CHAPTER 10 Anesthesia for cataract surgery
Local anesthesia (LA) techniques
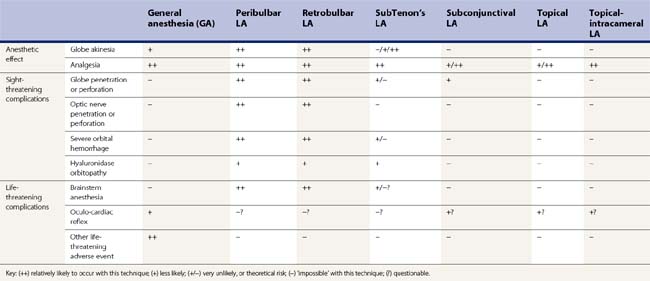
Several techniques of LA have been described for cataract surgery. There are three main categories: (i) sharp needle blocks (retrobulbar, peribulbar)1, (ii) blunt cannula blocks (subTenon’s)2, and (iii) minimal anesthesia (topical, topical-intracameral)3. These techniques are compared in Table 10.1. Other techniques have been described, including subconjunctival LA, and subTenon’s LA using a sharp needle. For any LA procedure, the patient should be warned what to expect beforehand. If sedation is not used, most patients find it reassuring to hold the hand of an assistant, who also monitors the patient during surgery. Guidelines for safe practice have been published4,5.
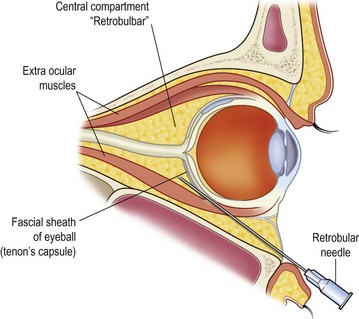
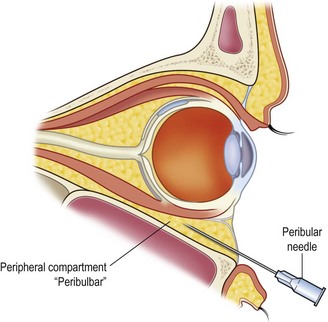
Sharp needle blocks
Retrobulbar and peribulbar LA injections1 (Figs 10.1, 10.2) give excellent akinesia and analgesia, although they are associated with sight-threatening and life-threatening complications. The needle may penetrate the globe or optic nerve, and this can result in blindness. Long myopic eyes, particularly those with a staphyloma, are at particular risk of this complication. If the needle penetrates the meninges around the optic nerve, the LA may enter the subdural space and track back to the brainstem; brainstem anesthesia may present with apnea, fitting, unstable blood pressure, and possibly death1,6. While these complications are rare, they are of course devastating. Therefore, it is recommended that these techniques are only used after suitable training, consideration of the anatomy and eyeball size/shape for each case, and with back-up available in case of an inadvertent brainstem injection1,4,5. Even in the best hands, these complications can occur with sharp needle blocks1. The advent of small-incision phacoemulsification was associated with renewed interest in LA techniques which should have a fewer complications.
SubTenon’s anesthesia
The SubTenon’s LA technique2 involves passing a blunt-ended cannula between Tenon’s capsule and the sclera. If the cannula is blunt enough, there should be no risk of penetrating the globe or optic nerve (Fig. 10.3). The anatomical connection between the sclera and dura means that the LA should not be able to reach the brainstem. Thus, the technique should be safer than sharp needle blocks.
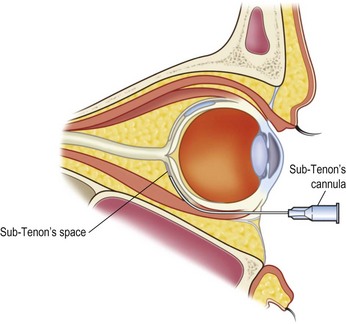
Fig. 10.3 SubTenon’s anesthesia.
