIGURE 14-14. Medial view of the right ankle region highlights the medial collateral (deltoid) ligament.
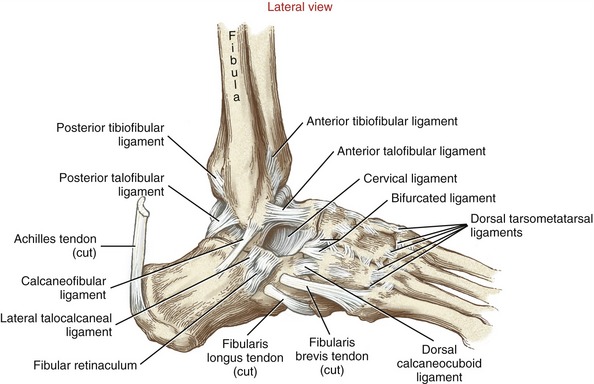
The lateral collateral ligaments of the ankle include the anterior and posterior talofibular and the calcaneofibular ligaments. Because of the relative inability of the medial malleolus to block the medial side of the mortise, the overwhelming majority of ankle sprains involve excessive inversion, often involving injury to the lateral collateral ligaments.8
The anterior talofibular ligament attaches to the anterior aspect of the lateral malleolus, then courses anteriorly and medially to the neck of the talus (Figure 14-15). This ligament is the most frequently injured of the lateral ligaments. Injury is often caused by excessive inversion or (horizontal plane) adduction of the ankle, especially when combined with plantar flexion—for example, when inadvertently stepping into a hole or onto someone’s foot while landing from a jump.115 The calcaneofibular ligament courses inferiorly and posteriorly from the apex of the lateral malleolus to the lateral surface of the calcaneus (see Figure 14-15). This ligament resists inversion across the talocrural joint (especially when fully dorsiflexed) and the subtalar joint. As a pair, the calcaneofibular and anterior talofibular ligaments limit inversion throughout most of the range of ankle dorsiflexion and plantar flexion.21 About two thirds of all lateral ankle ligament injuries involve both of these ligaments.36,54
The posterior talofibular ligament originates on the posterior-medial side of the lateral malleolus and attaches to the lateral tubercle of the talus (see Figures 14-12 and 14-15). Its fibers run horizontally across the posterior side of the talocrural joint, in an oblique anterior-lateral to posterior-medial direction (Figure 14-16). The primary function of the posterior talofibular ligament is to stabilize the talus within the mortise. In particular, it limits excessive abduction of the talus, especially when the ankle is fully dorsiflexed.21
The inferior transverse ligament is a small thick strand of fibers considered part of the posterior talofibular ligament (see Figure 14-12). The fibers continue medially to the posterior aspect of the medial malleolus, forming part of the posterior wall of the talocrural joint.
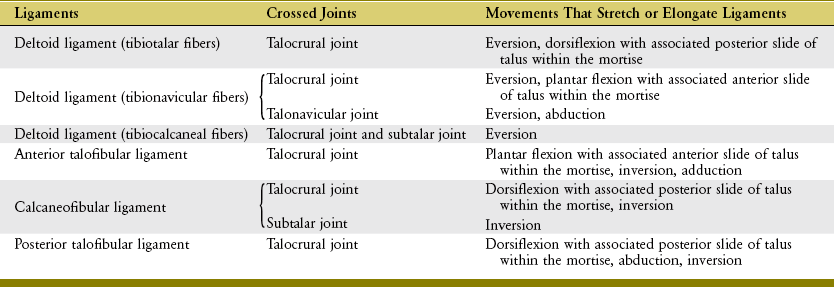
Several of the major ligaments that cross the talocrural joint also cross other joints of the foot, such as the subtalar and talonavicular joints. These ligaments therefore provide stability across multiple joints. Table 14-3 provides a summary of the movements that stretch the major ligaments of the ankle. This information helps explain the mechanisms that frequently injure these ligaments, as well as the rationale behind the manual stress tests performed to evaluate the structural integrity of the ligaments after injury.
Osteokinematics: The talocrural joint possesses one degree of freedom. Motion occurs around an axis of rotation that passes through the body of the talus and through the tips of both malleoli. Because the lateral malleolus is inferior and posterior to the medial malleolus (which should be verified by palpation), the axis of rotation departs slightly from a pure medial-lateral axis. As depicted in Figure 14-17, A and B, the axis of rotation (in red) is inclined slightly superiorly and anteriorly as it passes laterally to medially through the talus and both malleoli.78 The axis deviates from a pure medial-lateral axis about 10 degrees in the frontal plane (see Figure 14-17, A) and 6 degrees in the horizontal plane (see Figure 14-17, B). Because of the pitch of the axis of rotation, dorsiflexion is associated with slight abduction and eversion, and plantar flexion with slight adduction and inversion.118 By definition, therefore, the talocrural joint produces a movement of pronation and supination. Because the axis of rotation deviates only minimally from the pure medial-lateral axis, the main components of pronation and supination at the talocrural joint are overwhelmingly dorsiflexion and plantar flexion (see Figure 14-17, D and E).76,119 The horizontal and frontal plane components of pronation and supination are indeed small,88 and usually ignored in most clinical situations.
The 0-degree (neutral) position at the talocrural joint is defined by the foot held at 90 degrees to the leg. From this position, the talocrural joint permits about 15 to 25 degrees of dorsiflexion and 40 to 55 degrees of plantar flexion, although reported values differ considerably based on type and method of measurement.10,40,118 Accessory movements at the nearby subtalar joint may contribute to about 20% of the total reported range of motion.40 Dorsiflexion and plantar flexion at the talocrural joint need to be visualized when the foot is off the ground and free to rotate, and when the foot is fixed to the ground as the leg rotates forward, such as during the stance phase of gait.
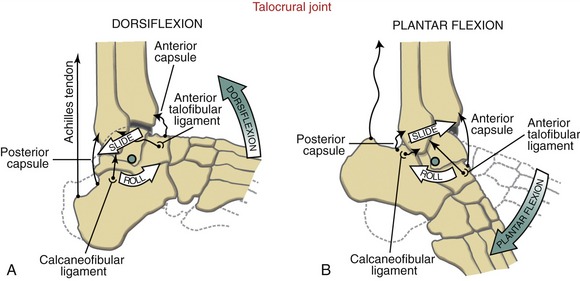
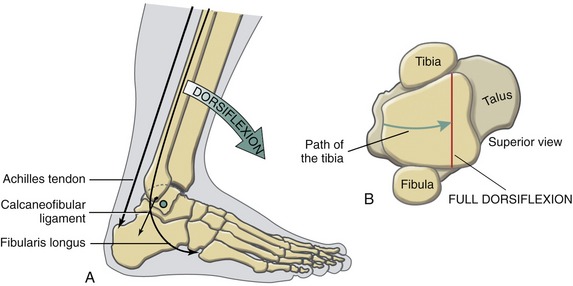
Arthrokinematics: The following discussion assumes that the foot is unloaded and free to rotate. During dorsiflexion, the talus rolls forward relative to the leg as it simultaneously slides posteriorly (Figure 14-18, A). The simultaneous posterior slide allows the talus to rotate forward with only limited anterior translation.22,134 Figure 14-18, A shows the calcaneofibular ligament becoming taut in response to the posterior sliding tendency of the talus-calcaneal segment. Generally, any collateral ligament that becomes increasingly taut on posterior translation of the talus also becomes increasingly taut during dorsiflexion. Maximal dorsiflexion elongates the posterior capsule and all tissues capable of transmitting plantar flexion torque, such as the Achilles tendon.
Full dorsiflexion of the ankle is often limited after a sprain of the lateral ankle. One therapeutic approach aimed at increasing dorsiflexion involves passive joint mobilization of the talocrural joint. Specifically, the clinician applies a posterior-directed translation of the talus and foot relative to the leg.38,134 An appropriately applied posterior slide is designed to mimic the natural arthrokinematics of dorsiflexion at the talocrural joint.
During plantar flexion, the talus rolls posteriorly as the bone simultaneously slides anteriorly (see Figure 14-18, B). Generally, any collateral ligament that becomes increasingly taut on anterior translation of the talus also becomes increasingly taut during plantar flexion. As depicted in Figure 14-18, B, the anterior talofibular ligament is stretched in full plantar flexion. (Although not depicted, the tibionavicular fibers of the deltoid ligament would also become taut at full plantar flexion [review Table 14-3]). Plantar flexion also stretches the dorsiflexor muscles and the anterior capsule of the joint.
Progressive Stabilization of the Talocrural Joint throughout the Stance Phase of Gait: At initial heel contact during walking, the ankle rapidly plantar flexes in order to lower the foot to the ground (Figure 14-19; from 0% to 5% of the gait cycle). As soon as the foot flat phase of gait is reached, the leg starts to rotate forward (dorsiflex) over the grounded foot.68 Dorsiflexion continues until after just after heel off phase. At this point in the gait cycle, the ankle becomes increasing stable owing to the increased tension in many stretched collateral ligaments and plantar flexor muscles (Figure 14-20, A). The dorsiflexed ankle is further stabilized as the wider anterior part of the talus wedges into the tibiofibular component of the mortise (see Figure 14-20, B).18 The wedging effect causes the distal tibia and fibula to spread apart slightly. This action is resisted by tension in the distal tibiofibular ligaments and interosseous membrane.6 At the initiation of the push off phase of walking (just after about 40% of the gait cycle; see Figure 14-19), the fully dorsiflexed talocrural joint is well stabilized to accept compression forces that may reach over four times body weight.121 This inherent stability may partially account for the relatively low frequency of idiopathic osteoarthritis at the talocrural joint.18,81 Posttraumatic arthritis at the talocrural joint is, however, relatively common. Residual incongruity within the mortise after trauma can increase intra-articular stress to damaging levels.
The slight natural spreading of the mortise at maximal dorsiflexion causes slight translation of the fibula.13 The line of force of the stretched anterior and posterior (distal) tibiofibular ligaments and interosseous membrane produces a slight superior translation of the fibula that is transferred proximally to the proximal tibiofibular joint. For this reason, the proximal tibiofibular joint is related more functionally to the ankle (talocrural joint) than to the knee.
Structure and Function of the Joints Associated with the Foot
The subtalar joint, as its name indicates, resides under the talus (see Figure 14-9). To appreciate the extent of subtalar joint motion, one need only firmly grasp the unloaded calcaneus and twist it in a side-to-side and rotary fashion. During this motion, the talus remains essentially stationary within the tight-fitting talocrural joint. Pronation and supination during non–weight-bearing activities occur as the calcaneus moves relative to the fixed talus. In weight bearing such as during the stance phase of walking, for example, pronation and supination occur as the calcaneus remains relatively stationary. This situation requires complex kinematics involving the leg and talus (as a common unit) rotating over the stable calcaneus. This mobility at the subtalar joint allows the foot to assume positions that are independent of the orientation of the superimposed ankle and leg. This function is essential to activities such as walking across a steep hill, standing with feet held wide apart, quickly changing directions while walking or running, and keeping one’s balance on a rocking boat.
Articular Structure: The large, complex subtalar joint consists of three articulations formed between the posterior, middle, and anterior facets of the calcaneus and the talus. These articulations are depicted in yellow in Figure 14-21.
The prominent posterior articulation of the subtalar joint occupies about 70% of the total articular surface area. (Some anatomy texts limit the description of the subtalar joint to the prominent posterior facets only, referring to it as the talocalcaneal joint.120) The concave posterior facet of the talus rests on the convex posterior facet of the calcaneus. The articulation is held tightly opposed by its interlocking shape, ligaments, body weight, and activated muscle. The closely aligned anterior and middle articulations consist of smaller, nearly flat joint surfaces. Although all three articulations contribute to movement at the subtalar joint, clinicians typically focus on the more prominent posterior articulation when performing mobilization techniques to increase the flexibility of the rearfoot.
Ligaments: The posterior and anterior-middle articulations within the subtalar joint are each enclosed by a separate capsule. The larger, posterior capsule is reinforced by three slender thickenings: medial, posterior, and lateral talocalcaneal ligaments (see Figures 14-12, 14-14, and 14-15). These ligaments are often indistinguishable from the capsule and serve as secondary stabilizers of the joint. Other more prominent ligaments provide the primary source of stabilization to the joint as a whole (Table 14-4). The calcaneofibular ligament limits excessive inversion, and the deltoid ligament (tibiocalcaneal fibers) limit excessive eversion. (The anatomy of these ligaments was described previously with the talocrural joint.)
TABLE 14-4.
Primary Functions of the Prominent Ligaments of the Subtalar Joint
| Ligament | Primary Function at the Subtalar joint |
| Calcaneofibular | Limits excessive inversion |
| Tibiocalcaneal fibers of the deltoid ligament | Limits excessive eversion |
| Interosseous (talocalcaneal) Cervical |
Both ligaments bind the talus with the calcaneus; limit the extremes of all motions, especially inversion |
The interosseous (talocalcaneal) and cervical ligaments attach directly between the talus and calcaneus120 and therefore provide the greatest nonmuscular stability to the subtalar joint. These broad and flat ligaments cross obliquely within the tarsal sinus and therefore are difficult to view unless the joint is disarticulated, as depicted previously in Figure 14-8. The interosseous (talocalcaneal) ligament has two distinct, flattened, anterior and posterior bands. These bands arise from the calcaneal sulcus and course superiorly to attach within the talar sulcus and adjacent regions. The larger cervical ligament has an oblique fiber arrangement similar to the interosseous ligament but attaches more laterally within the calcaneal sulcus. From this attachment the cervical ligament courses superiorly and medially to attach primarily to the inferior-lateral surface of the neck of the talus (hence the name “cervical”) (see Figure 14-15). The interosseous and cervical ligaments limit the extremes of all motions—most notably inversion.61,120,127
Although the ligaments within the tarsal sinus are recognized as primary stabilizers at the subtalar joint, a precise anatomic description and a full understanding of their function are unclear.53,127 This lack of knowledge has limited the development of standard clinical “stress tests” to aid in the diagnosis of ligamentous injury. Cadaveric study suggest that a lateral-to-medial translational force applied to the calcaneus specifically stresses the interosseous ligament.127 This finding is consistent with the ligament’s proposed function of resisting inversion at the subtalar joint.
Kinematics: The arthrokinematics at the subtalar joint involve a sliding motion among the three sets of facets, yielding a curvilinear arc of movement between the calcaneus and the talus. Although considerable variation exists from one person to another,71 the axis of rotation is typically described as a line that pierces the lateral-posterior heel and courses through the subtalar joint in anterior, medial, and superior directions (Figure 14-22, A to C, red).51,80,103 The axis of rotation is positioned 42 degrees from the horizontal plane (see Figure 14-22, A) and 16 degrees from the sagittal plane (see Figure 14-22, B).80
Pronation and supination of the subtalar joint occur as the calcaneus moves relative to the talus (or vice versa when the foot is planted) in an arc that is perpendicular to the axis of rotation (see the red circular arrows in Figure 14-22, A to C). Given the general pitch to the axis, only two of the three main components of pronation and supination are strongly evident: inversion and eversion, and abduction and adduction (see Figure 14-22, A and B). Pronation, therefore, has main components of eversion and abduction (see Figure 14-22, D); supination has main components of inversion and adduction (see Figure 14-22, E). The calcaneus does dorsiflex and plantar flex slightly relative to the talus; however, this motion is small and usually ignored clinically. Overall, the kinematic pattern expressed at the subtalar joint is much greater than at the talocrural joint.76
For simplicity, the osteokinematics of the subtalar joint have been pictorially demonstrated by the calcaneus moving relative to a fixed and essentially immobile talus. During walking, however, when the calcaneus is relatively immobile because of the load of body weight, a significant portion of pronation and supination occur by horizontal plane rotation of the talus and leg. Because of the inherent stability and fit provided by the mortise, the majority of the horizontal plane rotation of the talus is mechanically coupled to the rotation of the leg. Small horizontal plane accessory motions within the talocrural joint absorb a small component of this rotation.96
Range of Motion: Grimston and colleagues reported active range of inversion and eversion motions at the subtalar joint across 120 healthy subjects (aged 9 through 79 years).40 Results showed that inversion exceeds eversion by nearly double: inversion, 22.6 degrees; eversion, 12.5 degrees. Although these data include accessory rotations at the talocrural joint, the much greater ratio of inversion to eversion is typical of that reported for the subtalar joint alone.5,125 Studies that measure passive range of motion usually report greater magnitudes of motion, with inversion-to-eversion ratios approaching 3 : 1.142 Regardless of active or passive motion, the distally projecting lateral malleolus and the relatively thick deltoid ligament naturally limit eversion.
