CHAPTER 12 Altered Consciousness
Altered consciousness is a most common finding in patients evaluated by a consulting neurosurgeon or neurologist. The development of a comprehensive differential diagnosis, treatment plan, and prognosis for altered consciousness is well beyond the scope of a single book chapter (instead, see Posner and colleagues1). Here, emphasis is placed on conceptualizing neurological disorders of consciousness and formulating an organized and physiologically based approach to the general set of problems. A systematic approach to evaluate patients with altered consciousness requires a foundation of the basic principles that underlie maintenance of the normal wakeful conscious state.
A Brief Taxonomy
Schiff and Plum2 proposed the following working definition for the normal wakeful conscious state in humans modeled after that of James3 (1894):
Human conscious brain states are characterized by several neuropsychological components, including arousal, attention, intention, memory, awareness, and mood-emotion. A clinically oriented view of global disorders of consciousness suggests a roughly hierarchical organization of these components. The arousal level appears to influence all neuropsychological functions in humans and animals, and absence of an aroused state precludes behavior.4 Complete loss of patterned arousal is seen only in coma (and in brain death, which is operationally defined and an unambiguous condition equivalent to death5). In VS, limited recovery of arousal patterning occurs without evidence of the other neuropsychological components of human consciousness (see discussion later). Fragmentary elements of specific neuropsychological components are evident in these syndromes. For example, fragments of attentional function are evidently preserved in all forms of akinetic mutism, with varying levels of impairment in other components (see later). Similarly, purposeless intentional movements can occur in patients with hyperkinetic mutism or as partially integrated and organized goal-directed sensorimotor activity in those with complex partial seizures or delirium (see Schiff and Plum2 for a more extended review). Complex brain injuries typically produce a mix of the clinical features observed in these classic syndromes. Here we focus on the classification of global disorders of consciousness most frequently encountered and related to each other as recovery evolves after severe brain injury.
Vegetative State
The concept of VS was first introduced in 1972 by Jennett and Plum, who defined the clinical syndrome of the “persistent vegetative state” as being identified by dissociation of an apparent recovery of behavioral wakeful arousal associated with periods of eye opening that alternate with periods of eye closure in patients who show no evidence of awareness of self or their environment.6 Early use of the term arbitrarily identified VS lasting longer than 30 days as a “persistent vegetative state.” However, many organizations and countries have now advocated that the modifier “persistent” not be used because it is often misinterpreted to indicate probable permanence of the VS. The expectation for permanence of the VS can be assessed accurately only by considering the mechanism and elapsed time from the injury (see “Guide to Prognosis” later).
The VS typically follows an initial coma produced by an acute brain insult and most often is associated with patterns of injury that overlap those that produce coma. The two most common causes of VS are severe traumatic brain injury and cardiac arrest. Autopsy studies of patients who remain in VS after both conditions demonstrate a common pattern of extensive loss of thalamic neurons,7 particularly within the central thalamic intralaminar nuclei and closely adjacent components of thalamic association nuclei.8 Bilateral injuries restricted to these regions alone can produce coma.2,9 The severe loss of thalamic neurons reflects widespread disconnection of the corticothalamic system and neuronal death across the cerebrum. Although this finding of extensive thalamic neuronal loss can be seen after both diffuse axonal injury from brain trauma and oxygen deprivation associated with cardiac arrest, widespread neocortical neuronal death is common only with cardiac arrest (64% versus 11%7). Significant brainstem damage is not commonly found at autopsy of VS patients, an observation that emphasizes that VS is primarily a disorder of corticothalamic system integration.
