Chapter 97 Adult Thoracic and Lumbar Deformity
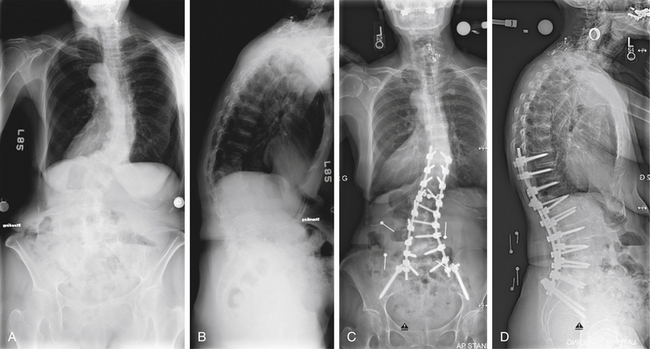
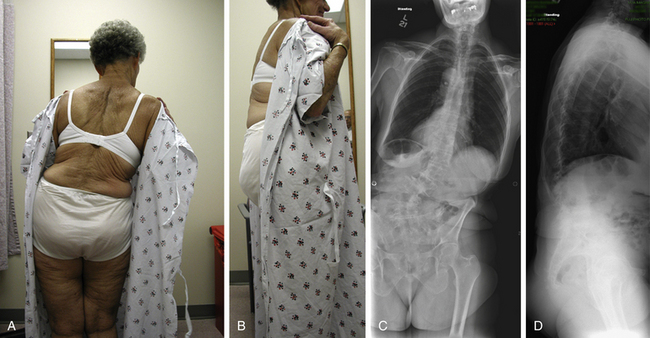
Deformity of the spine implies abnormality of proper spinal alignment that can lead to pain, instability, and neurologic and/or physiologic dysfunction. The deformity can occur in any plane (axial, coronal, or sagittal) and often involves a combination of abnormalities in multiple planes, as demonstrated by the patient in Figure 97-1. An accurate and accepted nomenclature is useful for describing deformities. Table 97-1 defines some common terms used in deformity and is in part adapted from the work of the Scoliosis Research Society (SRS) Terminology Committee and Working Group on Spinal Classification.1,2 Spinal deformity is a broad term that encompasses a variety of pathologies. Scoliosis is defined classically as “lateral curvature of the spine.” However, the pathophysiology of scoliosis can create a three-dimensional deformity involving abnormal spinal curvature (coronal deformity), rotation (axial deformity), and often kyphosis (sagittal deformity). Abnormal spinal profile in the sagittal plane (kyphosis or lordosis) can result in sagittal imbalance. In uncompensated hyperkyphosis, the normal upright posture of head over pelvis and feet (sagittal balance) is shifted forward. Spondylolisthesis is a regional abnormality in the sagittal plane in which one vertebra is displaced ventrally or dorsally in relation to an adjacent level.
TABLE 97-1 Glossary of Terms Frequently Used in Deformity
| Term | Meaning |
|---|---|
| Scoliosis | Lateral curvature of the spine (now recognized to be a three-dimensional deformity) |
| Kyphosis | Dorsal convex angulation of the spine |
| Hyperkyphosis | Kyphosis greater than the normal range |
| Hypokyphosis | Kyphosis of the thoracic spine less than the normal range |
| Lordosis | Ventral convex angulation of the spine |
| Hyperlordosis | Lordosis greater than the normal range |
| Hypolordosis | Lordosis of the cervical or lumbar spine less than the normal range |
| Kyphoscoliosis | Nonidiopathic scoliosis associated with an area of true hyperkyphosis |
| Lordoscoliosis | Scoliosis associated with an area of lordosis |
| Major curve | Curve with the largest Cobb measurement on upright long cassette radiograph of the spine |
| Minor curve | Any curve that does not have the largest Cobb measurement on upright long cassette radiograph of the spine |
| Structural curve | Measured spinal curve in the coronal plane in which the Cobb measurement fails to correct past zero on supine maximal voluntary lateral side-bending radiograph |
| Compensatory curve | Minor curve above or below a major curve that may or may not be structural |
| End vertebrae | Vertebrae that define the ends of a curve in a frontal or sagittal projection |
| Cephalad end vertebra | First vertebra in the cephalad direction from a curve apex whose superior surface is tilted maximally toward the concavity of the curve |
| Caudad end vertebra | First vertebra in the caudad direction from a curve apex whose inferior surface is tilted maximally toward the concavity of the curve |
| Neutral vertebra | Vertebra without axial rotation (in reference to the most cephalad and caudal vertebrae that are not rotated in a curve) |
| Apical vertebra | In a curve, the vertebra most deviated laterally from the vertical axis that passes through the patient’s sacrum (central sacral line) |
| Apical disc | In a curve, the disc most deviated laterally from the vertical axis of the patient that passes through the sacrum (central sacral line) |
| Stable vertebra | Thoracic or lumbar vertebra cephalad to a lumbar scoliosis that is most closely bisected by a vertically directed central sacral line assuming the pelvis is level. Alternatively, both pedicles of this vertebra should lie between vertical reference lines drawn from the sacroiliac joints. |
| Central sacral line (central sacral vertical line) | Vertical line in a frontal radiograph that passes through the center of the sacrum (identified by suitable landmarks, preferably on the first sacral segment) |
| C7 plumb line | Vertical line in a frontal radiograph drawn from the center of C7 (i.e., spinous process) down, which is used to measure compensation (coronal balance) relative to the central sacral line |
| Vertical line in a lateral radiograph drawn from the C7 centroid |
Spinal deformity has multiple causes, including, but not limited to, (1) unknown factors likely related to genetic presusceptibility (as in adolescent idiopathic scoliosis), (2) congenital abnormalities, (3) neuromuscular conditions (i.e., cerebral palsy, spinal cord injury), or (4) conditions associated with spinal cord dysfunction such as myelomeningocele. Deformity can also result as a consequence of trauma (i.e., posttraumatic kyphosis), infection, malignancy, degeneration, or iatrogenic causes. Table 97-2 lists some of these causes. The goal of deformity surgery, despite the etiology, is the relief of the patient’s symptoms while achieving a balanced spine.