TRANSVERSE TARSAL JOINT (TALONAVICULAR AND CALCANEOCUBOID JOINTS)
The transverse tarsal joint, also known as the midtarsal joint, consists of two anatomically distinct articulations: the talonavicular joint and the calcaneocuboid joint. These joints connect the rearfoot with the midfoot (see organization of joints illustrated in Figure 14-23).
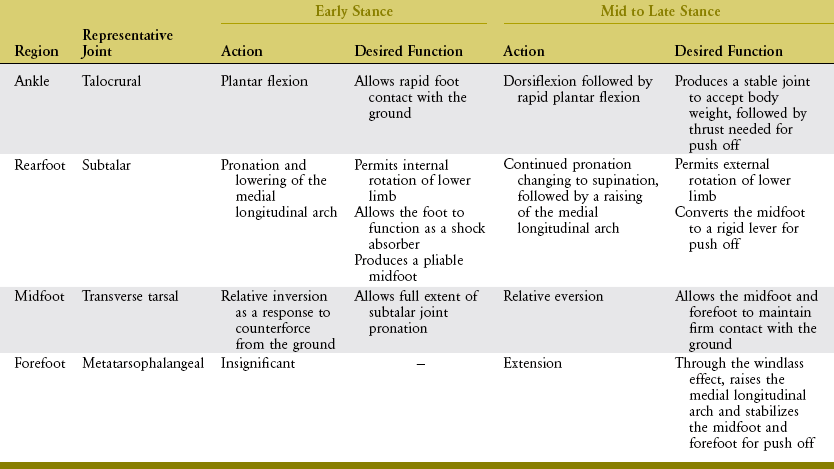
At this particular point in this chapter, it may be instructive to consider the functional characteristics of the transverse tarsal joint within the context of the other major joints of the ankle and foot. As described earlier, the talocrural (ankle) joint permits motion primarily in the sagittal plane: dorsiflexion and plantar flexion. The subtalar joint, however, permits a more oblique path of motion consisting of two primary components: inversion-eversion and abduction-adduction. This section now describes how the transverse tarsal joint, the most versatile joint of the foot, moves through a more oblique path of motion, cutting nearly equally through all three cardinal planes. Among other important functions, the path of pronation and supination at the transverse tarsal joint allows the weight-bearing foot to adapt to a variety of surface contours (Figure 14-24).
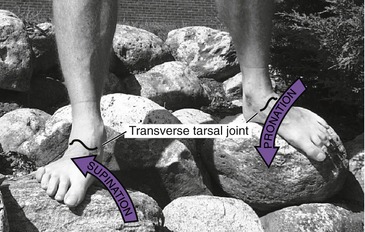
FIGURE 14-24. The transverse tarsal joints allow for pronation and supination of the midfoot while one stands on uneven surfaces.
Articular Structure and Ligamentous Support:
Talonavicular Joint: The talonavicular joint (the medial compartment of the transverse tarsal joint) resembles a ball-and-socket joint, providing substantial mobility to the medial (longitudinal) column of the foot. Much of this mobility is expressed as a twisting (inverting and everting) of the midfoot relative to the rearfoot.74 The talonavicular joint consists of the articulation between the convex head of the talus and the continuous, deep concavity formed by the proximal side of the navicular bone and “spring” ligament (see Figure 14-8). The convex-concave relationship of the talonavicular joint is evident in Figure 14-21. The spring ligament (labeled as SL in Figure 14-21) is a thick and wide band of collagenous connective tissue, spanning the gap between the sustentaculum talus of the calcaneus and the medial-plantar surface of the navicular bone.87 By directly supporting the medial and plantar convexity of the head of the talus, the spring ligament forms the structural “floor and medial wall” of the talonavicular joint. Considerable support is required in this region during standing because body weight tends to depress the head of the talus in plantar and medial directions—toward the earth. The surface of the spring ligament that directly contacts the head of the talus is lined with smooth fibrocartilage.120 (The more formal and precise name of the spring ligament is the plantar calcaneonavicular ligament. The term “spring” is actually a misnomer because it has little, if any, elasticity; its highly collagenous nature offers considerable strength and resistance to elongation. Nevertheless, the term spring remains well established in the clinical and research literature.87)
Calcaneocuboid Joint: The calcaneocuboid joint is the lateral component of the transverse tarsal joint, formed by the junction of the anterior (distal) surface of the calcaneus with the proximal surface of the cuboid (see Figure 14-23). Each articular surface has a concave and convex curvature. The joint surfaces form an interlocking wedge that resists sliding. The calcaneocuboid joint allows less motion than the talonavicular joint, especially in the frontal and horizontal planes.76 The relative inflexibility of the calcaneocuboid joint provides stability to the lateral (longitudinal) column of the foot.
The dorsal and lateral parts of the capsule of the calcaneocuboid joint are thickened by the dorsal calcaneocuboid ligament (see Figure 14-15).102 Three additional ligaments further stabilize the joint. The bifurcated ligament is a Y-shaped band of tissue with its stem attached to the calcaneus, just proximal to the dorsal surface of the calcaneocuboid joint. The stem of the ligament flares into lateral and medial fiber bundles. The aforementioned medial (calcaneonavicular) fibers reinforce the lateral side of the talonavicular joint. The lateral (calcaneocuboid) fibers cross the dorsal side of the calcaneocuboid joint, forming the primary bond between the two bones.120
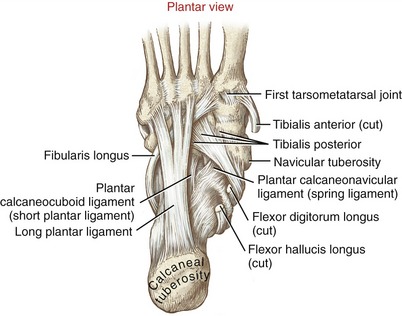
The long and short plantar ligaments reinforce the plantar side of the calcaneocuboid joint (Figure 14-25). The long plantar ligament, the longest ligament in the foot, arises from the plantar surface of the calcaneus, just anterior to the calcaneal tuberosity. The ligament inserts on the plantar surface of the bases of the lateral three or four metatarsal bones. The short plantar ligament, also called the plantar calcaneocuboid ligament, arises just anterior and deep to the long plantar ligament and inserts on the plantar surface of the cuboid bone. By passing perpendicularly to the calcaneocuboid joint, the plantar ligaments provide excellent structural stability to the lateral column of the foot.70
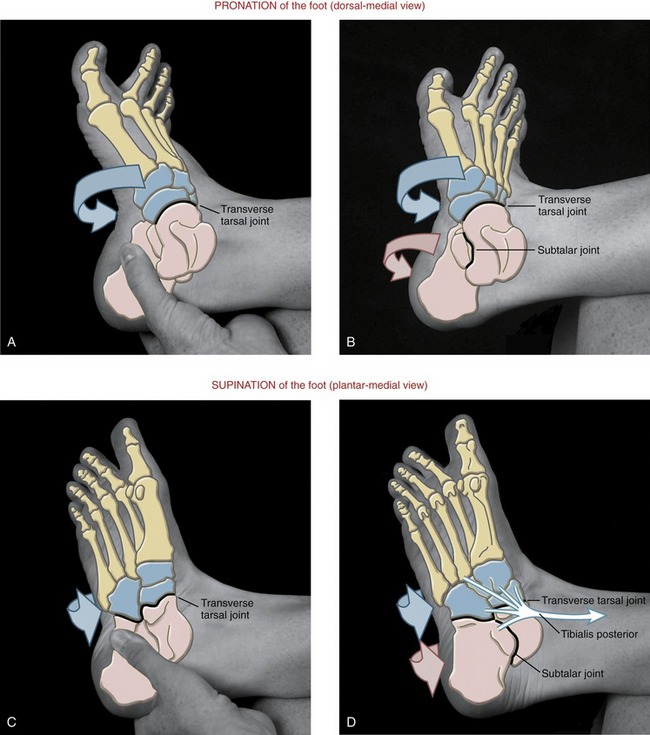
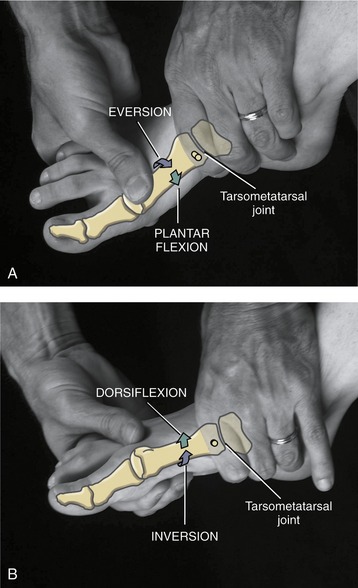
Kinematics: The transverse tarsal joint rarely moves without associated movements at nearby joints, especially the subtalar joint. To appreciate the mobility that occurs primarily at the transverse tarsal joint, hold the calcaneus firmly while maximally pronating and supinating the midfoot (Figure 14-26, A and C, respectively). During these motions the navicular spins within the talonavicular joint.74 Combining motions across both the subtalar and transverse tarsal joints accounts for most of the pronation and supination throughout the foot (see Figure 14-26, B and D, respectively). As evident throughout Figure 14-26, mobility of the forefoot contributes to the pronation and supination of the entire foot.
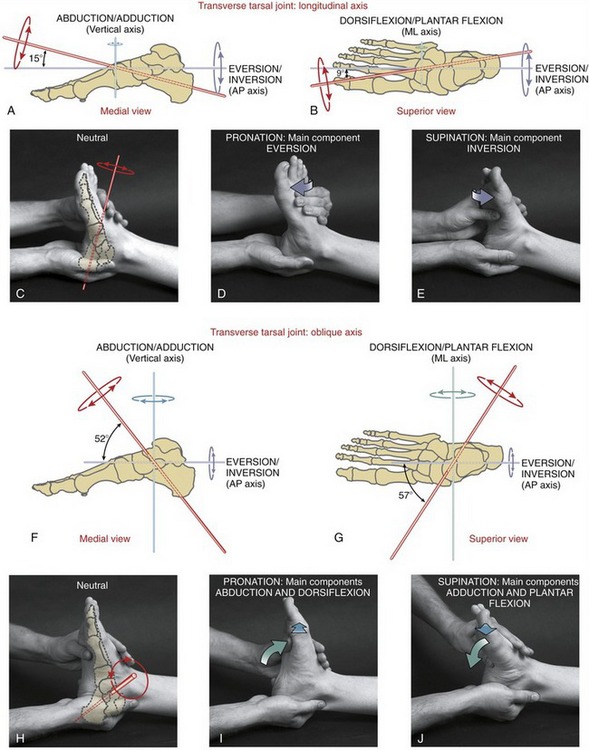
Axes of Rotation and Corresponding Movements: Manter originally described two axes of rotation for movement at the transverse tarsal joint: longitudinal and oblique.80 Movement at this joint therefore occurs naturally in two unique planes, each oriented perpendicular to a specific axis of rotation. The longitudinal axis is nearly coincident with the straight anterior-posterior axis (Figure 14-27, A to C), with the primary component motions of eversion and inversion (see Figure 14-27, D and E). The oblique axis, in contrast, has a strong vertical and medial-lateral pitch (see Figure 14-27, F to H). Motion around this axis, therefore, occurs freely as a combination of abduction and dorsiflexion (Figure 14-27, I), and adduction and plantar flexion (see Figure 14-27, J).
The transverse tarsal joint possesses two separate axes of rotation, with each axis producing a unique kinematic pattern. Although this may be technically correct, the functional kinematics associated with most weight-bearing activities occur as a blending of movements across both axes—a blend that yields the purest form of pronation and supination (i.e., movement that maximally expresses components of all three cardinal planes).76,95 Pronation and supination at the transverse tarsal joint allow the midfoot (and ultimately the forefoot) to adapt to many varied shapes and contours.
Arthrokinematics: The arthrokinematics at the transverse tarsal joint are best described in context with motion across both the rearfoot and midfoot. Consider the movement of active supination of the unloaded foot in Figure 14-26, D. The tibialis posterior muscle, with its multiple attachments, is the prime supinator of the foot.64 Because of the relatively rigid calcaneocuboid joint, an inverting and adducting calcaneus draws the lateral column of the foot “under” the medial column of the foot. The important pivot point for this motion is the talonavicular joint. The pull of the tibialis posterior contributes to the spin of the navicular, and to the raising of the medial longitudinal arch (instep) of the foot. During this motion, the concave proximal surface of the navicular and the spring ligament both spin around the convex head of the talus.
Medial Longitudinal Arch of the Foot: Figure 14-28 shows the locations of the medial longitudinal and transverse arches of the foot. Both arches lend very important elements of stability and resiliency to the loaded foot. The talonavicular joint serves as the keystone to the medial longitudinal arch. For this reason, the structure and function of the medial longitudinal arch is addressed in this section. The transverse arch is described later during the study of the distal intertarsal joints.
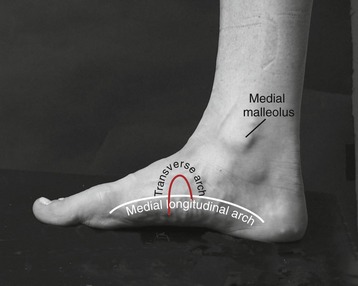
FIGURE 14-28. The medial side of a normal foot shows the medial longitudinal arch (white) and the transverse arch (red).
The medial longitudinal arch is evident as the characteristic concave “instep” of the medial side of the foot. This arch is the primary load-bearing and shock-absorbing structure of the foot.129 The bones that form the medial arch are the calcaneus, talus, navicular, cuneiforms, and associated three medial metatarsals. Without this arched configuration, the large and rapidly produced forces applied against the foot during running, for example, would likely exceed the physiologic weight-bearing capacity of the bones. Additional structures that assist the arch in absorbing loads are the plantar fat pads, sesamoid bones located at the plantar base of the great toe, and superficial plantar fascia (which attaches primarily to the overlying thick dermis, functioning primarily to reduce shear forces.) As will be described, the medial longitudinal arch and associated connective tissues are usually adequate to support the foot during relatively low-stress or near-static conditions—for example, standing at ease. Active muscular forces, however, assist the arch when the stresses and loads on the foot are larger and more dynamic, such as during standing on tiptoes, walking, jumping, or running. The following section describes the passive support mechanism provided by the medial longitudinal arch. The role of muscles in providing active support is described later, in the study of muscles of the ankle and foot.
Passive Support Mechanism of the Medial Longitudinal Arch: The talonavicular joint and associated connective tissues form the keystone of the medial longitudinal arch. Additional nonmuscular structures responsible for maintaining the height and general shape of this arch are the plantar fascia, spring ligament, and first tarsometatarsal joint. The plantar fascia of the foot provides the primary passive support to the medial longitudinal arch.26,48 This extremely strong fascia consists of a series of thick, longitudinal and transverse bands of collagen-rich tissue.59 The plantar fascia covers the sole and sides of the foot and is organized into superficial and deep fibers. The superficial fibers, introduced above, attach primarily to the overlying thick dermis. The more extensive deep plantar fascia attaches posteriorly to the medial process of the calcaneal tuberosity. From this origin, lateral, medial, and central sets of fibers course anteriorly, blending with and covering the first layer of the intrinsic muscles of the foot. The main, larger, central set of fibers extends toward the metatarsal heads, where the fibers attach to the plantar plates (ligaments) of the metatarsophalangeal joints and fibrous sheaths of the adjacent flexor tendons of the digits. Active toe extension therefore stretches the central band of deep fascia, adding tension to the medial longitudinal arch. This mechanism is useful because it increases tension in the arch when one stands on tiptoes, or during the push off phase of gait.
