Acute generalized exanthematous pustulosis

Management strategy
Treatment of AGEP involves establishing the correct diagnosis (Table 8.1) coupled with the withdrawal of any implicated medication (Table 8.2). Pustular psoriasis is its main differential diagnosis. A comprehensive drug history and a personal or family history of psoriasis is therefore required.
Table 8.1
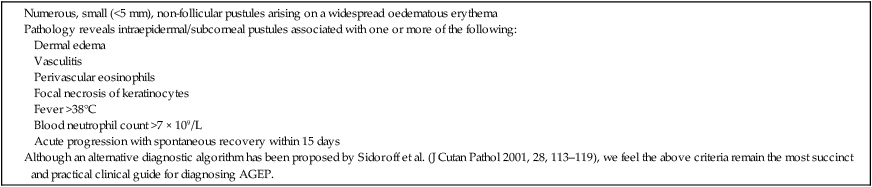
(From Roujeau, et al., 1991. Arch Dermatol 127, 1333–1338.)
Table 8.2
Drugs and other substances reported to have caused AGEP
| Drugs |
| Antibiotics |
|
Penicillins: amoxicillin, ampicillin, bacampicillin, pipemidic acid, piperacillin, propicillin, tazobactam Macrolides: azithromycin, erythromycin Quinolones: ciprofloxacin, norfloxacin, ofloxacin Tetracyclines: doxycycline, minocycline Cephalosporins: cefaclor, cefazolin, cefuroxime, cephalexin, cephradine Aminoglycosides: gentamicin, isepamicin sulfate, streptomycin Other antibiotics: chloramphenicol, clindamycin, co-trimoxazole, imipenem/cilastatin, lincomycin, metronidazole, nifuroxazide, sulfamethoxazole, teicoplanin, vancomycin, daptomycin, telavancin |
| NSAIDs |
| Celecoxib, etoricoxib, ibuprofen, naproxen, nimesulide, valdecoxib |
| ACE inhibitors |
| Captopril, enalapril |
| Calcium channel blockers |
| Nifedipine, nimodipine |
| Anticonvulsants |
| Carbamazepine, phenobarbital, phenytoin |
| Analgesia (opioid/non-opioid) |
| Acetaminophen, paracetamol, morphine, codeine, dextropropoxyphene |
| Anti-platelets |
| Aspirin, ticlopidine, clopidogrel |
| Benzodiazepines |
| Clobazam, nitrazepam, tetrazepam |
| Antimalarials |
| Chloroquine, hydroxychloroquine, proguanil, pyrimethamine |
| Antipsychotics |
| Clozapine, chlorpromazine |
| Antifungals |