TABLE 97-2 Etiology of Deformity
| Deformity | Etiology |
|---|---|
| Idiopathic scoliosis Infantile (2 months to 3 years of age) Juvenile (3 to 10 years of age) Adolescent (>10 years of age) Adult (after skeletal maturity) |
Unknown factors likely related to genetic presusceptibility subtype classified by age of onset |
| Congenital scoliosis | In utero derangement of vertebral formation or segmentation |
| Neuromuscular scoliosis | Result of neurologic injury such as spinal cord injury, cerebral palsy, or conditions associated with spinal cord dysfunction (myelomeningocele, tethered cord, spinal dysraphisim) |
| Posttraumatic deformity | Following fracture with progressive vertebral collapse and angulation |
| Postinfectious deformity | Following vertebral osteomyelitis/discitis with vertebral destruction following tuberculosis infection (Pott disease) |
| Degenerative scoliosis and kyphosis | Consequence of advanced degenerative changes |
| Iatrogenic deformity | Consequence of previous interventions (i.e., laminectomy) |
Conditions often detected and treated in the pediatric population, such as adolescent idiopathic scoliosis, Scheuermann kyphosis, congenital scoliosis, neuromuscular scoliosis, and scoliosis associated with other congenital syndromes (syndromic), are discussed in greater detail elsewhere in this text. This chapter will focus on the clinical and radiographic diagnosis, classification, and nonoperative management of adult thoracic and lumbar spinal deformity, with attention paid to scoliosis and kyphosis. Symptomatic deformity in adults is most frequently a consequence of advanced degenerative disease and is termed degenerative or de novo scoliosis. Curves are thought to result as a consequence of asymmetrical degeneration of lumbar discs and facet joints.3 The operative techniques used in treatment of adult thoracic and lumbar deformity are discussed in a later chapter.
Clinical Evaluation of the Adult Patient with Spinal Deformity
Key components of the physical examination include an assessment of the patient’s gait, a musculoskeletal evaluation, and a thorough neurologic examination. Signs of myelopathy such as hyperreflexia, clonus, and an impaired gait may be present in patients with severe thoracic or concomitant cervical disease. Other conditions that may contribute to the deformity such as a leg length discrepancy should be sought. The cosmetic appearance of the deformity is also a considerable factor in the psychosocial well-being of the patient. The importance of appearance is accepted in children but has yet to be thoroughly evaluated in adults.4,5
Diagnostic Imaging
Diagnostic imaging is crucial in the evaluation and management of patients with thoracic or lumbar deformity. A multimodal approach, including MRI and CT, is often used. However, much information can be elucidated from standard radiographs.
Conventional Radiographs
Standing frontal (anteroposterior or posteroanterior) and sagittal (lateral) whole spine (i.e., 14 × 36-inch long cassette or digitally stitched) radiographs are required in the proper evaluation of patients with spinal deformity. Radiographs should show the occiput and shoulders superiorly and the pelvis, including femoral heads, inferiorly.6 Standing views should be taken in a standardized position with the patient’s hips and knees in extension to remove potential compensation of sagittal imbalance. Frontal radiographs are oriented with the patient’s right side on the right side of the screen or view box. This orientation allows the observer to view the film as if he or she is standing behind the patient examining the spine, or as he or she would see it while performing surgery using a dorsal approach. Sagittal radiographs are oriented with the patient facing right. Proper orientation of full-length scoliosis radiographs is demonstrated in Figure 97-2.