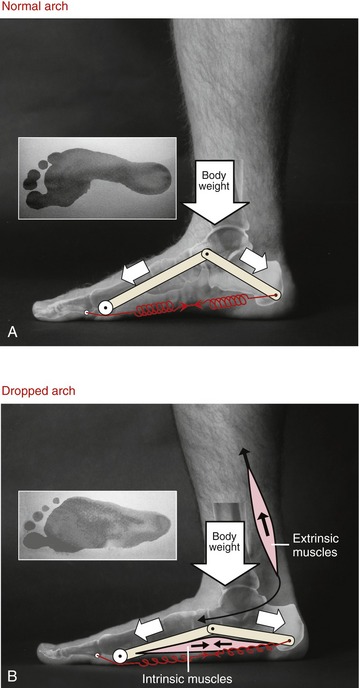
When one stands normally, the weight of the body falls through the foot near the region of talonavicular joint. This load is distributed anteriorly and posteriorly throughout the medial longitudinal arch, ultimately passing to the fat pads and the thick dermis over the heel and ball (metatarsal head region) of the foot (Figure 14-29, A). Normally the rearfoot receives about twice the compressive load as the forefoot.20 The mean pressure under the forefoot is usually greatest in the region of the heads of the second and third metatarsal bones.
During standing, body weight tends to depress the talus inferiorly and flatten the medial longitudinal arch. This action increases the distance between the calcaneus and metatarsal heads. Tension in stretched connective tissues, especially the deep plantar fascia, acts as a semi-elastic tie-rod that “gives” slightly under load, allowing only a marginal drop in the arch (see stretched spring in Figure 14-29, A). Acting like a truss, the tie-rod supports and absorbs body weight. Experiments on cadaveric specimens indicate that the deep plantar fascia is the major structure that maintains the height of the medial longitudinal arch; cutting the fascia decreased arch stiffness by 25%.48
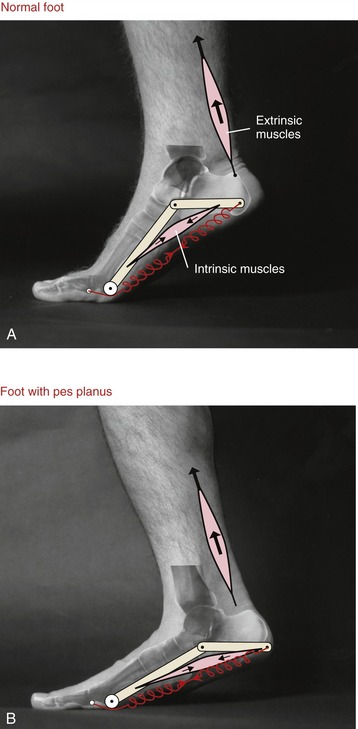
Standing at ease on healthy feet typically produces very little activity from the intrinsic or extrinsic muscles of the foot.4 The height and shape of the medial longitudinal arch is controlled primarily by passive restraints from the connective tissues depicted by the spring in Figure 14-29, A. Active muscle support during standing is usually required only as a “secondary line of support”—for example, when a heavy load is held, or when the arch lacks inherent support because of overstretched connective tissues.126
Pes Planus—“Abnormally Dropped” Medial Longitudinal Arch: Pes planus or “flatfoot” describes a chronically dropped or abnormally low medial longitudinal arch.58,144 This condition is often the result of joint laxity within the midfoot or proximal forefoot regions, typically combined with an overstretched or weakened plantar fascia, spring ligament, and tibialis posterior tendon.97,129 During the stance phase of walking, the subtalar joint subsequently pronates excessively as the rearfoot assumes an exaggerated valgus posture (calcaneus excessively everted away from the midline).129 The depressed talus and navicular bones often cause a callus on the adjacent skin.
Figure 14-29, B shows the foot of a person with pes planus. The abnormally wide midfoot region evident in the footprint is indicative of excessive laxity within the joints that normally support the arch.55 A person with moderate or severe pes planus typically has a compromised ability to dissipate loads optimally throughout the foot. Active forces from intrinsic and extrinsic muscles are often required to compensate for the lack of tension produced in overstretched or weakened connective tissues. Increased muscular activity may be needed even during quiet standing, which may contribute to fatigue and various overuse symptoms, including pain, “shin splints,” bone spurs, and a thickened and inflamed plantar fascia.136
Pes planus is often described as being either a rigid or a flexible deformity. The foot with rigid pes planus (as shown in Figure 14-29, B) demonstrates a dropped arch even in non–weight-bearing positions. This deformity is often congenital, secondary to bony or joint malformation, such as tarsal coalition (i.e., partial fusion of the calcaneus with the talus fixed in eversion). Pes planus may also occur from spastic paralysis and the resultant overpull from certain muscles. Because of the fixed nature and potential for producing painful symptoms, rigid pes planus may require surgical correction during childhood.
Flexible pes planus is the more common form of a dropped arch. The medial longitudinal arch appears essentially normal when unloaded but drops excessively on weight bearing. Acquired flexible pes planus is often associated with tendinopathy or generalized dysfunction of the tibialis posterior muscle, increased laxity of local connective tissues, or structural anomalies and/or compensatory mechanisms that cause excessive pronation of the foot. Surgical intervention is rarely indicated for flexible pes planus. Treatment is usually in the form of orthosis, specialized footwear, and exercise.31,64,66
COMBINED ACTION OF THE SUBTALAR AND TRANSVERSE TARSAL JOINTS
When the foot is unloaded (i.e., not bearing weight), pronation twists the sole of the foot outward, whereas supination twists the sole of the foot inward. While the foot is under load during the stance phase of walking, however, pronation and supination permit the leg and talus to rotate in all three planes relative to a relatively fixed calcaneus. This important mechanism is orchestrated primarily through an interaction among the subtalar joint, transverse tarsal joint, and medial longitudinal arch. Much remains to be learned about this complex topic.68,76,82
In the healthy foot the medial longitudinal arch rises and lowers cyclically throughout the gait cycle. During most of the stance phase, the arch lowers slightly in response to the progressive loading of body weight (Figure 14-31, A).19,50 Structures that resist the lowering of the arch help to absorb local stress as the foot is progressively compressed by body weight. Although not always verifiable through controlled research, this load attenuation mechanism likely protects the foot and lower limb against stress-related injury.27,56,86,138
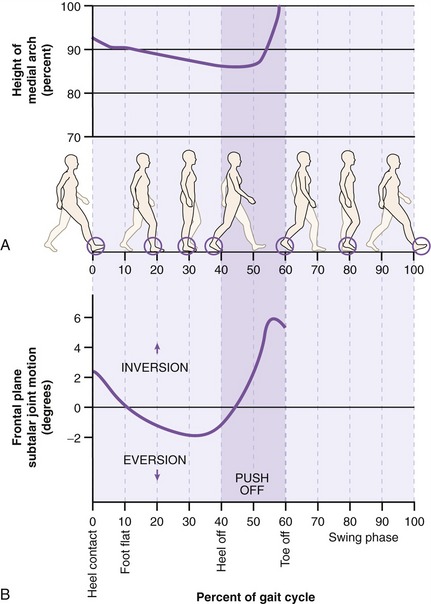
FIGURE 14-31. A, The percent change in height of the medial longitudinal arch throughout the stance phase (0% to 60%) of the gait cycle. On the vertical axis, the 100% value is the height of the arch when the foot is unloaded during the swing phase. B, Plot of frontal plane range of motion at the subtalar joint (i.e., inversion and eversion of the calcaneus) throughout the stance phase.24 The 0-degree reference for frontal plane motions is defined as the position of the calcaneus (observed posteriorly) while a subject stands at rest. The push off phase of walking is indicated by the darker shade of purple.
During the first 30% to 35% of the gait cycle, the subtalar joint pronates (everts), adding an element of flexibility to the midfoot (see Figure 14-31, B).24 By late stance, the arch rises as the supinated subtalar joint adds rigidity to the midfoot. The rigidity prepares the foot to support the large loads produced at the push off phase of gait. The ability of the foot to repeatedly transform from a flexible and shock-absorbent structure to a more rigid lever during each gait cycle is one of the most important and clinically relevant actions of the foot. As subsequently described, the subtalar joint is the principal joint that directs the pronation and supination kinematics of the foot.
Early to Mid-Stance Phase of Gait: Kinematics of Pronation at the Subtalar Joint: Immediately after the heel contact phase of gait, the dorsiflexed talocrural joint and slightly supinated subtalar joint rapidly plantar flex and pronate, respectively (compare Figures 14-19 and 14-31, B). Although the data plotted in Figure 14-31, B show only 2 degrees of average maximum eversion (beyond the resting posture),24 other researchers using asymptomatic subjects report higher values, in the range of 5 to 9 degrees.50,129,142 Differences in defining the 0-degree position of the subtalar joint, dissimilar sample sizes, and the varying measurement techniques account for much of this inconsistency within the literature.142 For this reason, it is often difficult to define what constitutes “abnormal” eversion (pronation) during walking.
The pronation (eversion) at the subtalar joint during stance occurs primarily by two mechanisms. First, the calcaneus tips into slight eversion in response to the ground reaction force passing upward and just lateral to the midpoint of the posterior calcaneus. The simultaneous impact of heel contact also pushes the head of the talus medially in the horizontal plane and inferiorly in the sagittal plane. Relative to the calcaneus, this motion of the talus abducts and (slightly) dorsiflexes the subtalar joint. These motions are consistent with the formal definition of pronation. A loosely articulated skeletal model aids in the visualization of this motion. Second, during the early stance phase, the tibia and fibula, and to a lesser extent the femur, internally rotate after initial heel contact.51,105 Because of the embracing configuration of the talocrural joint, the internally rotating lower leg steers the subtalar joint into further pronation. The argument is often raised that with the calcaneus in contact with the ground, pronation at the subtalar joint causes, rather than follows, internal rotation of the leg; either perspective is valid.
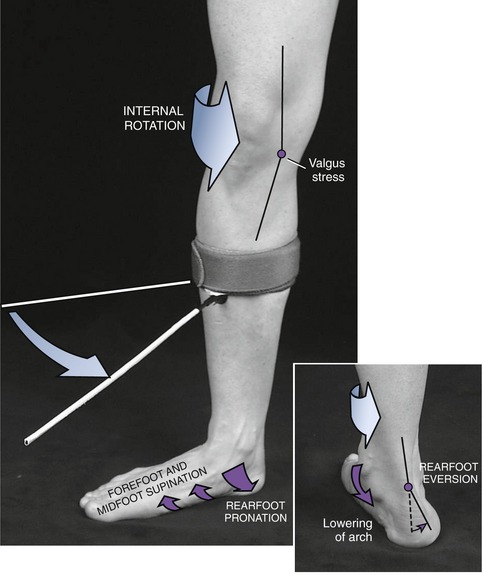
The amplitude of pronation at the subtalar joint during early to mid-stance phase of walking is indeed relatively small—about 5 degrees on average—occurring for only one quarter of a second during average-speed walking. The amount and the speed of the pronation nevertheless influence the kinematics of the more proximal joints of the lower extremity. These effects can be readily appreciated by exaggerating and dramatically slowing the pronation action of the rearfoot during the initial loading phase of gait. Consider the demonstration depicted in Figure 14-32. While standing over a loaded and fixed foot, forcefully but slowly internally rotate the lower limb and observe the associated pronation at the rearfoot (subtalar joint) and simultaneous lowering of the medial longitudinal arch.95 If sufficiently forceful, this action also tends to internally rotate, slightly flex, and adduct the hip and create a valgus stress on the knee (Table 14-5). These mechanical events are indeed exaggerated and do not all occur to this degree and pattern during walking at normal speed. Nevertheless, because of the linkages throughout the lower limb, excessive or uncontrolled pronation of the rearfoot could exaggerate one or more of these mechanically related joint actions.57 Clinically, a person who excessively pronates during early stance may complain of medial knee pain, possibly from excessive valgus stress placed on the knee and subsequent overstretching of the medial collateral ligament. Whether the overpronation causes excessive strain on the medial collateral ligament or vice versa is not always obvious.
TABLE 14-5.
| Joint or Region | Action |
| Hip | Internal rotation, flexion, and adduction |
| Knee | Increased valgus stress |
| Rearfoot | Pronation (eversion) with a lowering of medial longitudinal arch |
| Midfoot and forefoot | Supination (inversion) |
Although widely accepted, a predictable kinematic relationship between the magnitude and timing of excessive pronation and excessive internal rotation throughout the lower limb has not been established conclusively.105 Precise measurements of these kinematic relationships while a subject is walking are technically difficult. The kinematics themselves are highly variable and poorly defined. Some studies report the kinematics as a rotation of a single bone, and others report relative rotations between bones. Additional studies are needed in this area before definite cause-and-effect relationships are known. These relationships are important, as they serve as the basis for many exercises and for the use of orthotics to reduce painful conditions related to excessive or poorly controlled pronation.
Biomechanical Benefits of Limiting Pronation during the Stance Phase: Controlled pronation of the subtalar joint through the mid-stance phase of walking has several useful biomechanical effects. Pronation at the subtalar joint permits the talus and entire lower extremity to rotate internally slightly after the calcaneus has contacted the ground. The strong horizontal orientation of the facets at the subtalar joint certainly facilitates this action. Without such a joint mechanism, the plantar surface of the calcaneus would otherwise “spin” like a child’s top against the walking surface, along with the internally rotating leg. Eccentric activation of supinator muscles, such as the tibialis posterior, can help to decelerate the pronation and resist the lowering of the medial longitudinal arch. Controlled pronation of the subtalar joint favors relative flexibility of the midfoot, allowing the foot to accommodate to the varied shapes and contours of walking surfaces.
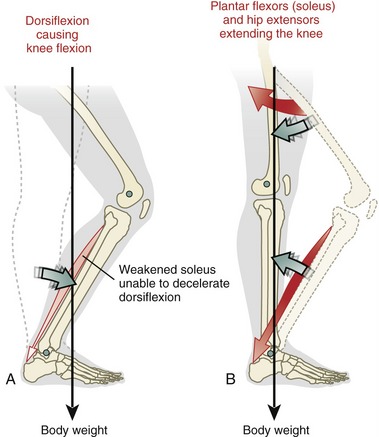
Biomechanical Consequences of Abnormal Pronation during the Stance Phase: Innumerable examples exist on how malalignment within the foot affects the kinematics of walking. One common scenario results from excessive, prolonged, or poorly controlled pronation at the subtalar joint during the stance phase. This disorder can have multiple causes, including weakness of muscles throughout the lower extremity, laxity or weakness in the mechanisms that normally support and control the medial longitudinal arch, or abnormal shape or mobility of the tarsal bones. Regardless of cause, the rearfoot falls into excessive valgus (eversion) after heel contact.83 Excessive subtalar joint pronation may be a compensation for excessive or restricted motion throughout the lower extremity, particularly in the frontal and horizontal planes.
Paradoxically, one of the most common structural deformities within an overpronated foot is a relatively fixed rearfoot varus. (Varus describes a segment of the foot that is inverted toward the midline.) As a response to rearfoot varus, the subtalar joint often overcompensates by excessively pronating, in speed and/or magnitude, to ensure that the medial aspect of the forefoot contacts the ground during stance phase.15,85 Similar compensations may occur with a forefoot varus deformity. Whether the forefoot varus deformity causes or results from excessive pronation of the rearfoot is not always clear.
