CHAPTER 7 Face and neck nerve blocks
Nerve blocks in the head and face are useful for the repair of lacerations and for scrubbing and debriding ‘roasties’. Nerve blocks in this region are less painful to the patient than local infiltration and they do not distort the anatomy. The supraorbital nerve, the infraorbital nerve and the mental nerve all exit their foramina along a line that can be drawn 25 mm lateral to the midline of the face through the pupil and the labial angle (Fig. 7.1).
Fig. 7.1 A line drawn through the pupil and the corner of the mouth will bisect the foramina of the supraorbital, infraorbital and mental nerves (from top to bottom).
Supraorbital and supratrochlear nerve blocks
The supraorbital and supratrochlear nerves supply sensation to the fontal aspect of the scalp (the forehead). The supraorbital nerve exits the skull through the supraorbital foramen that lies in the midpupillary line, which is approximately 25 mm lateral to the facial midline along the supraorbital ridge. The supratrochlear nerve exits the skull along the upper medial corner of the orbit in the supratrochlear notch, which is approximately 15 mm medial to the supraorbital foramen. Supraorbital and supratrochlear nerve blocks can be performed from either the area of the supraorbital foramen or the area of the supratrochlear notch. When in doubt, an ‘eyebrow block’ can be used to provide anaesthesia to virtually the entire ipsilateral forehead.
Ultrasound can also be used to identify the precise location of the supraorbital foramen.
Technique
Lateral or inferior approach
If performed from the side of the supraorbital foramen (Figs 7.2, 7.3):
•
Identify the target area for needle insertion – just lateral to the notch on the supraorbital ridge in the midpupillary line.
•
Raise a skin weal of local anaesthetic at the site with a 25G needle.
•
Puncture the skin and advance the needle posteriorly and superiorly until the bone is contacted. Withdraw the needle by 1 mm. Do not attempt to enter the foramen.
•
Aspirate. If no blood is detected, inject approximately 2 to 3 mL of local anaesthetic outside the foramen above the eyebrow.
•
If blood is aspirated, reposition the needle slightly and aspirate again.
•
If the patient complains of paraesthesias or severe pain with injection, withdraw the needle by 1 to 2 mm before the injection is continued.
•
To block the supratrochlear nerve, redirect the needle medially, with the syringe held parallel to the eyebrow, and advance it to a position 15 mm lateral to the junction of the supraorbital ridge and the root of the nose.
•
Aspirate. If no blood is withdrawn, inject 1 to 3 mL of local anaesthetic. Inject a further 1 to 3 mL as the needle is withdrawn.
Medial approach
If the block is performed from the area of the supratrochlear nerve (Fig. 7.4):
•
Identify the target point for needle insertion – the root of the nose at the junction of the nasal root and supraorbital ridge.
•
Raise a weal of local anaesthetic at the site with a 25G needle.
•
Puncture the skin with the syringe held parallel to the eyebrow. Infiltrate the skin along the length of the entire eyebrow with frequent aspiration to avoid intravascular injection.
•
For this field block, 2 to 4 mL of local anaesthetic solution per side is usually sufficient, and no more than 5 mL should be injected into either side.
•
Warn patients about the possibility of swelling in the upper and/or lower eyelids. There is a risk of ecchymosis or haematoma formation with this injection.
Ultrasound assistance
Ultrasound can be used to define the exact position of the supraorbital foramen (Figs 7.5, 7.6A&B). This position can then be marked on the skin and the procedure performed blind (an ultrasound-aided technique) or the out-of-plane approach can be used to advance the needle to a point just superficial to the foramen before injecting local anaesthetic (an ultrasound-guided technique).
Infraorbital nerve block
The infraorbital nerve innervates the lower eyelid, the medial aspect of the cheek, upper lip, and lateral portion of the nose. The infraorbital nerve exits the skull through the infraorbital foramen, which is 10 mm inferior to the orbital rim and approximately 25 mm lateral to the facial midline in the midpupillary line.
An infraorbital block may be performed either via an intraoral approach or by injecting through the skin. See page 24 in Chapter 4 for the intraoral approach to the infraorbital nerve block.
Technique
Direct transcutaneous injection (Fig. 7.7):
•
Identify the target area for needle insertion – 5 mm inferior to the infraorbital foramen.
•
Hold the syringe vertically, with the needle aimed superiorly, and puncture the skin 5 mm inferior to the foramen.
•
Advance the needle posteriorly and superiorly to contact the bone in the vicinity of the foramen and then withdraw the needle by 1 mm. Do not attempt to enter the canal.
•
Aspirate. If no blood is withdrawn, inject 2 to 3 mL of local anaesthetic near and around the foramen, but not into it.
•
Keep the injection pressures low since retrograde passage of local anaesthetic into the orbit can cause temporary blindness (very disconcerting to the patient).
•
If blood is aspirated, withdraw the needle slightly and redirect it.