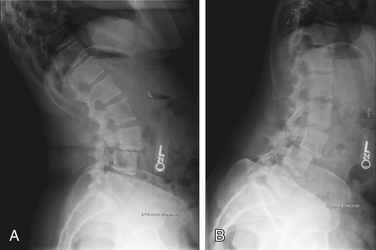
A comparison between the degree of deformity between weight-bearing and non–weight-bearing films (i.e., supine) gives some information regarding the rigidity of the deformity. Additional views to help determine stiffness of the deformity can be useful. These views include supine lateral bending films, bending films over a bolster, fulcrum bending films, and push and traction views. In the evaluation of spondylolisthesis, dynamic lateral views, shown in Figure 97-3, of the lumbar spine are used to help determine the degree of instability. Additional plain radiographic views that are useful in deformity include oblique views to visualize the pars interarticularis, the Ferguson view to better visualize the sacral region, and the Stagnara or Leeds view (an oblique view through the apical region of a scoliotic curve that accounts for rotation) to better visualize the pedicles.
Advanced Imaging
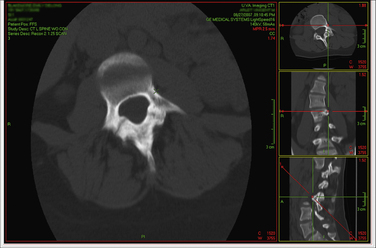
Advances in imaging software such as multiplanar rendering (MPR) allow the surgeon to view multislice CT and MRI data in multiple and adjustable planes. This allows for more accurate preoperative measurement of pedicle diameter and a greater appreciation of the disease process, as shown in Figure 97-4. Three-dimensional reconstructions can easily be created to aid in operative planning. It is also possible to have models of an individual patient’s spine fabricated and surgery simulated prior to the patient reaching the operating room.7,8 In our opinion, thin-cut CT myelography plus MPR provides extremely useful information in operative planning for deformity.
Diagnostic Imaging Conventions and Measurements
The location of a sagittal or coronal deformity is defined by the location of the apex of the curve. The apex is the disc or vertebra that is maximally displaced and minimally angulated. A deformity is considered thoracic if it has an apex between the T2 and the T11-12 disc, thoracolumbar if the apex lies between the T12 and L1 vertebrae, and lumbar if the apex is at or distal to the L1-2 disc.6 In scoliosis, the curve is described based on the side of its convexity. Convex to the right is known as dextroscoliosis, and convex to the left is known as levoscoliosis. Rarely is there just a single curve in scoliosis. The largest curve is called the “main” curve, which is typically structural (e.g., the curve does not correct completely on bending radiographs). Compensatory curves develop in response to the main structural curve and serve the purpose of maintaining spinal balance. Compensatory curves may or may not be structural.
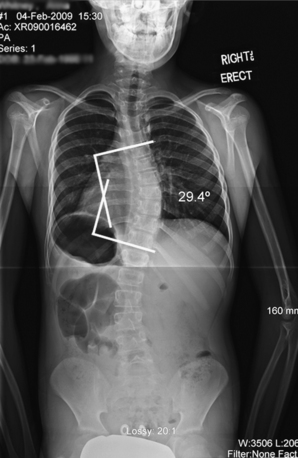
Curve degree is measured via the Cobb method as illustrated in Figure 97-5. Originally described by John Cobb in 1948, the technique involves selecting vertebrae maximally tilted into the curve (end vertebrae). Lines are drawn parallel to the superior end plate of the cephalad end vertebra and the inferior end plate of the caudal end vertebra. If the end plates are not clearly visualized, an alternative technique is to use the pedicle margins as the basis for these lines.9 Bisecting perpendicular lines from the end-plate lines are drawn and the angle determined. The Cobb technique is classically thought to have an inherent error of 3 to 5 degrees; therefore, a change in angle between consecutive films has to be greater than 5 degrees to be considered a true change. Intraobserver error ranges between 1% and 5%, and interobserver error can be as high as 10 degrees.10 Modern Picture Archive and Communication Systems (PACS) workstations and image viewers have tools to measure Cobb angles digitally. To date, studies comparing Cobb angle measurements of primary and secondary curves on digital radiographs and traditional radiographs have shown no statistical difference in the intraobserver or interobserver variance between the two techniques.11–13 New systems that automatically measure the Cobb angle and determine rotation are currently under development and may be able to reduce intraobserver and interobserver variability.14 Proximal and distal neutral vertebrae (not rotated in the axial plane) as well as stable vertebrae (vertebrae above and below the end vertebra that is bisected by the central sacral vertical line [CSVL]) should also be determined because these are used to help select fusion levels in operative planning.
