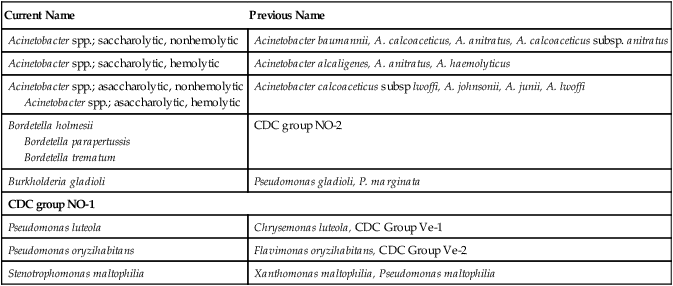
Acinetobacter, Stenotrophomonas, and Similar Organisms
1. List the most common gram-negative organisms discussed in this chapter that are encountered in clinical specimens.
2. Explain where Acinetobacter spp. are found and the patients most at risk of infection.
3. Describe the Gram stain morphology of Acinetobacter, Bordetella, and Stenotrophomonas spp.
4. Describe the appearance and odor of Stenotrophomonas maltophilia when grown on blood agar.
5. Differentiate between the two groups of Acinetobacter organisms and identify the most dependable test to distinguish between the groups.
General Characteristics
The organisms discussed in this chapter are considered together because, except for CDC group NO-1, they are all oxidase negative and grow on MacConkey agar, as do the Enterobacteriaceae. However, unlike the Enterobacteriaceae, which ferment glucose, these organisms either oxidize glucose (i.e., they are saccharolytic), or they do not utilize glucose (i.e., they are nonoxidizers, or asaccharolytic). Although CDC group NO-1 is oxidase negative and does not usually grow on MacConkey agar, it is included here because it must be distinguished from the asaccharolytic Acinetobacter spp. Based on molecular studies, approximately 21 species and/or strains of Acinetobacter spp. have been identified. The specific morphologic and physiologic features of the organisms are considered later in this chapter in the discussion of laboratory diagnosis. Of note, only Acinetobacter and Stenotrophomonas spp. are routinely found in clinical specimens. Bordetella parapertussis is included in Table 21-4 in this chapter but is discussed in Chapter 37.
Epidemiology
The organisms discussed in this chapter inhabit environmental niches. Acinetobacter spp. and Stenotrophomonas maltophilia are widely distributed in moist natural and hospital environments (Table 21-1). Acinetobacter spp. can be found on fomites and in soil, water, and animal food products. These organisms are capable of survival on inanimate objects for extended periods. Acinetobacter spp. is a human skin colonizer in 0.5% to 3% of the general population and has been identified from a number of human sources, including sputum, urine, feces, and vaginal secretions. S. maltophilia may be found in tap water and salads. Although none of these organisms are considered normal human flora, the relatively high prevalence of Acinetobacter spp. and S. maltophilia in hospitals frequently results in colonization of the skin and respiratory tract of patients. The prevalence of these organisms is evidenced by the fact that, excluding the Enterobacteriaceae, Acinetobacter spp. and S. maltophilia are the second and third most common gram-negative bacilli, respectively, encountered in clinical specimens. In contrast, Pseudomonas luteola, Pseudomonas oryzihabitans, and CDC group NO-1 are not commonly found in clinical specimens but have been isolated from wounds, blood cultures, and dialysis fluids.
TABLE 21-1
| Species | Habitat (Reservoir) | Mode of Transmission |
| Acinetobacter spp. | Widely distributed in nature, including the hospital environment. May become established as part of skin and respiratory flora of patients hospitalized for prolonged periods | Colonization of hospitalized patients from environmental factors; medical instrumentation (e.g., intravenous or urinary catheters) introduces organism to normally sterile sites |
| Stenotrophomonas maltophilia | Widely distributed in nature, including moist hospital environments. May become established as part of respiratory flora of patients hospitalized for prolonged periods | Colonization of hospitalized patients from environmental factors; medical instrumentation introduces organism to normally sterile sites (similar to transmission of Acinetobacter spp.) |
| CDC group NO-1 | Oropharynx of animals. Not part of human flora | Animal bite or scratch |
| Burkholderia gladioli | Environmental pathogen of plants; occasionally found in respiratory tract of patients with cystic fibrosis but not part of normal flora | Transmission to humans uncommon, mode of transmission not known |
| Pseudomonas luteola Pseudomonas oryzihabitans |
Environmental, including moist hospital environments (e.g., respiratory therapy equipment). Not part of normal human flora | Uncertain; probably involves exposure of debilitated hospital patients to contaminated fluids and medical equipment |
| Bordetella holmesii B. trematum |
Unknown or part of normal human flora | Unknown; rarely found in humans |
Pathogenesis and Spectrum of Disease
All of the organisms listed in Table 21-2 are opportunistic pathogens for which no definitive virulence factors are known. Because Acinetobacter spp. and S. maltophilia are relatively common colonizers of hospitalized patients, their clinical significance when found in patient specimens can be difficult to establish. In fact, these organisms are more frequently isolated as colonizers than as infecting agents. When infection does occur, it usually is seen in debilitated patients, such as those in burn or intensive care units and those who have undergone medical instrumentation and/or have received multiple antimicrobial agents. Acinetobacter baumannii is typically the species identified in hospital-acquired infections. Infections caused by Acinetobacter spp. and S. maltophilia usually involve the respiratory or genitourinary tract, bacteremia and, occasionally, wound infections, although infections involving several other body sites have been described. Community-acquired infections with these organisms can occur, but the vast majority of infections are nosocomial.
