CHAPTER 2 Anatomy of the Elbow Joint
This chapter discusses the normal anatomy of the elbow region. Abnormal and surgical anatomy is addressed in subsequent chapters of this book dealing with the pertinent condition.
TOPICAL ANATOMY AND GENERAL SURVEY
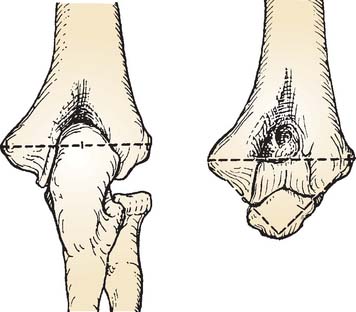
The contours of the biceps muscle and antecubital fossa are easily observed anteriorly. Laterally, the avascular interval between the brachioradialis and the triceps, the so-called column, is an important palpable landmark for surgical exposures (Fig. 2-1). Laterally, the tip of the olecranon, the lateral epicondyle, and the radial head also form an equilateral triangle and provide an important landmark for joint aspiration and for elbow arthro-scopy (see Chapters 37 and 77). The flexion crease of the elbow is in line with the medial and lateral epicondyles and thus is actually 1 to 2 cm proximal to the joint line when the elbow is extended (Fig. 2-2). The inverted triangular depression on the anterior aspect of the extremity distal to the epicondyles is called the cubital (or antecubital) fossa.
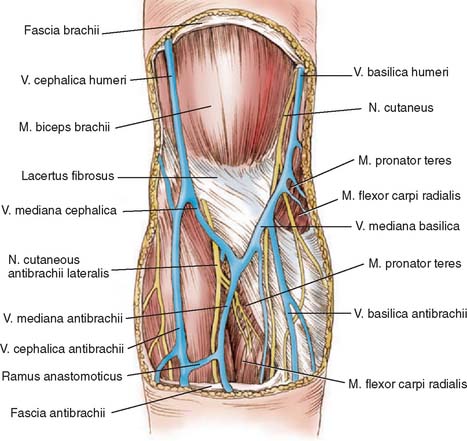
The superficial cephalic and basilic veins are the most prominent superficial major contributions of the anterior venous system and communicate by way of the median cephalic and median basilic veins to form an “M” pattern over the cubital fossa (Fig. 2-3).
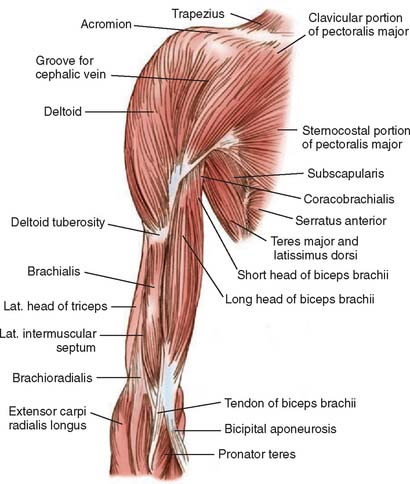
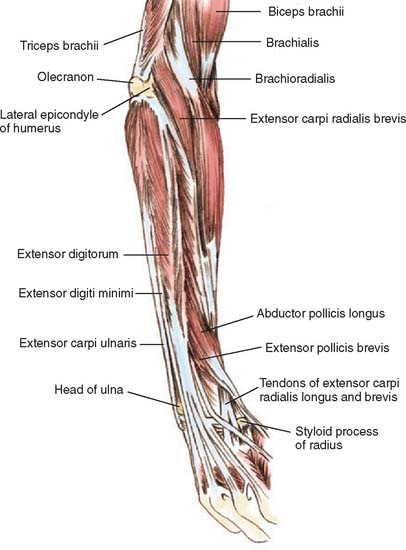
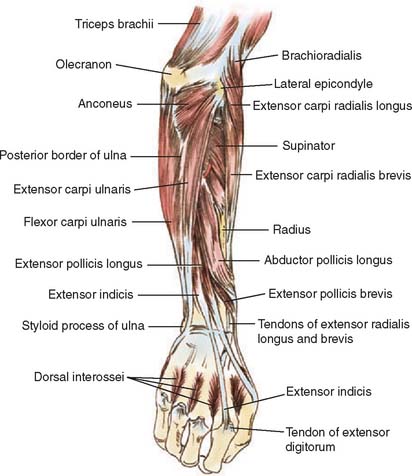
The extensor forearm musculature originates from the lateral epicondyle and was termed the mobile wad by Henry.37 This forms the lateral margin of the antecubital fossa and the lateral contour of the forearm and comprises the brachioradialis and the extensor carpi radialis longus and brevis muscles. The muscles comprising the contour of the medial anterior forearm include the pronator teres, flexor carpi radialis, palmaris longus, and flexor carpi ulnaris. Henry has demonstrated that their relationship and location can be approximated by placing the opposing thumb and the index, long, and ring fingers over the anterior medial forearm. The dorsum of the forearm is contoured by the lateral extensor musculature, consisting of the anconeus, extensor carpi ulnaris, extensor digitorum quinti, and extensor digitorum communis.
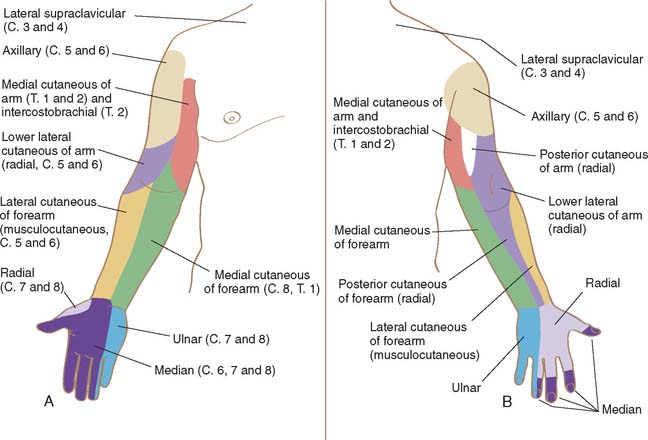
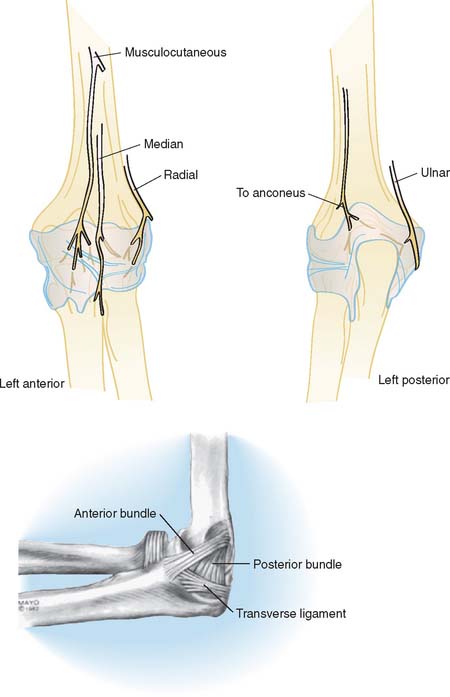
Dermal innervation about the proximal elbow is rather variable being provided by the lower lateral cutaneous (C5, C6) and medial cutaneous (radial nerve, C8, T1 and T2) nerves of the arm. The forearm skin is innervated by the medial (C8, T1), lateral (musculocutaneous, C5, C6), and posterior (radial nerve, C6-8) cutaneous nerves of the forearm (Fig. 2-4).
OSTEOLOGY
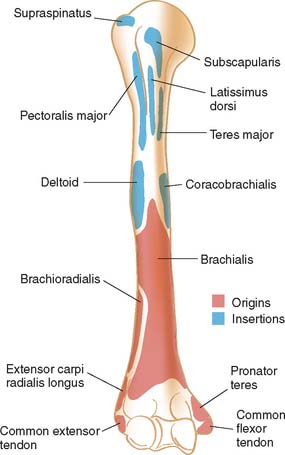
HUMERUS
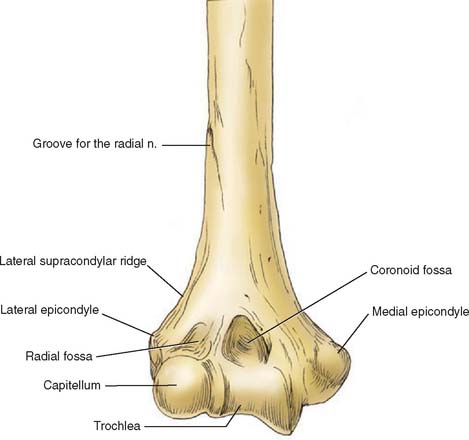
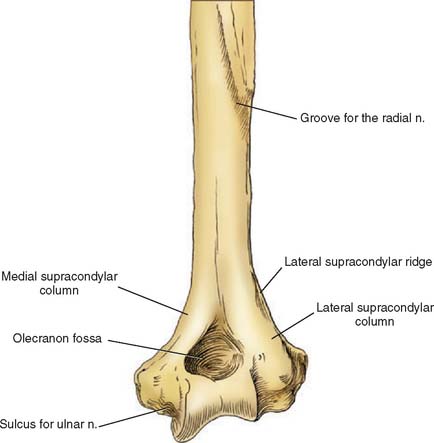
The distal humerus consists of an arch formed by two condyles that contain the articular surfaces of the trochlea and capitellum (Fig. 2-5).
