Chapter 158 Adjacent-Level Degeneration and Disease of the Cervical and Lumbar Spine
Spondylosis is a natural and evolving process that occurs with aging, and it reflects the degeneration of intervertebral discs. Approximately 60% of asymptomatic persons older than 40 years of age have radiographic evidence of cervical spondylosis. By 60 years of age, 95% of men and 70% of women show similar radiographic findings.1–3 In a separate study, Boden et al.4 demonstrated that in patients younger than 60 years of age, the prevalence of abnormal results on lumbar MRIs averaged about 20%, whereas the prevalence was 57% in asymptomatic subjects older than 60 years of age.
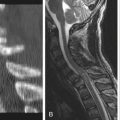
Cervical Spine
Biomechanical Evidence
Nearly 50 years ago, cervical spine fusion was introduced by Cloward, Bailey, and Badgley, and Robinson and Smith.5 Today, anterior cervical discectomy and fusion (ACDF) is a common surgical treatment for symptomatic cervical spondylosis. It is widely accepted, but it has been postulated that levels adjacent to a fused cervical segment(s) are prone to accelerated degenerative changes possibly owing to the significant forces transmitted to the adjacent levels after interbody fusion.
Certain biomechanical studies have generated data that lend credibility to the notion that fusion could cause degeneration of adjacent levels. Eck et al.6 evaluated motion and intradiscal pressures at adjacent levels in a cadaveric C5-6 ventral fusion model. Compared with intact specimens, flexion at C4-5 and C6-7 both increased, with greater increases in motion at the rostral level. Extension also increased at both levels adjacent to the fused level; however, motion was greater at the caudal level. Intradiscal pressures increased by 73% at C4-5 and by 45% at C6-7 compared with control specimens, indicating that fusion causes a transfer of load to adjacent levels. Park et al.7 reported similar findings in a cadaveric C5-7 ventral fusion model. The authors demonstrated that intradiscal pressures at C4-5 increased during physiologic range of motion. Cheng et al.8 compared fluoroscopic imaging in patients with normal, degenerative, and fused (C5-6) cervical spines. Range of motion and estimated in vivo forces at levels adjacent (C4-5 and C6-7) to a C5-6 ventral fusion were both higher compared with normal and degenerative cervical spines. In contrast to these studies, Rao et al.9 reported that intradiscal pressures and motion are not statistically different at adjacent levels after ventral fusion. Overall, most literature suggests that there is heightened loading and motion at levels adjacent to a fused segment(s).
Adjacent-Level Degeneration
Several authors have investigated adjacent-level degeneration radiographically. Baba et al.10 retrospectively reviewed 133 patients who underwent ventral cervical fusion with an average follow-up of 8.5 years. The authors reported a 25% incidence of spinal stenosis and increased motion at the adjacent rostral level on dynamic radiographs. In another retrospective evaluation with an average 5-year follow-up of 121 patients who underwent ventral cervical fusion, Gore and Sepic11 reported a 25% incidence of progression of spondylosis. In a radiographic review of 44 patients with a 4.5-year follow-up, Herkowitz et al.12 reported rates of 41% and 50% of adjacent-level degeneration in patients who underwent ACDF and posterior foraminotomy, respectively. This would suggest that ACDF did not directly cause the adjacent-level degeneration, because foraminotomy is a not a fusion procedure. There was no correlation found in any of these studies between adjacent-level degeneration and clinical deterioration.