TABLE 21-2
Pathogenesis and Spectrum of Diseases
| Species | Virulence Factors | Spectrum of Disease and Infections |
| Acinetobacter spp. | Unknown | Clinical isolates are often colonizers. True infections are usually nosocomial, occur during warm seasons, and most commonly involve the genitourinary tract, respiratory tract, wounds, soft tissues, and bacteremia |
| Bordetella holmesii Bordetella trematum |
Unknown | Bacteremia is the only type of infection described. |
| Burkholderia gladioli | Unknown | Role in human disease is uncertain; occasionally found in sputa of patients with cystic fibrosis, but clinical significance in this setting is uncertain. |
| Pseudomonas luteola, P. oryzihabitans | Unknown | Catheter-related infections, septicemia, and peritonitis, usually associated with continuous ambulatory peritoneal dialysis, and miscellaneous mixed infections of other body sites. |
| Stenotrophomonas maltophilia | Unknown. Intrinsic resistance to almost every commonly used antibacterial agent supports the survival of this organism in the hospital environment. | Most infections are nosocomial and include catheter-related infections, bacteremia, wound infections, pneumonia, urinary tract infections, and miscellaneous infections of other body sites. |
| CDC group NO-1 | Unknown | Animal bite wound infections |
Laboratory Diagnosis
Specimen Collection and Transport
No special considerations are required for specimen collection and transport of the organisms discussed in this chapter. Refer to Table 5-1 for general information on specimen collection and transport.
Cultivation
Media of Choice
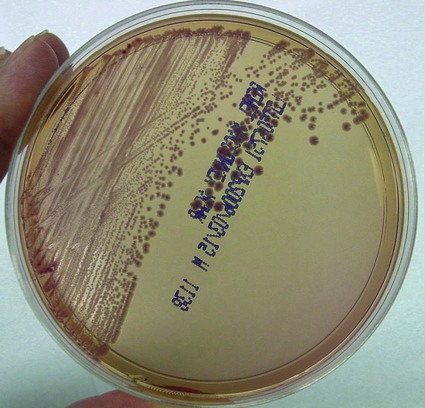
Colonial Appearance
Table 21-3 describes the colonial appearance and other distinguishing characteristics (e.g., hemolysis and odor) of each genus when grown on 5% sheep blood and MacConkey agars.
TABLE 21-3
Colonial Appearance and Characteristics
| Organism | Medium | Appearance |
| Stenotrophomonas maltophilia | BA | Large, smooth, glistening colonies with uneven edges and lavender-green to light purple pigment; greenish discoloration underneath growth; ammonia smell |
| Mac | NLF | |
| Acinetobacter spp. | BA | Smooth, opaque, raised, creamy, and smaller than Enterobacteriaceae; some genospecies are beta-hemolytic |
| Mac | NLF, but colonies exhibit a purplish hue that may cause the organism to be mistaken for LF (Figure 21-1) | |
| Burkholderia gladioli | BA | Yellow |
| Mac | NLF | |
| Bordetella parapertussis | BA | Smooth, opaque, beta-hemolytic |
| Mac | NLF, delayed growth | |
| Bordetella holmesii | BA | Punctate, semiopaque, convex, round, with greening of blood usually accompanied by lysis |
| Mac | NLF, delayed growth | |
| Bordetella trematum | BA | Convex, circular, grayish cream to white |
| Mac | NLF | |
| Pseudomonas oryzihabitans | BA | Wrinkled, rough or smooth, transparent, yellow |
| Mac | NLF | |
| Pseudomonas luteola | BA | Maybe rough and smooth, opaque, yellow |
| Mac | NLF | |
| CDC group NO-1 | BA | Small colonies that can be transferred intact with an inoculating needle |
| Mac | NLF, but only 20% of strains grow |
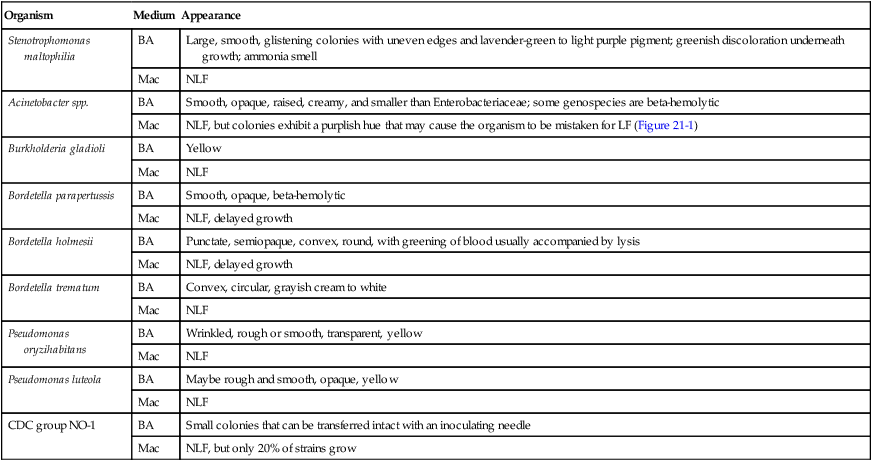
BA, 5% Sheep blood agar; LF, lactose fermenter; Mac, MacConkey agar; NLF, non–lactose fermenter.