In about 90% of individuals,86 a thin membrane of bone separates the olecranon and coronoid fossae (Fig. 2-6). The medial supracondylar column is smaller than the lateral and explains the vulnerability of the medial column to fracture with trauma and some surgical procedures.56 The posterior aspect of the lateral supracondylar column is flat, allowing ease of application of contoured plates (see Chapter 22). The prominent lateral supracondylar ridge serves as attachment for the brachioradialis and extensor carpi radialis longus muscles anteriorly and for the triceps posteriorly. It is also an important landmark for many lateral surgical approaches especially for the “column procedure” (see Chapters 7 and 32).
Proximal to the medial epicondyle, about 5 to 7 cm along the medial intramuscular septum, a supracondylar process is observed in 1% to 3% of individuals45,49,81 (Fig. 2-7). A fibrous band termed the ligament of Strothers may originate from this process and attach to the medial epicondyle.38 When present, this spur serves as an anomalous insertion of the coracobrachialis muscle and an origin of the pronator teres muscle.34 Various pathologic processes have been associated with the supracondylar process, including fracture45 and median4 and ulnar nerve38 entrapment (see Chapter 80).
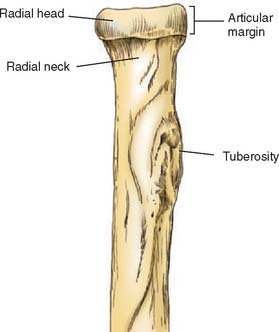
RADIUS
The radial head defines the proximal radius and articulates with the capitellum. It exhibits a cylindrical shape with a depression in the midportion to accommodate the capitellum. The disc-shaped head is secured to the ulna by the annular ligament (Fig. 2-8). Distal to the radial head, the bone tapers to form the radial neck, which, along with the head, is vulnerable to fracture.83 The radial tuberosity marks the distal aspect of the neck and has two distinct parts. The anterior surface is covered by a bicipitoradial bursa protecting the biceps tendon during full pronation (Fig. 2-9). However, it is the rough posterior aspect that provides the site of attachment of the biceps tendon. During full pronation the tuberosity is in a dorsal position and allows repair of a ruptured biceps tendon through a posterior approach12 (see Chapter 34) and is helpful to determine axial alignment of proximal radial fractures.26
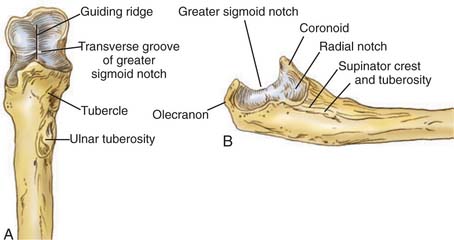
ULNA
The proximal ulna provides the greater sigmoid notch (incisura semilunaris), which serves as the major articulation of the elbow that is responsible for its inherent stability (Fig. 2-10). The cortical surface of the coronoid process serves as the site of insertion of the brachialis muscle and of the oblique cord. Medially the sublime tubercle serves as insertion site of the medial ulnar collateral ligament. The triceps tendon attaches to the posterior aspect of the olecranon process.
On the lateral aspect of the coronoid process, the lesser semilunar or radial notch articulates with the radial head and is oriented roughly perpendicular to the long axis of the bone. Distal to this the supinator crest serves as attachment to the supinator muscle, a tuberosity occurs on this crest, which is the site of insertion of the lateral ulnar collateral ligament.52,56,66
ELBOW JOINT STRUCTURE
ARTICULATION
The elbow joint articulation is classified as a trochoginglymoid joint.77 The ulnohumeral joint resembles a hinge (ginglymus), allowing flexion and extension. The radiohumeral and proximal radioulnar joint allows axial rotation or a pivoting (trochoid) type of motion.
Humerus
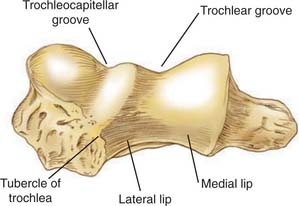
The trochlea is the hyperboloid, pulley-like surface that articulates with the semilunar notch of the ulna covered by articular cartilage through an arc of 300 degrees42,73,77 (Fig. 2-11). The medial contour is larger and projects more distally than does the lateral portion of the trochlea (Fig. 2-12). The two surfaces are separated by a groove that courses in a helical manner from an anterolateral to a posteromedial direction.
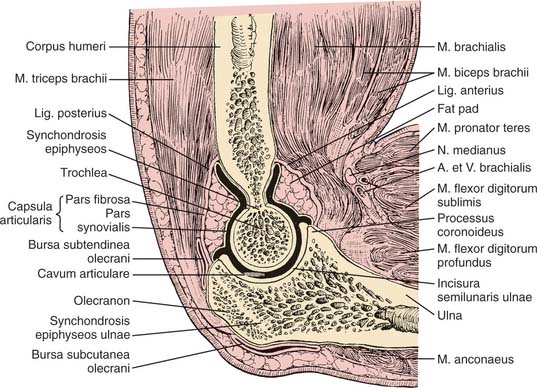
FIGURE 2-11 Sagittal section through the elbow region, demonstrating the high degree of congruity.
(Redrawn from Anson, B. J., and McVay, C. B.: Surgical Anatomy, Vol. 2, 5th ed. Philadelphia, W. B. Saunders Co., 1971.)
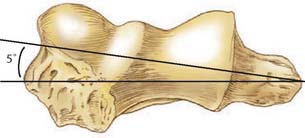
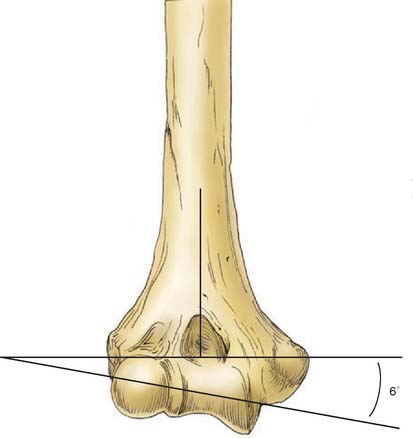
In the lateral plane, the orientation of the articular surface of the distal humerus is rotated anteriorly about 30 degrees with respect to the long axis of the humerus (Fig. 2-13). The center of the concentric arc formed by the trochlea and capitellum is on a line that is coplanar to the anterior distal cortex of the humerus.58 In the transverse plane, the articular surface and axis of rotation is rotated inward approximately 5 degrees (Fig. 2-14), and in the frontal plane, it is tilted approximately 6 degrees in valgus43,47,80 (Fig. 2-15).
Proximal Radius
Hyaline cartilage covers the depression of the radial head, which has an angular arc of about 40 degrees,77 as well as approximately 240 degrees of articular cartilage that articulates with the ulna, hence approximately 120 degrees of the radial circumference is not articular and amenable to open reduction internal fixation (ORIF) for fracture16 (Fig. 2-16). The lesser sigmoid fossa forms an arc of approximately 60 to 80 degrees,42,77 leaving an excursion of about 180 degrees for pronation and supination. The anterolateral third of the circumference of the radial head is void of cartilage. This part of the radial head lacks subchondral bone and thus is not as strong as the part that supports the articular cartilage; this part has been demonstrated to be the portion most often fractured.83 The head and neck are not co-linear with the rest of the bone and form an angle of approximately 15 degrees, with the shaft of the radius directed away from the radial tuberosity28 (Fig. 2-17).
Proximal Ulna
In most individuals, a transverse portion of non-articular cartilage divides the greater sigmoid notch into an anterior portion comprising the coronoid and the posterior olecranon (Fig. 2-18).
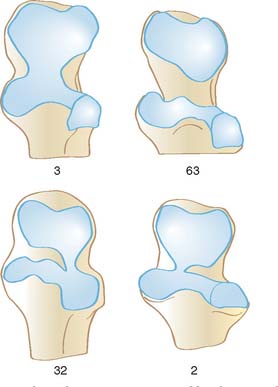
FIGURE 2-18 The relative percentage of hyaline cartilage distribution at the proximal ulna.
(Redrawn from Tillmann, B.: A Contribution to the Function Morphology of Articular Surfaces. Translated by G. Konorza. Stuttgart, George Thieme, Publishers; P. S. G. Publishing Co., Littleton, Mass., 1978.)
In the lateral plane, the sigmoid notch forms an arc of about 190 degrees.74 The contour is not a true hemicircle but rather is elipsoid. This explains the articular void in the midportion.85
The orientation of the articulation is oriented approximately 30 degrees posterior to the long axis of the bone (Fig. 2-19). This matches the 30 degrees anterior angulation of the distal humerus, providing stability in full extension (see Chapter 3). In the frontal plane, the shaft is angulated from about 1 to 6 degrees43,47,73 lateral to the articulation (Fig. 2-20). This angle contributes, in part, to the variation of the carrying angle, which is discussed in Chapter 3.
