56
Alopecias
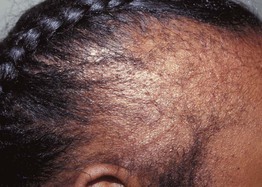
• In a normal scalp, 90–95% of hairs are in anagen phase, 5–10% in telogen phase (Fig. 56.1).
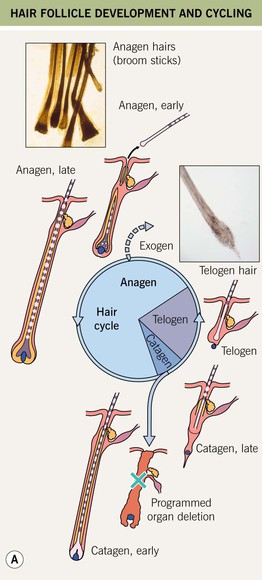
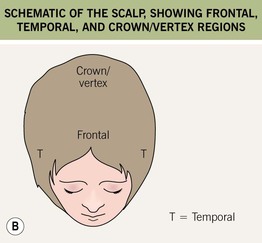
Fig. 56.1 General concepts. A Hair follicle development and cycling. B Schematic of the scalp, showing frontal, temporal, and crown/vertex regions. A, Courtesy, Ralf Paus, MD; Anagen hairs, Courtesy, Maria K. Hordinsky, MD; Telogen hair, Courtesy, Leonard C. Sperling, MD.
• About 50–100 hairs normally shed daily.
• Alopecias can be categorized as diffuse vs. circumscribed, patterned vs. non-patterned, and non-scarring vs. scarring loss (Fig. 56.2).
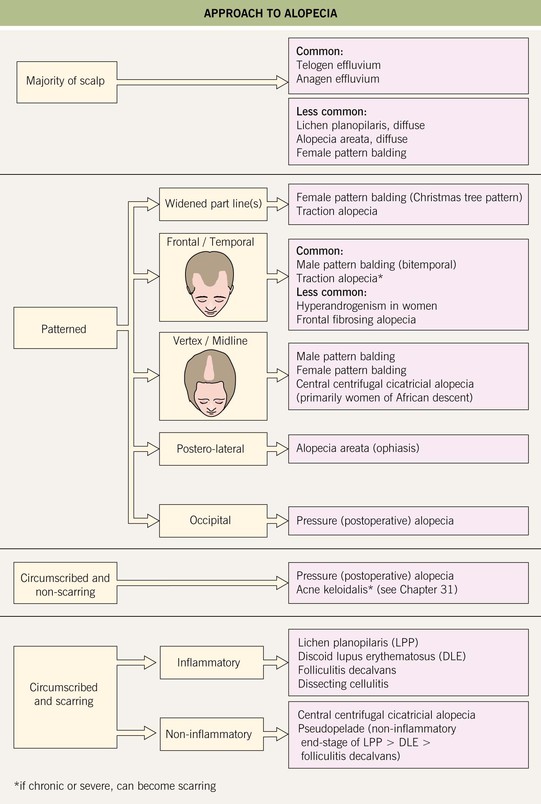
Fig. 56.2 Approach to alopecia.
Non-Scarring Alopecias
Male and Female Pattern Hair Loss (Androgenetic Alopecia)
• 80% of Caucasian men are affected by age 70 years.
• Women are less likely than men to have a family history of the disorder.
• Sensitivity of scalp hair to androgen hormones causes gradual miniaturization of hairs on the frontal/midline/vertex regions of men and the midline and crown of women (Fig. 56.3).
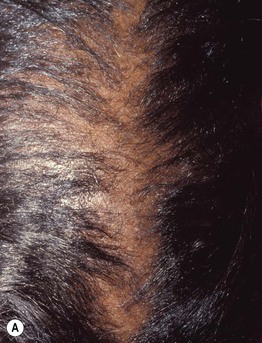

Fig. 56.3 Androgenetic alopecia. Comparison of partline on the crown (A) and the occiput (B). Courtesy, Leonard C. Sperling, MD.
• Should exclude hyperandrogenism (e.g. ovarian or adrenal source) in younger women or in women with signs of virilization (see Chapter 57).