As described previously, excessive rearfoot pronation is typically associated with excessive (horizontal plane) internal rotation of the talus and leg during walking. Such a movement may create a “chain reaction” of kinematic disturbances and compensations throughout the entire limb, such as those depicted in Figure 14-32. As described in Chapter 13, the abnormal kinematic sequence between the tibia and femur may alter the contact area at the patellofemoral joint, potentially increasing stress at this joint. Furthermore, excessive rearfoot eversion may create an increased valgus stress on the medial side of the knee.104 These situations may predispose a person to patellofemoral joint pain syndrome or instability. For these reasons, clinicians often note the position of the subtalar joint while the patient stands and walks as part of an evaluation for a mechanical cause of patellofemoral joint pain or other related dysfunction.137
The underlying pathomechanics of an excessively pronated foot are complex and not fully understood. The pathomechanics can involve many kinematic relationships, both within the joints of the foot and between the foot and the rest of the lower limb. The origin of the pathomechanics may be related to interactions between the hip and knee (described in Chapter 13) and expressed distally as impairments at the subtalar joint. Even if the pathomechanics are obviously located within the foot, abnormal motion in the forefoot may be compensated for by abnormal motion in the rearfoot and vice versa. Furthermore, extrinsic factors, such as footwear, orthotics, terrain, and speed of walking or running, alter the kinematic relationships within the foot and lower extremity. An understanding of the complex kinesiology of the entire lower extremity is a definite prerequisite for the effective treatment of the painful or misaligned foot.
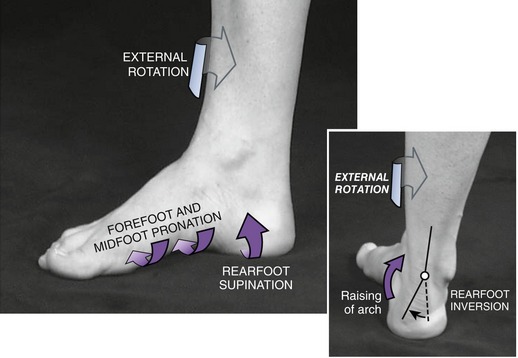
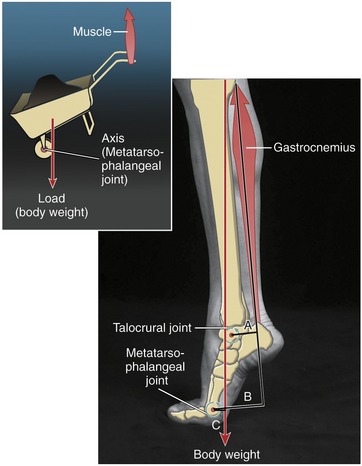
Mid-to-Late Stance Phase of Gait: Kinematics of Supination at the Subtalar Joint: At about 15% to 20% into the gait cycle, the entire stance limb reverses its horizontal plane motion from internal to external rotation.52,105 External rotation of the leg while the foot remains planted coincides roughly with the beginning of the swing phase of the contralateral lower extremity. With the stance foot securely planted, external rotation of the femur, followed by the tibia, gradually reverses the horizontal plane direction of the talus from internal to external rotation. As a result, at about 30% to 35% into the gait cycle, the pronated (everted) subtalar joint starts to move sharply toward supination (inversion) (see Figure 14-31, B). As demonstrated in Figure 14-33, with the rearfoot supinating, the midfoot and forefoot must simultaneously twist into relative pronation in order for the foot to remain in full contact with the ground.75,96 By late stance, the supinated subtalar joint and the elevated and tensed medial longitudinal arch convert the midfoot (and ultimately the forefoot) into a more rigid lever.50,68 Muscles such as the gastrocnemius and soleus use this stability to transfer forces from the Achilles tendon, through the midfoot, to the metatarsal heads during the push off phase of walking or running.
DISTAL INTERTARSAL JOINTS
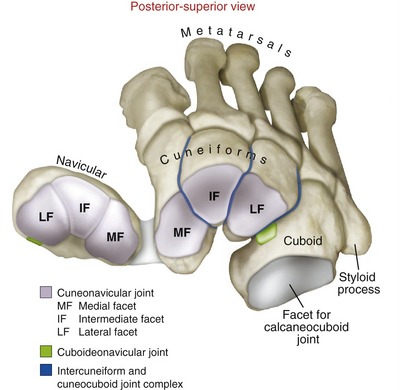
The distal intertarsal joints are a collection of three joints or joint complexes, each occupying a part of the midfoot (review organization of joints of the foot; see Figure 14-23). The articular surfaces of the distal intertarsal joints are exposed and color-coded in Figure 14-34.
Basic Structure and Function: As a group, the distal intertarsal joints (1) assist the transverse tarsal joint in pronating and supinating the midfoot, and (2) provide stability across the midfoot by forming the transverse arch of the foot. Motions in these joints are small and typically not formally described.
Cuneonavicular Joint: Three articulations are formed between the anterior side of the navicular and the posterior surfaces of the three cuneiform bones (see Figure 14-34, purple). Surrounding these articulations are plantar and dorsal ligaments. The slightly concave facets (lateral, intermediate, and medial) on each of the three cuneiforms fit into one of three slightly convex facets on the anterior side of the navicular. The major function of the cuneonavicular joint is to help transfer components of pronation and supination distally toward the forefoot.74
Cuboideonavicular Joint: The small synarthrodial (fibrous) or sometimes synovial cuboideonavicular joint is located between the lateral side of the navicular and a proximal region of the medial side of the cuboid (see Figure 14-34, green).120 This joint provides a relatively smooth contact point between the lateral and medial longitudinal columns of the foot. Observations on cadaver specimens show that the articular surfaces slide slightly against each other during most movements of the midfoot, most notably during inversion and eversion.
Intercuneiform and Cuneocuboid Joint Complex: The intercuneiform and cuneocuboid joint complex consists of three articulations: two between the set of three cuneiforms, and one between the lateral cuneiform and medial surface of the cuboid (see Figure 14-34, blue). Articular surfaces are essentially flat and aligned nearly parallel with the long axis of the metatarsals. Plantar, dorsal, and interosseous ligaments strengthen this set of articulations.
The intercuneiform and cuneocuboid joint complex forms the transverse arch of the foot (Figure 14-35, A). This arch provides transverse stability to the midfoot. Under the load of body weight, the transverse arch depresses slightly, allowing body weight to be shared across all five metatarsal heads. The transverse arch receives support from intrinsic muscles; extrinsic muscles, such as the tibialis posterior and fibularis longus; connective tissues; and the keystone of the transverse arch: the intermediate (IF) cuneiform (see Figure 14-34).
TARSOMETATARSAL JOINTS
Anatomic Considerations: The tarsometatarsal joints are frequently called Lisfranc’s joints, after Jacques Lisfranc, a French field surgeon in Napoleon’s army who described an amputation in this region of the foot. As a group, the five tarsometatarsal joints separate the midfoot from the forefoot (review organization of joints in Figure 14-23). The joints consist of the articulation between the bases of the metatarsals and the distal surfaces of the three cuneiforms and cuboid. Specifically, the first (most medial) metatarsal articulates with the medial cuneiform, the second with the intermediate cuneiform, and the third with the lateral cuneiform. The bases of the fourth and fifth metatarsals both articulate with the distal surface of the cuboid.
The articular surfaces of the tarsometatarsal joints are generally flat, although the medial two show slight, irregular curvatures. Dorsal, plantar, and interosseous ligaments add stability to these articulations. Only the first tarsometatarsal joint has a well-developed capsule.120
Kinematic Considerations: The tarsometatarsal joints serve as the base joints of the forefoot. Mobility is least at the second and third tarsometatarsal joints, in part because of strong ligaments and the wedged position of the base of the second ray between the medial and lateral cuneiforms (see Figure 14-35, B). Consequently, the second and third rays produce an element of longitudinal stability throughout the foot, similar to the second and third rays in the hand.67 This stability is useful in late stance as the forefoot prepares for the dynamics of push off.
Mobility is greatest in the first, fourth, and fifth tarsometatarsal joints, most notably in the first (most medial) joint.34 During walking, the first tarsometatarsal joint normally expresses about 10 degrees of sagittal plane movement; mobility in other planes is usually slight.23
During the early to mid-stance phase of walking, the first tarsometatarsal joint gradually dorsiflexes about 5 degrees. This motion occurs as body weight depresses the cuneiform region downward as the ground simultaneously pushes the distal end of the first ray upward. This movement is associated with a gradual lowering of the medial longitudinal arch37—a mechanism that helps absorb the stress of body weight acting on the foot. At late stance (push off) phase of gait, however, the first tarsometatarsal joint rapidly plantar flexes about 5 degrees.23 The plantar flexion of the first ray, controlled in part by pull of the fibularis longus, effectively “shortens” the medial column of the foot slightly, thereby helping to raise the medial longitudinal arch. This mechanism increases the stability of the arch (and medial column of the foot) at a time in the gait cycle when the midfoot and forefoot are under higher loads.
Although the descriptions are dated and still partially unresolved, most literature describes a natural mechanical coupling of the kinematics at the first tarsometatarsal joint: specifically, plantar flexion occurs with slight eversion, and dorsiflexion with slight inversion.37,45,68 Such passive mobility does indeed appear to occur naturally when assessed in a non–weight-bearing condition (Figure 14-36). These movement combinations are atypical, however, because they do not fit the standard definitions of pronation or supination. Nevertheless, the unique mobility at the first tarsometatarsal joint may provide useful functions. Combining plantar flexion and eversion, for example, allows the medial side of the foot to better conform around irregular surfaces on the ground (see Figure 14-35, C). (This motion of the first metatarsal is generally similar to the movement of the thumb metacarpal as the pronated hand attempts to grasp a large spherical object.) Exactly how these atypical movement combinations relate functionally to the overall kinematics of the foot during walking remains uncertain.
INTERMETATARSAL JOINTS
Structure and Function: Plantar, dorsal, and interosseous ligaments interconnect the bases of the four lateral metatarsals. These points of contact form three small intermetatarsal synovial joints. Although interconnected by ligaments, a true joint does not typically form between the bases of the first and second metatarsals. This lack of articulation increases the relative movement of the first ray, in a manner similar to the hand. Unlike in the hand, however, the deep transverse metatarsal ligaments interconnect the distal end of all five metatarsals. Slight motion at the intermetatarsal joints augments the flexibility at the tarsometatarsal joints.
METATARSOPHALANGEAL JOINTS
Anatomic Considerations: Five metatarsophalangeal joints are formed between the convex head of each metatarsal and the shallow concavity of the proximal end of each proximal phalanx (see Figure 14-23). These joints are located about 2.5 cm proximal to the “web spaces” of the toes. With the joints flexed, the prominent heads of the metatarsals are easily palpable on the dorsum of the distal foot.
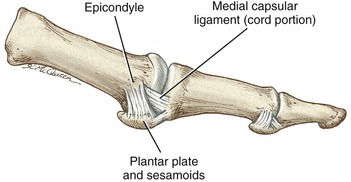
Articular cartilage covers the distal end of each metatarsal head (Figure 14-37). A pair of collateral ligaments spans each metatarsophalangeal joint, blending with and reinforcing the capsule. As in the hand, each collateral ligament courses obliquely from a dorsal-proximal to a plantar-distal direction, forming a thick cord portion and a fanlike accessory portion.
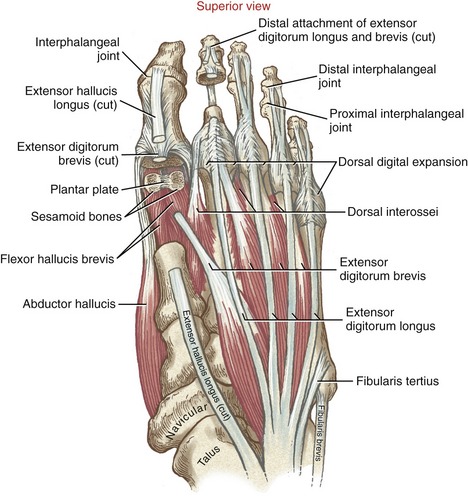
The accessory portion attaches to the thick, dense plantar plate, located on the plantar side of the joint. The plate, or ligament, is grooved for the passage of flexor tendons. Fibers from the deep plantar fascia attach to the plantar plates and sheaths of the flexor tendons. Two sesamoid bones located within the tendon of the flexor hallucis brevis rest against the plantar plate of the first metatarsophalangeal joint (Figure 14-38). Although not depicted in Figure 14-38, four deep transverse metatarsal ligaments blend with and join the adjacent plantar plates of all five metatarsophalangeal joints. By interconnecting all five plates, the transverse metatarsal ligaments help maintain the first ray in a similar plane as the lesser rays, thereby adapting the foot for propulsion and weight bearing rather than manipulation. In the hand, the deep transverse metacarpal ligament connects only the fingers, freeing the thumb for opposition.
Kinematic Considerations: Movement at the metatarsophalangeal joints occurs in two degrees of freedom. Extension (dorsiflexion) and flexion (plantar flexion) occur approximately in the sagittal plane about a medial-lateral axis; abduction and adduction occur in the horizontal plane about a vertical axis. The second digit serves as the reference digit for naming the movements of abduction and adduction of the toes. (The reference digit for naming abduction and adduction in the hand is the third or middle digit.) The axes of rotation for all volitional movements of the metatarsophalangeal joints are through the center of each metatarsal head.
Most people demonstrate limited dexterity in active movements at the metatarsophalangeal joints, especially in abduction and adduction. From a neutral position, the toes can be passively extended about 65 degrees and flexed about 30 to 40 degrees. The great toe typically allows greater extension, to near 85 degrees.131 This magnitude of extension is readily apparent as one stands up on “tiptoes.”
Deformities or Trauma Involving the Metatarsophalangeal Joint of the Great Toe:
Hallux Limitus: Hallux limitus, or “rigidus” in its less severe form, is primarily a posttraumatic condition characterized by gradual marked limitation of motion, articular degeneration, and pain at the metatarsophalangeal joint of the great toe. Although any trauma or sprain of the great toe can progress to hallux limitus, the mechanism of injury frequently involves forceful hyperextension of the metatarsophalangeal joint. More severe injuries may involve complete or incomplete tears of the plantar ligaments, capsule, and associated tendons, as well as fracture of the sesamoid bones.14
Injury caused by forced hyperextension of the great toe is often called “turf toe” and occurs relatively frequently in American football players. Historically, the term turf toe originated from the increase in this injury after the replacement of natural grass with artificial turf and the use of lighter-weight shoes.11 Regardless of the initiating trauma, a diagnosis of hallux limitus is often made if pain persists along with reduced range of extension, usually to less than 55 degrees.131 In some cases the condition will evolve to osteoarthritis; excessive osteophyte formation may then limit motion in all directions.
The impairments associated with hallux limitus can have significant impact on walking.131 Normally, walking requires about 65 degrees of extension at the first metatarsophalangeal joint as the heel rises at late stance phase. A person with hallux limitus may attempt to avoid extending the painful great toe during the late stance phase of walking. Often this is accomplished by walking on the outer surface of the affected foot, or by walking with the foot pointed outward and “rolling over” the medial arch of the foot.
Those affected may be advised to wear stiff-soled shoes (or stiff inserts placed within the shoes) and to avoid inclines or declines. Physical therapy has been shown to be effective in restoring range of motion and reducing pain.117 Surgery is often recommended in more severe cases.
