CHAPTER 3 Topical anaesthesia
Topical anaesthesia is an extremely useful adjunct to clinical practice in the ED and is underutilised, often because it is forgotten. It is used for local anaesthesia or analgesia on intact skin, mucous membranes and the eye through the application of local anaesthetic agents to the external epithelial surface. Topical agents may be used to decrease the pain and discomfort of medical procedures and for various skin and mucous membrane conditions, including pruritus and pain due to minor trauma, burns or inflammatory conditions affecting the skin (e.g. varicella, sunburn, contact dermatitis, insect bites).
Do not forget to ask patients about local anaesthetic allergies, as ester-linked agents (which more commonly provoke reactions) are often used for topical anaesthesia.
Cryoanaesthesia
Thermal anaesthesia (cryoanaesthesia) may be used for short-acting superficial anaesthesia for procedures such as venipuncture, intravenous cannula placement, and superficial abscess incision and drainage. Ice, refrigerant sprays and liquid nitrogen have been used for this purpose. This technique does not produce very good anaesthesia.
Technique
Dermal topical local anaesthesia
Topical anaesthesia to the skin is a very useful but underused form of local anaesthesia in the ED. If used correctly, it can dramatically decrease the pain and anxiety associated with injections and other minor procedures.
EMLA (eutectic mixture of local anaesthetics) cream is a combination of lidocaine and prilocaine which has good skin penetration and produces excellent anaesthesia of the skin. Anaesthesia to a depth of 3 mm is obtained after 60 minutes of application under an occlusive dressing, while after 120 minutes the depth of anaesthesia may reach a maximum of 5 mm. The onset of action may be more rapid in highly vascular areas (such as the face), and in damaged or inflamed skin. The maximum dose should never be exceeded. EMLA produces a biphasic vascular effect – vasoconstriction followed after 30 minutes of application by vasodilatation.
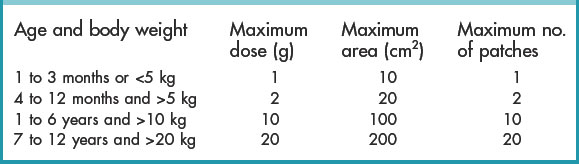
EMLA cream may be used to decrease the discomfort of vascular access, injections, lumbar puncture or superficial procedures. In children, while EMLA certainly has a role in minor procedures, it must be remembered that cooperation has as much to do with apprehension as it does with actual pain, so additional agents or methods may be needed to address this. EMLA cream may be applied under an occlusive dressing or as a pre-prepared product. EMLA should be used for small applications only, because of the toxicity of prilocaine, especially in children (principally methaemoglobinaemia). The maximum dose should not be exceeded (Table 3.1).
Recent studies have suggested that EMLA is safe even in neonates. At this stage, however, this would be an off-label application.
Technique
TAC (tetracaine 0.5%, adrenaline [epinephrine] 0.05% and cocaine 5–12%) has been used as an anaesthetic for repair of facial and scalp lacerations in children, but today sufficient concern exists about toxic potential that it should not be used.
Other options include LAT (lidocaine 4%, adrenaline 0.1% and tetracaine 0.5%) which is prepared as a premixed gel. Where it is not available, a similar mixture can be improvised:
Because of the vasoconstrictor effects it should not be used on the fingers, penis, nose or ears. Topical anaesthesia should be used with care on broken skin or mucous membranes and the patient carefully monitored for adverse reactions.
The ophthalmological preparation of tetracaine 1% can be used for topical anaesthesia on its own, especially on mucous membranes (e.g. in the mouth prior to injection for dental anaesthesia).
Lidocaine 2% gel may provide good topical anaesthesia to open wounds and damaged skin (‘roasties’) but is of little value on intact skin. Do not exceed the maximum permitted dose of 10 mL on broken skin, and 15 mL on mucosa at any one time!
Other formulations and methods
Other preparations include topical liposomal lidocaine formulations and heat-enhanced delivery systems (usually lidocaine and tetracaine preparations). Other needle-free devices for administering local anaesthetic have shown promise and new products will continue to appear. Emergency physicians should be aware of new developments in order to make their patient’s visit as minimally unpleasant as possible.
Ophthalmological applications
The ophthalmic division of the trigeminal nerve supplies the cornea, conjunctiva and sclera, via a terminal network of nerves that lies in proximity to the external surface of the eye. Local anaesthesia is therefore very effective in the eye (cataract surgery can be performed with topical anaesthesia alone).
Topical anaesthesia of the eye is useful in the ED:
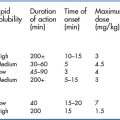
Ester-linked local anaesthetics (such as tetracaine and oxybuprocaine) have traditionally been used in the eye because of their rapid absorption and onset of action within 5 to 10 seconds, and duration of action of 10 to 20 minutes. Amides such as lidocaine and bupivacaine have become more popular because of their longer duration of action, despite their slower absorption. Buffered solutions of lidocaine or bupivacaine have a significantly longer duration of anaesthesia than ester agents, with an onset of action within 1 minute of instillation, and duration of action of 45–60 minutes for lidocaine, and 60–180 minutes for bupivacaine. There is no general consensus on which topical local anaesthetic eye drop provides the best analgesia, but studies have shown that proxymetacaine causes the least discomfort on administration. Tetracaine, oxybuprocaine, proxymetacaine, lidocaine and bupivacaine have all been used successfully in a variety of different concentrations. Availability may determine the choice of agent, but it is essential that the preparation is preservative-free. Increasing the preparation pH (buffering 1 mL of local anaesthetic with 0.1 mL of sodium bicarbonate [1:10]) may alter the duration of action but is probably of little clinical benefit in general. Topical non-steroidal anti-inflammatory drugs, such as ketorolac or diclofenac, may be co-administered with local anaesthetics and prescribed for follow-on outpatient treatment for traumatic eye discomfort. Topical steroids should in general only be used in consultation with an ophthalmologist.
Topical local anaesthetic drops should never be prescribed for patients’ own use for three main reasons:
Technique
Mucosal topical anaesthetic applications
Topical anaesthesia is very effective when applied to the mucous membranes of the ears, nose, throat, oral cavity, upper airway and genital mucosa because of its rapid absorption. For the same reason, the toxic potential of the local anaesthetic agent is high and the maximum dose should be strictly observed. Administration of topical anaesthetics should be performed with accuracy to ensure that a predetermined amount of drug is administered to allow for the intended effect while minimising the risk of toxicity.
Techniques