Adjacent-Level Disease
Attempts to define the incidence of adjacent-level disease, or clinically apparent adjacent-level degeneration, have been made by several authors. In 1968, Williams et al.13 retrospectively studied 60 patients who underwent ACDF with an average follow-up of 4.5 years. Seventeen percent of these patients required additional surgery for progressive spondylosis after fusion. In a larger series with an average follow-up of 5 years, Gore and Sepic2 reported that 14% of patients required further surgery after ACDF. In 1993, Bohlman et al.14 reported a 9% incidence of the adjacent-level degeneration in 122 patients after ACDF, with an average clinical and radiographic follow-up of 6 years; 81% (9 of 11) of patients with adjacent-level degeneration required further surgery at the adjacent level. Hilibrand et al.15 performed a 10-year survivorship analysis of 409 ventral decompression and stabilization procedures. They reported a 2.9% annual incidence of adjacent-level disease, and an overall prevalence of 14% (follow-up, 2–21 years). Kaplan-Meier survivorship analysis predicted a prevalence of adjacent-level disease of 13.6% at 5 years and 25.6% at 10 years. The authors also concluded that the greatest risk of adjacent-level deterioration involved single-level fusions, particularly at C5-6 and C6-7. The authors could not determine from these results if degeneration was a result of the prior fusion or simply a manifestation of the natural progression of the spondylosis. These four studies indicate that there is 9% to 17% prevalence and an annual incidence of 1.5% to 4% of adjacent-level disease after ACDF.16
In addition, the control arms for the Investigational Device Exemptions trials for the various cervical artificial discs brought to market provide level I evidence and shed more light on the incidence of adjacent-level disease after one-level ACDF with allograft and plate. Mummaneni et al.17 and Murrey et al.18 reported a 3.2% and 1% incidence, respectively, of secondary surgeries for symptomatic adjacent-level degeneration at 2-year follow-up. Clearly, this refers to surgeries performed for adjacent-level disease and does not provide the absolute incidence. Presumably, there was a cohort of patients treated nonoperatively for adjacent-level symptoms.
Several authors have compared fusion and nonfusion procedures to further study adjacent-level disease. Lundsford et al.19 reviewed 334 patients who underwent anterior discectomy, with and without fusion. They reported an annual prevalence of adjacent-level disease of 7% and an annual incidence of 2.5%. There was no difference in the development of adjacent-level disease between fusion and nonfusion procedures. In a review of 846 patients who underwent posterior foraminotomy without fusion, Henderson et al.20 reported an overall prevalence of adjacent-level disease of 9% and an annual incidence of about 3%. Thus, these two reports provide evidence that suggests adjacent-level disease is not necessarily related to prior fusion procedures.
Prevention of Adjacent-Level Degeneration
As outlined previously, whether fusion causes adjacent-level degeneration remains a topic of debate. Regardless, there are steps the surgeon can attend to in order to minimize iatrogenic injury to adjacent levels. Needle level localization during ventral cervical surgery has been studied recently by Nassr et al.21 They retrospectively followed 87 patients who underwent one- or two-level ACDF, 15 of whom had incorrect needle placement during level localization. In these patients, there was a threefold increase in adjacent-level degeneration compared with patients who had correct needle localization. Given these compelling data, it is very reasonable instead to place the needle into a vertebral body to avoid a potential disc injury. Surgeons should also avoid excessive subperiosteal dissection above or below the surgical levels. Typically, only 3 to 4 mm of the adjacent body needs to be exposed for plate placement. This minimizes the risk of injuring the adjacent level or compromising the integrity of the anterior longitudinal ligament and longus colli muscles.
Ventral plate placement has also been implicated in adjacent-level degeneration. Park et al.22 retrospectively reviewed 118 patients with solid ventral plated fusion. The authors demonstrated a statistically significant higher incidence of adjacent-level ossification when the end of the cervical plate is less than 5 mm from the adjacent disc space. Sixty-seven percent of adjacent rostral levels and 45% of adjacent caudal levels developed ossification disease when the plate was less than 5 mm from the adjacent disc. To maintain an appropriate distance from the adjacent disc, the graft-vertebral body interface should be visible through the terminal screw holes of the plate when placing the screws. The rostral screws are placed in a superior trajectory and the caudal screws are placed in an inferior trajectory.
Lumbar Spine
Biomechanical Evidence
Similar to biomechanical studies in the cervical spine, lumbar data also support the notion that fusion results in higher biomechanical loads and more motion at adjacent, unfused levels. In an early cadaveric study, Lee and Langrana23 demonstrated an increase in motion at unfused, adjacent levels after various forms of instrumented fusion. The authors also reported that loading of the cephalic adjacent facet joints increased with dorsal instrumentation compared with an anterior interbody fusion. Weinhoffer et al.24 demonstrated in a cadaveric study that intradiscal pressures increased during flexion at the level adjacent to a pedicle screw construct. They also reported that the rise in pressure occurred earlier in flexion above two-level constructs versus one-level constructs. Other authors25,26 have demonstrated biochemical degeneration of the lumbar intervertebral disc adjacent to fused segments in animal models.