The Cobb method, although initially described for measurement of coronal deformity, is also used to measure degree of lordosis and kyphosis in the sagittal plane. In patients with a normal spinal profile, thoracic kyphosis typically measures between 30 and 35 degrees and lumbar lordosis ranges between 35 and 50 degrees. Approximately two thirds of the total lordosis of the lumbar spine occurs at L4-S1.15
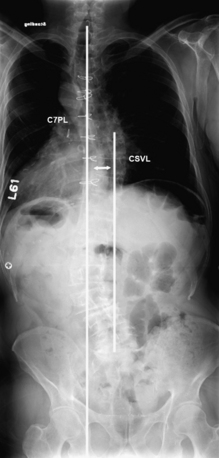
Spinal balance in the coronal and sagittal planes is determined through the use of vertical reference lines. The CSVL is a line drawn up through the center of the sacrum parallel to the edge of the film (e.g., perpendicular to the floor). The C7 plumb line (C7PL) on a frontal radiograph is a vertical line drawn down from the midportion of the C7 vertebral body (approximated by the spinous process, or more accurately through determination of the centroid). Coronal balance, demonstrated in Figure 97-6, is determined by measuring the distance between these reference lines. By convention, a difference with the C7PL to the left is considered negative and a difference toward the right is positive.
Sagittal balance, shown in Figure 97-7, is determined on a lateral radiograph by measuring the distance between the C7PL, drawn from the centroid (geometric center of the vertebrae) of C7 down and the dorsal/rostral corner of the sacrum. This difference is known as the sagittal vertical axis (SVA). The balance is considered positive if the C7PL falls ventral to this reference point and negative if it falls dorsal to it. Normal mean SVA offset is +0.5 cm and lies within a tight range between −1.0 and +1.0 cm.
Axial rotation on plain radiographs can be determined using the Nash-Moe method. The Nash-Moe method categorizes vertebral rotation into five grades based on the location of the pedicle in relation to the lateral aspect of the vertebral body.16 CT measurement of rotation may be more reliable than standard radiographic techniques.17
Overall sagittal balance of the patient is greatly affected by relationship of the spine to the pelvis.18 An adult patient with thoracic hyperkyphosis or loss of lumbar lordosis attempts to compensate for spinal sagittal imbalance through pelvic retroversion and hip extension, thereby attempting to bring his or her head back over the center of the pelvis. In the operative planning for deformity, including fusion to the sacrum or pelvis, spinopelvic relationships, including these compensatory mechanisms, should be taken into account. Figure 97-8 demonstrates the spinopelvic measurements, including pelvic tilt, sacral slope, and pelvic incidence. Pelvic tilt (a measure of the degree of pelvic retroversion [e.g., compensation for sagittal imbalance]) is the angle determined between a vertical reference line drawn up from the center of the femoral heads (femoral head axis) and a line drawn from the femoral head axis to the midpoint of the sacral end plate. If femoral heads are not perfectly aligned on a lateral radiograph, the location of the femoral head axis is approximated by the midpoint of a line connecting the geometric center of each femoral head. Sacral slope simply is the angle of a line drawn along the sacral end plate and the horizontal. Pelvic incidence is measured by determining the angle between a line drawn perpendicular to the sacral end plate at its midpoint and a line from the femoral head axis to this point. The pelvic incidence is equal to the pelvic tilt plus the sacral slope.19
The relationship between pelvic incidence and lumbar lordosis has been determined in normal subjects. It can be approximated by the pelvic incidence + 9 degrees (±9).19
Scoliosis Classification
Classification systems in spinal deformity are useful in that they can facilitate communication, allow comparison of similar cases, and provide a framework for an evidence-based approach to understanding prognosis and guiding management.20,21 The need for a reliable adult classification system distinct from established pediatric scoliosis classification systems (i.e., King-Moe, Lenke) has recently been recognized.22,23 Pediatric classification systems, when introduced, predominantly aimed to help select fusion levels for the correction of deformity in adolescent idiopathic scoliosis. In contrast, adult classification systems need to address a “wide variability in segmental, regional, and global alignment” plus incorporate the clinical symptoms affecting the patient in order to be clinically useful.24
Aebi Classification
In 2005, Max Aebi proposed classifying adult scoliosis into four groups based on the apparent etiology of the disease (Table 97-3).
Type I: primary degenerative (“de novo”) scoliosis due to asymmetrical disc and facet joint degeneration occurring most commonly in the lumbar or thoracolumbar region (apex at L2-3 or L3-4 most frequently)
Type II: progressive idiopathic scoliosis due to continued progression of a curve that has existed since childhood or adolescence
Type IIIa: secondary adult scoliosis with deformity due to a preexisting condition either intrinsic to the spine (i.e., an adjacent curve present since childhood or adolescence) or due to a condition extrinsic to the spine (i.e., pelvic obliquity caused by a leg length discrepancy)
Type IIIb: secondary adult deformity progressing due to bone weakness (i.e., caused by osteoporotic compression fracture)25
| Type | Description | Etiology |
|---|---|---|
| I | Primary degenerative scoliosis, apex at L2, L3, or L4 | Asymmetrical disc degeneration and facet joint degeneration |
| II | Progressive idiopathic scoliosis | Progression due to mechanical or degenerative changes of an already present adolescent scoliosis |
| III (a) | Secondary adult scoliosis | Secondary to an adjacent thoracic or thoracolumbar curve; obliquity of the pelvis with secondary lumbar/thoracolumbar curve |
| III (b) | Deformity progressing mostly due to bone weakness | Metabolic bone disease, osteoporosis |
Modified from Aebi M: The adult scoliosis. Eur Spine J 14:925–948, 2005.