A blunt cannula introduces the anesthetic between Tenon’s capsule and sclera.
Numerous variants of the STA technique have been described2. Common techniques include (i) posterior injection using a long metal subTenon’s cannula, (ii) anterior injection using a short plastic subTenon’s cannula, and (iii) posterior injection using a flexible intravenous cannula. Anterior injections are more likely to cause chemosis or subconjunctival hemorrhage. Larger volumes of injectate give better akinesia, and hyaluronidase can aid diffusion.
Complications of subTenon’s anesthesia do appear to be rarer, and less severe, than with sharp needle blocks2,6. Chemosis and subconjunctival hemorrhage are very common. Orbital hemorrhage occurs rarely, generally due to damage to a vortex vein. A scarred conjunctiva (e.g. from previous cryo/explant surgery) can make the initial dissection difficult or impossible. Posterior injections have rarely been associated with optic nerve infarcts, episodes suggestive of brainstem anesthesia, and even death2. It is possible that these reports are indeed true complications, perhaps due to anatomical variants at the optic nerve/scleral junction which may render some patients particularly susceptible. Because of these concerns, some authors have cautioned against using subTenon’s injections that are very posterior, particularly if a metal cannula is used.
Standard subTenon’s LA technique
Several variants of subTenon’s anesthesia have been described2. A simple and reliable technique is as follows. (i) A syringe is prepared with anesthetic and a blunt-ended subTenon’s cannula (e.g. curved Stevens type 19-gauge metal subTenon cannula). If the surgeon requires anesthesia without akinesia, 2 ml of lidocaine will be adequate. If the surgeon requires akinesia, then larger volumes and/or additional hyaluronidase may be used. (ii) Topical anesthesia (e.g. proxymetacaine) and povidone-iodine are instilled. (iii) A lid speculum is inserted, or the eyelids may be held open with the fingers. (iv) The patient is instructed to look ‘up and out’, thus exposing the conjunctiva in the inferonasal part of the globe. (v) The conjunctiva is grasped with conjunctival forceps, about 5 mm posterior to the limbus, between the insertions of the medial rectus and inferior rectus. (vi) The conjunctiva is elevated slightly, and spring scissors are used to make a small ‘snip’ in the conjunctiva and the underlying Tenon’s capsule. When positioned 5 mm from the limbus, a tiny snip (about 2–3 mm) will normally go through both layers and expose the shiny sclera below. Occasionally, the initial snip is insufficient to expose the sclera, and it may be necessary make a larger snip, or to make a small dissection by inserting the closed scissors into the incision, then opening the scissors to spread the tissues. (vii) The posterior edge of the incision is held with forceps, and the subTenon’s cannula is introduced. (viii) The cannula is advanced posteriorly with a sweeping motion, so that the cannula tip remains in contact with the sclera until it is behind the equator of the globe (see Fig. 10.3). Because the advancing cannula remains approximately tangential to the globe, there is no risk of globe penetration. (ix) Anesthetic is injected slowly, then the cannula is removed.
No-snip subTenon’s LA technique
The ‘no-snip’ technique is very similar to the above, except that it uses a slightly smaller, round-ended metal cannula. Some commercially-available cannulae are ‘sharp’ enough to penetrate the conjunctiva/Tenon’s without an initial snip, but too blunt to penetrate the sclera (e.g. Mendez–Goldbaum Tri-port cannula 100-21C, Eagle Labs, Rancho Cucamonga, CA). This type of cannula makes the initial snip unnecessary. The technique can give good results7, though some practitioners find that anesthetic can reflux back alongside the Eagle cannula. Slower injection, and/or larger volumes, will overcome this problem. With care, the Stevens cannula can also be used for the no-snip technique.