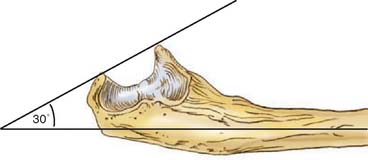
FIGURE 2-19 The greater sigmoid notch opens posteriorly with respect to the long axis of the ulna. This matches the 30-degree anterior rotation of the distal humerus, as shown in Figure 2-13.
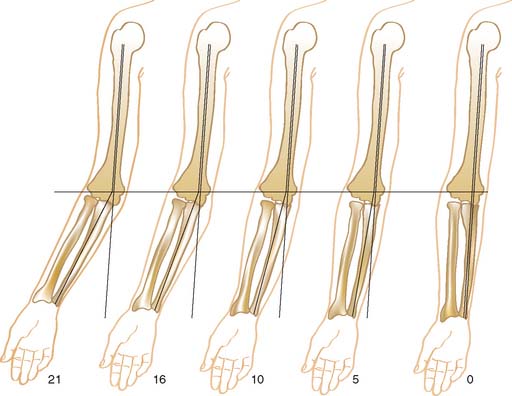
CARRYING ANGLE
The so-called carrying angle is the angle formed by the long axes of the humerus and the ulna with the elbow fully extended (Fig. 2-21). In men, the mean carrying angle is 11 to 14 degrees, and in women, it is 13 to 16 degrees.3,43,69 Furthermore, the carrying angle is approximately 1 degree greater in the dominant than nondominant side.88
JOINT CAPSULE
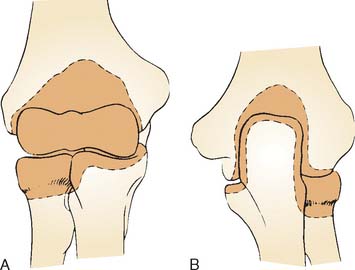
The anterior capsule inserts proximally above the coronoid and radial fossae (Fig. 2-22). Distally, the capsule attaches to the anterior margin of the coronoid medially as well as to the annular ligament laterally. Posteriorly, the capsule attaches just above the olecranon fossa, distally along the supracondylar bony columns. Distally, attachment is along the medial and lateral articular margin of the sigmoid notch. The greatest capacity of the elbow occurs at about 80 degrees of flexion40,70 and is 25 to 30 mL.70
The anterior capsule is normally a thin transparent structure but significant strength is provided by transverse and obliquely directed fibrous bands23,56 (Fig. 2-23). The anterior structure is, of course, taut in extension but becomes lax in flexion. The joint capsule is innervated by highly variable branches from all major nerves crossing the joint, including the contribution from the musculoskeletal nerve (Fig. 2-24).
LIGAMENTS
Medial Collateral Ligament Complex
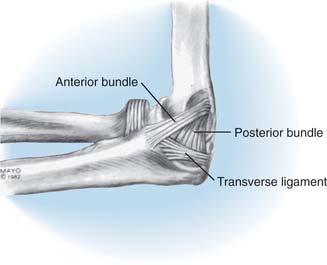
The medial collateral ligament consists of three parts: anterior, posterior, and transverse segments (Fig. 2-25). The anterior bundle is the most discrete component, the posterior portion being a thickening of the posterior capsule, and is well defined only in about 90 degrees of flexion. The transverse component (ligament of Cooper) appears to contribute little or nothing to elbow stability.
The ligament originates from a broad anteroinferior surface of the epicondyle.65 The ulnar nerve rests on the posterior aspect of the medial epicondyle but is not intimately related to the fibers of the anterior bundle of the medial collateral ligament itself. This has obvious implications with regard to the treatment of ulnar nerve decompression by medial epicondylar ostectomy. A more obliquely oriented excision might be most appropriate to both decompress the ulnar nerve and preserve the collateral ligament origin. On the lateral projection, the origin of the anterior bundle of the medial collateral ligament is precisely at the axis of rotation at the anterior, inferior margins of the medial epicondyle62 (Fig. 2-26). The posterior bundle inserts along the midportion of the medial margin of the semilunar notch. The width of the anterior bundle is approximately 4 to 5 mm compared with 5 to 6 mm at the midportion of the fan-shaped posterior segment.56 Recently ultrasound assessment has proved helpful in further documenting the dimensions of these structures.61
The function of the ligamentous structures is discussed in detail below. Clinically and experimentally, the anterior bundle is clearly the major portion of the medial ligament complex59 and has been divided into anterior, posterior and deep medial subcomponents.62
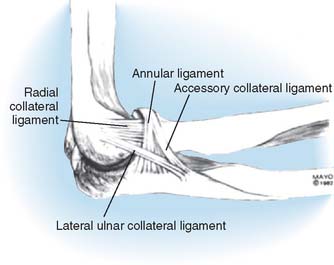
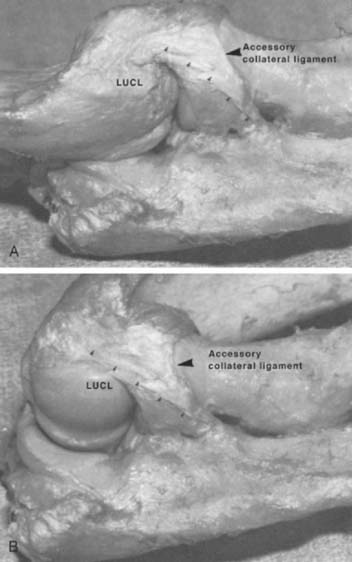
Lateral Ligament Complex
Unlike the medial collateral ligament complex, with its rather consistent pattern, the lateral ligaments of the elbow joint are less discrete, and individual variation iscommon.30,31,40,75 Our investigation has suggested that several components make up the lateral ligament complex: (1) the radial collateral ligament, (2) the annular ligament, (3) a variably present accessory lateral collateral ligament, and (4) the lateral ulnar collateral ligament. These observations have now been confirmed by others. The current thinking is to consider the complex to be roughly in the shape “Y,” the arms of which attach to the anterior and posterior aspect of the semilunar notch13,72 (Fig. 2-27).

FIGURE 2-27 Dissection demonstrating the “Y” orientation of the lateral collateral ligament complex.
Radial Collateral Ligament
This structure originates from the lateral epicondyle and is actually a complex of several components (Fig. 2-28). Its superficial aspect provides a source of origin for a portion of the supinator muscle. The length averages approximately 20 mm with a width of approximately 8 mm. This portion of the ligament is almost uniformly taut throughout the normal range of flexion and extension, indicating that the origin of the ligament is very near the axis of flexion (Fig. 2-29).
Annular Ligament
A strong band of tissue originating and inserting on the anterior and posterior margins of the lesser sigmoid notch forms the annular ligament and maintains the radial head in contact with the ulna. The ligament is tapered distally to give the shape of a funnel and contributes about four fifths of the fibro-osseous ring.52 The structure is not as simple as it appears because fibers arc medially and laterally to secure the annular ligament to the ulna.72 A synovial reflection extends distal to the lower margin of the annular ligament, forming the sacciform recess. The radial head is not a pure circular disc76; thus, it has been observed that the anterior insertion becomes taut during supination and the posterior aspect becomes taut during extremes of pronation.88
Lateral Ulnar Collateral Ligament
In 1985 Morrey and An first described the so-called lateral ulnar collateral ligament.56 Before this, however, Martin haddescribed a lateral ligament complex including “…additional fibers inserting from the tubercle of the supinator crest to the humerus.” This structure subsequently has been demonstrated to be invariably present and critically important clinically. It originates from the lateral epicondyle and blends with the fibers of the annular ligament arching superficial and distal to it.66 The insertion is at the tubercle of the crest of the supinator on the ulna. Although the origin blends with the origin of the lateral collateral ligament complex occupying the posterior portion, the insertion is more discrete at the tubercle (Fig. 2-30). The function of this ligament is to provide stability to the ulnohumeral joint and was shown to be deficient in posterolateral rotatory instability of the joint.64,65 As confirmed by several subsequent assessments, the key factor is that this ligament represents the primary lateral stabilizer of the elbow and is taut in flexion and extension (Fig. 2-31).
Accessory Lateral Collateral Ligament
This definition has been applied by Martin to the ulnar insertion of discrete fibers on the tubercle of the supinator as described previously. Others have termed this the lateral arm of the “Y” ligament.72 Proximally, the fibers tend to blend with the inferior margin of the annular ligament (see Fig. 2-27). Its function is to further stabilize the annular ligament during varus stress.
Quadrate Ligament
A thin, fibrous layer covering the capsule between the inferior margin and the annular ligament and the ulna is referred to as the quadrate ligament20,60 or the ligament of Denucè.76 Spinner and Kaplan have demonstrated a functional role for the structure, describing the anterior part as a stabilizer of the proximal radial ulnar joint during full supination.76 The weaker posterior attachment stabilizes the joint in full pronation.
