Adult Reconstruction
SECTION 1 HIP DYSPLASIA—ADULT PRESENTATION
SECTION 2 HIP ARTHRITIS ASSESSMENT
SECTION 3 HIP ARTHRITIS TREATMENT
SECTION 4 OSTEONECROSIS OF THE HIP
SECTION 5 TOTAL HIP ARTHROPLASTY
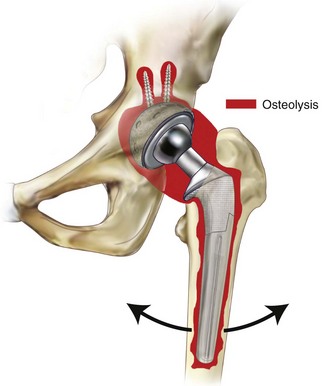
III. Osteolysis Around THA Prosthesis—Effective Joint Space
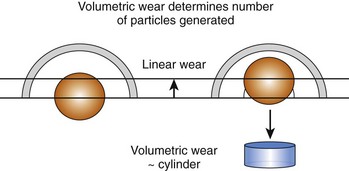
IV. Particle Debris Formation—Linear versus Volumetric Wear
SECTION 8 PERIPROSTHETIC THA FRACTURE
SECTION 9 TOTAL ARTICULAR RESURFACING
SECTION 11 THA—JOINT STABILITY
I. Incidence of THA Dislocation
II. Risk Factors for Dislocation
III. Dislocating THA—Assessment
SECTION 12 THA—ARTICULAR BEARING TECHNOLOGY
SECTION 13 KNEE ARTHRITIS ASSESSMENT
SECTION 14 KNEE ARTHRITIS TREATMENT
SECTION 15 TOTAL KNEE ARTHROPLASTY
IV. Preoperative Planning for TKA
VI. Coronal Plane Ligament Balancing in TKA
II. Cruciate-Retaining Primary TKA Design
III. Cruciate-Sacrificing Primary TKA Design
IV. Posterior Stabilized Primary TKA Design
V. Anterior Stabilized Primary TKA Design
VI. Tibial Rotating Platform in Primary TKA
SECTION 18 PATELLAR TRACKING IN TKA
III. TKA Techniques to Optimize Patellar Tracking
IV. Intraoperative Assessment of Maltracking
SECTION 19 CATASTROPHIC WEAR IN TKA
I. Premature Failure of TKA Implant
II. Factors Involved in Catastrophic Wear
SECTION 20 SHOULDER ARTHROPLASTY
I. Glenohumeral Arthritis and Glenoid Wear
II. Shoulder Arthroplasty—Contraindications
section 1 Hip Dysplasia—Adult Presentation
A Hip pain in adults under the age of 50 years usually is a result of hip dysplasia.
B Untreated dysplasia leads to degenerative joint disease in greater than 50% of patients by age 50 years.
C Initial presentation of symptoms is soon followed by degeneration.
III CLASSIFICATION OF ADULT HIP DYSPLASIA
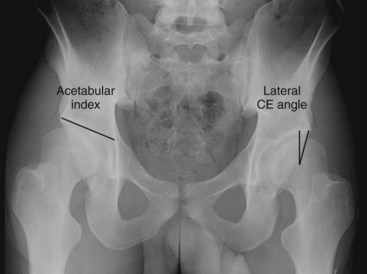
IV ACETABULAR DYSPLASIA (Box 5-1 and Figure 5-1)
A Classical (too little coverage)
VI CLINICAL SYNDROME ASSOCIATED WITH DYSPLASIA
A Femoral acetabular impingement
1. Impingement pain and hip inflammation
2. Labral degeneration leading to tears
D Causes of femoral acetabular impingement
E Femoral acetabular impingement—two types
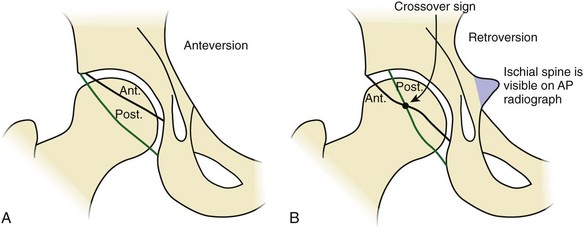
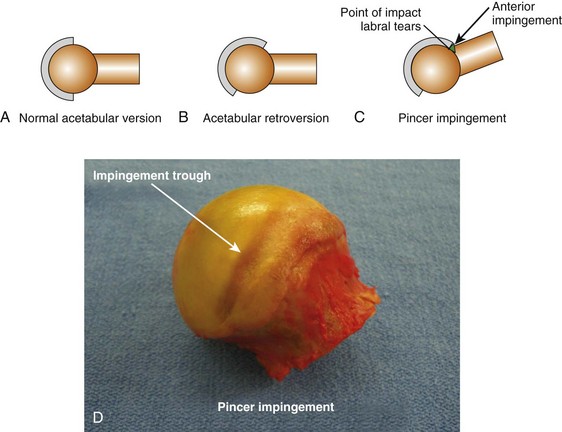
1. Pincer impingement (Figure 5-5)
 Anatomic aberration between socket and femoral neck that creates a mechanical block preventing further hip flexion
Anatomic aberration between socket and femoral neck that creates a mechanical block preventing further hip flexion
 The soft tissues between the bony mechanical block are pinched.
The soft tissues between the bony mechanical block are pinched.
 Typically the soft tissues damaged in pincer impingement are the acetabular labral complex.
Typically the soft tissues damaged in pincer impingement are the acetabular labral complex.
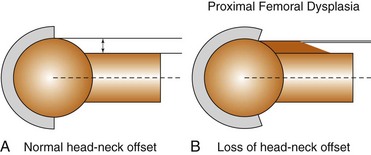
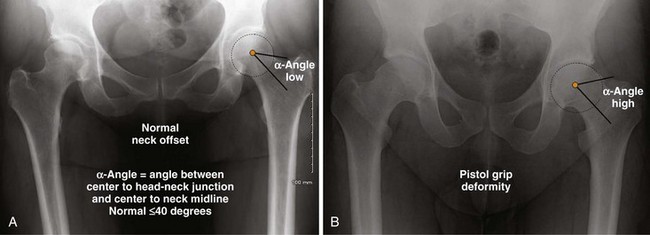
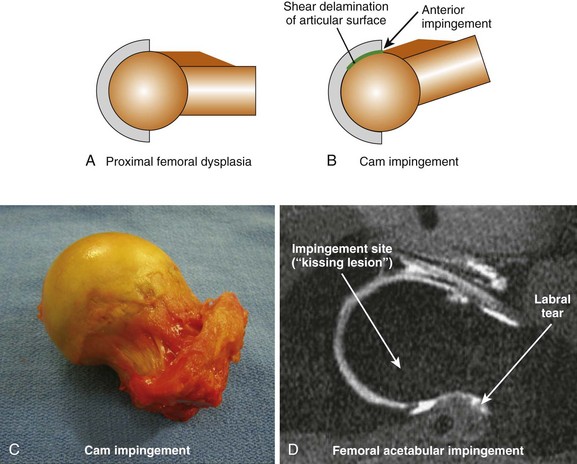
2. Cam impingement (Figure 5-6)
 Anatomic aberration in the proximal femoral neck creates a raised area (cam). The neck cam impinges upon the articular surface of the acetabulum in hip flexion.