Topical and topical-intracameral LA
Topical anesthesia is becoming increasingly popular for phacoemulsification. It has the advantage that virtually no training is required, no additional personnel or time is needed for the anesthetic, and patient satisfaction rates are high. Some surgeons use purely topical anesthesia (e.g. tetracaine 1% drops). Many will routinely supplement topical anesthesia with an intracameral dose of non-preserved anesthetic. A recent meta-analysis concluded that intracameral lidocaine does improve patient comfort, with no evidence of corneal toxicity or other adverse events3. Many surgeons feel that intracameral LA is important for patient comfort, particularly if the instruments inadvertently touch the iris.
It has been suggested that topical/intracameral LA may give an increased risk of surgical complications, because of a potentially mobile eye. However, many believe that the opposite is true. By fixating on the light, the patient keeps their eye perpendicular to the microscope, thus facilitating surgery. If an LA block is used, then the akinetic eye may make it difficult to position the patient with the eye ‘on axis’. Furthermore, the volume of LA behind the eye may increase vitreous bulge. At this author’s institution, topical/intracameral LA without sedation is used for over 98% of all cataract surgery (including for teaching trainees), and the rate of surgical complications is reassuringly low8.
LA cataract surgery in upright position
Some patients cannot position with their head horizontal for cataract surgery, because of medical problems such as ankylosing spondylitis or severe Meniere’s disease. They may be high risk for GA, but surgery can take place with the patient seated upright, using topical-intracameral LA9. The operating microscope is rotated toward the horizontal, and the surgeon sits or stands, facing the patient. An inferiorly placed incision is used. Topical-intracameral LA is particularly advantageous for these patients, because the patient will be able to keep the eye in line with the microscope. It is important to ensure that both patient and surgeon are happy with positioning before surgery commences.
No anesthesia
Corneal-incision phacoemulsification has been described, using a modified technique and no anesthesia at all. A randomized trial indicated no demonstrable difference between this and topical-intracameral LA10. It should be remembered that all patients (and surgeons) in this study consented to be randomized to the no-anesthesia group. For ‘normal’ patients, experience shows that anesthesia is required for safe and comfortable surgery.
1 Hamilton RC. Retrobulbar and peribulbar anesthesia for cataract surgery. In Steinert RF, editor: Cataract Surgery: Technique, Complications, and Management, 2nd edn, Philadelphia: Saunders, 2004.
2 Kumar CM, Williamson S, Manickam B. A review of sub-Tenon’s block: current practice and recent development. Eur J Anaesthesiol. 2005;22(8):567-577.
3 Ezra DG, Nambiar A, Allan BD. Supplementary intracameral lidocaine for phacoemulsification under topical anesthesia. A meta-analysis of randomized controlled trials. Ophthalmology. 2008;115(3):455-487.
4 London: Royal College of Ophthalmologists, Royal College of Anaesthetists; 2001 (new edition 2011/2) Available from www.rcophth.ac.uk
5 Anon. Anaesthesia. In: Benjamin L, et al, editors. Cataract surgery guidelines September 2010. London: Royal College of Ophthalmologists, 2010. Available from www.rcophth.ac.uk
6 Eke T, Thompson JR. Serious complications of local anaesthesia for cataract surgery: a one-year national survey in the United Kingdom. Br J Ophthalmol. 2007;91(4):470-475.
7 Allman KG, Theron AD, Byles DB. A new technique of incisionless minimally invasive sub-Tenon’s anaesthesia. Anaesthesia. 2008;63(7):782-783.
8 Shaw AD, Ang GS, Eke T. Complication rates for phacoemulsification surgery. Ophthalmology. 2007;114:2101-2102.
9 Lee RMH, Jehle T, Eke T. Face-to-face upright seated positioning for cataract surgery in patients who cannot lie flat. J Cataract Refract Surg. 2011;37:805-809.
10 Pandey SK, Werner L, Apple DJ, et al. No-anesthesia clear corneal phacoemulsification versus topical and topical plus intracameral anesthesia. Randomized clinical trial. J Cataract Refract Surg. 2001;27(10):1643-1650.