Oblique Cord
The oblique cord is a small and inconstant bundle of fibrous tissue formed by the fascia overlying the deep head of the supinator and extending from the lateral side of the tuberosity of the ulna to the radius just below the radial tuberosity (see Fig. 2-23). Although the morphologic significance is debatable53,76 and the structure is not considered to be of great functional consequence,31 it has been noted to become taut in full supination, and contracture of the oblique cord has been implicated in the etiology of idiopathic limitation of forearm supination.10 At this point, we consider this structure as a curiosity.
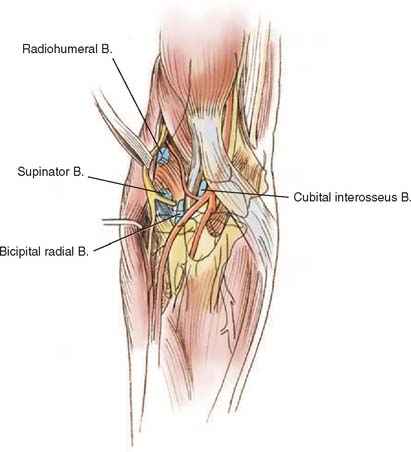
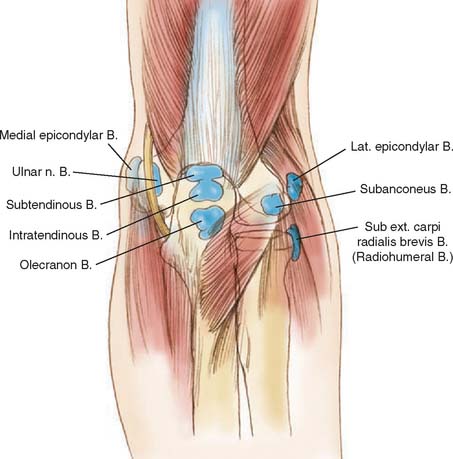
Bursae
The bursae were first detailed by Monro in 1788, and several bursae have been described at the elbow joint.55 Lanz recognized seven bursae, including three associated with the triceps.52 On the posterior aspect of the elbow, the superficial olecranon bursa, which develops around age 7 years,18 between the olecranon process and the subcutaneous tissue is wellknown33 (Fig. 2-32). A deep subtendinous bursa is present as the triceps inserts on the tip of the olecranon. An occasional deep subtendinous bursa is likewise present between the tendon and the tip of the olecranon. A bursa has also even been described deep to the anconeus muscle in about 12% of subjects by Henle,36 but we have not appreciated such a structure during more than 500 exposures of this region. On the medial and lateral aspects of the joint, the subcutaneous medial epicondylar bursa is frequently present, and the lateral subcutaneous epicondylar bursa occasionally has been observed. The radiohumeral bursa lies deep to the common extensor tendon, below the extensor carpi radialis brevis and superficial to the radiohumeral joint capsule. This entity has been implicated by several authors17,67 in the etiology of lateral epicondylitis but is probably not a major factor. The constant bicipitoradial bursa separates the biceps tendon from the tuberosity of the radius (see Fig. 2-9). Less commonly appreciated is the deep cubital interosseous bursa lying between the lateral aspect of the biceps tendon and the ulna, brachialis, and supinator fascia. This bursa is said to be present in about 20% of individuals.75 The clinical significance of the relevant bursae about the elbow is detailed in Chapter 85.
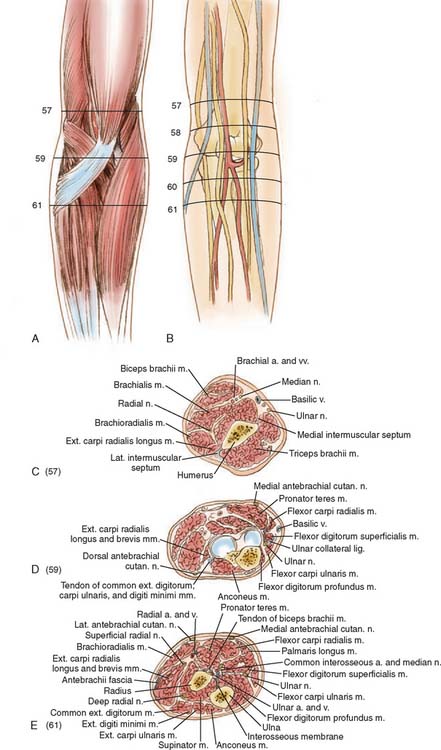
VESSELS
BRACHIAL ARTERY AND ITS BRANCHES
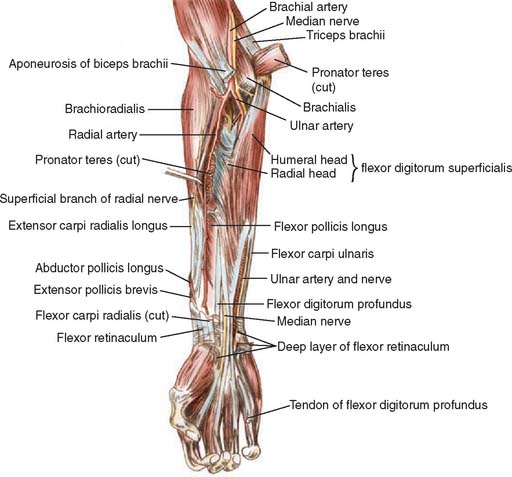
The cross-sectional relationship of the vessels, nerves, muscles, and bones is shown in Figure 2-33. The brachial artery descends in the arm, crossing in front of the intramuscular septum to lie anterior to the medial aspect of the brachialis muscle. The median nerve crosses in front of and medial to the artery at this point, near the middle of the arm (Fig. 2-34). The artery continues distally at the medial margin of the biceps muscle and enters the antecubital space medial to the biceps tendon and lateral to the nerve (Fig. 2-35). At the level of the radial head, it gives off its terminal branches, the ulnar and radial arteries, which continue into the forearm.
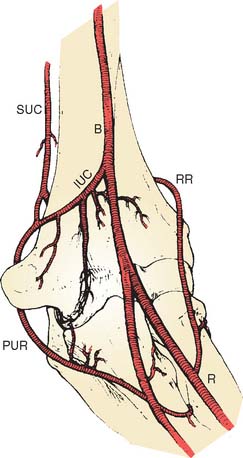
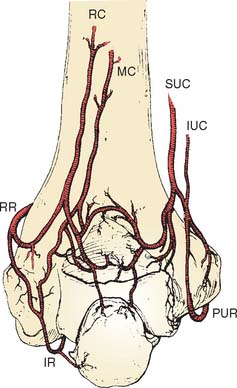
The detailed vascular anatomy of the elbow region has been nicely described recently in great detail by Yamaguchi et al.89 The major branches of the brachial artery are the superior and inferior ulnar collateral arteries, which originate medial and distal to the profunda brachial artery. The superior ulnar collateral artery is given off just distal to the midportion of the brachium, penetrates the medial intermuscular septum, and accompanies the ulnar nerve to the medial epicondyle, where it terminates by anastomosing with the posterior ulnar recurrent artery and variably with the inferior ulnar collateral artery (Fig. 2-36).
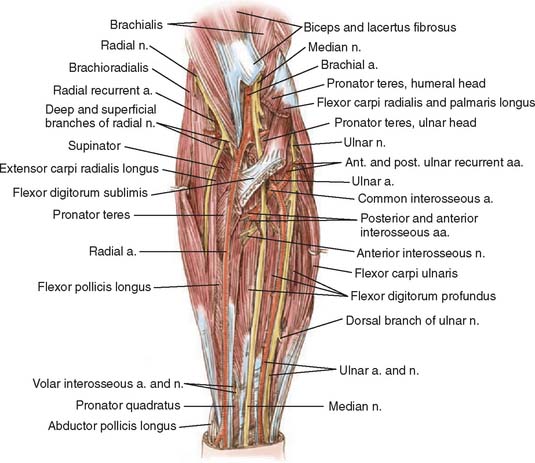
RADIAL ARTERY
The radial artery typically originates at the level of the radial head, emerges from the antecubital space between the brachioradialis and the pronator teres muscle, and continues down the forearm under the brachioradialis muscle. A more proximal origin occurs in up to 15% of individuals.54 The radial recurrent artery originates laterally from the radial artery just distal to its origin. It ascends laterally on the supinator muscle to anastomose with the radial collateral artery at the level of the lateral epicondyle, to which it provides circulation. For better visualization, the radial recurrent artery sometimes is sacrificed with the anterior elbow exposure.
ULNAR ARTERY
The larger of the two terminal branches of the brachial artery is the ulnar artery. There is relatively little variation in its origin, which is usually at the level of the radial head. The artery traverses the pronator teres between its two heads and continues distally and medially behind the flexor digitorum superficialis muscle. It emerges medially to continue down the medial aspect of the forearm under the cover of the flexor carpi ulnaris. Two recurrent branches originate just distal to the origin of the ulnar artery. The anterior ulnar recurrent artery ascends deep to the humeral head of the pronator teres and deep to the medial aspect of the brachialis muscle to anastomose with the descending superior and inferior ulnar collateral arteries. The posterior ulnar recurrent artery originates with or just distal to the smaller anterior ulnar recurrent artery and passes proximal and posterior between the superficial and deep flexors posterior to the medial epicondyle. This artery continues proximally with the ulnar nerve under the flexor carpi ulnaris to anastomose with the superior ulnar collateral artery. Additional extensive communication with the inferior ulnar and middle collateral branches constitutes the rete articulare cubiti (see Fig. 2-35).