Anatomic aberration in the proximal femoral neck creates a raised area (cam). The neck cam impinges upon the articular surface of the acetabulum in hip flexion.
 Compared to pincer impingement, the femoral neck is allowed to travel underneath the labrum a short distance, thus impinging more upon the articular surface.
Compared to pincer impingement, the femoral neck is allowed to travel underneath the labrum a short distance, thus impinging more upon the articular surface.
 Typically, the area of soft tissue damage in cam impingement is the chondral surface of the acetabulum.
Typically, the area of soft tissue damage in cam impingement is the chondral surface of the acetabulum.
A Treatment depends upon the extent of deformity and location.
B Surgical correction goals are to relieve pain and to correct anatomic deformity. Long-term goal is to reduce the occurrence of degenerative joint disease.
C Surgical correction addresses the main anatomic deformity: shallow socket, retroverted socket, reduced femoral neck offset (i.e., fat neck), abnormal femoral neck version.
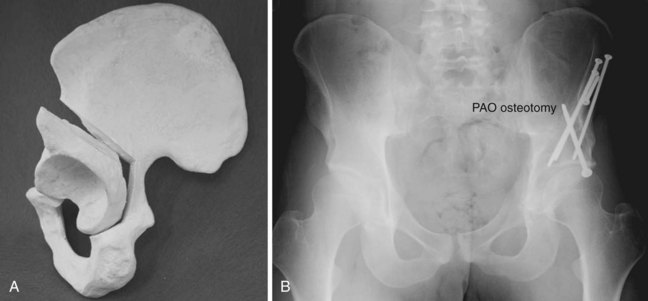
E Periacetabular osteotomy (Figure 5-7)
1. Allows large degree of socket correction
2. Permits joint medialization (i.e., center of hip rotation is positioned medial)
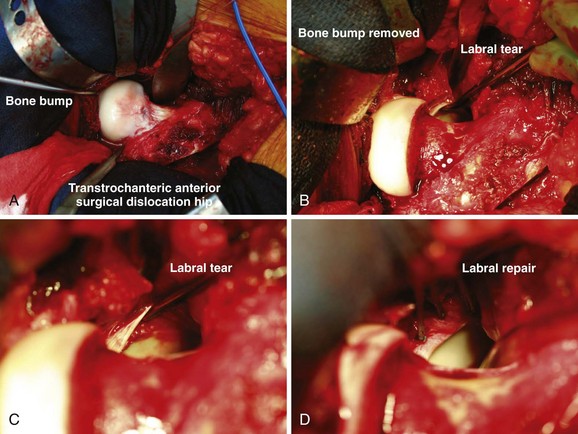
F Anterior hip decompression (Figure 5-8)
1. Technique is not used for shallow-socket dysplasia.
section 2 Hip Arthritis Assessment
I PHYSICAL EXAMINATION TESTS FOR HIP IRRITABILITY
2. Hip adduction and internal rotation yield pain response.
3. Hip internal rotation only yields pain response.
4. Pain located in area of anterior hip with pain radiating to either posterior hip or lateral hip
1. Patient is positioned supine. Finger rolling of leg (at calf level) into internal rotation and external rotation
1. Patient is positioned supine. Active straight leg raise of approximately 20 cm against mild resistance by examiner
2. Patient will feel pain in anterior hip against resistance.
1. Patient is positioned supine. Leg is positioned in figure-four position.
2. Pain will be elicited in area of anterior hip region or posterior hip region.
3. Be careful with interpretation of test. If pain is located over posterior pelvis, this indicates referred pain from L5-S1 facets or sacroiliac joint and not hip joint.
section 3 Hip Arthritis Treatment
 Traumatic labral tear not associated with dysplasia
Traumatic labral tear not associated with dysplasia
 Hip joint shows mechanical signs of locking, catching, and clicking.
Hip joint shows mechanical signs of locking, catching, and clicking.
2. Beware of labral resection in dysplasia.
 Acetabular labrum provides stability in a shallow acetabular socket (labrum usually is hypertrophic).
Acetabular labrum provides stability in a shallow acetabular socket (labrum usually is hypertrophic).
 Isolated removal of labrum will typically result in rapid progression of joint degeneration and pain.
Isolated removal of labrum will typically result in rapid progression of joint degeneration and pain.
 In cases of significant dysplasia, arthroscopic débridement is not recommended.
In cases of significant dysplasia, arthroscopic débridement is not recommended.
1. Less frequently used as THA technology advances
 Abnormal gait causes arthritis in these adjacent joints in 60% of patients.
Abnormal gait causes arthritis in these adjacent joints in 60% of patients.
 Symptoms of pain typically start within 25 years of hip fusion.
Symptoms of pain typically start within 25 years of hip fusion.
1. Usually last step before hip disarticulation in a frustrating downward clinical course
 Patients are most often immune compromised.
Patients are most often immune compromised.
 Recurrent periprosthetic THA infection
Recurrent periprosthetic THA infection
 Noncompliant patient with recurrent THA dislocation
Noncompliant patient with recurrent THA dislocation
 Intractable pain from arthritis
Intractable pain from arthritis
 Hip fracture with open decubitus ulcers
Hip fracture with open decubitus ulcers
 Significant contracture interfering with hygiene and posture
Significant contracture interfering with hygiene and posture
 Failed hip fusion in patient with prior major trauma to hip and/or pelvis
Failed hip fusion in patient with prior major trauma to hip and/or pelvis
1. Relegated to specific limited role
 Fracture treatment in low-demand elderly patient
Fracture treatment in low-demand elderly patient
 Best indication—displaced subcapital hip fracture with little or no prior history of symptomatic hip arthritis
Best indication—displaced subcapital hip fracture with little or no prior history of symptomatic hip arthritis
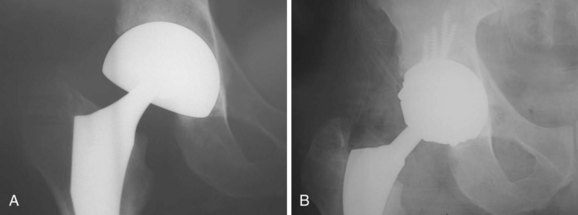
section 4 Osteonecrosis of the Hip
II ETIOLOGY (see Chapter 1, Basic Science)
A Hypercoagulable states may explain many idiopathic cases of osteonecrosis of the hip.
B In all cases, end-stage result is vascular occlusion in the juxtaarticular sinusoids adjacent to joint.
A Initial pain with sit to stand, stairs, inclines, and impact loading
B Pain location tends to be most noticeable in anterior hip.
C Can be acute in onset (acute infarct phenomenon), which can mimic an acute injury
A Start first with radiographs.
B MRI is the standard imaging modality when radiographs are negative and osteonecrosis is suspected.