Schwab Classification
In 2006, Frank Schwab introduced a classification system for adult scoliosis based on “high impact clinically significant radiographic parameters” through a prospective study of 947 adult patients with deformity.26 He justified this approach to classification through previous studies that demonstrated the “impact” of radiographic parameters on self-assessed function.27–29 Interestingly, sagittal imbalance through a loss of lumbar lordosis and lumbar vertebra obliquity, not the Cobb angle on frontal radiographs, most closely correlated with pain scores on self-assessment. Other “impact” radiographic factors included global imbalance, apical level of scoliotic deformity, and intervertebral subluxation.
The original Schwab system categorizes patients into five groups based on location of the apex of the main (major) curve on standing frontal full-length radiographs (Box 97-1). The scheme then further classifies patients through the use of two modifiers accounting for degree of lumbar lordosis and subluxation on either frontal or sagittal radiographs, because these factors were found to have the highest clinical significance. In 2007, the classification system was modified to account for patients with deformity in the sagittal plane alone through the addition of a sixth group. In addition, a global balance modifier was added; this factor has been increasingly recognized as being “high impact”30 (see Box 97-1).
BOX 97-1 Schwab Adult Classification of Adult Deformity
Type
Location of the deformity (apical level of the major curve or sagittal plane only)
• Type I: thoracic-only scoliosis (no thoracolumbar or lumbar component)
• Type II: upper thoracic major, apex T4-8 (with thoracolumbar or lumbar curve)
• Type III: lower thoracic major, apex T9-10 (with thoracolumbar/lumbar curve)
• Type IV: thoracolumbar major curve, apex T11-L1 (with any other minor curve)
• Type V: lumbar major curve, apex L2-4 (with any other minor curve)
From Schwab F, Lafage V, Farcy JP, et al: Surgical rates and operative outcome analysis in thoracolumbar and lumbar major adult scoliosis: application of the new adult deformity classification. Spine (Phila Pa 1976) 32:2723–2730, 2007.
Apical Level
The six groups of the Schwab classification are as follows:
Type I: patients with thoracic-only scoliosis, with no thoracolumbar or lumbar curvature
Type II: patients with an upper thoracic major curve, apex T4-8, with a thoracolumbar or lumbar minor curve
Type III: patients with a lower thoracic major curve, apex T9-10, with a thoracolumbar or lumbar minor curve
Type IV: patients with a thoracolumbar major curve, apex T11-L1, with any other minor curve
Type V: patients with a lumbar major curve, apex L2-4, with any other minor curve
Global Balance Modifier
Since its introduction, the authors of the Schwab classification system have been examining the scheme with regard to how the type of deformity and modifiers relate to rates of surgery, surgical approach, use of osteotomies, and fusion extension to the sacrum, as well as to predictors of outcome and complications.24,31 They found that modifiers of the classification had significant variation in surgical rates as the grade of modifier increased.24 As lordosis is lost, surgical rates increase significantly (group A, 37%, group C, 51%; P = .05). With increasing subluxation (0–++), the operative rate increases from 35% to 52% (P < .05). Similarly, as sagittal balance increases from N to P to VP, surgical rate significantly increases 39%, 46%, and 58%, respectively (N vs. VP; P = .02). Loss of lumbar lordosis, lordosis modifiers B and C, and marked subluxation (modifier ++) were associated with more circumferential surgery. Sagittal imbalance was associated with higher rates of dorsal-only surgery. Osteotomies were also used more frequently in cases of sagittal imbalance and increasing loss of lumbar lordosis. Higher rates of fixation to the sacrum were found to be associated with loss of lumbar lordosis (groups B and C) and with increasing positive sagittal balance (P = .0006).24
In evaluating the system in terms of surgical outcome, the authors found that patients with no lordosis (modifier C) had the greatest disability prior to surgery, showed the greatest improvement with dorsal-only procedures, and had the least disability at 1-year follow-up.24 Patients most likely to obtain significant benefit through surgery had higher grades of deformity through the classification modifiers and a higher degree of disability before surgery (high Oswestry Disability Index [ODI] score; low SRS and SF-12 scores). They propose that patients with less morbidity prior to surgical intervention have less of an opportunity to improve and may be more affected by the significant morbidity associated with surgery.31
Scoliosis Research Society Classification
In 2006, the SRS introduced and validated a classification system for adult deformity with the intention of providing an organizational structure for spinal deformity to permit comparison of similar cases and provide a framework for an evidence-based approach to operative and nonoperative management (Box 97-2).20 The classification categorizes patients into seven types based on the major curve type on standing radiographs. Modifiers are added for deformity in the sagittal plane, degenerative changes in the lumbar spine, and global balance in the sagittal and coronal planes.