The common interosseous artery is a large vessel originating 2.5 cm distal to the origin of the ulnar artery. It passes posteriorly and distally between the flexor pollicis longus and the flexor digitorum profundus just distal to the oblique cord, dividing into anterior and posterior interosseous branches. The interosseous recurrent artery originates from the posterior interosseous branch. This artery runs proximally through the supinator muscle to anastomose with the vascular network of the olecranon (see Fig. 2-36).
NERVES
Specific clinical and pertinent anatomic aspects of the nerves in the region of the elbow are discussed in subsequent chapters as appropriate. A general survey of the common anatomic patterns is given here (see Fig. 2-33).
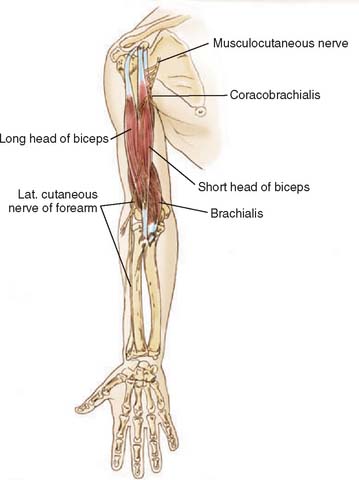
MUSCULOCUTANEOUS NERVE
The musculocutaneous nerve originates from C5-8 nerve roots and is a continuation of the lateral cord. It innervates the major elbow flexors, the biceps and brachialis, and continues through the brachial fascia lateral to the biceps tendon, terminating as the lateral antebrachial cutaneous nerve (Fig. 2-37). The motor branch enters the biceps and the brachialis approximately 15 and 20 cm below the tip of the acromion, respectively.48
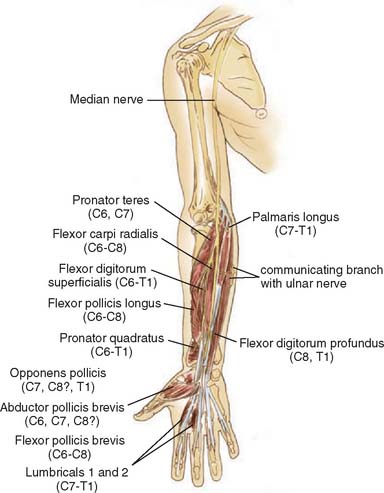
MEDIAN NERVE
Arising from the C5-8 and T1 nerve roots, the median nerve enters the anterior aspect of the brachium, crossing in front of the brachial artery as it passes across the intermuscular septum. It follows a straight course into the medial aspect of the antecubital fossa, medial to the biceps tendon and the brachial artery. It then passes under the bicipital aponeurosis. The first motor branch is provided to the pronator teres, through which it passes.2,39 It enters the forearm and continues distally under the flexor digitorum superficialis within the fascial sheath of this muscle.
There are no branches of the median nerve in the arm (Fig. 2-38). In the cubital fossa, a few small articular branches are given off before the motor branches to the pronator teres, the flexor carpi radialis, the palmaris longus, and the flexor digitorum superficialis. Because all branches arise medially, medial retraction of the nerve during exposure of the anterior aspect of the elbow is a safe technique.
RADIAL NERVE
The radial nerve is a continuation of the posterior cord and originates from the C6, C7, and C8 nerve roots withvariable contributions of the C5 and T1 roots. In the midportion of the arm, the nerve courses laterally just distal to the deltoid insertion to occupy the spiral groove in the humerus that bears its name. Before entering the anterior aspect of the arm, it gives off motor branches to the medial and lateral head of the triceps, accompanied by the deep branch of the brachial artery. It then emerges inferiorly and laterally to penetrate the lateral intermuscular septum. The nerve is at risk for injury from surgery or fracture at this site. Two recent studies have placed the position of the radial nerve as 54% of the acromion/ulnar distance22 or 1.7% of the transcondylar distance.41 After penetrating the lateral intermuscular septum in the distal third of the arm, it descends anterior to the lateral epicondyle behind the brachioradialis. It innervates the brachioradialis with a single branch to this muscle. In the antecubital space, the nerve divides into the superficial and deep branches. The superficial branch is a continuation of the radial nerve and extends into the forearm to innervate the mid-dorsal cutaneous aspect of the forearm (Fig. 2-39).
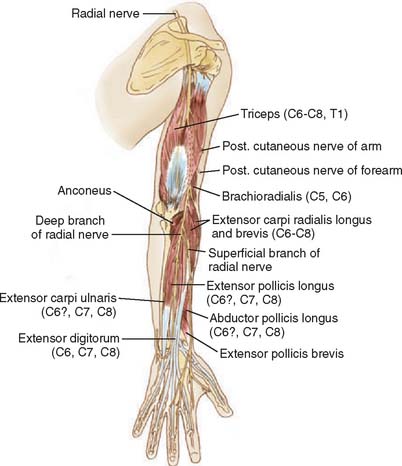
FIGURE 2-39 The muscles innervated by the right radial nerve.
(Redrawn from Langman, J., and Woerdeman, M. W.: Atlas of Medical Anatomy. Philadelphia, W. B. Saunders Co., 1976.)
The motor branches of the radial nerve are given off to the triceps above the spiral groove except for the branch to the medial head of the triceps, which originates at the entry to the spiral groove. This branch continues distally through the medial head to terminate as a muscular branch to the anconeus. This accounts for the variability of the anconeus when rotated or reflected from its origin.11,44,68
In the antecubital space, the recurrent radial nerve curves around the posterolateral aspect of the radius, passing deep to the supinator muscle, which it innervates. During its course through the supinator muscle, the nerve lies over a bare area, which is distal to and opposite to the radial tuberosity.23 The nerve is believed to be at risk at this site with fractures of the proximal radius.79 It emerges from the muscle as the posterior interosseous nerve, and the recurrent branch innervates the extensor digitorum minimi, the extensor carpi ulnaris, and occasionally, the anconeus. The posterior interosseous nerve is accompanied by the posterior interosseous artery and sends further muscle branches distally to supply the abductor pollicis longus, the extensor pollicis longus, the extensor pollicis brevis, and the extensor indicis on the dorsum of the forearm. The nerve is subject to compression as it passes through the supinator muscle15 or from synovial proliferation.25,28 Compression and entrapment problems are described in detail in Chapter 81.
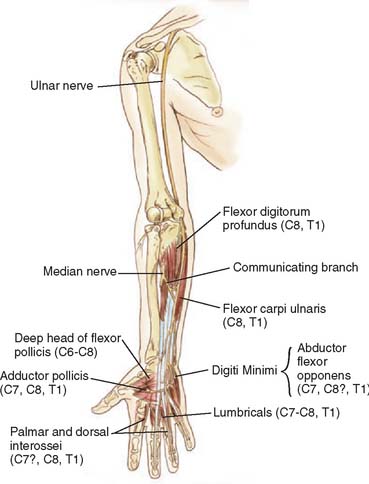
ULNAR NERVE
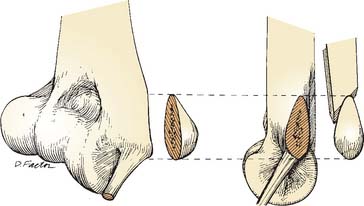
The ulnar nerve is derived from the medial cord of the brachial plexus from roots C8 and T1. In the midarm, it passes posteriorly through the medial intermuscular septum and continues distally anterior to the septum and under the medial margin of the triceps. It is accompanied by the superior ulnar collateral branch of the brachial artery and the ulnar collateral branch of the radial artery. Although supposedly there are no branches of this nerve in the brachium, an occasional motor branch to the triceps is encountered (Fig. 2-40). The ulnar nerve passes into the cubital tunnel under the medial epicondyle and rests against the posterior portion of the medial collateral ligament, where a groove in the ligament accommodates this structure. The roof of the cubital tunnel recently has been defined and termed the cubital tunnel retinaculum.64 Retinacular absence accounts for congenital subluxation of the ulnar nerve. Furthermore, the structure flattens with elbow flexion, thus decreasing the capacity of the cubital tunnel (Fig. 2-41).64 This accounts for the clinical observation of ulnar nerve paresthesia with elbow flexion. Similarly, elbow instability can cause traction injury to the nerve.51
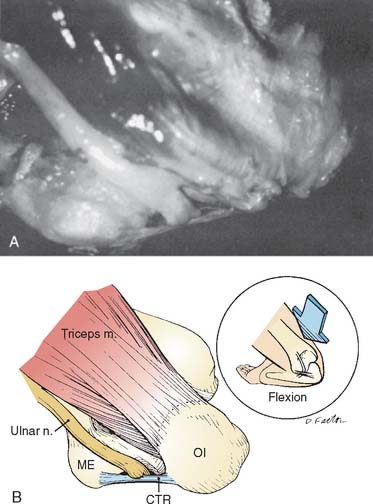
FIGURE 2-41 With flexion the cubital tunnel flattens, compressing the ulnar nerve (A and B).