Table 5-1![]()
Modified Ficat Staging System for Osteonecrosis of the Hip
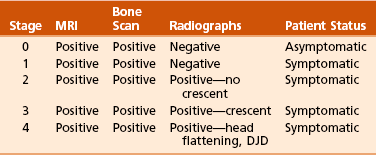
DJD, degenerative joint disease; MRI, magnetic resonance imaging.
1. Surgical treatment depends on these major variables.
 Head collapse (i.e., crescent)
Head collapse (i.e., crescent)
 Extent of head involvement (by osteonecrosis)
Extent of head involvement (by osteonecrosis)
 Described as volume head involvement
Described as volume head involvement
 Volume head involvement equals percent head involved on anteroposterior image multiplied by percent head involved on lateral image (e.g., 50% × 50% = 25% volume head involvement).
Volume head involvement equals percent head involved on anteroposterior image multiplied by percent head involved on lateral image (e.g., 50% × 50% = 25% volume head involvement).
 A—small lesion: less than 15% head involvement
A—small lesion: less than 15% head involvement
2. Younger age and crescent (or worse)
3. Younger age and no crescent
section 5 Total Hip Arthroplasty
A Debilitating pain affecting activities of daily living
1. Microinterlock with endosteal bone
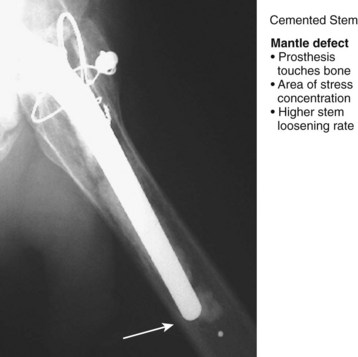
2. Cement will fatigue with cyclic loading.
 Fatigue starts at stress points within the cement mantle.
Fatigue starts at stress points within the cement mantle.
 A mantle defect is an area where the prosthesis touches bone. This is an area of significant stress concentration (Figure 5-11).
A mantle defect is an area where the prosthesis touches bone. This is an area of significant stress concentration (Figure 5-11).
3. Cemented cups fail at a higher rate than cemented stems.
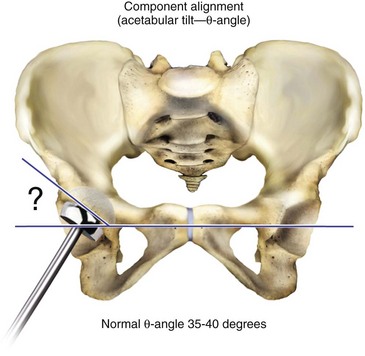
 Acetabular cup is positioned at an angle (i.e., theta (θ)-angle) relative to longitudinal axis of leg. This creates shear and tension forces at cement-bone interface.
Acetabular cup is positioned at an angle (i.e., theta (θ)-angle) relative to longitudinal axis of leg. This creates shear and tension forces at cement-bone interface.
 Cement is strongest in compression and weaker in tension.
Cement is strongest in compression and weaker in tension.
 Cemented stems fail at a lower rate than cups because stems see primarily a compression force.
Cemented stems fail at a lower rate than cups because stems see primarily a compression force.
1. Young, active patients have increased risk for failure.
2. Men are twice as likely to fail as women.
3. Young, active male is best candidate for cementless femoral stem.
1. Porosity reduction during mixing
 Decreased porosity reduces stress points in cement.
Decreased porosity reduces stress points in cement.
 Vacuum mixing is most common method to reduce cement porosity.
Vacuum mixing is most common method to reduce cement porosity.
2. Pressurization of cement before component insertion
3. Pulsatile lavage of bone before cementing
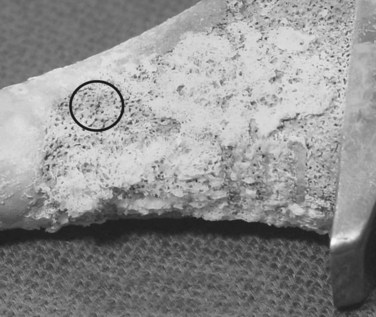
1. Bone ingrowth (Figure 5-12)
 Prosthesis is fabricated with metal pores into metallic alloy. Bone grows into the porous structure, stabilizing the prosthesis to bone.
Prosthesis is fabricated with metal pores into metallic alloy. Bone grows into the porous structure, stabilizing the prosthesis to bone.
 Successful bone ingrowth is based upon following factors.
Successful bone ingrowth is based upon following factors.
 Pore depth (i.e., deeper distance into metal) is directly related to increased fixation strength.
Pore depth (i.e., deeper distance into metal) is directly related to increased fixation strength.
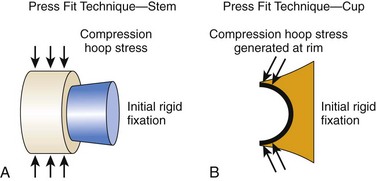
F Initial rigid fixation for cementless hip implants
1. Initial rigid implant fixation to host bone is required for long-term osteointegration. There are two techniques used. They are the press fit technique and the line-to-line technique.
2. Press fit technique (Figure 5-13)
 Bone is prepared such that a slightly oversized implant (relative to bone contour) is wedged into position.
Bone is prepared such that a slightly oversized implant (relative to bone contour) is wedged into position.
3. Complication of press fit technique
 Bone is prepared such that contour of bone is same size as implant.
Bone is prepared such that contour of bone is same size as implant.
 Femoral stem has an extensive porous coating. The extensive coating provides an initial frictional fit. The rough surface provides enough resistance to motion that the implant is stable once impacted into final position. The frictional fit is also known as scratch fit or interference fit.
Femoral stem has an extensive porous coating. The extensive coating provides an initial frictional fit. The rough surface provides enough resistance to motion that the implant is stable once impacted into final position. The frictional fit is also known as scratch fit or interference fit.
 Acetabular cup is placed into position. Cup is a hemispheric design. Cup is secured with multiple screws placed into bone.
Acetabular cup is placed into position. Cup is a hemispheric design. Cup is secured with multiple screws placed into bone.
1. Prosthetic surface is prepared by blasting surface with an abrasive grit material. Nickname is grit blast fixation.
2. Implant material for grit blast fixation is always titanium alloy.
3. Grit blasting process creates microdivots—no pores, just divots. Divot diameter approximately the same size as pore hole for a porous-coated implant
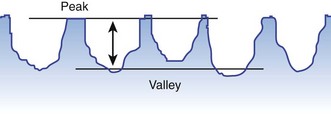
B Surface roughness (Ra) (Figure 5-14)
1. Ra is defined as average peak to valley on the surface of the implant.
2. Implant roughness determines strength of biologic fixation.
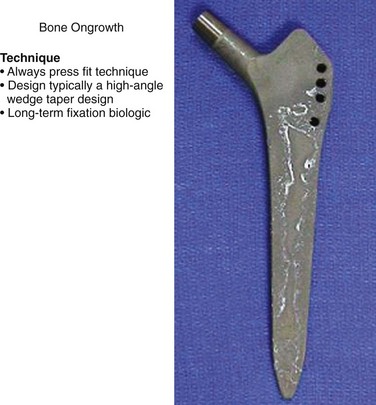
1. Initial rigid fixation of implant is always a press fit technique.
2. Femoral stem design is typically a high-angle double-wedge taper (wedge in both coronal and sagittal planes) (Figure 5-15).