Adjacent-Level Degeneration
In 1987, Penta et al.27 reported a 32% incidence of adjacent-level degeneration after anterior lumbar interbody fusion, and also noted that its evolution was independent of fusion achievement (vs. pseudarthrosis) and of length of fusion. These authors reported a 2.5% incidence of adjacent-level stenosis, which is in stark contrast to the study by Lehmann et al. (30%).28 Leong et al.29 also evaluated adjacent-level degeneration after anterior lumbar interbody fusion, but reported an incidence of 52%. Many other studies have reported a wide range (20–64%) of adjacent-level degeneration after dorsal fusion.30–33
Instability and listhesis (anteroposterior translation) at adjacent levels have been reported by several authors. Lehmann et al.28 evaluated outcomes at long-term follow-up after dorsal lumbar fusion, and reported a 45% incidence of adjacent-level instability. Luk et al.34 retrospectively reviewed a series of patients 12.8 years after fusion for idiopathic scoliosis and reported asymptomatic hypermobility of the adjacent level. In 1997, Wimmer et al.35 reported a 10.8% incidence of asymptomatic adjacent-level listhesis after circumferential fusion. This was very similar to the 9.7% incidence of instability noted by Chen et al.36 after dorsal instrumented fusion, but less than the 30% to 35% rate of listhesis reported by Guigui et al.30 after dorsal instrumented fusion.
Radiographically apparent spinal stenosis as a consequence of adjacent-level degeneration has been reported less commonly. Like the reported rates of disc degeneration and listhesis/instability, the incidence range of stenosis is also quite wide, at 18% to 62%.28 Overall, our ability to understand the magnitude of adjacent-level degeneration is limited. Again, this is due to the wide variety of reporting methods and study designs that have been used over the last several decades. Nonetheless, even the most conservative estimates of adjacent-level degeneration report a 20% rate of occurrence.
Adjacent-Level Disease
The literature suggests that most patients who develop radiographically apparent adjacent-level degeneration after lumbar fusion do not have symptoms referable to it. Etebar and Cahill37 retrospectively reviewed 125 patients at 44-month follow-up after instrumented dorsal lumbar fusion for degenerative spondylolisthesis. They reported that 14% of patients required adjacent-level surgery. This is in contrast to another study38 that reported only a 3% incidence of symptomatic L5-S1 degeneration after L4-5 fusion at 7-year follow-up. Throckmorton et al.39 performed a retrospective review of 25 patients treated consecutively with a dorsal lumbar fusion ending adjacent to a degenerative disc (n = 20) or a normal one (n = 5). Surprisingly, at a minimum 2-year follow-up, patients with normal adjacent discs scored more poorly on the Short-Form Health Survey (SF-36), which suggests that radiographic degeneration alone is a poor indicator of future problems. In an important study, Ghiselli et al.40 retrospectively reviewed 215 patients after lumbar fusion and reported a 27.4% incidence of second surgery at adjacent levels (decompression n = 15; fusion n = 45). Kaplan-Meier analysis predicted that the rate of secondary surgery at adjacent levels for either decompression or fusion was 16% at 5 years and 36% at 10 years.
Prevention of Adjacent-Level Degeneration
Several risk factors for adjacent-level degeneration after lumbar fusion have been identified. The addition of instrumentation to fusion has consistently been associated with faster appearance and higher rates of adjacent degeneration. Two separate studies demonstrated adjacent-level listhesis at 25 months41 and 27 months37 after dorsal lumbar instrumented fusion. This is in significant contrast to the studies of noninstrumented fusion by Schlegel et al.42 and Lee43 that reported adjacent-level breakdown at 8 and 13 years after surgery, respectively. The association of instrumentation and adjacent-level deterioration is likely multifactorial. Clearly, the instrumented segments are initially more rigid, particularly when an interbody fusion is added to the construct. This may accelerate the initial loading of the adjacent level and henceforth its degeneration. As mentioned in a previous section, the fusion itself is associated with increased loading of both the disc and the facet joints and, as such, it is possible that fusion really is a cause of accelerated degeneration at adjacent levels.