(Redrawn from O’Driscoll, S. W., Horii, E., Carmichael, S. W., and Morrey, B. F.: The cubital tunnel and ulnar neuropathy. J. Bone Joint Surg. 73B:613, 1991.)
A few small capsular twigs are given to the elbow joint in this region.8 As the nerve enters the forearm between the two heads of the flexor carpi ulnaris, it gives off a single nerve to the ulnar origin of the pronator and one to the epicondylar head of the flexor carpi ulnaris. Distally, the nerve sends a motor branch to the ulnar half of the flexor digitorum profundus. Two cutaneous nerves arise from the ulnar nerve in the distal half of the forearm and innervate the skin of the wrist and the ulnar two digits of the hand.
MUSCLES
ELBOW FLEXORS
Biceps
The biceps covers the brachialis muscle in the distal arm and passes into the cubital fossa as the biceps tendon, which attaches to the posterior aspect of the radial tuberosity (Fig. 2-42). The constant bicipitoradial bursa separates the tendon from the anterior aspect of the tuberosity, and the cubital bursa has been described as separating the tendon from the ulna and the muscles covering the radius (see Fig. 2-9). The bicipital aponeurosis, or lacertus fibrosus, is a broad, thin band of tissue that is a continuation of the anterior medial and distal muscle fasciae. It runs obliquely to cover the median nerve and brachial artery and inserts into the deep fasciae of the forearm and possibly into the ulna as well.19
The biceps is a major flexor of the elbow that has a large cross-sectional area but an intermediate mechanical advantage because it passes relatively close to the axis of rotation. In the pronated position, the biceps is a strong supinator.6 The distal insertion may undergo spontaneous rupture,57,78 and this condition is discussed in detail later (Chapter 34).
Brachialis
This muscle has the largest cross-sectional area of any of the elbow flexors but suffers from a poor mechanical advantage because it crosses so close to the axis of rotation. The origin consists of the entire anterior distal half of the humerus, and it extends medially and laterally to the respective intermuscular septa (Fig. 2-43). The muscle crosses the anterior capsule, with some fibers inserting into the capsule that are said to help retract the capsule during elbow flexion. The major attachment is to the coronoid process about 2 mm distal from its articular margin. More than 95% of the cross-sectional area is muscle tissue at the elbow joint,50 a relationship that may account for the high incidence of trauma to this muscle and the development of myositis ossificans with elbow dislocation.84
Brachioradialis
The brachioradialis has a lengthy origin along the lateral supracondylar bony column that extends proximally to the level of the junction of the mid and distal humerus (see Fig. 2-43). The origin separates the lateral head of the triceps and the brachialis muscle. The lateral border of the cubital fossa is formed by this muscle, which crosses the elbow joint with the greatest mechanical advantage of any elbow flexor. It progresses distally to insert into the base of the radial styloid (Figs. 2-44 and 2-45). The muscle protects and is innervated by the radial nerve (C5, C6) as it emerges from the spiral groove. Its major function is elbow flexion. Rarely, the muscle may be ruptured.35
Extensor Carpi Radialis Longus
The extensor carpi radialis longus originates from the supracondylar bony column joint just below the origin of the brachioradialis (see Fig. 2-44). The origin of this muscle is identified as the first fleshy fibers observed proximal to the common extensor tendon. As it continues into the midportion of the dorsum of the forearm, it becomes largely tendinous and inserts into the dorsal base of the second metacarpal. Innervated by the radial nerve (C6, C7), the motor branches arise just distal to those of the brachioradialis muscle.
In addition to wrist extension, its orientation suggests that this muscle might function as an elbow flexor.
Clinically, the origin of this muscle and its relationship with that of the extensor carpi radialis brevis have been implicated in the pathologic anatomy of tennis elbow by Nirschl (Chapter 44).
Extensor Carpi Radialis Brevis
The extensor carpi radialis brevis originates from the lateral superior aspect of the lateral epicondyle (see Fig. 2-43). Its origin is the most lateral of the extensor group and is covered by the extensor carpi radialis longus. This relationship is important as the most commonly implicated site of lateral epicondylitis. The extensor digitorum communis originates from the common extensor tendon and is just medial or ulnar to the extensor carpi radialis brevis. At its humeral origin, the fibers of the extensor digitorum communis and brevis are grossly and histologically indistinguishable from one another32 (see Fig. 2-44). The longus and brevis shares the same extensor compartment as they cross the wrist under the extensor retinaculum. The brevis inserts into the dorsal base of the third metacarpal. The function of the extensor carpi radialis brevis is pure wrist extension, with little or no radial or ulnar deviation.1 The extensor carpi radialis brevis is innervated by fibers of the sixth and seventh cervical nerves. The motor branch arises from the radial nerve in the region of its division into deep and superficial branches.
Extensor Digitorum Communis
Originating from the anterior distal aspect of the lateral epicondyle, the extensor digitorum communis accounts for most of the contour of the extensor surface of the forearm (see Fig. 2-44). The muscle extends and abducts the fingers. According to Wright, the muscle can assist in elbow flexion when the forearm is pronated. This observation is not, however, supported by our cross-sectional studies.1 Innervation is from the deep branch of the radial nerve, with contributions from the sixth through eighth cervical nerves.
Extensor Carpi Ulnaris
The extensor carpi ulnaris originates from two heads, one above and the other below the elbow joint. The humeral origin is the most medial of the common extensor group (Fig. 2-46) (see also Fig. 2-43). The ulnar attachment is along the aponeurosis of the anconeus and at the superior border of this muscle. It is a valuable landmark for exposures of the lateral elbow joint. The insertion is on the dorsal base of the fifth metacarpal after crossing the wrist in its own compartment under the extensor retinaculum. The extensor carpi ulnaris is a wrist extensor and ulnar deviator. Fibers of the sixth through eighth cervical nerve routes innervate the muscle from branches of the deep radial nerve.
Supinator
This flat muscle is characterized by the virtual absence of tendinous tissue and a complex origin and insertion. It originates from three sites above and below the elbow joint: (1) the lateral anterior aspect of the lateral epicondyle; (2) the lateral collateral ligament; and (3) the proximal anterior crest of the ulna along the crista supinatoris. The form of the muscle is approximately that of a rhomboid, because it runs obliquely, distally, and radially to wrap around and insert diffusely on the proximal radius, beginning lateral and proximal to the radial tuberosity and continuing distal to the insertion of the pronator teres at the junction of the proximal and middle third of the radius (see Fig. 2-46). It is important to note that the radial nerve passes through the supinator to gain access to the extensor surface of the forearm. This anatomic feature is clinically significant with regard to exposure of the lateral aspect of the elbow joint and the proximal radius and in certain entrapment syndromes.76
The muscle obviously supinates the forearm but is a weaker supinator than the biceps.38 Unlike the biceps, however, the effectiveness of the supinator is not altered by the position of elbow flexion. The innervation is derived from the muscular branch given off by the radial nerve just before and during its course through the muscle with nerve fibers derived primarily from the sixth cervical root.
ELBOW EXTENSORS
Triceps Brachii
The entire posterior musculature of the arm is composed of the triceps brachii (see Fig. 2-39). The long head has a discrete origin from the infraglenoid tuberosity of the scapula. The lateral head originates in a linear fashion from the proximal lateral intramuscular septum on the posterior surface of the humerus. The medial head originates from the entire distal half of the posteromedial surface of the humerus bounded laterally by the radial groove and medially by the intramuscular septum. Thus, each head originates distal to the other, with progressively larger areas of origin. The long and lateral heads are superficial to the deep medial head, blending in the midline of the humerus to form a common muscle that then tapers into the triceps tendon and attaches to the tip of the olecranon with Sharpey’s fibers.14 The tendon usually is separated from the olecranon by the subtendinous olecranon bursa. The distal 40% of the triceps mechanism consists of a layer of fascia that blends with the triceps distally.
Innervated by the radial nerve, the long and lateral heads are supplied by branches that arise proximal to the entrance of the radial nerve into the groove. The medial head is innervated distal to the groove with a branch that enters proximally and passes through the entire medial head to terminate by innervating the anconeus, an anatomic feature of considerable importance when considering some approaches (e.g., Kocher, Bryan-Morrey, Boyd, and Pankovitch) to the joint.
Subanconeus Muscle
The attachment of some muscle fibers of the medial head of the triceps to the posteromedial capsule has been termed the subanconeus muscle. This may have some functional relevance of stabilizing the fat pad to help cushion the elbow as it comes into full extension.87
Anconeus
This muscle has little tendinous tissue because it originates from a rather broad site on the posterior aspect of the lateral epicondyle and from the lateral triceps fascia and inserts into the lateral dorsal surface of the proximal ulna (see Fig. 2-46). It is innervated by the terminal branch of the nerve to the medial head of the triceps. Curiously, the function of this muscle has been the subject of considerable speculation. Possibly the most accurate description of function is that proposed by Basmajian and Griffin and by DaHora, who suggest that its primary role is that of a joint stabilizer.5,21 The muscle covers the lateral portion of the annular ligament and the radial head. For the surgeon, the major significance of this muscle is its position as a key landmark in various lateral and posterolateral exposures and is emerging for usefulness reconstruction of the lateral elbow.