Telogen Effluvium
• Sometimes a definable precipitating event ~3 months prior precedes diffuse shedding, leading to a reduced density of hair on the entire scalp and occasionally other areas of body hair (Table 56.1).
Table 56.1
Causes of telogen effluvium.
Some authors also propose vitamin B12 or iron deficiency as causes.
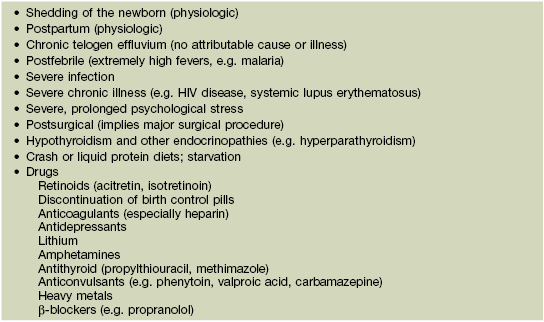
• Shed hairs are predominantly telogen hairs (Fig. 56.1).
• Generally complete hair regrowth occurs after months to years.
• Some women have chronic telogen effluvium without a definable cause.
• Rx: discontinue any potentially offending drugs, exclude thyroid abnormality and etiologies listed in Table 56.1.
Alopecia Areata
• Autoimmune disease with increased T-cells present in the hair matrix.
• Average lifetime risk for developing this disease is 1–2%.
• Circular to oval areas of alopecia that may progress to total scalp hair loss (alopecia totalis) or total body hair loss (alopecia universalis) (Fig. 56.4).






Fig. 56.4 Alopecia areata. A Circular area of alopecia in a child. B Exclamation point hair with the distal end broader than the proximal end. C Total alopecia of scalp, eyebrows, and eyelashes in a patient with alopecia universalis. D Ophiasis with a band-like pattern of hair loss along the periphery of the temporal and occipital scalp. E Diffuse variant of alopecia areata. F Typical yellow dots seen dermoscopically in alopecia areata. B, Courtesy, Julie V. Shaffer, MD; C, Courtesy, Leonard C. Sperling, MD; E, Courtesy, Maria K. Hordinsky, MD. F, Courtesy, Iris Zalaudek, MD.
• May see exclamation point hairs at borders (Fig. 56.4).
• Ophiasis pattern is a band-like pattern of loss along the temporal/occipital scalp (Fig. 56.4) that may be less responsive to therapy.
Trichotillomania
Postoperative (Pressure-Induced Alopecia)
Drug-Induced Alopecia
Scarring (Cicatricial) Alopecias
• Classically defined as loss of hair follicles with scarring (e.g. lupus erythematosus, lichen planopilaris) or an alopecia in which hair does not grow back (e.g. chronic, long-standing traction alopecia).
• In secondary scarring alopecia, the hair is destroyed nonspecifically, i.e. secondary to burns, radiation dermatitis, cutaneous malignancy (see Chapter 100), sarcoidosis, morphea, necrobiosis lipoidica, infections (e.g. severe kerion), mucous membrane (cicatricial) pemphigoid.
Central Centrifugal Cicatricial Alopecia (CCCA)
• Most commonly observed in black women.
• May be related to the use of chemical hair relaxers or thermal relaxers (e.g. flat iron).
• Slowly progressive; centered on the crown/vertex and midline (Fig. 56.5).

Fig. 56.5 Central centrifugal cicatricial alopecia in an African-American woman. Alopecia is most prominent on the crown/vertex and the midline. Courtesy, Leonard C. Sperling, MD.
• Symptoms may be mild or absent.
• Occasionally patients have secondary changes, especially crusting or pustules.
Lichen Planopilaris
• Women > men, more common in Caucasians.
• 50% may have associated lichen planus involving the skin, mucous membranes, or nails (see Chapters 9 and 58).
• Usually several foci of alopecia with loss of follicles and scarring centrally (may be clinically subtle); peripheral follicles having a central, keratotic plug and a rim of inflammation (pink to violet in color) (Fig. 56.6).


Fig. 56.6 Lichen planopilaris. A Perifollicular erythema in association with scale. B Later stage showing scarring with loss of follicular openings, but less erythema. Some of the follicles still have a rim of inflammation. A, Courtesy, Jean L. Bolognia, MD.