Approach to Identification
Acinetobacter spp. and S. maltophilia are reliably identified by the API 20E system (bioMérieux, St. Louis, Missouri), although other commercial systems may not perform as well. Automated identification systems typically identify the organisms in this chapter to the genus level. Additional testing may be required to speciate the organisms using conventional biochemical and physiologic characteristics, such as those outlined in Table 21-4.
TABLE 21-4
Key Biochemical and Physiologic Characteristics
| Organism | Growth on MacConkey | Motile | Oxidizes Glucose | Oxidizes Maltose | Esculin Hydrolysis | Lysine Decarboxylase | Nitrate Reduction | Urea Christensen’s |
| Stenotrophomonas maltophilia | + | + | + | + | V | + | V | − |
| Saccharolytic Acinetobacter | + | − | + | − | − | − | − | V |
| Asaccharolytic Acinetobacter | + | − | − | V | − | − | − | V |
| Burkholderia gladioli* | + | + | + | − | − | − | V | V |
| Bordetella parapertussis | + | − | − | − | − | ND | − | + |
| Bordetella holmesii† | + or (+) | − | − | − | − | − | − | − |
| Bordetella trematum | + | + | − | − | − | − | V | − |
| Pseudomonas oryzihabitans | + | + p, 1-2 | + | + | − | − | − | V |
| Pseudomonas luteola | + | + p, >2 | + | + | + | − | V | V |
| CDC group NO-1 | V | − | − | − | − | − | + | − |
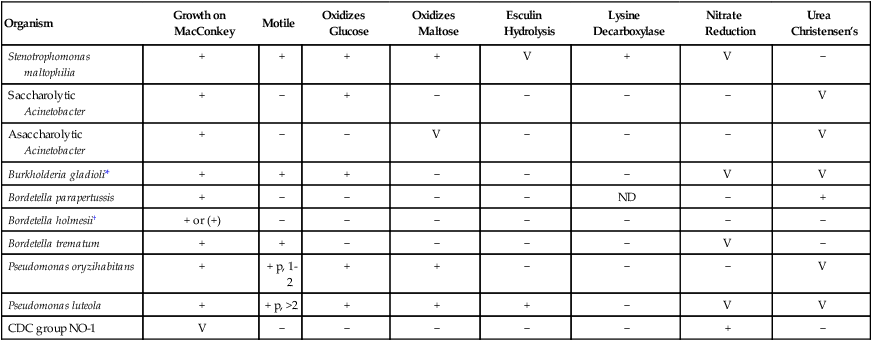
Compiled from Reed RP: Flavimonas oryzihabitans sepsis in children, Clin Infect Dis 22:733, 1996; Seifert H, Strate A, Pulverer G: Nosocomial bacteremia due to Acinetobacter baumannii: clinical features, epidemiology, and predictors of mortality, Medicine 74:340, 1995; and Weyant RS, Hollis DG, Weaver RE et al: Bordetella holmesii sp nov: a new gram-negative species associated with septicemia, J Clin Microbiol 33:1, 1995.
V, Variable; +, > 90% of strains are positive; −, > 90% of strains are negative; ( ), delayed; ND, no data; p, polar flagella.
*B. gladioli is included with the oxidase-negative organisms because oxidase reactions are frequently weak and may only be positive with Kovacs method.