Since the original definition of VS, research efforts have typically focused on clinical indicators of permanence and underlying neuropathology (reviewed by Jennett10). A small number of early neuroimaging studies of VS patients measured cerebral metabolism with fluorodeoxyglucose-positron emission tomography (FDG-PET) scans. In these studies, VS patients showed a reproducible reduction in resting metabolism to typically 30% to 50% of normal metabolic rates across cerebral structures.11,12 Comparable reductions in cerebral metabolic rates are found in normal subjects in the pharmacologic coma produced by surgical anesthesia.13 More recently, several groups have examined functional activation of cerebral networks in response to sensory stimuli in VS patients by using functional neuroimaging methods (15O-PET and functional magnetic resonance imaging [fMRI)]. These studies demonstrate widespread failure of functional responses to elementary sensory stimuli in cortical regions remote from the primary sensory cortices in VS patients.14,15 In some VS patients, unusual behavioral and physiologic variations are correlated with evidence of isolated islands of metabolic activity.16 In one such VS patient, rare single understandable words were emitted for 20 years without linkage to environmental stimulation. In this patient, the left cerebral structures (including Wernicke’s area in the temporal association cortex and Broca’s area in the frontal opercular region) demonstrated relatively increased metabolic rates (nearly twice the rates in surrounding brain tissue) and physiologic connections consistent with partial and isolated preservation of brain structures of the human language system.17 The behavioral fragments more typically identified in chronic VS patients are stereotyped emotional-limbic responses such as grimaces. These emotional displays most probably reflect isolated limbic networks tightly linked to brainstem and basal forebrain structures that operate without functional connection to the thalamocortical systems that are typically severely damaged in VS patients.
Minimally Conscious State
The first level of behavioral recovery beyond VS is operationally defined as MCS. MCS patients show evidence on bedside examination of contingent responses to environmental stimuli or self-initiated behavior that provides unequivocal but inconsistent evidence of awareness of self or the environment18 (Table 12-1). A wide range of behavioral expressions are currently consistent with the operational criteria for MCS.19 For example, consistent and sustained visual tracking or fixation may be the only behavioral evidence of responsiveness in an MCS patient. Alternatively, an MCS patient may exhibit intermittent spoken language responses or inconsistent and inaccurate communication with gestural or verbal output. Recovery of functional communication (operationally defined as the ability to consistently and accurately answer simple contextual yes or no questions) defines the upper boundary of MCS. Beyond MCS, varying levels of severe disability are not currently subcategorized.
TABLE 12-1 Aspen Working Group Criteria for Clinical Diagnosis of the Minimally Conscious State
|
Evidence of limited but clearly discernible self or environmental awareness on a reproducible or sustained basis, as demonstrated by one or more of the following types of behavior:
|
From Giacino JT, Ashwal S, Childs N, et al. The minimally conscious state: definition and diagnostic criteria. Neurology. 2002;58:349-353.
Even though only subtle findings may distinguish VS and MCS patients at the bedside, a wide separation in underlying functional cerebral substrates associated with the two conditions is indicated by neuroimaging and electrophysiologic and pathologic studies.20–23 Autopsy studies of patients with clinical histories consistent with MCS demonstrate reduced overall levels of cerebral cell death and, in some MCS patients, no evidence of significant thalamic cell loss or severe diffuse axonal injury—a pattern never observed in VS patients.23 Neuroimaging studies generally show widespread preservation of distributed cerebral network activation in response to sensory stimuli, including passive language stimuli20,24 and auditory15 and somatosensory stimuli.21 Electrophysiologic studies typically show recovery of a broad range of frequency content on the electroencephalogram and, in some MCS patients, preservation of high-level passive semantic processing of spoken language.22 Such large-scale integrative network responses that involve cortical association regions are not typically seen in VS patients. The presence of recruitable large-scale cerebral networks in some MCS patients suggests a potential substrate for further recovery in these patients. These observations probably underlie the rare, but verified cases of late recovery of spoken language in some severely brain-injured patients with clinical histories consistent with long-standing MCS.25 In a recent single-subject study, one MCS patient who had demonstrated preserved passive language responses recovered spoken language and consistent verbal and gestural communication with bilateral electrical stimulation of the central thalamus.26
Akinetic Mutism