3. Grit surface is extensile. The fixation strength with grit blast fixation is significantly lower than porous coating. Therefore the area of surface coating is greater.
4. There are very few cups designed with bone ongrowth surface coating.
A Formula is Ca10(PO4)6 (OH)2.
C Effect—allows more rapid closure of gaps between bone and prosthesis
V PRIMARY THA—FIXATION SELECTION
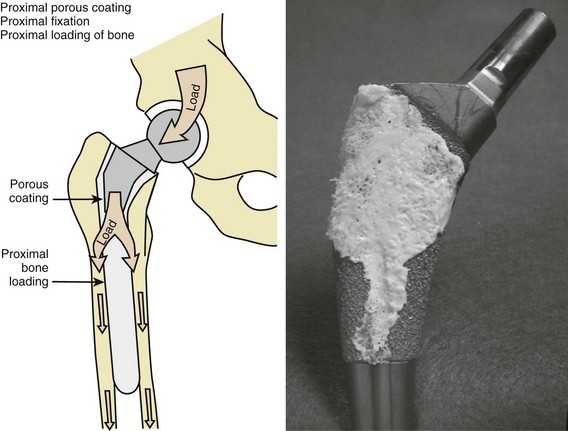
A Proximal porous coating (Figure 5-16)
1. Mechanical load is transferred to metaphysis and proximal diaphysis. This is termed proximal bone loading.
2. Proximal bone density is better maintained with proximal porous-coated implants.
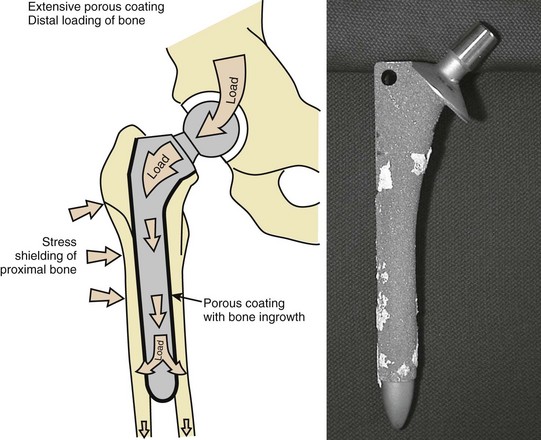
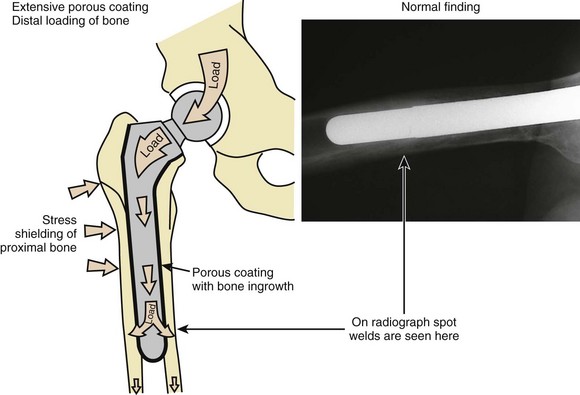
B Extensive porous coating (Figure 5-17)
1. More of the mechanical load bypasses the proximal femur because porous ingrowth is present throughout the diaphysis. This is termed distal bone loading.
2. In a well-fixed extensively porous-coated femoral stem there will be endosteal consolidation of bone near the end of the stem. This is called a spot weld (Figure 5-18).
1. Proximal femoral bone density loss observed over time in the presence of a solidly fixed implant; typically refers to cementless implants
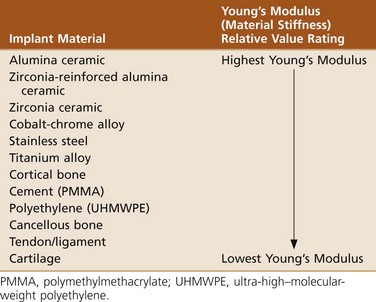
1. Stem stiffness is main factor.
 Problem is modulus mismatch between stem and femoral cortex.
Problem is modulus mismatch between stem and femoral cortex.
 Hoek’s law—When two springs are placed next to each other and loaded, more force is transmitted through the stiff spring and less through the flexible spring. Thus a cementless femoral stem that has a higher modulus than bone (i.e., stiff spring) sees much more loading stress than the surrounding proximal femur.
Hoek’s law—When two springs are placed next to each other and loaded, more force is transmitted through the stiff spring and less through the flexible spring. Thus a cementless femoral stem that has a higher modulus than bone (i.e., stiff spring) sees much more loading stress than the surrounding proximal femur.
section 6 Revision THA
A Start-up pain is the most common initial presentation.
B Infection must always be ruled out as a cause of pain.
C Anterior iliopsoas impingement and tendinitis is poorly understood and may be the cause of a painful THA when a prominent or malpositioned cup is present and no other causes can be found.
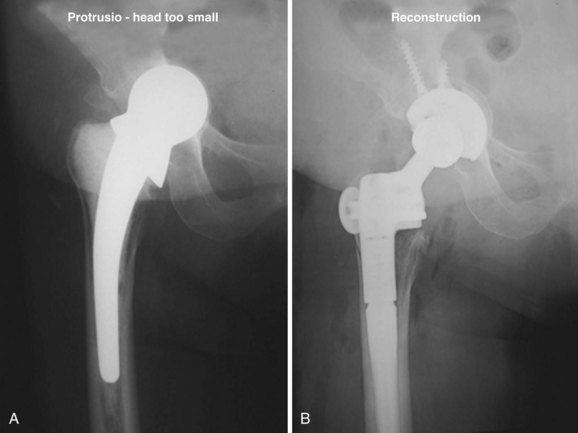
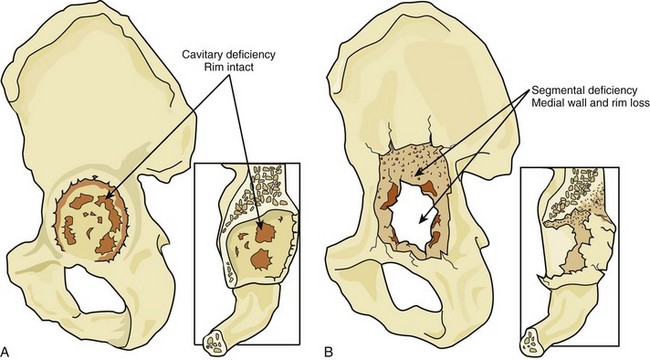
II ACETABULAR SIDE (Figure 5-20)
A Identify bone defects in acetabulum and pelvis.
1. Cavitary deficiency is a loss of cancellous bone without compromise of main structural bone support.
2. Segmental deficiency is loss of main bony support structures.
B Well-fixed cementless implant with osteolytic defect
1. Can be treated with débridement, bone grafting, and bearing component exchange
2. Contraindications to this are a poorly positioned cup, poor implant design, an ongrowth fixation surface, or damaged locking mechanism.
C Cementing a polyethylene (PE) liner into a damaged cup is associated with an increased rate of dislocation.