BOX 97-2 Scoliosis Research Society Classification System for Adult Deformity
Adult Spinal Deformity Modifiers
Regional sagittal modifier (include only if outside normal range, as listed)
• Proximal thoracic (PT; T2-5): 20 degrees
• Main thoracic (MT; T5-12): 50 degrees
Lumbar degenerative modifier (include only if present)
• Two-disc height and facet arthropathy based on radiograph; include lowest involved level between L1 and S1
• Listhesis (rotational, coronal, or sagittal) 3 mm; include lowest level between L1 and L5
• Junctional L5-S1 curve 10 degrees (intersection angle superior end plates L5 and S1)
Global balance modifier (include only if imbalance present)
Scoliosis Research Society definition of regions
Criteria for specific major curve types
• Apical vertebral body lateral to C7 plumb line
• T1 rib or clavicle angle 10 degrees upper thoracic curves
2. Thoracolumbar and lumbar curves
• Apical vertebral body lateral to CSVL
3. Primary sagittal plane deformity
• One or more regional sagittal measurements (PT, MT, TL, L) outside normal range
From Lowe T, Berven SH, Schwab FJ, et al: The SRS classification for adult spinal deformity: building on the King/Moe and Lenke classification systems. Spine (Phila Pa 1976) 31:S119–S125, 2006.
Major Curve Types
The system identifies six major coronal curve types, plus a seventh additional type:
Sagittal Modifiers
Proximal thoracic (PT) T2-5 for kyphosis: greater than or equal to 20 degrees
Main thoracic (MT) T5-12 for kyphosis: greater than or equal to 50 degrees
Thoracolumbar (TL) T10-L2 for kyphosis: greater than or equal to 20 degrees
Lumbar (L) T12-S1 for kyphosis (loss of lordosis): greater than or equal to −40 degrees
Lumbar Degenerative Modifiers
Lumbar degenerative change modifiers were included in the system because it has been recognized that degenerative changes within the lumbar spine are often responsible for the presenting clinical symptoms in adult patients with deformity.20 Modifiers included in the system account for the following conditions:
Global Balance Modifier
The SRS system was evaluated for interobserver variability through the analysis of 14 expert surgeons’ choice of classification of 25 radiographic cases. There was good interobserver reliability for primary curve type (κ = 0.64), regional sagittal modifier (κ = 0.73), degenerative lumbar modifier (κ = 0.65), and global balance modifier (κ = 0.92). These same surgeons were queried regarding selection of fusion levels for operative intervention. Although there was good agreement on selection of the caudal level (κ = 0.77), there was significantly higher variability in choice of cephalad level (κ = 0.56).20 Figure 97-9 shows a case example of a patient with adult degenerative scoliosis. This patient demonstrates how to use both the Schwab and SRS classification systems properly.
Initial Management of Adult Thoracic and Lumbar Deformity
Indications for operative intervention in adult deformity include worsening pain, worsening neurologic function, progression of the deformity clinically and radiographically, and failure of nonoperative management. Predictive models are being developed to determine which patients will receive the most benefit through operative versus nonoperative approaches to deformity.31 In most instances, conservative management is attempted before proceeding with surgery (often prior to referral to a spine surgeon), although evidence to support many of the modalities used is lacking. Nonoperative strategies include pain management with oral analgesics and nonsteroidal anti-inflammatory drugs, fluoroscopic-guided steroid injections (epidural steroid injection, facet joint blocks, selective nerve root block), physical therapy to increase core strength (including strategies to help unload the spine such as aquatic therapy), and nonconventional therapies such as massage and acupuncture.32 Bracing has not been shown to be of considerable benefit in adult deformity and may lead to deconditioning.32,33
In 2010, Glassman et al. evaluated the costs and benefits of nonoperative management for adult scoliosis in a cohort of 123 patients. The researchers used data collected prospectively over a 2-year period. They divided patients into three groups based on degree of disability: low-symptom (ODI ≤ 20), mid-symptom (ODI 21 to 39), and high-symptom (ODI ≥ 40). Fewer total resources were used by the low-symptom group; however, all groups used substantial resources. Modalities included medications, exercise therapy, injections, physical therapy, chiropractic care, bed rest, and bracing. None of these treatments demonstrated benefit as measured by health-related quality of life (HR-QOL) scores. Patients who received no treatment actually showed slightly better outcomes over the 2-year period than patients who had some form of nonoperative therapy. The mean cost of treatment was $4418 in the first year and $6397 in the second year. There was no significant difference in treatment cost between the groups.34
Several recent papers have demonstrated significant, long-term benefit for the surgical management of patients, including the elderly, with adult deformity.35–37 Smith et al., in a recent retrospective review of prospectively collected multicenter data for adult deformity, evaluated 206 patients treated surgically for deformity. Patients were divided into groups based on age: 25 to 44 years, 45 to 64 years, and 65 to 85 years. Risks and benefits were assessed through evaluation of complications suffered (minor and major) and through accepted measures of health status, disability, and pain (HR-QOL, ODI, SF-12, SRS-22 questionnaire, Numeric Rating Scale [NRS]). In each of the age groups evaluated, outcome measures improved significantly on 2-year follow-up. The oldest group of patients at baseline had the greatest degree of disability and pain as well as the worst health status of the groups. The eldest group also experienced the highest rate of surgical complications, having close to four times the number of minor complications and five times the number of major complications when compared to the youngest age group.37 Despite this, the group with the oldest patients at 2 years had measures of disability, pain, and health status indistinguishable from the other groups.37 These results suggested that elderly high-risk patients may stand to gain disproportionately greater improvement in disability and pain.”37 However, the degree of disability has to be weighed against an individual’s comorbidities and risk of surgical complications. Conservative management should be attempted initially in most cases.