The syndrome of akinetic mutism includes patients who fulfill the criteria for MCS and patients who can functionally communicate when formally assessed yet demonstrate a severe reduction in spontaneous behavior or extremely slowed interactive responses. Patients with akinetic mutism may appear highly attentive and vigilant with wide eye opening, deliberate visual tracking of the examiner around the room, but no other types of behavior. These patients are included in the MCS spectrum. Other patients sometimes described as akinetic mutes may appear awake but somnolent with apparent psychomotor retardation similar to a variety of subcortical dementias.27 The patterns of brain injury most commonly associated with these syndromes are bilateral damage to the anterior medial regions of the cerebral cortex, bilateral injury to caudate nuclei (or unilateral dominant hemisphere caudate nucleus), bilateral central thalamic lesions, large basal forebrain injuries, or damage to the mesencephalic reticular formation.2,28 Akinetic mutism is a classic finding after rupture of an anterior communicating artery aneurysm. Some authors27 have defined “slow syndrome” to identify this subgroup of patients as a related behavioral phenotype characterized primarily by severe memory loss, severely slowed behavioral responses, and a listless, apathetic appearance sometimes referred to as “abulia.”29 The pattern of focal injuries associated with both akinetic mutism and “slow syndrome” overlaps entirely with those producing acute coma and VS when the lesions are bilateral and larger in rostrocaudal extent.2
An Organizing Strategy to Assess Disorders of Consciousness Based on Anatomic and Physiologic Considerations
If psychogenic processes are excluded, observed alteration of consciousness in all settings implies one of the following possibilities: (1) diffuse functional impairment of both hemispheres as a result of direct injury and toxic/metabolic alterations associated, for example, with cardiopulmonary dysfunction, infection, poisoning, or a variety of other processes producing bilateral cerebral dysfunction, such as antibody-mediated alteration of neurons or axons, and (2) selective impairment of midline and paramedian upper brainstem and basal forebrain regions containing nuclei associated with ascending arousal input to the anterior forebrain, often damaged in combination with central thalamic nuclei (or isolated to the central thalamus if the lesions are bilateral and relatively large in rostrocaudal extent).9,30 The severity of a disturbance in consciousness directly reflects the functional disturbance produced in cerebral neurons diffusely or within the relatively restricted network of subsystems involved in forebrain arousal and regulation of arousal.
Identification of patients in the first category—those with overwhelming structural brain injury—can frequently be done by inspection and clinical judgment (e.g., a patient with complete infarction of the dominant hemisphere and central herniation but not quite meeting brain death criteria). Prospective studies of large numbers of patients in coma have codified a number of strong clinical predictors of death or outcomes limited to permanent VS after the two most common causes: cardiac arrest and severe traumatic brain injury (see Posner and colleagues1 for a comprehensive review). For example, coma associated with loss of motor response and pupil and corneal reflexes initially and enduring over the first 48 to 72 hours is invariably associated with outcomes no better than permanent VS after cardiac arrest once potential confounding variables are excluded.
When the available information does not support the inference that the patient’s functional level is due to overwhelming neuronal death or disconnection, it should prompt consideration of functional disturbances at both the neuronal subcellular and the population (“circuit”) level. Many toxic, infectious, inflammatory, and autoimmune processes will alter neuronal function and reduce the capacity of cortical, striatal, and thalamic neurons to maintain firing rates and their functional roles in local networks.1 Systematic diagnostic evaluations of such mechanisms are currently available, and the clinician should make a judgment about whether the functional level of the patient is well anticipated by the features of the history and structural imaging while recognizing that reversible and irreversible severe cerebral dysfunction will often be functionally indistinguishable. Similarly, mechanisms that underlie neuronal population-level (or “circuit-level”) disturbances are not yet well classified but are recognized.31–33 Among the most important population-level phenomena encountered in the severely brain-injured population is selective vulnerability of the anterior forebrain systems (corticostriatopallidothalamocortical loop systems) to reduced overall background synaptic activity and dopamine levels.32,34 When not contraindicated, an initial trial of a dopamine agonist (e.g., amantadine) is a reasonable empirical first step in a medically stable patient to see whether behavioral changes can be identified. The most common transitional signs from VS to MCS are visual fixation and visual tracking.35
In general, patients who are medically stable and have not recovered past MCS behavioral levels are often quickly transferred out of the care of neurosurgeons and neurologists. Nonetheless, it should be recognized that several observations have demonstrated that severely brain-injured patients may harbor considerable functional integrative capacity despite months and years without clinically evident change.25 At the least, it can be recommended that time trials of stimulant pharmacologic agents be attempted under the guidance of a physician who can recognize subtle neurological changes on bedside examination and that patients undergo periodic reassessment of their neurological status.36 Although these are reasonable general recommendations for all patients with persistent alteration of consciousness, it is important to recognize the wide differences in expectation for further recovery in VS and MCS patients over the first 12 months after severe brain injuries.