D Significance of bone defects
1. Major segmental bone deficiencies require a reconstruction cage and/or a structural bone graft. This is the recommended technique.
2. A structure bone graft (a graft that reconstructs a segmental defect) alone without a cage has a high loosening rate.
E Fixation revision of acetabulum
1. Cementless porous biologic fixation is preferred.
2. Hemispheric porous cup with screw is standard.
 Must have at least two thirds of rim and a reasonable initial press fit to work
Must have at least two thirds of rim and a reasonable initial press fit to work
 Recommended cup replacement is to recreate the native center of rotation.
Recommended cup replacement is to recreate the native center of rotation.
 Cup placement should be inferior and medial (i.e., low and in).
Cup placement should be inferior and medial (i.e., low and in).
 Cup placement superior and lateral (i.e., up and out) is not recommended.
Cup placement superior and lateral (i.e., up and out) is not recommended.
 Fill cavitary deficiencies with particulate bone graft.
Fill cavitary deficiencies with particulate bone graft.
 Acetabular metallic wedge augmentation is an acceptable adjuvent to hemispheric cup provided that cup is placed in good position and initial rigid fixation is achieved.
Acetabular metallic wedge augmentation is an acceptable adjuvent to hemispheric cup provided that cup is placed in good position and initial rigid fixation is achieved.
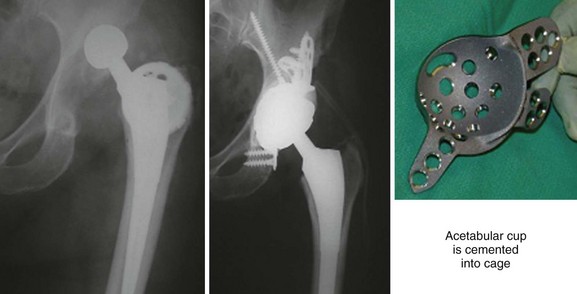
3. Reconstruction cage (Figure 5-21)
 Recommended when segmental bone deficiencies prevent initial rigid fixation of a hemispheric porous cup in desired position
Recommended when segmental bone deficiencies prevent initial rigid fixation of a hemispheric porous cup in desired position
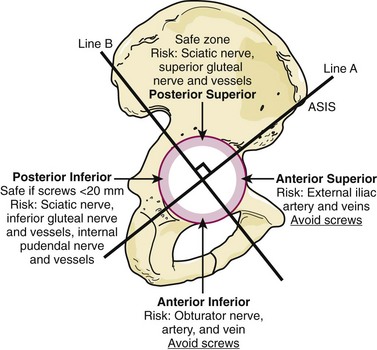
4. Acetabular screw placement (Figure 5-22)
 Posterior-superior quadrant is the safe zone for acetabular screw placement. This is preferred zone for screw placement.
Posterior-superior quadrant is the safe zone for acetabular screw placement. This is preferred zone for screw placement.
 Anterior-superior quadrant is considered the zone of death. Screws and/or drill that penetrate too far risk laceration to the external iliac artery and veins.
Anterior-superior quadrant is considered the zone of death. Screws and/or drill that penetrate too far risk laceration to the external iliac artery and veins.
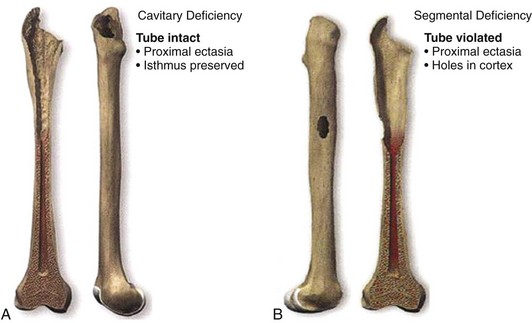
III FEMORAL SIDE (Figure 5-23)
A Identify bone defects in femur.
1. Cavitary deficiency is loss of endosteal bone. Cortical tube remains intact.
 Endosteal ectasia is a form of cavitary deficiency in which the outer cortex has increased in diameter as a result of mechanical irritation by a loose femoral stem.
Endosteal ectasia is a form of cavitary deficiency in which the outer cortex has increased in diameter as a result of mechanical irritation by a loose femoral stem.
2. Segmental bone deficiency is a loss of part of the cortical tube either in the form of holes or complete loss of a portion of the proximal femur.
B Significance of bone defects
1. Cementless porous biologic fixation is preferred.
2. Extensive porous-coated long-stem prosthesis is standard.
3. Longer stem than previous stem is recommended.
4. Impaction grafting technique
 Acceptable revision technique with limited indication
Acceptable revision technique with limited indication
 Place distal PE restrictor into diaphysis.
Place distal PE restrictor into diaphysis.
 Impact particulate allograft bone (fresh frozen bone recommended) into endosteal canal. Bone is impacted around a femoral stem trial.
Impact particulate allograft bone (fresh frozen bone recommended) into endosteal canal. Bone is impacted around a femoral stem trial.
 Cement polished tapered stem into impacted allograft bone.
Cement polished tapered stem into impacted allograft bone.
 Polished tapered stem is allowed to settle slightly within cement. Mechanical load forces are transmitted as compression forces upon allograft bone.
Polished tapered stem is allowed to settle slightly within cement. Mechanical load forces are transmitted as compression forces upon allograft bone.
 Allograft heals to endosteal bone.
Allograft heals to endosteal bone.
 Significant linear PE wear associated with progressive radiographic osteolysis and/or mechanical symptoms of subluxation
Significant linear PE wear associated with progressive radiographic osteolysis and/or mechanical symptoms of subluxation
 Must exchange both liner and head
Must exchange both liner and head
 Bone graft osteolytic lesions behind cup with particulate graft through cup holes or small iliac trap door
Bone graft osteolytic lesions behind cup with particulate graft through cup holes or small iliac trap door
section 7 Osteolysis in THA
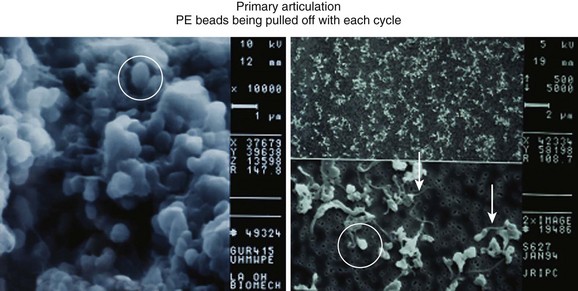
A PE wear debris is the main culprit (when using traditional PE cup bearing). PE wear comes from two sources.
1. PE bearing wear—head-cup articulation
2. Backside wear—This occurs when the PE insert rubs against the metal shell, creating PE debris. This occurs because the PE locking mechanism does not completely inhibit PE micromotion against the metal shell. The more backside micromotion allowed, the more PE debris generated
B Submicron-sized particles shed by the PE bearing are responsible for eliciting the osteolysis reaction.
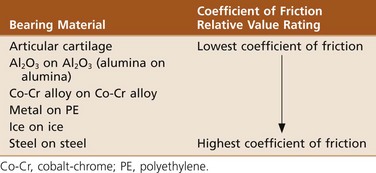
C Adhesive bearing wear is the most important process that generates submicron-sized PE particles.