Factors that can affect outcome should be addressed prior to intervention. Smoking is a relative contraindication to spinal fusion procedures, because it leads to higher rates of pseudarthrosis. In his recent evaluation of reoperation after primary fusion for adult spinal deformity, Mok found that smoking was a significant risk factor for revision.38 Patients who smoke should make every attempt not only to quit but to wean themselves from nicotine dependence. Bone health, especially in elderly patients, needs to be considered and maximized.39 A bone mineral density scan should be obtained in patients suspected of being osteopenic or osteoporotic, and medical therapy to increase bone density started if indicated. The vitamin D level should be checked, and supplementation with vitamin D and calcium should be started in many patients. Patients with significant medical comorbidities should have appropriate clearance for operative intervention. Finally, patients suspected of having some respiratory compromise should have pulmonary function tests and an evaluation by a pulmonologist.
Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925-948.
Bridwell K.H., Baldus C., Berven S., et al. Changes in radiographic and clinical outcomes with primary treatment adult spinal deformity surgeries from two years to three- to five-years follow-up. Spine (Phila Pa 1976). 2010;35:1849-1854.
Lenke L.G., Betz R.R., Harms Jr., et al. Adolescent idiopathic scoliosis. J Bone Joint Surg [Am]. 2001;83:1169.
Smith J.S., Shaffrey C.I., Glassman S.D., et al. Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine (Phila Pa 1976). 2011;36(15):1218-1228.
Smith J.S., Shaffrey C.I., Kuntz C.I.V., et al. Classification systems for adolescent and adult scoliosis. Neurosurgery. 2008;63:A16-A24.
Stokes I.A. Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine (Phila Pa 1976). 1994;19:236-248.
1. Lenke L. SRS Terminology Committee and Working Group on Spinal Classification Revised Glossary of Terms. 2000. www.srs.org/professionals/glossary/glossary.php.
2. Stokes I.A. Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine (Phila Pa 1976). 1994;19:236-248.
3. Birknes J.K., Harrop J.S., White A.P., et al. Adult degenerative scoliosis: a review. Neurosurgery. 2008;63:A94-A103.
4. Koch K.D., Buchanan R., Birch J.G., et al. Adolescents undergoing surgery for idiopathic scoliosis: how physical and psychological characteristics relate to patient satisfaction with the cosmetic result. Spine (Phila Pa 1976). 2001;26:2119-2124.
5. Smith P.L., Donaldson S., Hedden D., et al. Parents’ and patients’ perceptions of postoperative appearance in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2006;31:2367-2374.
6. Angevine P.D., Kaiser M.G. Radiographic measurement techniques. Neurosurgery. 2008;63(Suppl 3):A40-A45.
7. Mao K., Wang Y., Xiao S., et al. Clinical application of computer-designed polystyrene models in complex severe spinal deformities: a pilot study. Eur Spine J. 2010;19:797-802.
8. Yamazaki M., Okawa A., Fujiyoshi T., et al. Simulated surgery for a patient with neurofibromatosis type-1 who had severe cervicothoracic kyphoscoliosis and an anomalous vertebral artery. Spine (Phila Pa 1976). 2010;35:E368-E373.
9. Mehta S.S., Modi H.N., Srinivasalu S., et al. Interobserver and intraobserver reliability of Cobb angle measurement: endplate versus pedicle as bony landmarks for measurement: a statistical analysis. J Pediatr Orthop. 2009;29:749-754.