A Guide to Formulating Prognosis in Patients with Disorders of Consciousness
The uncertainty of outcome for an individual patient in coma, VS, or MCS will vary considerably, depending on the details of clinical findings obtained from bedside examinations, time from the initial injury, and the specific cause of the injury. Accordingly, it is not possible to comprehensively review the possible circumstances relevant to formulate a prognosis for an individual patient here (but see Posner and coworkers1 for an extended review and tabular information specific to etiology, diagnostic category, and time windows). Instead, general principles for organizing information and a guide to develop a prognosis for patients with disorders of consciousness are presented.
The prognosis of VS patients similarly depends on the mechanism that underlies the brain injury. A patient who remains in VS for 3 months after cardiac arrest or other nontraumatic, diffuse brain injury that produces loss of blood flow or brain oxygen is considered to be in a permanent VS. To apply these guidelines beyond patients with known hypoxic-ischemic encephalopathy is risky. For example, patients with encephalitis are difficult to assess with these guidelines. Time frames for recovery after posttraumatic VS are considerably longer, and 1 year is required to expect permanence. After diffuse axonal injury, the widespread neuronal death in thalamic neurons is an indirect result of more delayed transneuronal degeneration, unlike the immediate effects of oxygen deprivation, which induces rapid neuronal death after roughly 6 minutes of oxygen loss. Although a continuum of outcomes after an initial transition from coma to VS is well recognized, the outcomes are not equally distributed across a continuum. Anoxic brain injuries produce relatively sharp cutoffs associated with global neuronal death and frequently lead to VS with an underlying anatomic pathology similar to that of brain death. This underlying mechanistic difference probably controls the much longer time course of recovery and the point beyond which permanence is expected for VS after traumatic brain injury as opposed to cardiac arrest and similar injuries. Recovery after prolonged traumatic coma and VS is well described, and unlike VS after cardiac arrest, unconsciousness for 3 months does not necessarily preclude significant recovery. However, no large studies have continued to monitor patients who remain in VS at 1 year after brain trauma. Some case reports suggest that a small percentage of such patients may show some recovery of conscious awareness past the 1-year time frame.19
Prognosis in MCS is the least well characterized because the diagnostic category is relatively new and the available studies suggest that significant further recovery may occur in some patients after 1 year in MCS.35 Importantly, MCS patients typically show faster changes in the rate of recovery within the first year after injury from either traumatic or nontraumatic injury than do VS patients. In the small cohorts of MCS patients studied, some attain outcomes better than severe disability at 1 year despite remaining in MCS for 1 to 3 months.35 A recent small prospective cohort study also found a limited correlation between time in MCS and functional outcome at 2 to 5 years.35 Thus, it is essential that the often small clinical finding that distinguishes VS from MCS be identified on bedside examinations performed within the first few months after injury. Importantly, all verified examples of late recovery of communication in severely brain-injured patients have occurred in the MCS patient population; this indicates the importance of prospective tracking and reassessment of these patients.36
Emerging Role of Neuroimaging in Altered Consciousness: Opportunities and Limitations
Several recent neuroimaging studies of VS and MCS patients suggest that functional imaging tools may become part of the comprehensive assessment of neurological disorders of consciousness.15,20,25,37
Owen and colleagues used fMRI to demonstrate unambiguous evidence of command following in a single patient with no visible behavioral response who fit the behavioral criteria for VS.37 This patient was asked to imagine playing tennis and to imagine walking around her home. The patient’s brain activation patterns in the supplementary motor area matched the activity profile of normal subjects who imagined playing tennis. Similar activations of the parahippocampal gyrus and posterior parietal cortex were observed when she imagined spatial navigation through her home. The findings provide evidence that in principle, neuroimaging tools may have the potential to identify false-positive VS diagnoses. Simple command following is an objective criterion for MCS, and the imaging findings are arguably an unambiguous proxy for small movements of a finger, thumb, or eye in response to simple commands.