• Centered on the crown/vertex or midline, or predominantly affecting the frontal hairline and eyebrows (‘frontal fibrosing alopecia’) (Fig. 56.7), or rarely a diffuse pattern.
Discoid Lupus Erythematosus (DLE)
• A type of chronic cutaneous lupus erythematosus.
• More common in adult women, especially black women.
• Minority of patients fulfill the criteria for systemic lupus erythematosus (see Chapter 33), but patients need to be evaluated at the time of diagnosis of DLE and followed longitudinally.
• Circular lesions of erythema, atrophy, dilated/plugged follicles, and scale as well as alopecia.
• As lesions age, central hypopigmentation and peripheral hyperpigmentation may appear, along with scarring (Fig. 56.8).
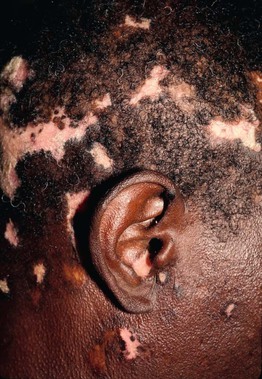
Fig. 56.8 Discoid lupus erythematosus. Alopecia with dyspigmentation on the scalp and face. Note involvement of the conchal bowl. Courtesy, Joyce Rico, MD.
• May see similar-appearing lesions elsewhere (especially face and ears).
Acne Keloidalis
• Favors young black men (see Chapter 31).
• Occipital scalp most common site, but sometimes involves the crown/vertex.
• Smooth, firm papules > pustules.
• Initial lesions resolve with alopecia and/or protuberant papules.
• Coalescence of lesions leads to alopecia.
• Rx: intralesional CS, oral antibiotics, excision (see Table 31.6).
Dissecting Cellulitis
Folliculitis Decalvans
Pseudopelade
Traction Alopecia (Late-Stage)
• Occurs after years of hair styling that causes traction.
• Generally seen in black women on the bitemporal/frontal scalp line (Fig. 56.10).
Hair Shaft Abnormalities
• Four main categories: (1) fractures (trichorrhexis nodosa and invaginata, trichoschisis); (2) irregularities (monilethrix); (3) twisting (pili torti, woolly hair, trichonodosis); and (4) extraneous matter (Fig. 56.11).
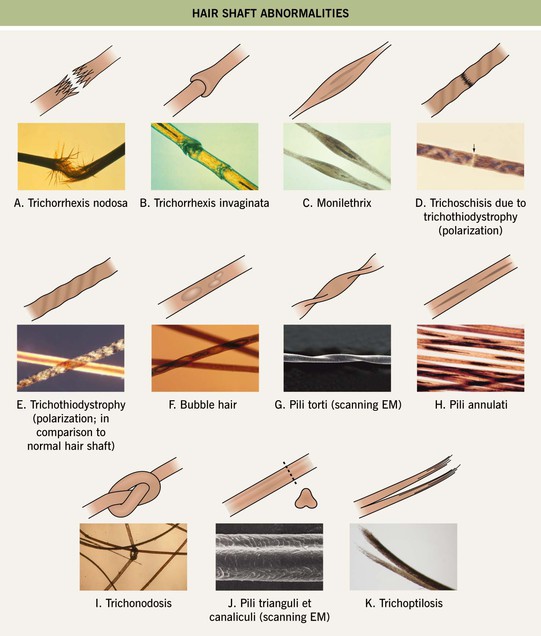
Fig. 56.11 Schematic drawings and microscopic appearance of hair shaft abnormalities. A Trichorrhexis nodosa. B Trichorrhexis invaginata. C Monilethrix. D Trichoschisis (due to trichothiodystrophy). E Trichothiodystrophy (polarization; in comparison to normal hair shaft). F Bubble hair. G Pili torti (scanning electron microscopy [EM]). H Pili annulati. I Trichonodosis. J Pili trianguli et canaliculi (‘spun glass hair’). K Trichoptilosis. Some of the hair shaft abnormalities are seen in genetic syndromes (e.g. trichorrhexis invaginata in Netherton syndrome, trichoschisis in trichothiodystrophy). A, B, Courtesy, Maria K. Hordinsky, MD; F, Courtesy, Jean L. Bolognia, MD.
For further information see Ch. 69. From Dermatology, Third Edition.