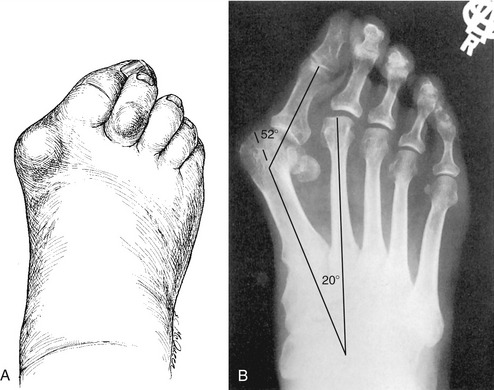
Hallux Valgus: The central feature of hallux valgus (or bunion) is a progressive lateral deviation of the great toe relative to the midline of the body. Although the deformity appears to involve primarily the metatarsophalangeal joint, the pathomechanics of hallux valgus typically involve the entire first ray (Figure 14-39, A and B). As depicted in the radiograph, hallux valgus is typically associated with excessive adduction of the first metatarsal (defined in this case relative to the body and not the second digit) about its tarsometatarsal joint.30 The adducted position of the first metatarsal can eventually lead to lateral dislocation of the metatarsophalangeal joint, thereby completely exposing the metatarsal head as a lump or “bunion.” The deformed metatarsophalangeal joint often becomes inflamed and painful. If the proximal phalanx laterally deviates in excess of about 30 degrees, the proximal phalanx often begins to evert about its long axis. The bunion deformity is also referred to as “hallux abducto-valgus” in order to account for the deviations in both horizontal and frontal planes.
The progressive axial rotation of the laterally deviated proximal phalanx of the hallux creates a muscular imbalance in the forces that normally align the metatarsophalangeal joint.2 The abductor hallucis muscle (normally located medial to the first metatarsophalangeal joint) may gradually shift toward the plantar side of the joint. The subsequent unopposed pull of the adductor hallucis and lateral head of the flexor hallucis brevis progressively increases the lateral deviation posture of the proximal phalanx. In time, the overstretched medial collateral ligament and capsule may weaken or rupture, removing an important source of reinforcement to the medial side of the joint. Persons with marked hallux valgus may avoid bearing weight over the first metatarsophalangeal joint, causing the lateral metatarsal bones to accept a greater proportion of the load. The pathomechanics of marked hallux valgus involve a zigzag-like collapse of the first ray, similar to the “ulnar drift” of the metacarpophalangeal joint in the hand with rheumatoid arthritis (see Chapter 8).
INTERPHALANGEAL JOINTS
All interphalangeal joints of the foot possess similar anatomic features. The joint consists of the convex head of the more proximal phalanx articulating with the concave base of the more distal phalanx. The proximal phalanx of the second toe is removed in Figure 14-38 to expose the concave side of the proximal interphalangeal joint. The structure and function of the connective tissues at the interphalangeal joints are generally similar to those described for the metatarsophalangeal joints. Collateral ligaments, plantar plates, and capsules are present but smaller and less defined.
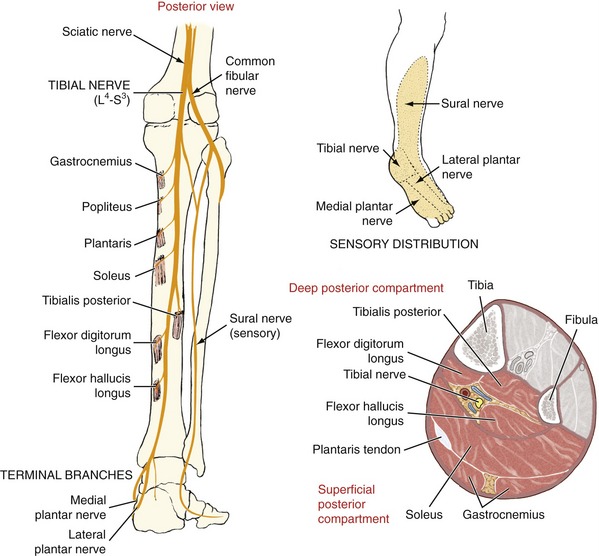
ACTION OF THE JOINTS WITHIN THE FOREFOOT DURING THE LATE STANCE PHASE OF GAIT
During the end of the stance phase, the midfoot and forefoot must become relatively stable to accept the stress associated with push off. In addition to activation of local intrinsic and extrinsic muscles, a rising of the medial longitudinal arch further stabilizes the foot. Although the rise of the arch is highly variable, it averages 6 mm during the push off phase.114 The primary mechanism used to lift the arch has been historically described as the “windlass effect,” which is demonstrated by standing on tiptoes (Figure 14-40, A). Because of the attachments of the deep plantar fascia to the proximal phalanges, full extension of the metatarsophalangeal joints increases the tension throughout the medial longitudinal arch. In theory, the increased tension raises and stabilizes the arch. As the heel and most of the foot are lifted, body weight shifts anteriorly toward the more medial metatarsal heads. Local fat pads reduce potentially damaging stress to the bone, and the sesamoid bones protect the long flexor tendon of the great toe. Once stabilized by the stretched plantar fascia and a reinforced arch, the second and third rays act as rigid levers capable of withstanding the potentially large bending moments created by the contracting gastrocnemius and soleus muscles. The tensile force within the stretched plantar fascia during very late stance phase has been estimated to be near 100% of body weight.26 Failure of the plantar fascia to transmit this force from the calcaneus to the base of the toes would limit the effectiveness of the windlass mechanism in raising the arch. This, indeed, is often observed by noting the guarded or ineffective manner of “push off” in a person who has had a plantar fasciotomy or is experiencing painful plantar fasciitis.
In contrast to the healthy foot, consider the pathomechanics involved as a person with an unstable “flat foot” (pes planus) attempts to rise up on tiptoes (see Figure 14-40, B). Although the individual has no neuromuscular pathology, there is significant loss in the lift of the heel, even on maximal muscular effort. Without an effective medial longitudinal arch, the unstable, unlocked midfoot and forefoot sag under body weight. This typically causes a movement toward dorsiflexion of the tarsometatarsal joints (in contrast to normal slight plantar flexion). This kinematic response may stretch the extrinsic toe flexor muscles and, if significant, limit toe extension. Regardless of the specific cause-and-effect relationship, the reduced extension of the metatarsophalangeal joints reduces the effectiveness of the windlass effect for stabilizing the foot.
The final section on kinematics closes with Table 14-6, which summarizes the important functions of the ankle and foot during the entire stance phase of walking.
MUSCLE AND JOINT INTERACTION
Innervation of Muscles and Joints
INNERVATION OF MUSCLES
The extrinsic muscles are arranged in three compartments of the leg: anterior, lateral, and posterior. A different motor nerve innervates the muscles within each compartment (see cross-sections in Figures 14-41 and 14-42). Each motor nerve is a branch of the sciatic nerve, formed from the L4-S3 spinal nerve roots of the sacral plexus.
Lateral to the head of the fibula, the common fibular (peroneal) nerve (L4-S2) divides into a deep and superficial branch (see Figure 14-41). The deep branch of the fibular nerve innervates the muscles within the anterior compartment: the tibialis anterior, extensor digitorum longus, extensor hallucis longus, and fibularis (peroneus) tertius. The deep branch continues distally to innervate the extensor digitorum brevis (an intrinsic muscle located within the dorsum of the foot). It also supplies sensory innervation to a triangular area of skin in the web space between the first and second toes. The superficial branch of the fibular nerve innervates the fibularis longus and fibularis brevis within the lateral compartment. The nerve then continues distally as a sensory nerve to much of the skin on the dorsal and lateral aspects of the leg and foot.
The tibial nerve (L4-S3) and its terminal branches innervate the remainder of the extrinsic and intrinsic muscles of the foot and ankle (see Figure 14-42). The muscles within the posterior compartment are divided into superficial and deep sets. The superficial set includes the calf muscles: the gastrocnemius and soleus (together known as the triceps surae) and the small plantaris. The deep set includes the tibialis posterior, flexor hallucis longus, and flexor digitorum longus. As the tibial nerve approaches the medial side of the ankle, it sends a sensory branch to the skin over the heel.
The spinal nerve roots that supply the muscles of the lower extremity are listed in Appendix IV, Part A. Part B of this appendix lists key muscles typically used to test the functional status of the L2-S3 spinal nerve roots. Part C shows a dermatome map of the lower extremity.
SENSORY INNERVATION OF THE JOINTS
The talocrural joint receives sensory innervation from the deep branch of the fibular nerve. In general, the sensory innervation to the other joints of the foot is supplied by nerve branches that cross the region. Each major joint receives multiple sources of sensory innervation, traveling to the spinal cord primarily through S1 and S2 nerve roots.120
Anatomy and Function of the Muscles
The muscles of the ankle and foot not only control the specific actions of the underlying joints, but also provide the stability, thrust, and shock absorption necessary for locomotion. Both intrinsic and extrinsic muscles perform these functions. Additional discussion of the muscular interactions during walking follows in Chapter 15.
Because all extrinsic muscles cross multiple joints, they possess multiple actions. Many of these actions are evident by noting where the tendons cross the axes of rotation at the talocrural and subtalar joints (Figure 14-43). Although Figure 14-43 is oversimplified (by lacking the transverse tarsal joint as well as other components of pronation and supination of the foot), it can nevertheless serve as a useful guide to understanding many of the actions of the extrinsic muscles.
EXTRINSIC MUSCLES
Anatomy: The four muscles of the anterior compartment are listed in the box. As a group, these “pretibial” muscles have their proximal attachments on the anterior and lateral aspects of the proximal half of the tibia, the adjacent fibula, and the interosseous membrane (Figure 14-44). The tendons of these muscles cross the dorsal side of the ankle, restrained by a synovial-lined superior and inferior extensor retinaculum. Located most medially is the prominent tendon of the tibialis anterior, coursing distally to attach to the medial-plantar surface of the first tarsometatarsal joint (Figure 14-45). The tendon of the extensor hallucis longus passes just lateral to the tendon of the tibialis anterior as it courses toward the dorsal surface of the great toe (see Figure 14-44). Progressing laterally across the dorsum of the ankle are the tendons of the extensor digitorum longus and the fibularis tertius (or “third” fibularis muscle). The four tendons of the extensor digitorum longus attach to the dorsal surface of the middle and distal phalanges via the dorsal digital expansion. The fibularis tertius is part of the extensor digitorum longus muscle and may be considered as this muscle’s fifth tendon. The fibularis tertius attaches to the base of the fifth metatarsal bone.140
Joint Action: All four pretibial muscles are dorsiflexors because they cross anterior to the axis of rotation at the talocrural joint (see Figure 14-43). From the anatomic position, the tibialis anterior also inverts the subtalar joint by passing just medial to the axis of rotation. The tibialis anterior inverts and adducts the talonavicular joint, as well as providing secondary support to the medial longitudinal arch.
The pretibial muscles are most active during the early stance phase and again throughout the entire swing phase of gait (see Figure 15-29, tibialis anterior). During early stance, the muscles are eccentrically active to control the rate of plantar flexion (i.e., the period between heel contact and foot flat; see Figure 14-19). Controlled plantar flexion is necessary for a soft landing of the foot. Through similar eccentric activation, the tibialis anterior helps to decelerate the lowering of the medial longitudinal arch and therefore indirectly helps to control pronation (eversion) of the rearfoot (review Figure 14-31). During the swing phase, the pretibial muscles actively dorsiflex the ankle and extend the toes to ensure that the foot clears the ground.
Anatomy: The fibularis longus and the fibularis brevis muscles (formerly called the peroneus longus and peroneus brevis, respectively) occupy the lateral compartment of the leg muscles (Figure 14-46). Both muscles attach proximally along the lateral fibula. The tendon of the fibularis longus, the more superficial of the two, courses distally a remarkable distance. After wrapping around the posterior side of the lateral malleolus, the tendon enters the plantar side of the foot through a groove in the cuboid bone. The tendon then travels between the long and short plantar ligaments to its final distal attachment on the plantar-lateral aspect of the first tarsometatarsal joint (see Figure 14-45). It is noteworthy that the fibularis longus and tibialis anterior attach on either side of the plantar surface first tarsometatarsal joint. This pair of muscles therefore provides kinetic stability to the base of the first ray.
The tendon of the fibularis brevis travels posterior to the lateral malleolus alongside the fibularis longus. Both fibular tendons occupy the same synovial sheath as they pass under the fibular retinaculum (see Figure 14-46). Just distal to the retinaculum, the tendon of the fibularis brevis separates from the fibularis longus tendon and courses toward its distal attachment on the styloid process of the fifth metatarsal. Frequently observed in dancers, the styloid process may experience an avulsion fracture after a very strong contraction of the fibularis brevis, often in response to a sudden and extreme inversion movement of the ankle or foot.
Joint Action: The fibularis longus and fibularis brevis muscles are the primary evertors of the foot (see Figure 14-43). These muscles provide the main source of active stability to the lateral side of the ankle. For this reason, strengthening, conditioning, and coordination exercises involving these muscles are often designed for persons who may be vulnerable to inversion sprains of the ankle, such as athletes playing basketball or volleyball. Of interest, although these lateral muscles are very effective at resisting inversion, a purely reflexive muscular contraction in response to an unexpected inversion movement is typically too slow to prevent injury.62 Other, more complex neuromuscular mechanisms are required for this protection, likely those involving feed-forward or anticipatory responses to an impending inversion injury.
The fibularis longus and brevis have substantial moment arms for eversion across the subtalar joint—over 2 cm.60 The lateral malleolus, serving as a fixed pulley, routes the fibular tendons posterior to the axis of rotation at the talocrural joint.60 Both muscles therefore are also plantar flexors of the talocrural joint. Although not evident in Figure 14-43, the fibularis longus and brevis also abduct the subtalar and transverse tarsal joints.
The distal attachment of the fibularis longus generates eversion torque as far anterior as the forefoot. This is evident as the base of the first ray everts and depresses (plantar flexes) slightly during maximal-effort pronation of the unloaded foot. In addition, the fibularis longus stabilizes the first tarsometatarsal joint against the potent medial pull of the tibialis anterior. Without this stability, the first ray may migrate medially, predisposing a person to a hallux valgus deformity.30
The fibularis longus and brevis are most active throughout the middle and late stance phases of walking.111,123 During most of this time, the subtalar joint is supinating (inverting) as the dorsiflexing talocrural joint rapidly changes its direction to plantar flexion (review Figures 14-19 and 14-31). An important function of the fibularis muscles during this phase of walking is to decelerate, and thus control, the rate and extent of the supinating subtalar joint. Furthermore, the active force within the fibularis longus helps to fixate the first ray securely to the ground, an action demonstrated by the forefoot in Figure 14-33. With weakness, paralysis, or inhibition of the fibularis longus, the potent supination pull of the tibialis posterior on the forefoot is unopposed. As a result, the forefoot follows the rearfoot into supination, causing the person to walk on the lateral border of the foot, possibly increasing the likelihood of an inversion sprain.
At very late stance phase, during push off, the fibularis longus and brevis muscles assist other muscles with plantar flexion at the talocrural joint. The lateral position of the fibularis muscles helps neutralize the strong inversion (supination) bias of the remaining active plantar flexors, including the tibialis posterior, and, to a limited degree, the gastrocnemius. The necessity for balance of these muscle forces is shown as a subject stands on tiptoes in Figure 14-47. As the heel rises, the strongly activated fibularis longus and tibialis posterior muscles neutralize each other as they form a functional “sling” that supports the transverse and medial longitudinal arches. The net effect of this muscle interaction slightly supinates the unloaded rearfoot, which provides further stability to the medial longitudinal arch and more distal regions of the foot. This stability ensures that the plantar flexion torque required to stand on tiptoes (or propel the body upward and forward) is effectively transferred distally through the foot, toward the metatarsal heads.
Posterior Compartment Muscles:
Anatomy: The muscles of the posterior compartment are divided into two groups. The superficial group includes the gastrocnemius, soleus (together known as the triceps surae), and plantaris (Figure 14-48). The deep group includes the tibialis posterior, flexor digitorum longus, and flexor hallucis longus (Figure 14-49).
