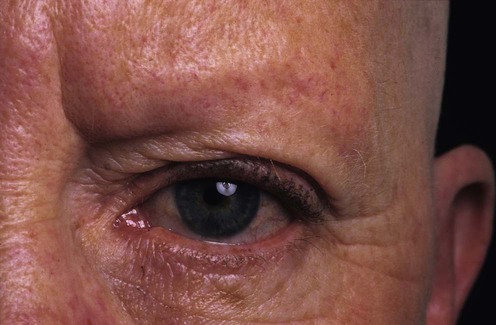
Alopecia areata
First-Line therapies
Second-Line therapies
Lack of efficacy of topical latanoprost and bimatoprost ophthalmic solutions in promoting eyelash growth in patients with alopecia areata.
Roseborough I, Lee H, Chwalek J, Stamper RL, Price VH. J Am Acad Dermatol 2009; 60: 705–6.
A controlled trial of 16 weeks duration with 11 patients did not confirm any response.
Another small trial of similar design has also shown the same negative result.
Third-Line therapies


 Intralesional steroids
Intralesional steroids Topical immunotherapy
Topical immunotherapy Topical corticosteroids
Topical corticosteroids Anthralin/dithranol
Anthralin/dithranol Retinoic acid
Retinoic acid Topical minoxidil
Topical minoxidil Bimatoprost / Latanoprost eye drops (for eyelashes)
Bimatoprost / Latanoprost eye drops (for eyelashes) PUVA
PUVA Systemic corticosteroids
Systemic corticosteroids Systemic cyclosporine
Systemic cyclosporine Oral minoxidil
Oral minoxidil Sulphasalazine
Sulphasalazine Methotrexate
Methotrexate Azathioprine
Azathioprine Inosiplex (inosine pranobex)
Inosiplex (inosine pranobex) Nitrogen mustard
Nitrogen mustard Dermatography
Dermatography Cryotherapy
Cryotherapy Pulsed infrared diode laser
Pulsed infrared diode laser Excimer laser
Excimer laser Topical bexarotene
Topical bexarotene Topical azelaic acid
Topical azelaic acid Combination treatment of simvastatin and ezetimibe
Combination treatment of simvastatin and ezetimibe Aromatherapy
Aromatherapy Onion juice
Onion juice Combination of topical garlic gel and topical betamethasone valerate
Combination of topical garlic gel and topical betamethasone valerate