10. Morrissy R.T., Goldsmith G.S., Hall E.C., et al. Measurement of the Cobb angle on radiographs of patients who have scoliosis. Evaluation of intrinsic error. J Bone Joint Surg [Am]. 1990;72:320-327.
11. Gstoettner M., Sekyra K., Walochnik N., et al. Inter- and intraobserver reliability assessment of the Cobb angle: manual versus digital measurement tools. Eur Spine J. 2007;16:1587-1592.
12. Kuklo T.R., Potter B.K., Schroeder T.M., et al. Comparison of manual and digital measurements in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2006;31:1240-1246.
13. Mok J.M., Berven S.H., Diab M., et al. Comparison of observer variation in conventional and three digital radiographic methods used in the evaluation of patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2008;33:681-686.
14. Zhang J., Lou E., Hill D.L., et al. Computer-aided assessment of scoliosis on posteroanterior radiographs. Med Biol Eng Comput. 2010;48:185-195.
15. Jackson R.P., McManus A.C. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine (Phila Pa 1976). 1994;19:1611-1618.
16. Nash C.L.Jr., Moe J.H. A study of vertebral rotation. J Bone Joint Surg [Am]. 1969;51:223-229.
17. Lam G.C., Hill D.L., Le L.H., et al. Vertebral rotation measurement: a summary and comparison of common radiographic and CT methods. Scoliosis. 2008;3:16.
18. Schwab F., Lafage V., Patel A., et al. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). 2009;34:1828-1833.
19. Boulay C., Tardieu C., Hecquet J., et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415-422.
20. Lowe T., Berven S.H., Schwab F.J., et al. The SRS classification for adult spinal deformity: building on the King/Moe and Lenke classification systems. Spine (Phila Pa 1976). 2006;31:S119-S125.
21. Smith J.S., Shaffrey C.I., Kuntz C.I.V., et al. Classification systems for adolescent and adult scoliosis. Neurosurgery. 2008;63:A16-A24.
22. King H.A., Moe J.H., Bradford D.S., et al. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg [Am]. 1983;65:1302-1313.
23. Lenke L.G., Betz R.R., Harms J.Jr., et al. Adolescent idiopathic scoliosis. J Bone Joint Surg [Am]. 2001;83:1169.
24. Schwab F., Lafage V., Farcy J.P., et al. Surgical rates and operative outcome analysis in thoracolumbar and lumbar major adult scoliosis: application of the new adult deformity classification. Spine (Phila Pa 1976). 2007;32:2723-2730.
25. Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925-948.
26. Schwab F., Farcy J.P., Bridwell K., et al. A clinical impact classification of scoliosis in the adult. Spine (Phila Pa 1976). 2006;31:2109-2114.
27. Glassman S.D., Berven S., Bridwell K., et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 2005;30:682-688.
28. Schwab F., Dubey A., Pagala M., et al. Adult scoliosis: a health assessment analysis by SF-36. Spine (Phila Pa 1976). 2003;28:602-606.
29. Schwab F., el-Fegoun A.B., Gamez L., et al. A lumbar classification of scoliosis in the adult patient: preliminary approach. Spine (Phila Pa 1976). 2005;30:1670-1673.
30. Glassman S.D., Bridwell K., Dimar J.R., et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30:2024-2029.
31. Schwab F.J., Lafage V., Farcy J.P., et al. Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine (Phila Pa 1976). 2008;33:2243-2247.
32. Silva F.E., Lenke L.G. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus. 2010;28:E1.
33. Heary R.F., Kumar S., Bono C.M. Bracing for scoliosis. Neurosurgery. 2008;63:A125-A130.
34. Glassman S.D., Carreon L.Y., Shaffrey C.I., et al. The costs and benefits of nonoperative management for adult scoliosis. Spine (Phila Pa 1976). 2010;35:578-582.
35. Bridwell K.H., Baldus C., Berven S., et al. Changes in radiographic and clinical outcomes with primary treatment adult spinal deformity surgeries from two years to three- to five-years follow-up. Spine (Phila Pa 1976). 2010;35:1849-1854.
36. Smith J.S., Shaffrey C.I., Berven S., et al. Operative versus nonoperative treatment of leg pain in adults with scoliosis: a retrospective review of a prospective multicenter database with two-year follow-up. Spine (Phila Pa 1976). 2009;34:1693-1698.
37. Smith J.S., Shaffrey C.I., Glassman S.D., et al. Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine. 2011;36(15):1218-1228.
38. Mok J.M., Cloyd J.M., Bradford D.S., et al. Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine. 2009;34:832-839.
39. Dipaola C.P., Bible J.E., Biswas D., et al. Survey of spine surgeons on attitudes regarding osteoporosis and osteomalacia screening and treatment for fractures, fusion surgery, and pseudoarthrosis. Spine J. 2009;9:537-544.