FLEXOR PRONATOR MUSCLE GROUP
Pronator Teres
This is the most proximal of the flexor pronator group. There are two heads of origin: The largest arises from the anterosuperior aspect of the medial epicondyle and the second from the coronoid process of the ulna, an attachment absent in about 10% of individuals39 (see Fig. 2-37). The two origins of the pronator muscle provide an arch through which the median nerve passes to gain access to the forearm. This anatomic characteristic is a significant feature in the etiology of the median nerve entrapment syndrome and is discussed in detail in Chapter 80. The common muscle belly proceeds radially and distally under the brachioradialis, inserting at the junction of the proximal and middle portions of the radius by a discrete broad tendinous insertion into a tuberosity on the lateral aspect of the bone. Obviously, a strong pronator of the forearm, it also is considered a weak flexor of the elbow joint.1,7,82 The muscle usually is innervated by two motor branches from the median nerve before the nerve leaves the cubital fossa.
Flexor Carpi Radialis
The flexor carpi radialis originates just inferior to the origin of the pronator teres and the common flexor tendon at the anteroinferior aspect of the medial epicondyle (see Fig. 2-43). It continues distally and radially to the wrist, where it can be easily palpated before it inserts into the base of the second and sometimes the third metacarpal. Proximally, the muscle belly partially covers the pronator teres and palmaris longus muscles and shares a common origin from the intermuscular septum, which it shares with these muscles. The innervation is from one or two twigs of the median nerve (C6, C7), and its chief function is as a wrist flexor. At the elbow no significant flexion moment is present.1,24
Palmaris Longus
This muscle, when present, arises from the medial epicondyle, and from the septa it shares with the flexor carpi radialis and flexor carpi ulnaris (see Fig. 2-43). It becomes tendinous in the proximal portion of the forearm and inserts into and becomes continuous with the palmar aponeurosis. It is absent approximately in 10% of extremities.71 Its major function is as a donor tendon for reconstructive surgery, and it is innervated by a branch of the median nerve.
Flexor Carpi Ulnaris
The flexor carpi ulnaris is the most posterior of the common flexor tendons originating from the medial epicondyle (see Figs. 2-38 and 2-43). A second and larger source of origin is from the medial border of the coronoid and the proximal medial aspect of the ulna. The ulnar nerve enters and innervates (T7-8 and T1) the muscle between these two sites of origin with two or three motor branches given off just after the nerve has entered the muscle. These are the first motor branches of the ulnar nerve, and therefore, they are useful in localizing the level of an ulnar nerve lesion. The muscle continues distally to insert into the pisiform, where the tendon is easily palpable, because it serves as a wrist flexor and ulnar deviator. With an origin posterior to the axis of rotation, weak elbow extension also may be provided by the flexor carpi ulnaris.1
Flexor Digitorum Superficialis
This muscle is deep to those originating from the common flexor tendon but superficial to the flexor digitorum profundus; thus, it is considered the intermediate muscle layer. This broad muscle has a complex origin (Fig. 2-47). Medially, it arises from the medial epicondyle by way of the common flexor tendon and possibly from the ulnar collateral ligament and the medial aspect of the coronoid.38 The lateral head is smaller and thinner and arises from the proximal two thirds of the radius. The unique origin of the muscle forms a fibrous margin under which the median nerve and the ulnar artery emerge as they exit from the cubital fossa. The muscle is innervated by the median nerve (C7, C8, T1) with branches that originate before the median nerve enters the pronator teres. The action of the flexor digitorum superficialis is flexion of the proximal interphalangeal joints.
1 An K.N., Hui F.C., Morrey B.F., Linscheid R.L., Chao E.Y. Muscles across the elbow joint: a biomechanical analysis. J. Biomechan.. 1981;14:659.
2 Anson B.J., McVay C.B.. 5th ed.. Surgical Anatomy, Vol. 2. W. B. Saunders Co., Philadelphia, 1971.
3 Atkinson W.B., Elftman H. The carrying angle of the human arm as a secondary sex character. Anat. Rec.. 1945;91:49.
4 Barnard L.B., McCoy S.M. The supracondyloid process of the humerus. J. Bone Joint Surg.. 1946;28:845.
5 Basmajian J.V., Griffin W.R. Function of anconeus muscle. J. Bone Joint Surg.. 1972;54A:1712.
6 Basmajian J.V., Latif A. Integrated actions and functions of the two flexors of the elbow: a detailed myographic analysis. J. Bone Joint Surg.. 1957;39A:1106.
7 Basmajian J.V., Travell A. Electromyography of the pronator muscles in the forearm. Anat. Rec.. 1961;139:45.
8 Bateman J.E. Denervation of the elbow joint for the relief of pain: a preliminary report. J. Bone Joint Surg.. 1948;30B:635.
9 Beetham W.P. Physical Examination of the Joints. Philadelphia: W. B. Saunders Co., 1965.
10 Bert J.M., Linscheid R.L., McElfresh E.C. Rotatory contracture of the forearm. J. Bone Joint Surg.. 1980;62A:1163.
11 Boyd H.B. Surgical exposure of the ulna and proximal third of the radius through one incision. Surg. Gynec. Obstet.. 1940;71:86.
12 Boyd H.D., Anderson L.D. A method for reinsertion of the biceps tendon brachii tendon. J. Bone Joint Surg.. 1961;43A:1141.
13 Bozkurt M., Acar H.I., Apaydin N., Leblebicioglu G., Elhan A., Tekdemir I., Tonuk E. The annular ligament: an anatomical study. Am. J. Sports Med.. 2005;33:114.
14 Bryan R.S., Morrey B.F. Extensive posterior exposure of the elbow: a triceps-sparing approach. Clin. Orthop.. 1982;166:188.
15 Capener N. The vulnerability of the posterior interosseous nerve of the forearm: a case report and anatomic study. J. Bone Joint Surg.. 1966;48B:770.
16 Caputo A.E., Mazzocca A.D., Santoro V.M. The nonarticulating portion of the radial head: anatomic and clinical correlations for internal fixation. J. Hand Surg.. 1998;23A(6):1082.
17 Carp L. Tennis elbow (epicondylitis) caused by radiohumeral bursitis. Arch. Surg.. 1932;24:905.
18 Chen J., Alk D., Eventov I., Weintroub S. Development of the olecranon bursa: an anatomic cadaver study. Acta Orthop. Scand.. 1987;58:408.
19 Congdon E.D., Fish H.S. The chief insertion of the biceps after neurosis in the ulna: a study of collagenous bundle patterns of antebrachial fascia and bicepital aponeurosis. Anat. Rec.. 1953;116:395.
20 Cunningham D.J.. Romanes G.J., editor. Textbook of Anatomy, 12th ed., New York: Oxford University Press, 1981.
21 DaHora B. Musculus Anconeus. Thesis, University of Recife, Recife, Brazil, 1959. Cited by Basmajian, J. V., and Griffin, W. R. J. Bone Joint Surg. 1972;54A:1712.
22 D’Alton E.J., Mennen U. Instructional Course Article: The position of the radial nerve in the upper arm. S. African Orthop. J.. 2003;August:32-36.
23 Davies F., Laird M. The supinator muscle and the deep radial (posterior interosseous nerve). Anat. Rec.. 1948;101:243.
24 Duchenne G.B.. Kaplan E.B., editor. Physiology of Motion. Philadelphia: J. B. Lippincott Co., 1949.
25 El-Hadidi S., Burke F.D. Posterior interosseous nerve syndrome caused by a bursa in the vicinity of the elbow. J. Hand Surg.. 1987;12B:23.
26 Evans E.M. Rotational deformity in the treatment of fractures of both bones of the forearm. J. Bone Joint Surg.. 1945;27:373.
27 Eycleshymer A.C., Schoemaker D.M. A Cross-Section Anatomy. New York: D. Appleton, 1930.
28 Field J.H. Posterior interosseous nerve palsy secondary to synovial chondromatosis of the elbow joint. J. Hand Surg.. 1981;6:336.
29 Gardner E. The innervation of the elbow joint. Anat. Rec.. 1948;102:161.
30 Grant J.C.B. Atlas of Anatomy, 6th ed. Baltimore: Williams & Wilkins, 1972.
31 Gray H.. Warwick R., Williams P.L., editors. Anatomy, Descriptive and Applied, 35th ed.. W. B. Saunders Co., Philadelphia, 1980;429.
32 Greenbaum B., Itamura J., Vangsness C.T., Tibone J., Atkinson R. Extensor carpi radialis brevis. An anatomical analysis of its origin. J. Bone Joint Surg.. 1999;81B:926.