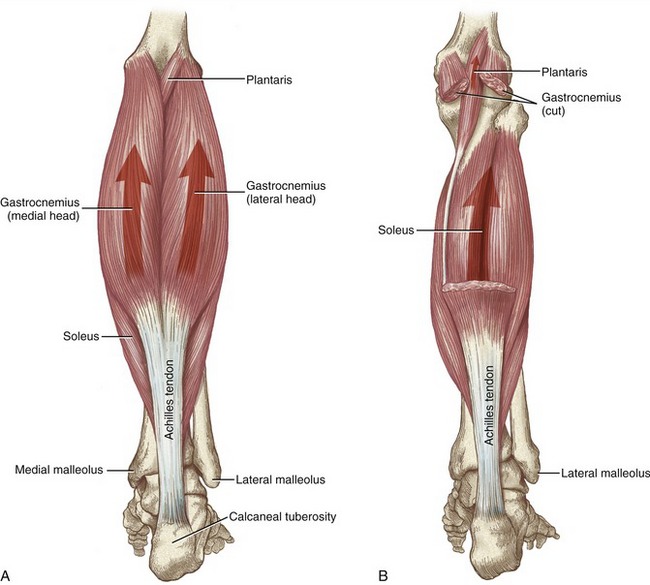
FIGURE 14-48. The superficial muscles of the posterior compartment of the right leg are shown: A, gastrocnemius; B, soleus and plantaris.
Superficial Group: The gastrocnemius muscle forms the prominent belly of the calf. This two-headed muscle attaches by separate heads from the posterior side of the medial and lateral femoral condyles. The larger, medial head joins the lateral head midway down the leg to form a tendinous expansion that, after insertion of the tendon from the soleus muscle, forms the Achilles tendon. The broad flat soleus muscle lies deep to the gastrocnemius, arising primarily from the posterior side of the proximal fibula and middle tibia. Like the gastrocnemius, the soleus blends with the Achilles tendon for its distal attachment to the calcaneal tuberosity. The soleus is a very thick muscle, approximately twice the cross-sectional area as the overlying gastrocnemius.139 The gastrocnemius crosses the knee but the soleus does not.
The plantaris muscle arises from the lateral supracondylar line of the femur. The fusiform muscle belly is only 7 to 10 cm long,120 unusually small compared with the other muscles in the area. The plantaris has a very long, slender tendon that courses between the gastrocnemius and soleus, eventually fusing with the medial margin of the Achilles tendon.
Deep Group: The tibialis posterior, flexor hallucis longus, and flexor digitorum longus muscles are located deep to the soleus muscle (see Figure 14-49). As a group, these muscles arise from the posterior side of the tibia, fibula, and interosseous membrane. The more centrally located tibialis posterior muscle is framed and partially covered by the flexor hallucis longus laterally and the flexor digitorum longus medially. At their distal musculotendinous junctions, all three muscles enter the plantar aspect of the foot from its medial side (see Figure 14-45). The position of the tendons as they cross the ankle and foot explains the strong supination (inversion) component of these muscles, most notably the tibialis posterior (see Figure 14-43).60 The tibialis posterior, flexor digitorum longus, and tibial neurovascular bundle course through the tarsal tunnel, located just deep to the flexor retinaculum (Figure 14-50). The tarsal tunnel is analogous to the carpal tunnel in the wrist. “Tarsal tunnel syndrome” (analogous to carpal tunnel syndrome) is characterized by entrapment of the tibial nerve beneath the flexor retinaculum and subsequent paresthesia over the plantar aspect of the foot.
The tendon of the flexor hallucis longus courses distally through the ankle in a groove formed between the tubercles of the talus and the inferior edge of the sustentaculum talus (see Figure 14-12). Fibrous bands convert this groove into a synovial-lined canal, anchoring the position of the tendon. The deeper (lateral) position of the tendon relative to the tibialis posterior and flexor digitorum longus explains why the flexor hallucis longus is not a structure within the tarsal tunnel. Once in the plantar aspect of the foot, the tendon of the flexor hallucis longus courses between the two sesamoid bones of the first metatarsophalangeal joint, finally attaching to the plantar side of the base of the distal phalanx of the great toe (see Figure 14-45).
The tendon of the flexor digitorum longus courses distally across the ankle posterior to the medial malleolus. At about the level of the base of the metatarsals, the main tendon of the flexor digitorum longus divides into four smaller tendons, each attaching to the base of the distal phalanx of the lesser toes (see Figure 14-45).
The tendon of the tibialis posterior muscle lies just anterior to the tendon of the flexor digitorum longus in a shared groove on the posterior side of the medial malleolus (see Figure 14-50). The tendon of the tibialis posterior continues distally and passes deep to the flexor retinaculum but superficial to the deltoid ligament. At this point the tendon divides into superficial and deep parts, establishing attachments to every tarsal bone, except the talus, and to the bases of several of the more central metatarsals (see Figure 14-45). The most prominent distal attachment of the tibialis posterior is on the navicular tuberosity. The tendon is usually palpable for several centimeters just proximal to the navicular tuberosity during resisted adduction and inversion of the foot.
The main tendon of the tibialis posterior provides direct mechanical support to the adjacent spring ligament, thereby adding significant stability to the medial longitudinal arch.87 A ruptured or overstretched tibialis posterior tendon typically results in the collapse of the medial longitudinal arch, with an associated drop in the height of the talus.64,129
The tendons of both the tibialis posterior and the flexor digitorum longus use the medial malleolus as a fixed pulley to direct their force posterior to the axis of rotation at the talocrural joint.60 An analogous pulley exists for the fibularis longus and brevis tendons, as these structures pass posterior to the lateral malleolus (see Figure 14-46). Tendons of the tibialis posterior and flexor digitorum longus are positioned posterior to the medial malleolus by the flexor retinaculum. The flexor hallucis longus uses a different plantar flexion pulley system, formed proximally by the medial and lateral tubercles of the talus and distally by the sustentaculum talus of the calcaneus.
Joint Action: With the exception of the fibularis longus and brevis, all muscles that plantar flex the talocrural joint also supinate (invert) the subtalar or transverse tarsal joints. This strong inversion bias is evidenced by the position of all muscles within the posterior compartment of the leg relative to the subtalar joint (see Figure 14-43). From the anatomic position, even the triceps surae inverts slightly, as the force of the Achilles tendon passes just medial to the subtalar joint’s axis of rotation.60
The tibialis posterior, flexor hallucis longus, and flexor digitorum longus are the primary supinators of the foot. The tibialis posterior likely produces the greatest supination torque (especially in the direction of adduction) across the subtalar and transverse tarsal joints.31,60,65 The muscle’s extensive distal attachments, especially to the navicular, provide an effective inversion “twist” of the midfoot (see Figure 14-26, D). In addition to plantar flexion and supination, the flexor digitorum longus and flexor hallucis longus have additional actions at the more distal joints of the foot, especially at the metatarsophalangeal and interphalangeal joints.
Activation of the Plantar Flexor and Supinator Muscles during Walking: The plantar flexor and supinator muscles are active throughout most of the stance phase of gait, particularly between foot flat and toe off phases (see activation of the gastrocnemius and soleus, for example, in Figure 15-29).123,124 These muscles become active immediately after the dorsiflexor muscles relax. From foot flat to just before heel off, the plantar flexors act eccentrically to decelerate the forward rotation (dorsiflexion) of the leg over the fixed talus.50,93 Between the heel off and toe off phases, however, the muscles switch to a concentric activation to assist with the necessary thrust for push off and early swing phase. Furthermore, active forces in the flexor hallucis longus, flexor digitorum longus, and intrinsic foot muscles (lumbricals and interossei) hold the plantar surface of the extending toes firmly against the ground. This action expands the weight-bearing surfaces of the toes, thereby minimizing contact pressures.
The tibialis posterior, flexor hallucis longus, and flexor digitorum longus muscles are all capable of resisting pronation and assisting with supination during the stance phase of walking. Of the three muscles, however, the tibialis posterior is most designed for this function.4,31,64 EMG studies show that the tibialis posterior is active during the stance phase longer than any other supinator muscle, from just before foot flat through heel off phase.123 As the entire foot contacts the ground, the tibialis posterior decelerates the pronating rearfoot, which assists with a gradual and controlled lowering of the medial longitudinal arch (review Figure 14-31). Through this eccentric action, the tibialis posterior absorbs some of the impact of loading. Persons who excessively and/or rapidly pronate during the stance phase may place excessive braking (decelerating) demands on the tibialis posterior, possibly leading to tendinopathy, muscle fatigue, or stress-related anterior leg pain (more generically known as “shin splints”).110 It is not always certain whether excessive pronation causes or results from tibialis posterior dysfunction.64,129 In either scenario, reduced function of the tibialis posterior limits an important shock absorption mechanism of the foot.
Plantar Flexion Torque Generated for Propulsion: At the very end of stance phase, the muscles within the posterior compartment concentrically contract to plantar flex the talocrural joint. The fibularis longus and brevis (within the lateral compartment) also contribute to this torque. The amount of muscular activity produced by the plantar flexor muscles during push off depends strongly on the speed and vigor of walking. Although these muscles provide the primary propulsive force for walking, secondary energy sources may include the ipsilateral hip extensors (generated at early stance) and the ipsilateral hip flexors (generated at very late stance).16,106
In healthy persons, maximal isometric plantar flexion torque exceeds the torque potential of all other movements about the ankle and foot combined (Figure 14-51).41,100,116 Such a large plantar flexion torque reserve is needed to rapidly accelerate the body up and forward during brisk walking, running, jumping, and climbing. Plantar flexion torque is greatest when the ankle approaches full dorsiflexion (i.e., when plantar flexor muscles are elongated) and is least when the ankle is fully plantar flexed.99 The ankle is typically dorsiflexed as one prepares to sprint or jump. Of interest, as the ankle vigorously plantar flexes at the “take off” of a sprint or jump, the contracting gastrocnemius is simultaneously elongated by the action of the extending knee. This biarticular arrangement prevents the gastrocnemius from overshortening, allowing greater torques throughout a larger range of ankle motion.52 Because the soleus muscle does not cross the knee, its length-tension relationship is unaffected by the position of the knee. The relative slow-twitch muscle characteristics of the soleus are more suited to control the slow and subtle postural sway movements of the leg over the talus during standing. The faster-twitch characteristics of the gastrocnemius, on the other hand, are apparently better suited for providing a propulsive plantar flexion torque for activities that also involve dynamic knee extension, such as jumping and sprinting.
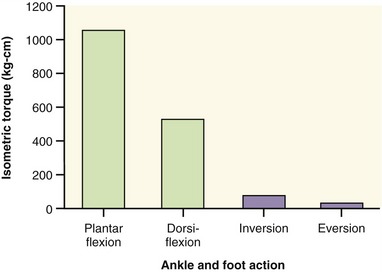
FIGURE 14-51. The magnitude of maximal-effort isometric torque is shown for four actions of the ankle and foot. (N = 86 healthy men and women.)116
Of all the plantar flexor muscles, the gastrocnemius and soleus are by far the most powerful, theoretically capable of producing about 80% of the total plantar flexion torque at the ankle.93 The large torque potential of the triceps surae results in part from the muscles’ large cross-sectional area and relatively long moment arm. The protruding calcaneal tuberosity provides the triceps surae with a moment arm of about 5.3 cm from the talocrural joint, nearly twice the average moment arm of the other plantar flexor muscles.60
MUSCULAR PARALYSIS AFTER INJURY TO THE FIBULAR OR TIBIAL NERVE
Injury to the Common Fibular Nerve and Its Branches: The common fibular nerve winds around the neck of the fibula, just deep to the fibularis longus. This nerve is injured relatively frequently from lacerations or trauma that involves a fractured proximal fibula. Injury to the deep branch of the fibular nerve can result in paralysis of all the dorsiflexor (pretibial) muscles (see Figure 14-41). With paralysis of the dorsiflexor muscles, the foot rapidly and uncontrollably plantar flexes immediately after the heel contact phase of walking. During the swing phase, the hip and knee must excessively flex to ensure that the toes clear the ground.
An injury to the superficial branch of the fibular nerve may result in paralysis of the fibularis longus and fibularis brevis (see Figure 14-41). Over time, paralysis may lead to a supinated or inverted posture of the foot, a condition called pes varus. An injury to the common fibular nerve may involve both deep and superficial nerve branches. The resulting paralysis of all dorsiflexor and evertor muscles strongly predisposes a person to a deformity of combined plantar flexion of the ankle and supination of the foot, a condition referred to as pes equinovarus.
Injury to the Tibial Nerve and Its Branches: Injury to the tibial nerve may cause varying levels of weakness or paralysis in the muscles of the posterior compartment (see Figure 14-42). Isolated paralysis of the gastrocnemius and soleus because of tibial nerve injury is rare. Nevertheless, regardless of underlying pathology, paralysis of these muscles results in profound loss of plantar flexion torque. Over time, a fixed dorsiflexion posture may result at the talocrural joint, a condition known as pes calcaneus. The term calcaneus is used to describe the often prominent heel pad that forms in response to the heel of the chronically dorsiflexed ankle sharply striking the ground at the initiation of the stance phase.
Injury to the tibial nerve within the leg typically involves the more distal medial and lateral plantar nerves (see Figure 14-42). Paralysis of the intrinsic muscles within the foot often results in a “clawing” of the toes: hyperextension of the metatarsophalangeal joints with flexion of the interphalangeal joints. This deformity results primarily from an unopposed pull of the extrinsic toe extensor muscles across the metatarsophalangeal joints. The pathomechanics of clawing caused by weakness of the intrinsic muscles of the foot are similar to those of clawing of the fingers after a combined ulnar and median nerve injury (see Chapter 8).
The common fixed deformities or abnormal postures of the ankle, foot, and toes are summarized according to nerve injury in Table 14-7.
INTRINSIC MUSCLES
Anatomic and Functional Considerations: Intrinsic muscles are those that originate and insert within the foot. The following discussion highlights the primary attachments and actions of the intrinsic muscles. More detailed attachments of these muscles is presented in Appendix IV, Part D.
The dorsum of the foot has one intrinsic muscle, the extensor digitorum brevis, which is innervated by the deep branch of the fibular nerve. The extensor digitorum brevis originates on the dorsal-lateral surface of the calcaneus, just proximal to the calcaneocuboid articulation. The muscle belly sends four tendons: one to the dorsal surface of the great toe (often designated as the extensor hallucis brevis), and three that join the tendons of the extensor digitorum longus of the second through the fourth toes (see Figure 14-44). The extensor digitorum brevis assists the extensor hallucis longus and extensor digitorum longus in extension of the toes.
The remaining intrinsic muscles originate and insert within the plantar aspect of the foot. These muscles are organized into four layers (Figure 14-53). The plantar fascia is located just superficial to the first layer of muscles.
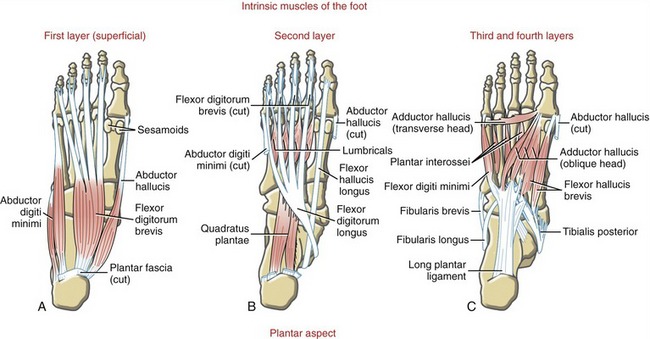
FIGURE 14-53. The intrinsic muscles of the plantar aspect of the foot are organized into four layers.