The patient studied by Owen and associates had remained in VS for 5 months after a severe traumatic brain injury.37 This time frame provides a nearly 20% chance to recover consciousness at 1 year and a 4% chance to achieve an outcome better than severe disability despite remaining in VS.10,38 The fMRI measurements in this patient may have measured the early aspects of the natural recovery process inasmuch as visual tracking to a mirror was identified at 11 months and thus provided behavioral evidence of MCS at that time. Although compelling, there are limitations to the findings. First, obtaining reliable fMRI data from severely brain-injured patients is often not possible because of hardware in the brain or skull or uncontrolled patient movement. Second, the signal characteristics in patients in general may be different from those in normal subjects, and simply knowing that it is possible to obtain the result in one patient provides no information about the generalizability and feasibility of using these techniques. This important question, however, has not been systematically studied. Third, it is important to avoid overinterpretation. The evocative picture of carrying out the imagery tasks is suggestive of high-level cognitive function. However, many MCS patients will demonstrate clear and reliable command following by performing small visible movements but cannot establish a communication system to accurately answer simple situational questions. Without further measurements or the use of the imaging tools to assess capacity for communication, the only reasonable conclusion is that the patient’s function is at least MCS and not VS.39
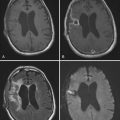
Another recent and provocative neuroimaging study demonstrated evidence of late structural changes in the brain of an MCS patient.25 The patient recovered fluent spoken language after 20 years in MCS after a severe traumatic brain injury suffered in a motor vehicle accident. Structural MRI in this patient showed marked diffuse cerebral and subcortical atrophy, particularly brainstem and frontal lobe atrophy. Diffusion tensor imaging (DTI) showed significant reductions in fractional anisotropy across cerebral structures consistent with severe diffuse axonal injury, thus demonstrating that the patient had initially suffered a very severe brain injury. DTI measurements also revealed large regions of increased fractional anisotropy in posterior brain white matter not seen in normal subjects. An 18-month longitudinal study of this patient’s brain demonstrated significant changes in fractional anisotropy and left-right directionality of DTI-measured diffusion within the medial posterior parieto-occipital regions and the midline cerebellar white matter. The latter findings correlated with clinical improvements in motor control, including limited recovery of lower extremity and left upper extremity motor control and improved dysarthria. These findings suggest a role of slow structural changes within the patient’s white matter in the recovery process. A recent prospective study of a cohort of severely brain-injured patients after traumatic injury also found a correlation of recovery of fractional anisotropy to normal or supernormal levels in areas with early significant reductions and recovery of neurological function.40
, Boly M, Faymonville ME, Peigneux P, et al. Cerebral processing of auditory and noxious stimuli in severely brain injured patients: differences between VS and MCS. Neuropsychol Rehabil. 2005;15:283-290.
, Coleman MR, Rodd JM, Davis MH, et al. Do vegetative patients retain aspects of language comprehension? Evidence from fMRI. Brain. 2007;130:2494-2507.
, Fins JJ, Schiff ND, Foley K. Late recovery from the minimally conscious state. Neurology. 2007;68:304-307.
, Fins JJ, Schiff ND. Shades of gray: new insights into the vegetative state. Hastings Center Rep. 2006;36(6):8.
, Giacino JT, Whyte J. The vegetative state and minimally conscious state: current knowledge and remaining questions. J Head Trauma Rehabil. 2005;20:30-50.
, Kotchoubey B, Lang S, Mezger G, et al. Information processing in severe disorders of consciousness: vegetative state and minimally conscious state. Clin Neurophysiol. 2005;116:2441-2453.
, Lammi MH, Smith VH, Tate RL. The minimally conscious state and recovery potential: a follow-up study 2 to 5 years after traumatic brain injury. Arch Phys Med Rehabil. 2005;86:746-754.