 Adhesive wear (Figure 5-24)—This is most important mechanism in osteolysis process.
Adhesive wear (Figure 5-24)—This is most important mechanism in osteolysis process.
 Abrasive wear—A rough femoral head surface causes mechanical scratching of PE surface with loss of PE material (cheese grater effect).
Abrasive wear—A rough femoral head surface causes mechanical scratching of PE surface with loss of PE material (cheese grater effect).
 Third-body particles—Particles within the joint space get between head and PE cup, causing abrasion. These particles cause PE to be removed from cup surface. Third-body particle sources include
Third-body particles—Particles within the joint space get between head and PE cup, causing abrasion. These particles cause PE to be removed from cup surface. Third-body particle sources include
A Phagocytes of submicron-sized PE particles by macrophage; macrophage becomes activated
B Additional macrophage recruitment via cytokines released by activated macrophage
C Release of osteolytic factors (cytokines) by the activated macrophage; these factors include
1. Tumor necrosis factor-α—interleukin-1-β
2. Transforming growth factor-β—interleukin-6
3. Platelet-derived growth factor—receptor activator of nuclear factor κB ligand (RANKL)
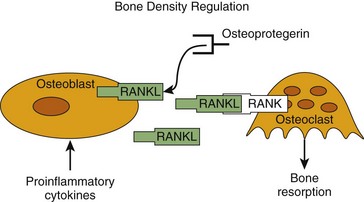
D Bone resorption mediated via RANKL
E Mechanism of bone resorption mediated by osteoblast/RANKL (Figure 5-25)
1. RANKL is produced by the osteoblast.
2. RANKL attaches to RANK receptor on osteoclast, which activates bone resorption process.
3. Osteoprotegerin, produced by many cell lines, blocks RANKL and mitigates bone resorption.
4. The only cell that resorbs bone is the osteoclast.
5. The RANKL/osteoprotegerin ratio in the bone microenvironment determines overall bone homeostasis.
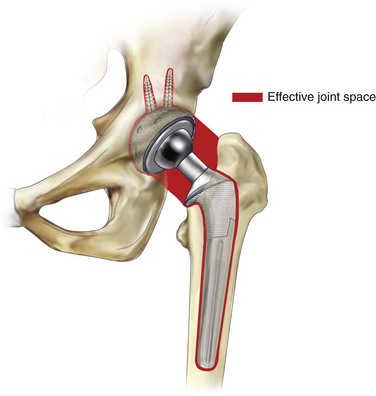
III OSTEOLYSIS AROUND THA PROSTHESIS—EFFECTIVE JOINT SPACE
A The intraarticular generation by PE particles elicits an inflammatory response that results in a hydrostatic pressure buildup within the joint.
B PE particles are then disseminated throughout the effective joint space (Figure 5-26).
1. Effective joint space is defined as any contiguous area around the joint where the implant touches bone. The effective joint space includes the area around the cup, stem, and screws.
C Osteolysis can occur anywhere within the effective joint space (Figure 5-27).
1. Fluid moves in the path of least resistance.
 Areas well sealed by biologic integration will inhibit particle dissemination.
Areas well sealed by biologic integration will inhibit particle dissemination.
 Areas that are vulnerable to particulate debris dissemination include
Areas that are vulnerable to particulate debris dissemination include
 With an extensively porous-coated stem, most osteolysis is seen at the greater trochanter and proximal femur. This can lead to late insufficiency fracture of the greater trochanter.
With an extensively porous-coated stem, most osteolysis is seen at the greater trochanter and proximal femur. This can lead to late insufficiency fracture of the greater trochanter.
 Proximal porous-coated femoral stems that do not have circumferential porous coating allow particles to be pumped toward distal stem region.
Proximal porous-coated femoral stems that do not have circumferential porous coating allow particles to be pumped toward distal stem region.
IV PARTICLE DEBRIS FORMATION—LINEAR VERSUS VOLUMETRIC WEAR
A Volumetric wear is main determinant of the number of PE particles generated.
B Volumetric wear is directly related to the square of the radius of the head (Figure 5-28).
1. The wear track generated approximates a cylinder. The volume of a cylinder, and hence the amount of PE debris generated, is formulated as follows:
where V is the volumetric wear of the PE cup, r is the radius of the femoral head, and w is the linear head wear (i.e., the distance the head has penetrated into the cup).
2. Head size is most important factor in predicting the amount of PE particles generated.
3. Linear wear rates in excess of 0.1 mm/yr are associated with osteolysis.
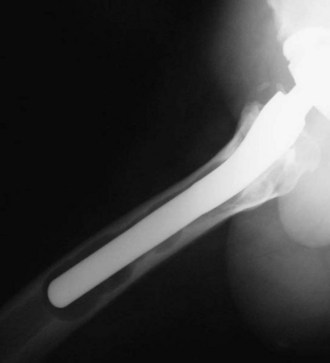
V OSTEOLYSIS—RADIOGRAPHIC FINDINGS IN THA
A Endosteal scalloping in femoral endosteal canal is hallmark finding (Figure 5-29).
B Round lytic lesions behind acetabular cup with screw holes is common finding.
C Round lytic lesion surrounding acetabular screw is also a typical finding.
D Osteolytic lesions develop later in prosthetic life cycle (usually starting after 10 years). Osteolytic lesions spotted within the first 2 to 3 years of the prosthetic life cycle are most likely a result of infection.
section 8 Periprosthetic THA Fracture
A Most late fractures occur at stem tip.
 Nonoperative if minimal displacement
Nonoperative if minimal displacement
 ORIF with cable/wiring if significant displacement and minimal osteolysis
ORIF with cable/wiring if significant displacement and minimal osteolysis
3. Proximal metaphysis or diaphysis
 For stem tip fracture that involves less than 25% of stem (cement and cementless stems) treatment options allowed are
For stem tip fracture that involves less than 25% of stem (cement and cementless stems) treatment options allowed are
 ORIF with cortical allograft struts and cables/wires
ORIF with cortical allograft struts and cables/wires
 Choice for fixation depends upon construct that can provide stability for healing yet not compromise stem fixation.
Choice for fixation depends upon construct that can provide stability for healing yet not compromise stem fixation.
 For stem tip fracture that involves more than 25% of cemented stem (cement mantle is compromised), there is only one recommended treatment.
For stem tip fracture that involves more than 25% of cemented stem (cement mantle is compromised), there is only one recommended treatment.
 For stem tip fracture that involves more than 25% of cementless stem (stem fixation biologically remains intact) treatment options allowed are
For stem tip fracture that involves more than 25% of cementless stem (stem fixation biologically remains intact) treatment options allowed are
5. Supracondylar fracture distant to stem tip
 Stem is not a major factor in fixation planning.
Stem is not a major factor in fixation planning.
 ORIF with lateral reconstruction plate is preferred treatment.
ORIF with lateral reconstruction plate is preferred treatment.
6. Supracondylar fracture at tip of long-stem revision prosthesis
section 10 THA—Miscellaneous
A Eighty percent of injuries are to sciatic nerve; 20% involve femoral nerve.
