161 Alcoholic Ketoacidosis
• Alcoholic ketoacidosis accounts for up to 20% of cases of ketoacidosis.
• The characteristic example is an alcoholic person who abruptly abstains and has signs and symptoms such as vomiting, abdominal pain, malnutrition, and an anion gap metabolic acidosis, but no measurable alcohol levels.
• Initial glucose levels may be low, normal, or high.
• A ratio of β-hydroxybutyrate to acetoacetate in excess of 10 : 1 is pathognomonic for alcoholic ketoacidosis, whereas a 3 : 1 ratio is more common in diabetic ketoacidosis.
• Treatment emphasizes hydration with dextrose-containing solutions and thiamine; resolution of the acidosis usually occurs within 6 to 12 hours.
• Mortality from uncomplicated alcoholic ketoacidosis is less than 1%.
Definition and Epidemiology
The diagnosis of alcoholic ketoacidosis (AKA) is established when an alcoholic patient is found to have an anion gap metabolic acidosis without historical or laboratory evidence suggesting an alternative cause. AKA may develop after protracted vomiting in malnourished, chronic alcoholics who consume a daily average of 200 g of ethanol. AKA generally occurs with equal frequency in adult men and women between 20 and 60 years of age. Its incidence and prevalence remain undefined. Up to one half of patients are likely to suffer recurrence. It is unclear whether these individuals have a genetic predisposition to AKA or whether they repeatedly reproduce the hormonal milieu that precipitates ketoacidosis. Almost one fifth of cases of ketoacidosis are alcoholic ketoacidosis.1–3
Pathophysiology
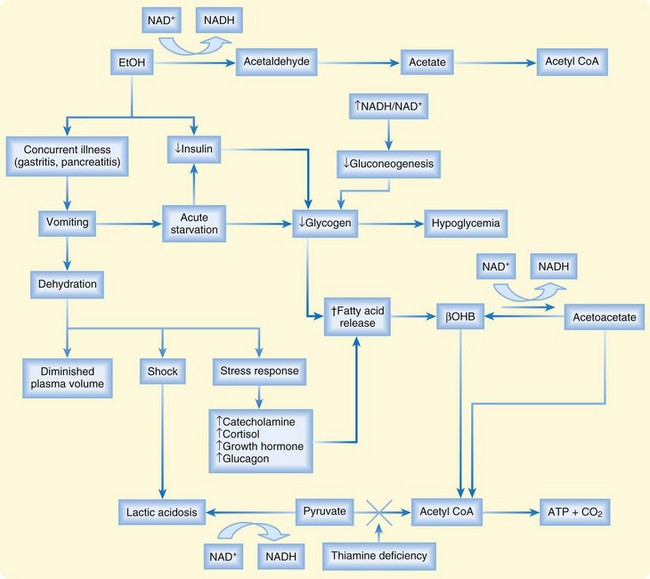
The term alcoholic acidosis describes a syndrome of four types of metabolic acidosis that occur in alcoholics and vary in severity: ketoacidosis, lactic acidosis, acetic acidosis, and loss of bicarbonate in urine. AKA arises from a complicated interplay of the metabolic effects of alcohol in fasted, dehydrated alcoholics who abruptly stop their intake of ethanol.4
β-Hydroxybutyrate is the predominant ketoacid.5 Metabolism of ethanol to acetaldehyde is catalyzed by alcohol dehydrogenase in the liver and results in accumulation of the reduced form of nicotinamide adenine dinucleotide (NADH) relative to the oxidized form of nicotinamide adenine dinucleotide (NAD+). The altered ratio of NADH/NAD+ is the rate-limiting step in alcohol metabolism and favors the conversion of acetoacetate to β-hydroxybutyrate, as illustrated in Figure 161.1.
Lactic acidosis is a common, concurrent acid-base disorder, in addition to ketoacidosis. Although lactic acidosis may result from another cause such as sepsis or seizures, alcohol consumption can cause mild accumulation of lactic acid by two distinct mechanisms. First, the elevated NADH/NAD+ ratio can shift the pyruvate–lactic acid equilibrium in favor of lactic acidosis. Second, the thiamine deficiency common in chronic alcoholics prohibits the alternative oxidation of pyruvate to acetyl coenzyme A because thiamine is a coenzyme in this reaction.6,7
Presenting Signs and Symptoms
Patients typically have a clear sensorium, are not confused, and are able to provide a complete history, although there are case reports of encephalopathic manifestations. Box 161.1 summarizes the sensitivity of signs and symptoms for AKA.