, Maxwell WL, MacKinnon MA, Smith DH, et al. Thalamic nuclei after human blunt head injury. J Neuropathol Exp Neurol. 2006;65:478-488.
, Multisociety Task Force on PVS. Medical aspects of the persistent vegetative state. Part 1. N Engl J Med. 1994;330;:1499-1508.
, Owen AM, Coleman MR, Boly M, et al. Detecting awareness in the vegetative state. Science. 2006;313:1402.
, Posner JB, Saper CB, Schiff ND, et al. The Diagnosis of Stupor and Coma, 4th ed. Oxford: Oxford University Press; 2007.
, Schiff ND. Modeling the minimally conscious state: measurements of brain function and therapeutic possibilities. Prog Brain Res. 2005;150:477-497.
, Schiff ND, Plum F. The role of arousal and “gating” systems in the neurology of impaired consciousness. J Clin Neurophysiol. 2000;17:438-459.
, Schiff ND, Posner JP. Another “awakenings.”. Ann Neurol. 2007;62:5-7.
, Schiff ND, Rodriguez-Moreno D, Kamal A, et al. fMRI reveals large-scale network activation in minimally conscious patients. Neurology. 2005;64:514-523.
, Sidaros A, Engberg AW, Sidaros K, et al. Diffusion tensor imaging during recovery from severe traumatic brain injury and relation to clinical outcome: a longitudinal study. Brain. 2008;131:559-572.
, Voss HU, Uluç AM, Dyke JP, et al. Possible axonal regrowth in late recovery from the minimally conscious state. J Clin Invest. 2006;116:2005-2011.
1 Posner JB, Saper CB, Schiff ND, et al. The Diagnosis of Stupor and Coma, 4th ed. Oxford: Oxford University Press; 2007.
2 Schiff ND, Plum F. The role of arousal and “gating” systems in the neurology of impaired consciousness. J Clin Neurophysiol. 2000;17:438-459.
3 James W. Principles of Psychology. 1890. Reprinted by Dover Books, 1950
4 Pfaff D, Westberg L, Kow LM. Generalized arousal of mammalian central nervous system. J Comp Neurol. 2005;493:86-91.
5 Wijdicks EF. The diagnosis of brain death. N Engl J Med. 2001;344:1215-1221.
6 Jennett B, Plum F. Persistent vegetative state after brain damage. A syndrome in search of a name. Lancet. 1972;1:734-737.
7 Adams JH, Graham DI, Jennett B. The neuropathology of the vegetative state after acute insult. Brain. 2000;123:1327-1338.
8 Maxwell WL, MacKinnon MA, Smith DH, et al. Thalamic nuclei after human blunt head injury. J Neuropathol Exp Neurol. 2006;65:478-488.
9 Castaigne P, Lhermitte F, Buge A, et al. Paramedian thalamic and midbrain infarcts: clinical and neuropathological study. Ann Neurol. 1981;10:127-148.
10 Jennett B. Vegetative State. Cambridge: Cambridge University Press; 2002.
11 Levy DE, Sidtis JJ, Rottenberg DA, et al. Differences in cerebral blood flow and glucose utilization in vegetative versus locked-in patients. Ann Neurol. 1987;22:673-682.
12 DeVolder AG, Goffinet AM, Bol A, et al. Brain glucose metabolism in postanoxic stroke. Arch Neurol. 1990;47:197-204.
13 Laureys SL, Owen AM, Schiff ND. Brain function in coma, vegetative state and related disorders. Lancet Neurol. 2004;3:537-546.
14 Laureys S, Faymonville ME, Peigneux P, et al. Cortical processing of noxious somatosensory stimuli in the persistent vegetative state. Neuroimage. 2002;17:732-741.
15 Boly M, Faymonville ME, Peigneux P, et al. Auditory processing in severely brain injured patients: differences between the minimally conscious state and the persistent vegetative state. Arch Neurol. 2004;61:233-238.
16 Schiff N, Ribary U, Moreno D, et al. Residual cerebral activity and behavioral fragments in the persistent vegetative state. Brain. 2002;125:1210-1234.