B Compression is most common pathologic mechanism of injury.
1. In patients who have a nerve injury after primary THA, only 35% to 40% will recover to normal strength.
C Sciatic nerve travels closest to acetabulum at the level of ischium.
1. During surgery, the most common reason for sciatic nerve injury is errant retractor placement causing excess compression to nerve.
2. Peroneal nerve division is most often involved because this part of nerve is closest to acetabulum.
D Risk factors for nerve injury
E Developmental dysplasia of the hip
III THA—SPECIFIC COMPLICATIONS
1. Associated with higher risk for heterotopic ossification
2. Hip hyperextension due to fixed pelvic deformity can lead to a higher anterior dislocation rate.
2. Rehabilitation—Limit external rotation and extension.
3. This approach is more commonly associated with gluteus medius lurch.
4. Abductor dysfunction caused by excessive proximal splitting of gluteus medius muscle and damage to superior gluteal nerve
section 11 THA—Joint Stability
I INCIDENCE OF THA DISLOCATION
II RISK FACTORS FOR DISLOCATION
III DISLOCATING THA—ASSESSMENT
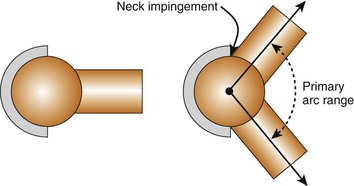
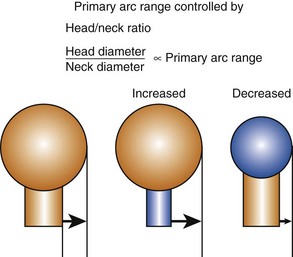
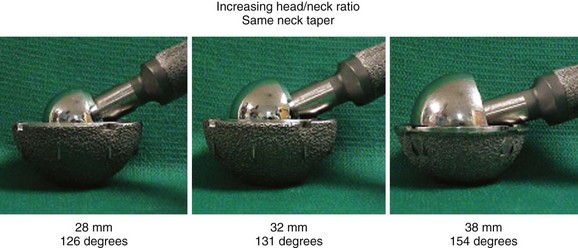
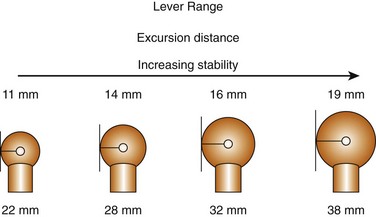
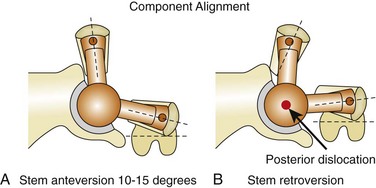
A Primary arc range is controlled by the head/neck ratio (Figure 5-32).
1. Head diameter/neck diameter is head/neck ratio.
2. Best stability is achieved by maximizing head/neck ratio (Figure 5-33).
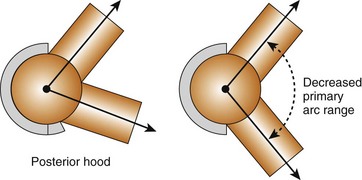
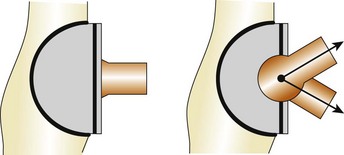
B Additions to acetabulum and/or femoral neck decrease primary arc range.
VII COMPONENT DESIGN—BEST RANGE IN THA
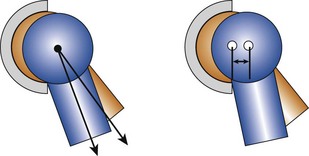
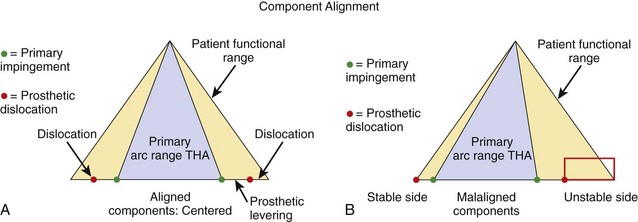
A Primary arc range must be centered within patient’s functional hip range (Figure 5-37).
B Component malalignment does not decrease primary arc range.
C Placement of components in a malaligned position results in a stable side and unstable side of the functional hip range.
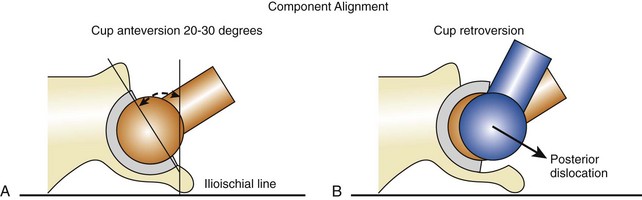
1. Cup anteversion—20 to 30 degrees (Figure 5-38)
2. Cup theta (θ)-angle (also known as coronal tilt)—35 to 40 degrees (Figure 5-39)
A Abductor complex is key to hip stability.
1. Consists primarily of gluteus medius muscle and gluteus minimus muscle
2. Prosthetic implant design and positioning must maintain/restore proper abductor hip tension.
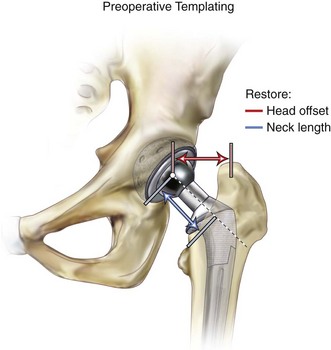
B Restoration of abductor tension achieved by the following (Figure 5-41):
2. Increased joint reaction force (decreased abductor lever arm)
3. Positive Trendelenburg sign
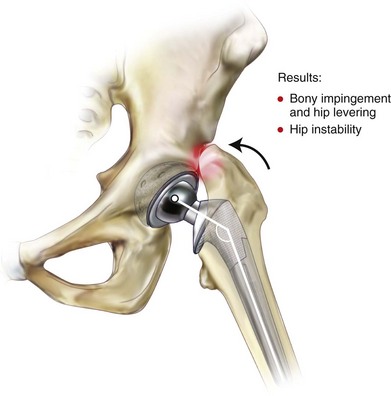
1. Short neck length occurs by making a low neck cut or using a short prosthetic neck length (or both).
2. Shortens abductor muscle length, resulting in abductor weakness
3. Decreases hip offset, which also weakens abductor complex
4. Results in bony impingement of greater trochanter against pelvis during hip range (Figure 5-42)
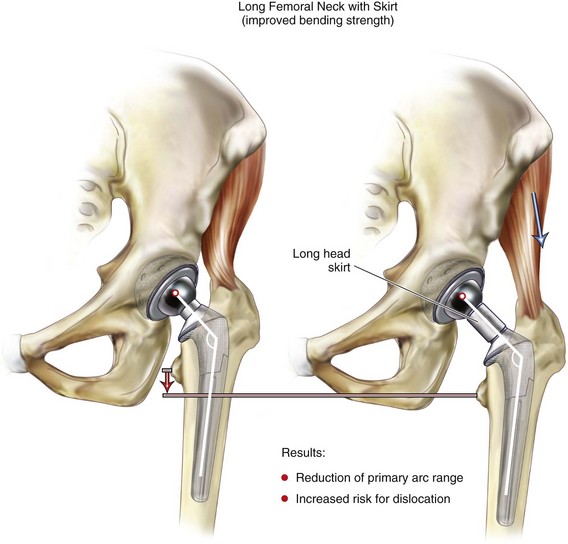
E Restored neck length using long head—problems
1. A short femoral neck cut can be compensated with an extralong prosthetic neck length. However, a long neck length requires a skirt (Figure 5-43).