Layer 1: The intrinsic muscles in the first layer of the foot are the flexor digitorum brevis, abductor hallucis, and abductor digiti minimi (see Figure 14-53, A). As a group, these muscles originate on the lateral and medial processes of the calcaneal tuberosity and nearby connective tissues. The flexor digitorum brevis attaches to both sides of the plantar aspect of the middle phalanges of the four lesser toes. Proximal to this distal attachment, each tendon divides to allow passage of the tendons of the flexor digitorum longus. (Note the similar relationship between the flexor digitorum superficialis and profundus of the hand.) The flexor digitorum brevis assists the flexor digitorum longus with flexing the toes. The abductor hallucis forms the medial border of the foot, providing a covered passage for the nerves that enter the plantar aspect of the foot. The abductor muscle attaches distally to the medial border of the proximal phalanx of the great toe, sharing an attachment with the medial head of the flexor hallucis brevis (see Figure 14-53, C). The abductor digiti minimi helps form the lateral-plantar margin of the foot, attaching distally to the lateral border of the base of the proximal phalanx of the fifth toe. Each muscle abducts and assists with flexion of its respective digit.
Layer 2: The intrinsic muscles in the second layer are the quadratus plantae and the lumbricals (see Figure 14-53, B). Both muscles are anatomically related to the tendons of the flexor digitorum longus. The quadratus plantae (flexor digitorum accessorius) attaches by two heads to the plantar aspect of the calcaneus. Both heads attach distally to the lateral edge of the common tendon of the flexor digitorum longus. The quadratus plantae helps to stabilize the tendons of the flexor digitorum longus, preventing them from migrating medially.72 The four lumbricals have their proximal attachment from the tendons of the flexor digitorum longus. These small fleshy muscles pass on the medial side of the lesser toes to attach into the extensor digital expansion. The lumbricals flex the metatarsophalangeal joints and extend the interphalangeal joints—actions that are functionally equivalent to the actions performed by the lumbricals of the hand.
Layer 3: The intrinsic muscles in the third layer are the adductor hallucis, flexor hallucis brevis, and flexor digiti minimi (see Figure 14-53, C). As a group, these short muscles arise from the plantar aspect of the cuboid, cuneiforms, and bases of more central metatarsal bones, and from local connective tissues. Similar to the adductor pollicis in the hand, the adductor hallucis arises from two heads: oblique and transverse. Both heads attach to the lateral base of the proximal phalanx of the great toe and adjacent lateral sesamoid bone.101 The muscle adducts and assists with flexion of the metatarsophalangeal joint of the great toe. The flexor hallucis brevis has two heads that attach distally to the medial and lateral sides of the base of the proximal phalanx of the great toe. Medial and lateral sesamoid bones are located within the two tendons of this muscle, providing greater leverage for the production of toe flexion torque.1 The flexor digiti minimi attaches to the lateral base of the proximal phalanx of the fifth toe, sharing a common attachment with the abductor digiti minimi. Both short flexor muscles flex the metatarsophalangeal joint of their respective toes.
Layer 4: The fourth layer of intrinsic muscles contains three plantar and four dorsal interossei muscles. The plantar interossei are shown in Figure 14-53, C, along with the muscles of the third layer. The dorsal interossei are illustrated in Figure 14-38. The overall plan of the interossei is nearly identical to that of the hand, except that the “reference digit” for abduction and adduction of the toes is the second instead of the third digit as in the hand.
The dorsal interossei are two-headed, bipennate muscles. The second digit contains two dorsal interossei, whereas the third and fourth digits contain one each. All dorsal interossei insert on the base of the proximal phalanges; the first and second interossei insert on the medial and lateral side of the second digit, respectively, and the third and fourth dorsal interossei insert on the lateral side of the third and fourth digit (review attachments in Figure 14-4). Each dorsal interosseus muscle abducts the metatarsophalangeal joint. Each of the third, fourth, and fifth digits contains a plantar interosseus muscle. Each muscle consists of one head and inserts on the medial side of the base of the corresponding proximal phalanx (review attachments in Figure 14-5). These muscles adduct their respective metatarsophalangeal joint.
The actions assigned to each of the intrinsic muscles assume the foot is unloaded and the toes are free to move. Although these unique actions allow the clinician to test the strength and dexterity of these muscles, the actions are not very relevant functionally. The intrinsic muscles of the foot are used less for manual dexterity, such as in the hand, and more for assisting with standing and walking balance and, most notably, providing structural stability to the foot and the medial longitudinal arch during the push off phase of walking. These functions explain why most of the intrinsic muscles are maximally active during late stance, just as the heel is rising off the floor.52
Most of the intrinsic muscles of the foot are anatomically analogous to an intrinsic muscle of the hand. One exception, however, is that the foot does not contain muscles that perform opposition of the first and fifth digits. Understanding these analogies should help with learning the anatomy, innervation, and action of these muscles. Table 14-8 summarizes the relevant information on the intrinsic muscles of the foot.
REFERENCES
1. Aper, RL, Saltzman, CL, Brown, TD. The effect of hallux sesamoid excision on the flexor hallucis longus moment arm. Clin Orthop Relat Res. 1996;325:209–217.
2. Arinci Incel, N, Genc, H, Erdem, HR, Yorgancioglu, ZR. Muscle imbalance in hallux valgus: an electromyographic study. Am J Phys Med Rehabil. 2003;82:345–349.
3. Arnold, AS, Anderson, FC, Pandy, MG, Delp, SL. Muscular contributions to hip and knee extension during the single limb stance phase of normal gait: a framework for investigating the causes of crouch gait. J Biomech. 2005;38:2181–2189.
4. Basmajian, JV, Stecko, G. The role of muscles in arch support of the foot. J Bone Joint Surg Am. 1963;45:1184–1190.
5. Beimers, L, Tuijthof, GJ, Blankevoort, L, et al. In-vivo range of motion of the subtalar joint using computed tomography. J Biomech. 2008;41:1390–1397.
6. Beumer, A, van Hemert, WL, Swierstra, BA, et al. A biomechanical evaluation of the tibiofibular and tibiotalar ligaments of the ankle. Foot Ankle Int. 2003;24:426–429.
7. Beynnon, BD, Vacek, PM, Murphy, D, et al. First-time inversion ankle ligament trauma: the effects of sex, level of competition, and sport on the incidence of injury. Am J Sports Med. 2005;33:1485–1491.
8. Jones, MH, Amendola, AS. Acute treatment of inversion ankle sprains: immobilization versus functional treatment. Clin Orthop Relat Res. 2007;455:169–172.
9. Blackwood, CB, Yuen, TJ, Sangeorzan, BJ, Ledoux, WR. The midtarsal joint locking mechanism. Foot Ankle Int. 2005;26:1074–1080.
10. Boone, DC, Azen, SP. Normal range of motion of joints in male subjects. J Bone Joint Surg Am. 1979;61:756–759.
11. Bowers, KD, Jr., Martin, RB. Turf-toe: a shoe-surface related football injury. Med Sci Sports. 1976;8:81–83.
12. Boytim, MJ, Fischer, DA, Neumann, L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19:294–298.
13. Bozkurt, M, Tonuk, E, Elhan, A, et al. Axial rotation and mediolateral translation of the fibula during passive plantarflexion. Foot Ankle Int. 2008;29:502–507.
14. Bronner, S, Novella, T, Becica, L. Management of a delayed-union sesamoid fracture in a dancer. J Orthop Sports Phys Ther. 2007;37:529–540.
15. Buchanan, KR, Davis, I. The relationship between forefoot, midfoot, and rearfoot static alignment in pain-free individuals. J Orthop Sports Phys Ther. 2005;35:559–566.
16. Buczek, FL, Cooney, KM, Walker, MR, et al. Performance of an inverted pendulum model directly applied to normal human gait. Clin Biomech (Bristol, Avon). 2006;21:288–296.
17. Bullock-Saxton, JE. Local sensation changes and altered hip muscle function following severe ankle sprain. Phys Ther. 1994;74:17–28.
18. Calhoun, JH, Li, F, Ledbetter, BR, Viegas, SF. A comprehensive study of pressure distribution in the ankle joint with inversion and eversion. Foot Ankle Int. 1994;15:125–133.
19. Cashmere, T, Smith, R, Hunt, A. Medial longitudinal arch of the foot: stationary versus walking measures. Foot Ankle Int. 1999;20:112–118.
20. Cavanagh, PR, Rodgers, MM, Iiboshi, A. Pressure distribution under symptom-free feet during barefoot standing. Foot Ankle. 1987;7:262–276.
21. Colville, MR, Marder, RA, Boyle, JJ, Zarins, B. Strain measurement in lateral ankle ligaments. Am J Sports Med. 1990;18:196–200.
22. Corazza, F, Stagni, R, Castelli, VP, Leardini, A. Articular contact at the tibiotalar joint in passive flexion. J Biomech. 2005;38:1205–1212.
23. Cornwall, MW, McPoil, TG. Motion of the calcaneus, navicular, and first metatarsal during the stance phase of walking. J Am Podiatr Med Assoc. 2002;92:67–76.
24. Cornwall, MW, McPoil, TG. Three-dimensional movement of the foot during the stance phase of walking. J Am Podiatr Med Assoc. 1999;89:56–66.
25. Cowan, DN, Jones, BH, Robinson, JR. Foot morphologic characteristics and risk of exercise-related injury. Arch Fam Med. 1993;2:773–777.
26. Erdemir, A, Hamel, AJ, Fauth, AR, et al. Dynamic loading of the plantar aponeurosis in walking. J Bone Joint Surg Am. 2004;86:546–552.
27. Esterman, A, Pilotto, L. Foot shape and its effect on functioning in Royal Australian Air Force recruits. Part 1: prospective cohort study. Mil Med. 2005;170:623–628.
28. Evans, T, Hertel, J, Sebastianelli, W. Bilateral deficits in postural control following lateral ankle sprain. Foot Ankle Int. 2004;25:833–839.
29. Ferber, R, Davis, IM, Williams, DS, III. Effect of foot orthotics on rearfoot and tibia joint coupling patterns and variability. J Biomech. 2005;38:477–483.
30. Ferrari, J, Malone-Lee, J. A radiographic study of the relationship between metatarsus adductus and hallux valgus. J Foot Ankle Surg. 2003;42:9–14.
31. Flemister, AS, Neville, CG, Houck, J. The relationship between ankle, hindfoot, and forefoot position and posterior tibial muscle excursion. Foot Ankle Int. 2007;28:448–455.
32. Franettovich, M, Chapman, A, Blanch, P, Vicenzino, B. A physiological and psychological basis for anti-pronation taping from a critical review of the literature. Sports Med. 2008;38:617–631.
33. Freeman, MA, Dean, MR, Hanham, IW. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678–685.
34. Fritz, GR, Prieskorn, D. First metatarsocuneiform motion: a radiographic and statistical analysis. Foot Ankle Int. 1995;16:117–123.
35. Fujii, T, Kitaoka, HB, Luo, ZP, et al. Analysis of ankle-hindfoot stability in multiple planes: an in vitro study. Foot Ankle Int. 2005;26:633–637.
36. Fujii, T, Luo, ZP, Kitaoka, HB, An, KN. The manual stress test may not be sufficient to differentiate ankle ligament injuries. Clin Biomech (Bristol, Avon). 2000;15:619–623.
37. Glasoe, WM, Yack, HJ, Saltzman, CL. Anatomy and biomechanics of the first ray. Phys Ther. 1999;79:854–859.
38. Green, T, Refshauge, K, Crosbie, J, Adams, R. A randomized controlled trial of a passive accessory joint mobilization on acute ankle inversion sprains. Phys Ther. 2001;81:984–994.
39. Gribble, PA, Hertel, J, Denegar, CR. Chronic ankle instability and fatigue create proximal joint alterations during performance of the Star Excursion Balance Test. Int J Sports Med. 2007;28:236–242.
40. Grimston, SK, Nigg, BM, Hanley, DA, Engsberg, JR. Differences in ankle joint complex range of motion as a function of age. Foot Ankle. 1993;14:215–222.
41. Guette, M, Gondin, J, Martin, A, et al. Plantar flexion torque as a function of time of day. Int J Sports Med. 2006;27:171–177.
42. Hale, SA, Hertel, J, Olmsted-Kramer, LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2007;37:303–311.
43. Hertel, J. Functional instability following lateral ankle sprain. Sports Med. 2000;29:361–371.
44. Hertel, J, Olmsted-Kramer, LC. Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture. 2007;25:33–39.
45. Hicks, JH. The mechanics of the foot. I. The joints. J Anat. 1953;87:345–357.
46. Higginson, JS, Zajac, FE, Neptune, RR, et al. Effect of equinus foot placement and intrinsic muscle response on knee extension during stance. Gait Posture. 2006;23:32–36.
47. Holmes, CF, Wilcox, D, Fletcher, JP. Effect of a modified, low-dye medial longitudinal arch taping procedure on the subtalar joint neutral position before and after light exercise. J Orthop Sports Phys Ther. 2002;32:194–201.
48. Huang, CK, Kitaoka, HB, An, KN, Chao, EY. Biomechanical evaluation of longitudinal arch stability. Foot Ankle. 1993;14:353–357.
49. Hubbard, TJ, Hertel, J, Sherbondy, P. Fibular position in individuals with self-reported chronic ankle instability. J Orthop Sports Phys Ther. 2006;36:3–9.
50. Hunt, AE, Smith, RM. Mechanics and control of the flat versus normal foot during the stance phase of walking. Clin Biomech (Bristol, Avon). 2004;19:391–397.
51. Inman, VT. The joints of the ankle. Baltimore: Williams & Wilkins; 1976.
52. Inman, VT, Ralston, HJ, Todd, F. Human walking. Baltimore: Williams & Wilkins; 1981.
53. Jotoku, T, Kinoshita, M, Okuda, R, Abe, M. Anatomy of ligamentous structures in the tarsal sinus and canal. Foot Ankle Int. 2006;27:533–538.
54. Kaikkonen, A, Hyppänen, E, Kannus, P, Järvinen, M. Long-term functional outcome after primary repair of the lateral ligaments of the ankle. Am J Sports Med. 1997;25:150–155.
55. Kanatli, U, Gözil, R, Besli, K, et al. The relationship between the hindfoot angle and the medial longitudinal arch of the foot. Foot Ankle Int. 2006;27:623–627.
56. Kaufman, KR, Brodine, SK, Shaffer, RA, et al. The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med. 1999;27:585–593.
57. Khamis, S, Yizhar, Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture. 2007;25:127–134.
58. Kitaoka, HB, Luo, ZP, An, KN. Three-dimensional analysis of flatfoot deformity: cadaver study. Foot Ankle Int. 1998;19:447–451.
59. Kitaoka, HB, Luo, ZP, Growney, ES, et al. Material properties of the plantar aponeurosis. Foot Ankle Int. 1994;15:557–560.
60. Klein, P, Mattys, S, Rooze, M. Moment arm length variations of selected muscles acting on talocrural and subtalar joints during movement: an in vitro study. J Biomech. 1996;29:21–30.
61. Knudson, GA, Kitaoka, HB, Lu, CL, et al. Subtalar joint stability. Talocalcaneal interosseous ligament function studied in cadaver specimens. Acta Orthop Scand. 1997;68:442–446.
62. Konradsen, L. Sensori-motor control of the uninjured and injured human ankle. J Electromyogr Kinesiol. 2002;12:199–203.
63. Konradsen, L, Bech, L, Ehrenbjerg, M, Nickelsen, T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002;12:129–135.
64. Kulig, K, Burnfield, JM, Reischl, S, et al. Effect of foot orthoses on tibialis posterior activation in persons with pes planus. Med Sci Sports Exerc. 2005;37:24–29.
65. Kulig, K, Burnfield, JM, Requejo, SM, et al. Selective activation of tibialis posterior: evaluation by magnetic resonance imaging. Med Sci Sports Exerc. 2004;36:862–867.
66. Kulig, K, Reischl, SF, Pomrantz, AB, et al. Nonsurgical management of posterior tibial tendon dysfunction with orthoses and resistive exercise: a randomized controlled trial. Phys Ther. 2009;89:26–37.