Eck J.C., Humphreys S.C., Lim T.H., et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976). 2002;27:2431-2434.
Lee C.K. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine (Phila Pa 1976). 1988;13:375-377.
Lee C.K., Langrana N.A. Lumbosacral spinal fusion: a biomechanical study. Spine (Phila Pa 1976). 1984;9:574-581.
Lehmann T.R., Spratt K.F., Tozzi J.E., et al. Long-term follow-up of lower lumbar fusion patients. Spine (Phila Pa 1976). 1987;12:97-104.
Rao R.D., Wang M., McGrady L.M., et al. Does anterior plating of the cervical spine predispose to adjacent segment changes? Spine (Phila Pa 1976). 2005;30:2788-2792. discussion 2793
1. Boden S.D., McCowin P.R., Davis D.O., et al. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg [Am]. 1990;72:1178-1184.
2. Gore D.R., Sepic S.B. Anterior discectomy and fusion for painful cervical disc disease: a report of 50 patients with an average follow-up of 21 years. Spine (Phila Pa 1976). 1998;23:2047-2051.
3. Lehto I.J., Tertti M.O., Komu M.E., et al. Age related MRI changes at 0.1 T in cervical discs in asymptomatic subjects. Neuroradiology. 1994;36:49-53.
4. Boden S.D., Davis D.O., Dina T.S. Abnormal magnetic resonance scans of the lumbar spine in asymptomatic subjects. J Bone Joint Surg [Am]. 1990;72:403-408.
5. Yoon S.T., Howard S.A. Cervical degenerative disc disease. In: Vaccaro A.P., Betz R.R., Zeidman S.M., editors. Principles and practice of spine surgery. Philadelphia: Mosby; 2003:319-332.
6. Eck J.C., Humphreys S.C., Lim T.H., et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976). 2002;27:2431-2434.
7. Park D.H., Ramakrishnan P., Cho T.H., et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine. 2007;7:336-340.
8. Cheng J.S., Liu F., Komistek R.D., et al. Comparison of cervical spine kinematics using a fluoroscopic model for adjacent segment degeneration. J Neurosurg Spine. 2007;7:509-513.
9. Rao R.D., Wang M., McGrady L.M., et al. Does anterior plating of the cervical spine predispose to adjacent segment changes? Spine (Phila Pa 1976). 2005;30:2788-2792. discussion 2793
10. Baba H., Furusawa N., Imura S., et al. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine (Phila Pa 1976). 1993;15:2167-2173.
11. Gore D.R., Sepic S.B. Anterior cervical fusion for degenerated or protruded discs: a review of one hundred forty-six patients. Spine (Phila Pa 1976). 1984;9:667-671.
12. Herkowitz H.N., Kurz L.T., Overholt D.P. Surgical management of cervical soft disc herniation: a comparison between the anterior and posterior approach. Spine (Phila Pa 1976). 1990;15:1026-1030.
13. Williams J.L., Allen M.B.Jr., Harkess J.W. Late results of cervical discectomy and interbody fusion: some factors influencing the results. J Bone Joint Surg [Am]. 1968;50:277-286.
14. Bohlman H.H., Emery S.E., Goodfellow D.B., et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy: long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg [Am]. 1993;75:1298-1307.
15. Hilibrand A.S., Carlson G.D., Palumbo M.A., et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg [Am]. 1999;81:519-528.
16. Hilibrand A.S., Matthews R. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004;4(Suppl 6):S190-S194.
17. Mummaneni P.V., Burkus J.K., Haid R.W., et al. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. 2007;6:198-209.
18. Murrey D., Janssen M., Delamarter R., et al. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J. 2009;9:275-286.
19. Lundsford L.D., Bissonette D.J., Jannetta P.J., et al. Anterior surgery for cervical disc disease. Part I: Treatment of lateral cervical disc herniation in 253 cases. J Neurosurg. 1980;53:1-11.
20. Henderson C.M., Hennessy R.G., Shuey H.M., et al. Posterior-lateral foraminotomy as an exclusive operative technique for cervical radiculopathy: a review of 846 consecutively operated cases. Neurosurgery. 1983;13:504-512.