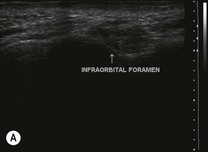
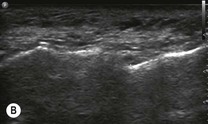
Ultrasound assistance
The exact position of this nerve can be more difficult to determine by palpation, but can be easily seen with ultrasound. The probe should be positioned with the edge right against the nose, about 10 mm below the eye (Fig. 7.8). The foramen can be seen as a defect in the cortex (Fig. 7.9A&B). The block can then be performed with real-time ultrasound guidance or once the position has been marked on the skin.
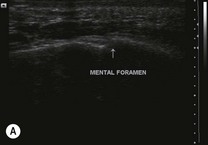
Mental nerve block
The mental nerve innervates the lower lip and chin. The mental nerve exits the mandible through the mental foramen, which is located approximately 25 mm from the midline of the face in the midpupillary line. Either a transcutaneous or intraoral approach can be used to block the mental nerve. See page 30 in Chapter 4 for the intraoral approach to the mental nerve block.
Technique
Direct transcutaneous injection:
•
Identify the mental foramen 25 mm lateral to the facial midline, 7 to 10 mm above the inferior border of the mandible.
•
This block may be approached from inferiorly (superior needle direction) or from posteriorly (anterior needle direction). The horizontal approach is better if the foramen is not easily palpable, as the position of the foramen can be variable. It is frequently more posterior than expected and a block using this approach will still be successful.
•
Posterior approach (
Fig. 7.10):
•
The target point for needle insertion is 10 mm posterior to the mental foramen.
•
Hold the syringe parallel to the inferior aspect of the mandible. Puncture the skin 10 mm posterior to the mental foramen and advance the needle into the vicinity of the mental foramen (do not attempt to enter the canal).
•
After aspirating, inject 1 to 2 mL of local anaesthetic near and around the foramen. Inject a further 1 mL while withdrawing the needle. If blood is withdrawn, reposition the needle slightly before injecting.
•
Inferior approach (
Fig. 7.11):
•
The target point for needle insertion is 5 mm inferior to the mental foramen (immediately superior to the inferior border of the mandible).
•
Hold the syringe with the needle pointing superiorly (towards the pupil). Puncture the skin 5 mm inferior to the mental foramen and advance the needle superiorly and posteriorly until the bone is contacted (do not attempt to enter the canal).
•
Withdraw the needle by 1 mm and aspirate. If blood is aspirated, reposition the needle slightly.
•
If no blood is aspirated, inject 2 to 3 mL of local anaesthetic in the vicinity of the foramen.
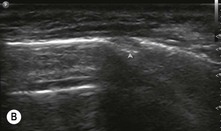
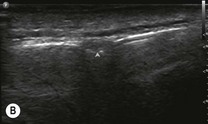
Ultrasound assistance
The mental nerve has the most variable bony exit point of the facial nerves. This can be precisely determined using ultrasound (Figs 7.12, 7.13A&B), and the nerve blocked under real-time guidance or blindly after the position has been marked on the skin.
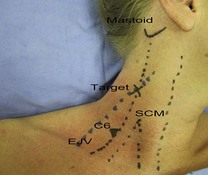
Superficial cervical plexus block
The superficial cervical plexus supplies sensation to the skin of the anterolateral neck through the anterior nerve roots of C2, C3 and C4. This block is useful to provide anaesthesia for procedures or wound repair in the anterior and posterior triangles of the neck.
Preparation
•
Position the patient supine or in semi-Fowler’s position with the head facing away from the side to be blocked.
•
Draw a line from the mastoid process to the transverse process of C6. Mark the midpoint of this line, which often corresponds to the point at which the external jugular vein crosses the posterior border of sternocleidomastoid. This is the point at which the branches of the superficial cervical plexus emerge from deep to the muscle. This is the target for needle insertion (
Fig. 7.14).
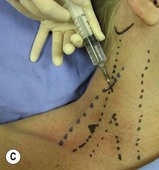
Technique
•
Prepare the field by cleaning the skin with an antiseptic solution and positioning sterile drapes.
•
Identify the target area for the initial needle insertion – the posterior border of sternocleidomastoid at the midpoint of a line connecting the mastoid process to the transverse process of C6.
•
Raise a superficial weal of local anaesthetic at the needle insertion site.
•
Puncture the skin at the target point with a 25 mm to 50 mm nerve-block needle.
•
Inject 10 mL of local anaesthetic subcutaneously along the posterior border of sternocleidomastoid, and just deep to the muscle itself. Use a fan technique to distribute local anaesthetic 30 to 40 mm superior and inferior to the puncture site (
Fig. 7.15A–C).
•
Avoid deep needle insertion (not more than 10 to 20 mm), and do not advance the needle towards the brachial plexus.
•
Subcutaneous midline infiltration of local anaesthetic along a line from the thyroid cartilage to the suprasternal notch will block nerve branches that cross from the contralateral side.
•
Aspirate intermittently to avoid intravascular injection.
•
Onset of anaesthesia will be within 10 to 20 minutes.