67. Lakin, RC, DeGnore, LT, Pienkowski, D. Contact mechanics of normal tarsometatarsal joints. J Bone Joint Surg Am. 2001;83:520–528.
68. Leardini, A, Benedetti, MG, Berti, L, et al. Rear-foot, mid-foot and fore-foot motion during the stance phase of gait. Gait Posture. 2007;25:453–462.
69. Lees, A, Lake, M, Klenerman, L. Shock absorption during forefoot running and its relationship to medial longitudinal arch height. Foot Ankle Int. 2005;26:1081–1088.
70. Leland, RH, Marymont, JV, Trevino, SG, et al. Calcaneocuboid stability: a clinical and anatomic study. Foot Ankle Int. 2001;22:880–884.
71. Lewis, GS, Kirby, KA, Piazza, SJ. Determination of subtalar joint axis location by restriction of talocrural joint motion. Gait Posture. 2007;25:63–69.
72. Lewis, OJ. The comparative morphology of M. flexor accessorius and the associated long flexor tendons. J Anat. 1962;96:321–333.
73. Löfvenberg, R, Kärrholm, J, Sundelin, G, Ahlgren, O. Prolonged reaction time in patients with chronic lateral instability of the ankle. Am J Sports Med. 1995;23:414–417.
74. Lundberg, A, Svensson, OK, Bylund, C, et al. Kinematics of the ankle/foot complex—Part 2: pronation and supination. Foot Ankle. 1989;9:248–253.
75. Lundberg, A, Svensson, OK, Bylund, C, et al. Kinematics of the ankle/foot complex—Part 3: influence of leg rotation. Foot Ankle. 1989;9:304–309.
76. Lundgren, P, Nester, C, Liu, A, et al. Invasive in vivo measurement of rear-, mid- and forefoot motion during walking. Gait Posture. 2008;28:93–100.
77. MacLean, C, Davis, IM, Hamill, J. Influence of a custom foot orthotic intervention on lower extremity dynamics in healthy runners. Clin Biomech (Bristol, Avon). 2006;21:623–630.
78. Biomechanics of the foot. In: Mann RA, ed. American academy of orthopedic surgeons, editors: Atlas of orthotics: biomechanical principles and application. St Louis: Mosby, 1975.
79. Manoli, A, Graham, B. The subtle cavus foot, “the underpronator” [Review]. Foot Ankle Int. 2005;26:256–263.
80. Manter, JT. Movements of the subtalar joint and transverse tarsal joint. Anat Rec. 1941;80:397–410.
81. Martin, RL, Stewart, GW, Conti, SF. Posttraumatic ankle arthritis: an update on conservative and surgical management. J Orthop Sports Phys Ther. 2007;37:253–259.
82. Mattingly, B, Talwalkar, V, Tylkowski, C, et al. Three-dimensional in vivo motion of adult hind foot bones. J Biomech. 2006;39:726–733.
83. McCulloch, MU, Brunt, D, Vander, LD. The effect of foot orthotics and gait velocity on lower limb kinematics and temporal events of stance. J Orthop Sports Phys Ther. 1993;17:2–10.
84. McKinley, TO, Rudert, MJ, Koos, DC, Brown, TD. Incongruity versus instability in the etiology of posttraumatic arthritis. Clin Orthop Relat Res. 2004;423:44–51.
85. McPoil, TG, Knecht, HG, Schuit, D. A survey of foot types in normal females between ages of 18 and 30 years. J Orthop Sports Phys Ther. 1988;9:406–409.
86. Mei-Dan, O, Kahn, G, Zeev, A, et al. The medial longitudinal arch as a possible risk factor for ankle sprains: a prospective study in 83 female infantry recruits. Foot Ankle Int. 2005;26:180–183.
87. Mengiardi, B, Zanetti, M, Schöttle, PB, et al. Spring ligament complex: MR imaging–anatomic correlation and findings in asymptomatic subjects. Radiology. 2005;237:242–249.
88. Michelson, JD, Helgemo, SL, Jr. Kinematics of the axially loaded ankle. Foot Ankle Int. 1995;16:577–582.
89. Milgrom, C, Giladi, M, Kashtan, H, et al. A prospective study of the effect of a shock-absorbing orthotic device on the incidence of stress fractures in military recruits. Foot Ankle. 1985;6:101–104.
90. Mohammadi, F. Comparison of 3 preventive methods to reduce the recurrence of ankle inversion sprains in male soccer players. Am J Sports Med. 2007;35:922–926.
91. Monaghan, K, Delahunt, E, Caulfield, B. Ankle function during gait in patients with chronic ankle instability compared to controls. Clin Biomech (Bristol, Avon). 2006;21:168–174.
92. Mundermann, A, Nigg, BM, Neil, HR, Stefanyshyn, DJ. Foot orthotics affect lower extremity kinematics and kinetics during running. Clin Biomech (Bristol, Avon). 2003;18:254–262.
93. Murray, MP, Guten, GN, Sepic, SB, et al. Function of the triceps surae during gait. Compensatory mechanisms for unilateral loss. J Bone Joint Surg Am. 1978;60:473–476.
94. Myers, JB, Riemann, BL, Hwang, JH, et al. Effect of peripheral afferent alteration of the lateral ankle ligaments on dynamic stability. Am J Sports Med. 2003;31:498–506.
95. Nester, C, Bowker, P, Bowden, P. Kinematics of the midtarsal joint during standing leg rotation. J Am Podiatr Med Assoc. 2002;92:77–81.
96. Nester, CJ, Findlow, AF, Bowker, P, Bowden, PD. Transverse plane motion at the ankle joint. Foot Ankle Int. 2003;24:164–168.
97. Neville, C, Flemister, A, Tome, J, Houck, J. Comparison of changes in posterior tibialis muscle length between subjects with posterior tibial tendon dysfunction and healthy controls during walking. J Orthop Sports Phys Ther. 2007;37:661–669.
98. Nigg, BM, Khan, A, Fisher, V, Stefanyshyn, D. Effect of shoe insert construction on foot and leg movement. Med Sci Sports Exerc. 1998;30:550–555.
99. Nistor, L, Markhede, G, Grimby, G. A technique for measurements of plantar flexion torque with the Cybex II dynamometer. Scand J Rehabil Med. 1982;14:163–166.
100. Ordway, NR, Hand, N, Briggs, G, et al. Reliability of knee and ankle strength measures in an older adult population. J Strength Cond Res. 2006;20:82–87.
101. Owens, S, Thordarson, DB. The adductor hallucis revisited. Foot Ankle Int. 2001;22:186–191.
102. Patil, V, Ebraheim, N, Wagner, R, Owens, C. Morphometric dimensions of the dorsal calcaneocuboid ligament. Foot Ankle Int. 2008;29:508–512.
103. Piazza, SJ. Mechanics of the subtalar joint and its function during walking. Foot Ankle Clin. 2005;10:425–442.
104. Powers, CM, Maffucci, R, Hampton, S. Rearfoot posture in subjects with patellofemoral pain. J Orthop Sports Phys Ther. 1995;22:155–160.
105. Reischl, SF, Powers, CM, Rao, S, Perry, J. Relationship between foot pronation and rotation of the tibia and femur during walking. Foot Ankle Int. 1999;20:513–520.
106. Requião, LF, Nadeau, S, Milot, MH, et al. Quantification of level of effort at the plantarflexors and hip extensors and flexor muscles in healthy subjects walking at different cadences. J Electromyogr Kinesiol. 2005;15:393–405.
107. Richie, DH, Jr. Effects of foot orthoses on patients with chronic ankle instability. J Am Podiatr Med Assoc. 2007;97:19–30.
108. Root, ML. Development of the functional orthosis. Clin Podiatr Med Surg. 1994;11:183–210.
109. Rotem-Lehrer, N, Laufer, Y. Effect of focus of attention on transfer of a postural control task following an ankle sprain. J Orthop Sports Phys Ther. 2007;37:564–569.
110. Ruohola, JP, Kiuru, MJ, Pihlajamaki, HK. Fatigue bone injuries causing anterior lower leg pain. Clin Orthop Relat Res. 2006;444:216–223.
111. Santilli, V, Frascarelli, MA, Paoloni, M, et al. Peroneus longus muscle activation pattern during gait cycle in athletes affected by functional ankle instability: a surface electromyographic study. Am J Sports Med. 2005;33:1183–1187.
112. Santos, MJ, Liu, W. Possible factors related to functional ankle instability. J Orthop Sports Phys Ther. 2008;38:150–157.
113. Sawkins, K, Refshauge, K, Kilbreath, S, Raymond, J. The placebo effect of ankle taping in ankle instability. Med Sci Sports Exerc. 2007;39:781–787.
114. Scott, SH, Winter, DA. Biomechanical model of the human foot: kinematics and kinetics during the stance phase of walking. J Biomech. 1993;26:1091–1104.
115. Self, BP, Harris, S, Greenwald, RM. Ankle biomechanics during impact landings on uneven surfaces. Foot Ankle Int. 2000;21:138–144.
116. Sepic, SB, Murray, MP, Mollinger, LA, et al. Strength and range of motion in the ankle in two age groups of men and women. Am J Phys Med. 1986;65:75–84.
117. Shamus, J, Shamus, E, Gugel, RN, et al. The effect of sesamoid mobilization, flexor hallucis strengthening, and gait training on reducing pain and restoring function in individuals with hallux limitus: a clinical trial. J Orthop Sports Phys Ther. 2004;34:368–376.
118. Sheehan, FT, Seisler, AR, Siegel, KL. In vivo talocrural and subtalar kinematics: a non-invasive 3D dynamic MRI study. Foot Ankle Int. 2007;28:323–335.
119. Siegler, S, Chen, J, Schneck, CD. The three-dimensional kinematics and flexibility characteristics of the human ankle and subtalar joints—Part I: kinematics. J Biomech Eng. 1988;110:364–373.
120. Standring, S. Gray’s anatomy: the anatomical basis of clinical practice, ed 40. St Louis: Elsevier; 2009.
121. Stauffer, RN, Chao, EY, Brewster, RC. Force and motion analysis of the normal, diseased, and prosthetic ankle joint. Clin Orthop Relat Res. 1977;127:189–196.
122. Strauss, JE, Forsberg, JA, Lippert, FG, III. Chronic lateral ankle instability and associated conditions: a rationale for treatment. Foot Ankle Int. 2007;28:1041–1044.
123. Sutherland, DH. An electromyographic study of the plantar flexors of the ankle in normal walking on the level. J Bone Joint Surg Am. 1966;48:66–71.
124. Sutherland, DH. The evolution of clinical gait analysis. Part l: kinesiological EMG. Gait Posture. 2001;14:61–70.
125. Taylor, KF, Bojescul, JA, Howard, RS, et al. Measurement of isolated subtalar range of motion: a cadaver study. Foot Ankle Int. 2001;22:426–432.
126. Thordarson, DB, Schmotzer, H, Chon, J, Peters, J. Dynamic support of the human longitudinal arch. A biomechanical evaluation. Clin Orthop Relat Res. 1995;316:165–172.
127. Tochigi, Y, Amendola, A, Rudert, MJ, et al. The role of the interosseous talocalcaneal ligament in subtalar joint stability. Foot Ankle Int. 2004;25:588–596.
128. Tochigi, Y, Rudert, MJ, Saltzman, CL, et al. Contribution of articular surface geometry to ankle stabilization. J Bone Joint Surg Am. 2006;88:2704–2713.
129. Tome, J, Nawoczenski, DA, Flemister, A, Houck, J. Comparison of foot kinematics between subjects with posterior tibialis tendon dysfunction and healthy controls. J Orthop Sports Phys Ther. 2006;36:635–644.
130. Van Deun, S, Staes, FF, Stappaerts, KH, et al. Relationship of chronic ankle instability to muscle activation patterns during the transition from double-leg to single-leg stance. Am J Sports Med. 2007;35:274–281.
131. Van Gheluwe, B, Dananberg, HJ, Hagman, F, Vanstaen, K. Effects of hallux limitus on plantar foot pressure and foot kinematics during walking. J Am Podiatr Med Assoc. 2006;96:428–436.
132. Verhagen, E, van der Beek, A, Twisk, J, et al. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32:1385–1393.
133. Verhagen, RA, de Keizer, G, van Dijk, CN. Long-term follow-up of inversion trauma of the ankle. Arch Orthop Trauma Surg. 1995;114:92–96.
134. Vicenzino, B, Branjerdporn, M, Teys, P, Jordan, K. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther. 2006;36:464–471.
135. Wan, L, de Asla, RJ, Rubash, HE, Li, G. In vivo cartilage contact deformation of human ankle joints under full body weight. J Orthop Res. 2008;26:1081–1089.
136. Wearing, SC, Smeathers, JE, Sullivan, PM, et al. Plantar fasciitis: are pain and fascial thickness associated with arch shape and loading? Phys Ther. 2007;87:1002–1008.
137. Whittingham, M, Palmer, S, Macmillan, F. Effects of taping on pain and function in patellofemoral pain syndrome: a randomized controlled trial. J Orthop Sports Phys Ther. 2004;34:504–510.
138. Williams, DS, III., McClay, IS, Hamill, J. Arch structure and injury patterns in runners. Clin Biomech (Bristol, Avon). 2001;16:341–347.
139. Winter, DA. Biomechanics and motor control of human movement. New Jersey: John Wiley & Sons; 2005.
140. Witvrouw, E, Borre, KV, Willems, TM, et al. The significance of peroneus tertius muscle in ankle injuries: a prospective study. Am J Sports Med. 2006;34:1159–1163.
141. Yoshioka, Y, Siu, DW, Scudamore, RA, Cooke, TD. Tibial anatomy and functional axes. J Orthop Res. 1989;7:132–137.
142. Youberg, LD, Cornwall, MW, McPoil, TG, Hannon, PR. The amount of rearfoot motion used during the stance phase of walking. J Am Podiatr Med Assoc. 2005;95:376–382.
143. Younger, AS, Hansen, ST, Jr. Adult cavovarus foot. J Am Acad Orthop Surg. 2005;13:302–315.
144. Younger, AS, Sawatzky, B, Dryden, P. Radiographic assessment of adult flatfoot. Foot Ankle Int. 2005;26:820–825.
STUDY QUESTIONS
1. List the bones that make up (a) the ankle and (b) the rearfoot. Which bone is common to both regions?
2. Explain how excessive tibial torsion could mask the functional expression of excessive femoral anteversion.
3. Describe the path of the tendon of the flexor hallucis longus, from its belly to its insertion on the great toe.
4. Describe the primary arthrokinematics of inversion and eversion at the talonavicular joint.
5. Describe how the first tarsometatarsal joint is frequently involved with the development of hallux valgus (bunion).
6. Using Figure 14-43 as a reference, contrast the inversion torque potential of the tibialis anterior and the extensor hallucis longus.
7. Explain why a person with a weak calf muscle may complain of “buckling” of the knee prior to the push off phase of walking.
8. Compare the distal attachments of the fibularis brevis and fibularis tertius. Justify how these muscles have different actions within the sagittal plane but similar actions in the frontal plane.
9. Which structures (joints and connective tissues) bind the fibula to the tibia?
10. Describe the roll-and-slide arthrokinematics of dorsiflexion at the talocrural joint with the foot free (Figure 14-18, A) and with the foot fixed (Figure 14-20, A).
11. Which part of the gait cycle requires greater dorsiflexion at the talocrural joint: the stance phase or the swing phase?
12. What factors contribute to the stability of the talocrural joint in full dorsiflexion?
13. Which muscle is considered the most direct antagonist to the fibularis longus?
14. Propose a mechanism that could explain why active plantar flexion torque at the ankle is about 20% to 30% greater with the knee extended than when flexed.
15. Which deformity would most likely develop after weakness of the invertor muscles? Which muscles would you stretch? Which muscles would you attempt to strengthen?
 Answers to the study questions can be found on the Evolve website.
Answers to the study questions can be found on the Evolve website.