Diagnostic Testing
![]() Facts and Formulas
Facts and Formulas
Osmolar gap = [2 (Na) + (glucose/18) + (BUN/2.8) + (EtOH/4.6)].
An osmolar gap greater than 25 mOsm/kg is specific for methanol or ethylene glycol.
A β-hydroxybutyrate level greater than 386 µmol/L has been proposed as a forensic pathology cutoff to identify “ketoalcoholic death.” Levels higher than 2500 µmol/L can be fatal.
Because the nitroprusside reaction used in a urine dipstick tests for DKA, a negative urine dipstick test for “ketones” does not exclude AKA. In such instances, the dipstick may show paradoxic worsening of urine ketones as AKA resolves with treatment and β-hydroxybutyrate is converted to acetoacetate.8,9
Hypokalemia and hypophosphatemia are common with AKA, particularly as treatment progresses. Alcohol levels are generally zero, although case reports have noted the presence of AKA even when ethanol is detectable.10–12
Treatment
Initially normal levels of magnesium, potassium, and phosphorus decrease during treatment and require repletion. Intravenous thiamine supplementation (100 mg) provides theoretic prophylaxis against Wernicke encephalopathy and may help reverse the lactic acidosis. Exogenous insulin and bicarbonate therapy is rarely indicated.12–14
Disposition
If a thorough evaluation fails to reveal additional acute health issues, the acidosis can be treated and resolved within 6 to 12 hours. Discharged patients should have appropriate follow-up to address issues of chronic alcohol abuse. Patients may also benefit from an alcohol rehabilitation program (see Chapter 199). Discharge instructions should advise patients of their predisposition for recurrent episodes of AKA, as well as the potentially detrimental effect of alcohol abuse on other aspects of their health. Return precautions should include intractable vomiting, caloric starvation, and increasing abdominal pain.
1 Adams SL. Alcoholic ketoacidosis. Emerg Med Clin North Am. 1990;8:749–760.
2 Adams SL, Matthews JJ, Flaherty JJ. Alcoholic ketoacidosis. Ann Emerg Med. 1987;16:90–97.
3 Fulop M. Alcoholic ketoacidosis. Endocrinol Metab Clin North Am. 1993;22:209–219.
4 McGuire LC, Cruickshank AM, Munro PT. Alcoholic ketoacidosis. Emerg Med J. 2006;23:417–420.
5 Elliott S, Smith C, Cassidy D. The post mortem relationship between beta-hydroxybutyrate (BHB), acetone, and ethanol in ketoacidosis. Forensic Sci Int. 2010;198:53–57.
6 Halperin ML, Hammeke M, Josse RG, et al. Metabolic acidosis in the alcoholic: a pathophysiologic approach. Metabolism. 1983;32:308–315.
7 Iten PX, Meier M. Beta-hydroxybutyric acid—an indicator for an alcoholic ketoacidosis as cause of death in deceased alcohol abusers. J Forensic Sci. 2000;45:624–632.
8 Taboulet P, Haas L, Porcher R, et al. Urinary acetoacetate or capillary beta-hydroxybutyrate for the diagnosis of ketoacidosis in the emergency department setting. Eur J Emerg Med. 2004;11:251–258.
9 Smith SW, Manini AF, Szekely T, et al. Bedside detection of urine beta-hydroxybutyrate in diagnosing metabolic acidosis. Acad Emerg Med. 2008;15:751–756.
10 Umpierrez GE, DiGirolamo M, Tuvlin JA, et al. Differences in metabolic and hormonal milieu in diabetic and alcohol-induced ketoacidosis. J Crit Care. 2000;15:52–59.
11 Schelling JR, Howard RL, Winter SD, et al. Increased osmolal gap in alcoholic ketoacidosis and lactic acidosis. Ann Intern Med. 1990;113:580–582.
12 Hojer J. Severe metabolic acidosis in the alcoholic: differential diagnosis and management. Hum Exp Toxicol. 1996;15:482–488.
13 Marinella MA. Alcoholic ketoacidosis presenting with extreme hypoglycemia. Am J Emerg Med. 1997;15:280–281.
14 Bakker SJL, Ter Maaten JC, Hoorntje SJ, et al. Protection against cardiovascular collapse in an alcoholic patient with thiamine deficiency by concomitant alcoholic ketoacidosis. J Intern Med. 1997;242:179–183.