21. Nassr A., Lee J.Y., Bashir R.S., et al. Does incorrect level needle localization during anterior cervical discectomy and fusion lead to accelerated disc degeneration? Spine (Phila Pa 1976). 2009;34:189-192.
22. Park J.B., Cho Y., Riew K.D. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg [Am]. 2005;87:558-563.
23. Lee C.K., Langrana N.A. Lumbosacral spinal fusion: a biomechanical study. Spine (Phila Pa 1976). 1984;9:574-581.
24. Weinhoffer S.L., Guyer R.D., Herbert M., et al. Intradiscal pressure measurements above an instrumented fusion. Spine (Phila Pa 1976). 1995;20:526-531.
25. Phillips F.M., Reuben J., Wetzel F.T. Intervertebral disc degeneration adjacent to a lumbar fusion: an experimental rabbit model. J Bone Joint Surg [Br]. 2002;84:289-294.
26. Bushell G.R., Ghosh P., Taylor T.F., et al. The effect of spinal fusion on the collagen and proteoglycans of the canine intervertebral disc. J Surg Res. 1978;25:61-69.
27. Penta M., Sandhu A., Fraser R.D. Magnetic resonance imaging assessment of disc degeneration 10 years after anterior lumbar interbody fusion. Spine (Phila Pa 1976). 1995;20:743-747.
28. Lehmann T.R., Spratt K.F., Tozzi J.E., et al. Long-term follow-up of lower lumbar fusion patients. Spine (Phila Pa 1976). 1987;12:97-104.
29. Leong J.C., Chun S.Y., Grange W.J., et al. Long-term results of lumbar intervertebral disc prolapse. Spine (Phila Pa 1976). 1983;8:793-799.
30. Guigui P., Lambert P., Lassale B., et al. Long-term outcome at adjacent levels of lumbar arthrodesis [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1997;83:685-696.
31. Kumar M.N., Jacquot F., Hall H. Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J. 2001;10:309-313.
32. Nakai S., Yoshizawa H., Kobayashi S. Long-term follow-up study of posterior lumbar interbody fusion. J Spinal Disord. 1999;12:293-299.
33. Pihlajamaki H., Bostman O., Ruuskanen M., et al. Posterolateral lumbosacral fusion with transpedicular fixation: 63 consecutive cases followed for 4 (2–6) years. Acta Orthop Scand. 1996;67:63-68.
34. Luk K.D., Lee F.B., Leong J.C., et al. The effect on the lumbosacral spine of long spinal fusion for idiopathic scoliosis: a minimum 10-year follow-up. Spine (Phila Pa 1976). 1987;12:996-1000.
35. Wimmer C., Gluch H., Krismer M., et al. AP-translation in the proximal disc adjacent to lumbar spine fusion: a retrospective comparison of mono- and polysegmental fusion in 120 patients. Acta Orthop Scand. 1997;68:269-272.
36. Chen W.J., Niu C.C., Chen L.H., et al. Survivorship analysis of DKS instrumentation in the treatment of spondylolisthesis. Clin Orthop Relat Res. 1997;339:113-120.
37. Etebar S., Cahill D.W. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 1999;90(Suppl 2):163-169.
38. Ghiselli G., Wang J.C., Wellington K.H., et al. L5-S1 segment survivorship and clinical outcome analysis after L4-L5 isolated fusion. Spine (Phila Pa 1976). 2003;28:1275-1280.
39. Throckmorton T.W., Hilibrand A.S., Mencio G.A., et al. The impact of adjacent level disc degeneration on health status outcomes following lumbar fusion. Spine (Phila Pa 1976). 2003;28:2546-2550.
40. Ghiselli G., Wang J.C., Bhatia N.N., et al. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg [Am]. 2004;86:1497-1503.
41. Aota Y., Kumano K., Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 1995;8:464-473.
42. Schlegel J.D., Smith J.A., Schleusener R.L. Lumbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine (Phila Pa 1976). 1996;21:970-981.
43. Lee C.K. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine (Phila Pa 1976). 1988;13:375-377.