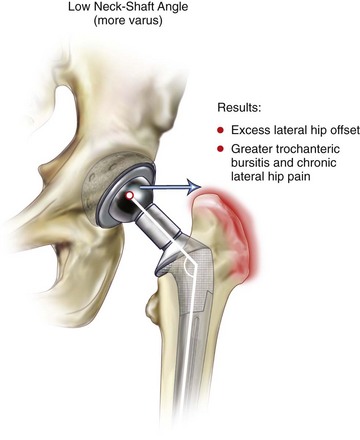
F Narrow-offset femoral stem design
1. A femoral stem with an offset designed with more narrow angle than the native hip will reduce hip offset. This reduces abductor tension and increases risk for hip dislocation.
2. A narrow-offset stem can be compensated by employing a longer femoral head length (i.e., neck length). This creates two potential problems.
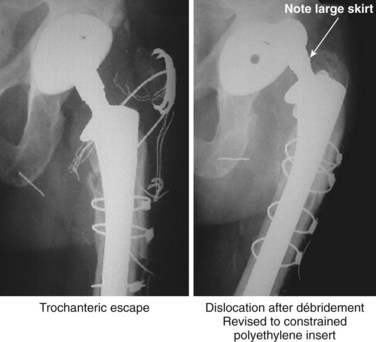
G Greater trochanteric escape (Figure 5-45)
1. Greater trochanteric escape occurs when the greater trochanter pulls away from the proximal femur.
 Usually a result of failed trochanter fixation after revision THA
Usually a result of failed trochanter fixation after revision THA
 Because the hip abductor complex attaches to the greater trochanter, trochanteric escape results in a loss of hip compression and increases risk for hip dislocation.
Because the hip abductor complex attaches to the greater trochanter, trochanteric escape results in a loss of hip compression and increases risk for hip dislocation.
 There is increased external and internal hip rotation because the greater trochanter no longer restricts rotation range. This also increases the risk for dislocation because the hip can more easily approach and exceed lever range.
There is increased external and internal hip rotation because the greater trochanter no longer restricts rotation range. This also increases the risk for dislocation because the hip can more easily approach and exceed lever range.
 The greater trochanter fragment can impinge between the hip and pelvis, causing hip levering.
The greater trochanter fragment can impinge between the hip and pelvis, causing hip levering.
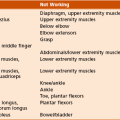
A The soft tissues about the hip are controlled by several body systems. All are integrated together to provide hip stability. The three main factors controlling soft tissue function include
B CNS mechanisms causing disruption to hip function and increasing risk for dislocation
C CNS conditions affecting hip function
D Peripheral nervous system mechanisms causing disruption to hip function, increasing risk for dislocation
E Peripheral nervous system conditions affecting hip
F Local soft tissue integrity mechanisms causing disruption to hip function and increasing risk for dislocation
G Local soft tissue conditions affecting hip function
A Each case of hip dislocation is unique. There is not one common treatment.
C Clinical review of dislocating event important
1. Was dislocation at extreme end range or within usual activities of daily living?
E Initial treatment for dislocated THA
1. Two thirds of patients with a first-time THA dislocation can be successfully treated with closed measures.
 Sedation or anesthesia preferred to minimize soft tissue trauma
Sedation or anesthesia preferred to minimize soft tissue trauma
 During closed reduction, take hip through full range and assess position of dislocation.
During closed reduction, take hip through full range and assess position of dislocation.
 Maximize head/neck ratio to increase primary arc range.
Maximize head/neck ratio to increase primary arc range.
 Recreate center of hip rotation and head offset.
Recreate center of hip rotation and head offset.
 Stabilize greater trochanter (if possible) if it is detached.
Stabilize greater trochanter (if possible) if it is detached.
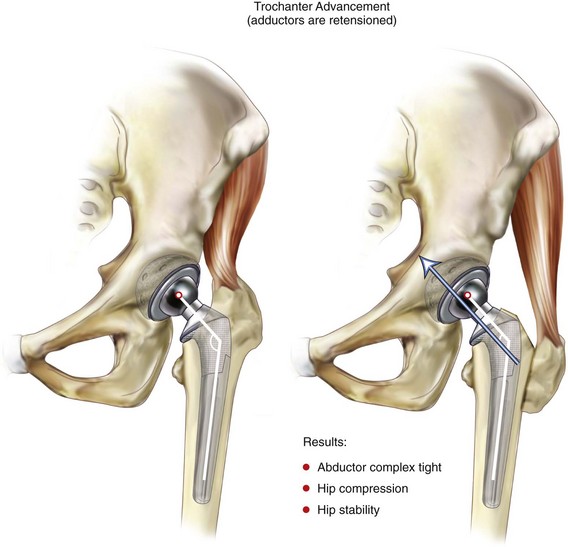
4. Greater trochanter advancement (also known as Charnley tensioning) (Figure 5-46)
 Technique is to perform trochanteric osteotomy, advance greater trochanter distally on lateral femur, and resecure with claw, cables, and/or wires.
Technique is to perform trochanteric osteotomy, advance greater trochanter distally on lateral femur, and resecure with claw, cables, and/or wires.
 By advancing greater trochanter distally, the abductor complex is tensioned tighter, which increases hip compression forces.
By advancing greater trochanter distally, the abductor complex is tensioned tighter, which increases hip compression forces.
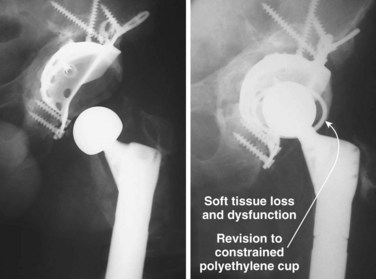
 A constrained PE socket encloses the femoral head and mechanically prevents hip from distracting out of socket.
A constrained PE socket encloses the femoral head and mechanically prevents hip from distracting out of socket.
 Reserved for the multiple dislocator with soft tissue dysfunction
Reserved for the multiple dislocator with soft tissue dysfunction
6. Bipolar hemiarthroplasty conversion
 Technique—Remove acetabular component. Ream remaining bone to a hemisphere. Press fit bipolar ball to rim of acetabulum (minimizes risk for medial migration of head).
Technique—Remove acetabular component. Ream remaining bone to a hemisphere. Press fit bipolar ball to rim of acetabulum (minimizes risk for medial migration of head).
 Maximize fully head/neck ratio.
Maximize fully head/neck ratio.
 Bipolar construct has a little more inherent stability than monopolar ball.
Bipolar construct has a little more inherent stability than monopolar ball.