Antimicrobial Susceptibility Testing and Therapy
Acinetobacter spp. and S. maltophilia can exhibit resistance to a wide array of antimicrobial agents, making the selection of agents for optimal therapy difficult (Table 21-5). In addition, automated methods for determining the minimum inhibitory concentration (MIC) for Acinetobacter spp. does not correlate with disk diffusion methods. This underscores the importance of establishing the clinical significance of individual isolates before antimicrobial testing is performed and results are reported (see Chapter 12 for a discussion of criteria used to establish significance). Failure to do so could lead to inappropriate treatment of patients with expensive and potentially toxic agents. If susceptibility testing must be performed, it is recommended that an overnight MIC method be used.
TABLE 21-5
Antimicrobial Therapy and Susceptibility Testing
| Species | Therapeutic Options | Potential Resistance to Therapeutic Options | Validated Testing Methods* | Comments |
| Acinetobacter spp. | No definitive guidelines. Potentially active agents include β-lactam, β-lactam inhibitor, combinations, ceftazidime, imipenem, ciprofloxacin, tigecycline, and aminoglycosides | Yes; resistance to β-lactams, carbapenems, aminoglycosides, and quinolones | Disk diffusion, broth dilution, and agar dilution | In vitro susceptibility testing results are important for guiding therapy. |
| Bordetella holmesii | No definitive guidelines. Potentially active agents include penicillins, cephalosporins, and quinolones | Unknown | Not available | |
| Burkholderia. gladioli | No definitive guidelines. Potentially active agents include imipenem, piperacillin, and. ciprofloxacin | Yes | See CLSI document M100, Performance Standards for Antimicrobial Susceptibility Testing | Rarely involved in human infections. Reliable therapeutic data are limited. |
| Pseudomonas luteola P. oryzihabitans |
No definitive guidelines. Potentially active agents include cefotaxime, ceftriaxone, ceftazidime, imipenem, quinolones, and aminoglycosides | Yes | See CLSI document M100. | Rarely involved in human infection. |
| Stenotrophomonas maltophilia | Multiple resistance leaves few therapeutic choices; therapy of choice is trimethoprim-sulfamethoxazole. Potential alternatives include minocycline, ticarcillin/clavulanic acid, and chloramphenicol |
Yes; intrinsically resistant to most beta-lactams and aminoglycosides; frequently resistant to quinolones | See CLSI document M100. | May be tested by various methods, but profiles obtained with beta-lactams can be seriously misleading. |
| CDC group NO-1 | No definitive guidelines. Appear susceptible to beta-lactam antibiotics | Unknown | Not available |
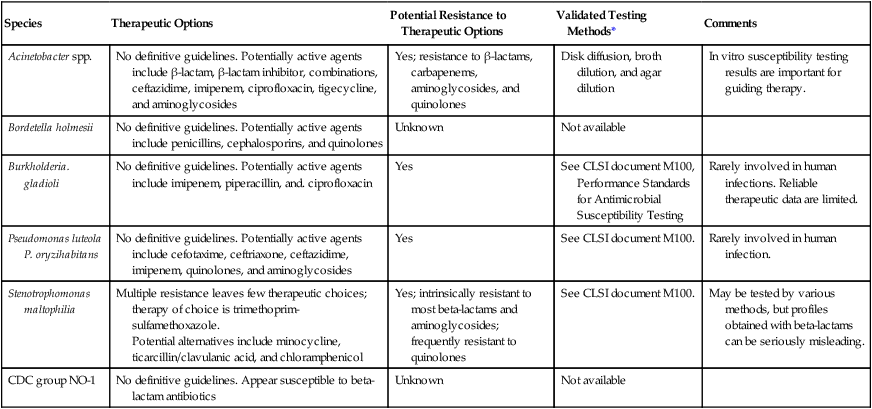
*Validated testing methods include standard methods recommended by the Clinical and Laboratory Standards Institute (CLSI) and commercial methods approved by the U.S. Food and Drug Administration (FDA).
For urinary tract infections caused by Acinetobacter spp., single-drug therapy is usually sufficient. In contrast, more serious infections, such as pneumonia or bacteremia, may require the use of a β-lactam in combination with an aminoglycoside. Tigecycline also has potent activity against these organisms. Because this genus is able to acquire and express resistance to most antimicrobial agents, including imipenem, in vitro testing is recommended for clinically relevant isolates. Methods outlined by the Clinical and Laboratory Standards Institute (CLSI) appear to be suitable for testing Acinetobacter spp., S. maltophilia, and other organisms listed in Table 21-5.
The other agents should be considered only when trimethoprim-sulfamethoxazole–resistant strains are encountered. Even then, the potential efficacy of these other agents is suspect because of the ability of S. maltophilia to rapidly develop resistance. As indicated in Table 21-5, CLSI guidelines are available for the testing of several of the organisms listed in this chapter.