| Amphotericin, fluconazole, itraconazole, nystatin, terbinafine |
| Antivirals |
| Lamivudine, lopinavir, ritonavir, zidovudine |
| Anti-TB drugs |
| Isoniazid, rifampicin |
| Proton pump inhibitors |
| Lansoprazole, omeprazole |
| Immunosuppressants |
| Azathioprine |
| Calcium channel blockers |
| Diltiazem |
| Antidepressants |
| Amoxapine, sertraline |
| Antihistamines |
| Clemastine, hydroxyzine |
| Beta agonists |
| Buphenine, fenoterol, nadolol |
| H2 receptor antagonists |
| Cimetidine, famotidine, ranitidine |
| Corticosteroids |
| Dexamethasone, methylprednisolone, prednisolone |
| Diuretics |
| Furosemide, hydrochlorothiazide |
| Anti-neoplastic drugs |
| Gefitinib, imatinib |
| Other drugs |
| Acetazolamide, allopurinol, bleomycin, carbimazole, cytarabine, disulfiram, eperisone hydrochloride, eprazinone, fluindione, icodextrin, interferon, metamizole, pentoxifylline, piperazine, bamifylline, propafenone, aprostadil, pseudoephidrine, psoralen + UVA, quinidine, salbutiamine, senna, simvastatin, sulfasalazine, terazosin, thalidomide, cadralazine, progestogens, dalteparin, carbutamide |
| Other substances |
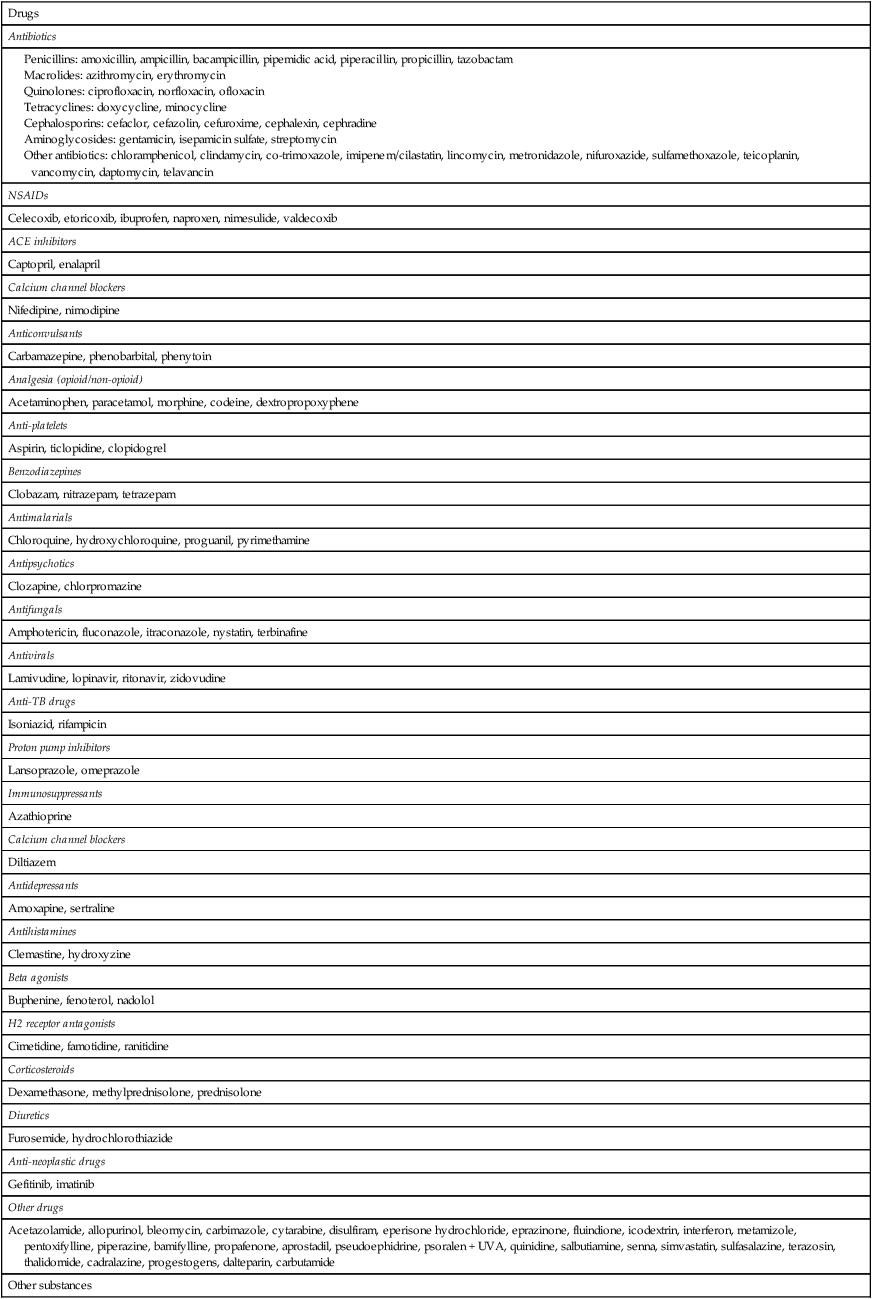

Antibiotics (primarily penicillin or macrolide based) are the most frequently implicated medications. Numerous case reports have cited various other causative agents, including calcium channel blockers, non-steroidal anti-inflammatory drugs (NSAIDs), angiotensin-converting enzyme (ACE) inhibitors and anticonvulsants (Table 8.2). Acute enterovirus infection, cytomegalovirus, parvovirus B19, spider bites, Chinese herbal compounds (ginkgo biloba), contrast media, and mercury exposure have also been reported as possible causes.






 Drug withdrawal
Drug withdrawal Corticosteroids
Corticosteroids