33 Gruber W. Monographie der bursae mucosae cubitales. Mem. Acad. Sc. Petersburg. 1866;VII:10.
34 Gruber W. Monographie Les Canalis Supracondylaideus Humeri. Mem. Acad. Sc. Petersburg. Cited by Morris, H.: Human Anatomy, 3rd ed., Philadelphia: Blakiston; 1953:214.
35 Hamilton A.T., Raleigh N.C. Subcutaneous rupture of the brachioradialis muscle. Surgery. 1948;23:806.
36 Henle J. Handbuch Der Systematischen Anatomie des Menschen Muskellehre. Berlin: Braunschweig, 1866;224.
37 Henry A.K. Extensile Exposure, 2nd ed. Baltimore: Williams & Wilkins, 1966.
38 Hollinshead W.H.. The back and limbs. Anatomy for Surgeons, Vol. 3. Harper & Row, New York, 1969;379.
39 Jamieson R.W., Anson B.J. The relation of the median nerve to the heads of origin of the pronator teres muscle: a study of 300 specimens. Q. Bull Northwestern Univ. Med. School. 1952;26:34.
40 Johansson O.. Capsular and ligament injuries of the elbow joint. Acta Chir. Scand., 1962;Suppl.:287.
41 Wadia F., Kamineni S., Dhotare S., Amis A. Radiographic measurements of normal elbows: clinical relevance to olecranon fractures. Clin. Anat.. 2007;20:407.
42 Kapandji I.A. The Physiology of Joints. Vol. I: Upper Limb, 2nd ed. Baltimore: Williams & Wilkins, 1970.
43 Keats T.E., Teeslink R., Diamond A.E., Williams J.H. Normal axial relationships of the major joints. Radiology. 1966;87:904.
44 Kocher T.. Stiles H.J., Paul C.B., editors. Textbook of Operative Surgery, 3rd ed., London: A. & C. Black, 1911.
45 Kolb L.W., Moore R.D. Fractures of the supracondylar process of the humerus. J. Bone Joint Surg.. 1967;49A:532.
46 Langman J., Woerdeman M.W. Atlas of Medical Anatomy. Philadelphia: W. B. Saunders Co., 1976.
47 Lanz T., Wachsmuth W. Praktische Anatomie. ARM, Berlin: Springer, 1959.
48 Linell E.A. The distribution of nerves in the upper limb, with reference to variables and their clinical significance. J. Anat.. 1921;55:79.
49 Lipmann K., Rang M. Supracondylar spur of the humerus. J. Bone Joint Surg.. 1966;48B:765.
50 Loomis L.K. Reduction and after-treatment of posterior dislocation of the elbow: With special attention to the brachialis muscle and myositis ossificans. Am. J. Surg.. 1944;63:56.
51 Malkawi H. Recurent dislocation of the elbow accompanied by ulnar neuropathy: a case report and review of the literature. Clin. Orthop.. 1981;161:170.
52 Martin B.F. The annular ligament of the superior radial ulnar joint. J. Anat.. 1958;52:473.
53 Martin B.F. The oblique cord of the forearm. J. Anat.. 1958;52:609.
54 McCormick L.J., Cauldwell E.W., Anson B.J. Brachial and antebrachial artery patterns: a study of 750 extremities. Surg. Gynecol. Obstet.. 1953;96:43.
55 Schaeffer. Human Anatomy, 11th ed. Philadelphia: Blakiston, 1953.
56 Morrey B.F., An K.N. Functional anatomy of the elbow ligaments. Clin. Orthop.. 1985;201:84.
57 Morrey B.F., Askew L., An K.N., Dobyns J. Rupture of the distal tendon of the biceps brachii. J. Bone Joint Surg.. 1985;67A:418.
58 Morrey B.F., Chao E.Y. Passive motion of the elbow joint. A biomechanical analysis. J. Bone Joint Surg.. 1976;58A:501.
59 Morrey B.F., Tanaka S., An K.N. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin. Orthop.. 1991;265:187.
60 Morris H.. Schaeffer J.P., editor. Human Anatomy, 11th ed., Philadelphia: Blakiston, 1953.
61 Nazarian L.N., McShane J.M., Ciccotti M.G., O’Kane P.L., Harwood M.I. Dynamic US of the anterior band of the ulnar collateral ligament of the elbow in asymptomatic major league baseball pitchers. Radiology. 2003;227:149.
62 Ochi N., Ogura T., Hashizume H., Shigeyama A.Y., Senda M., Inoue H. Anatomic relation between the medial collateral ligament of the elbow and the humero-ulnar joint axis. J. Shoulder Elbow Surg.. 1999;8:6.
63 O’Driscoll S.W., Bell D.F., Morrey B.F. Posterolateral rotatory instability of the elbow. J. Bone Joint Surg.. 1991;73A:440.
64 O’Driscoll S.W., Horii E., Carmichael S.W., Morrey B.F. The cubital tunnel and ulnar neuropathy. J. Bone Joint Surg.. 1991;73B:613.
65 O’Driscoll S.W., Horii E., Morrey B.F. Anatomy of the attachment of the medial ulnar collateral ligament. J. Hand Surg.. 1992;17:164.
66 O’Driscoll S.W., Horii E., Morrey B.F., Carmichael S.W. Anatomy of the ulnar part of the lateral collateral ligament of the elbow. Clin. Anat.. 1992;5:296.
67 Osgood R.B. Radiohumeral bursitis, epicondylitis, epicondylalgia (tennis elbow). Arch Surg.. 1922;4:420.
68 Pankovich A.M. Anconeus approach to the elbow joint and the proximal part of the radius and ulna. J. Bone Joint Surg.. 1977;59A:124.
69 Paraskevas G., Papadopoulos A., Papaziogas B., Spanidou S., Argiriadou H., Gigis J. Study of the carrying angle of the human elbow joint in full extension: a morphometric analysis. Surg. Radiol. Anat.. 2004;26:19.
70 Polonskaja R. Zur frage der arterienanastomosen im gobiete der ellenbagenbeuge des menschen. Anat. Anz.. 1932;74:303.
71 Reimann A.F., Daseler E.H., Anson B.J., Beaton L.E. The palmaris longus muscle and tendon: a study of 1600 extremities. Anat. Rec.. 1944;89:495.
72 Seki A., Olsen B.S., Jensen S.L., Eygendaal D., Sojbjerg J.O. Functional anatomy of the lateral collateral ligament complex of the elbow: configuration of Y and its role. J. Shoulder Elbow Surg.. 2002;11:53.
73 Shiba R., Siu D., Sorbie C. Geometric analysis of the elbow joint. J. Orthop. Res.. 1988;6:897.
74 Sorbie C., Shiba R., Siu D., Saunders G., Wevers H. The development of a surface arthroplasty for the elbow. Clin. Orthop.. 1986;208:100.
75 Spalteholz V.. Baker L.F., editor. Hand Atlas of Human Anatomy, 2nd ed., Philadelphia: J. B. Lippincott Co., 1861.
76 Spinner M., Kaplan E.B. The quadrate ligament of the elbow: its relationship to the stability of the proximal radio-ulnar joint. Acta Orthop. Scand. 1970;41:632.
77 Steindler A. Kinesiology of the Human Body, 5th ed. Springfield, IL: Charles C Thomas, 1977.
78 Stimson H. Traumatic rupture of the biceps brachii. Am. J. Surg. 1935;29:472.
79 Strachan J.H., Ellis B.W. Vulnerability of the posterior interosseous nerve during radial head resection. J. Bone Joint Surg. 1971;53B:320.
80 Tanaka S., An, K. N., and Morrey, B. F.: Kinematics of ulnohumeral joint in simulated active elbow motion. Submitted for publication.
81 Terry R.J. New data on the incidence of the supracondylar variation. Am. J. Phys. Anthropol.. 1926;9:265.
82 Thepaut-Mathieu C., Maton B. The flexor function of the m. pronator teres in man: a quantitative electromyographic study. Eur. J. Appl. Physiol.. 1985;54:116.
83 Thomas T.T. A contribution to the mechanism of fractures and dislocations in the elbow region. Ann. Surg.. 1929;89:108.
84 Thompson H.C.III, Garcia A. Myositis ossificans: aftermath of elbow injuries. Clin. Orthop.. 1967;50:129.
85 Tillman B. A Contribution to the Function Morphology of Articular Surfaces. Translated by G. Konorza. Stuttgart: Georg Thieme, P. S. G. Publishing, 1978.
86 Trotter M. Septal apertures in the humerus of American whites and negros. Am. J. Phys. Anthropol. 1934;19:213.
87 Tubbs R.S., Oakes W.J., Salter E.G. The subanconeus muscle. Folia Morphol. (Warsz.). 2006;65:22.
88 Yilmaz E., Karakurt L., Belhan O., Bulut M., Serin E., Avci M. Variaton of carrying angle with age, sex, and special reference to side. Orthopedics. 2005;28:1360.
89 Yamaguchi K., Sweet F.A., Bindra R., Morrey B.F., Gelberman R.H. The extraosseous and intraosseous arterial anatomy of the adult elbow. J. Bone Joint Surg.. 1997;79A:1653.