17 Schiff ND, Ribary U, Plum F, et al. Words without mind. J Cogn Neurosci. 1999;1:650-656.
18 Giacino JT, Ashwal S, Childs N, et al. The minimally conscious state: definition and diagnostic criteria. Neurology. 2002;58:349-353.
19 Giacino JT, Whyte J. The vegetative state and minimally conscious state: current knowledge and remaining questions. J Head Trauma Rehabil. 2005;20:30-50.
20 Schiff ND, Rodriguez-Moreno D, Kamal A, et al. fMRI reveals large-scale network activation in minimally conscious patients. Neurology. 2005;64:514-523.
21 Boly M, Faymonville ME, Peigneux P, et al. Cerebral processing of auditory and noxious stimuli in severely brain injured patients: differences between VS and MCS. Neuropsychol Rehabil. 2005;15:283-290.
22 Kotchoubey B, Lang S, Mezger G, et al. Information processing in severe disorders of consciousness: vegetative state and minimally conscious state. Clin Neurophysiol. 2005;116:2441-2453.
23 Jennett B, Adams JH, Murray LS, et al. Neuropathology in vegetative and severely disabled patients after head injury. Neurology. 2001;56:486-490.
24 Coleman MR, Rodd JM, Davis MH, et al. Do vegetative patients retain aspects of language comprehension? Evidence from fMRI. Brain. 2007;130:2494-2507.
25 Voss HU, Uluç AM, Dyke JP, et al. Possible axonal regrowth in late recovery from the minimally conscious state. J Clin Invest. 2006;116:2005-2011.
26 Schiff ND, Giacino JT, Kalmar K, et al. Behavioral improvements with thalamic stimulation after severe traumatic brain injury. Nature. 2007;448:600-603.
27 Katz DI, Alexander MP, Mandell AM. Dementia following strokes in the mesencephalon and diencephalon. Arch Neurol. 1987;44:1127-1133.
28 Mega MS, Cohenour RC. Akinetic mutism: disconnection of frontal-subcortical circuits. Neuropsychiatry Neuropsychol Behav Neurol. 1997;10:254-259.
29 Fisher CM. Honored guest presentation: abulia minor vs. agitated behavior. Clin Neurosurg. 1983;31:9-31.
30 Plum F. Coma and related global disturbances of the human conscious state. In: Jones E, Peters P, editors. Cerebral Cortex, Vol. 9. New York: Plenum Press; 1991.
31 Schiff ND. Modeling the minimally conscious state: measurements of brain function and therapeutic possibilities. Prog Brain Res. 2005;150:477-497.
32 Schiff ND, Posner JP. Another “awakenings.”. Ann Neurol. 2007;62:5-7.
33 Brefel-Courbon C, Payoux P, Ory F, et al. Clinical and imaging evidence of zolpidem effect in hypoxic encephalopathy. Ann Neurol. 2007;62:102-105.
34 Schiff ND. Central thalamic contributions to arousal regulation and neurological disorders of consciousness. Ann N Y Acad Sci. 2008;1129:105-118.
35 Lammi MH, Smith VH, Tate RL. The minimally conscious state and recovery potential: a follow-up study 2 to 5 years after traumatic brain injury. Arch Phys Med Rehabil. 2005;86:746-754.
36 Fins JJ, Schiff ND, Foley K. Late recovery from the minimally conscious state. Neurology. 2007;68:304-307.
37 Owen AM, Coleman MR, Boly M, et al. Detecting awareness in the vegetative state. Science. 2006;313:1402.
38 Multisociety Task Force on PVS. Medical aspects of the persistent vegetative state. Part 1. N Engl J Med. 1994;330;:1499-1508.
39 Fins JJ, Schiff ND. Shades of gray: new insights into the vegetative state. Hastings Center Rep. 2006;36(6):8.
40 Sidaros A, Engberg AW, Sidaros K, et al. Diffusion tensor imaging during recovery from severe traumatic brain injury and relation to clinical outcome: a longitudinal study. Brain. 2008;131:559-572.