Pathologists have always sat at a very quiet but very important crossroads in healthcare. Every biopsy, every resection, every suspicious smear eventually passes through their hands. For decades, that work happened almost entirely through a microscope, a glass slide and a lot of hard-earned expertise.
Over the past few years, that picture has started to change. High-resolution scanning, cheap storage, faster networks and more mature AI models have combined to push pathology into a truly digital era. The changes are not theoretical anymore. Whole slide imaging is being used for primary diagnosis, AI tools are running inside real clinical workflows and comprehensive laboratory information systems are becoming the backbone that ties everything together.
This shift is not about replacing pathologists. It is about giving them better tools, more context and more time to focus on the hard diagnostic questions.
From glass slides to whole slide images
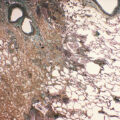
The foundation of modern digital pathology is whole slide imaging. Instead of a pathologist physically moving a glass slide under the microscope, high-throughput scanners now capture the entire slide as a detailed digital file that can be viewed, zoomed and navigated on screen. Recent reviews describe whole slide imaging as a proven technology that supports routine diagnostics, education and research, especially in histopathology.
Regulatory bodies have started to catch up with the technology. In multiple regions, whole slide imaging systems have been cleared for primary diagnosis, and new reimbursement codes have been introduced specifically for digital workflows. That regulatory recognition matters, because it gives hospital and reference labs the confidence to invest in scanners, storage and image management at scale.
Once the hardware is in place, the benefits become obvious fairly quickly. Digital slides can be reviewed remotely, shared instantly with subspecialty experts, incorporated into tumor boards and used for teaching without tying up physical slides. For busy centers and understaffed practices, the ability to route work to wherever the right pathologist is sitting that day is a major advantage.
What AI is actually doing in digital pathology right now
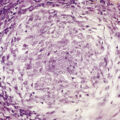
Artificial intelligence is often discussed in broad, abstract terms, but in digital pathology the use cases are becoming concrete. AI models trained on whole slide images are already being evaluated for tasks like tumor detection, grading, margin assessment, quantifying immunohistochemical stains and predicting certain molecular alterations directly from H&E slides.
Systematic reviews of AI in digital pathology show that, when models are trained and validated properly, their diagnostic accuracy can approach that of expert pathologists in narrow tasks. That does not mean an algorithm is signing out reports on its own. What it does mean is that AI can pre-screen slides, highlight suspicious regions, count cells or structures that are tedious to quantify by hand and provide second opinions on borderline features.
Some of the most active areas include:
Pathology triage, where AI flags high-priority cancer cases or potential margin involvement so they can move to the top of the queue.
Quantitative scoring, for example counting positive cells in PD-L1 or Ki-67 stains, which improves consistency across different readers and sites.
Prognostic and predictive modeling, in which deep learning models extract subtle patterns from tissue architecture and cell distribution that correlate with outcomes or treatment response.
The common thread is that AI handles volume and repetition very well. It does not tire, it does not lose focus after the hundredth slide and it can apply a consistent set of criteria across thousands of cases. The pathologist remains the decision-maker, but now with an additional set of measurements and alerts available at a glance.
How AI is changing daily life in the lab
From the outside, it is easy to focus on headline claims about accuracy. Inside the lab, the impact often shows up first in workflow and collaboration.
Once slides are scanned, AI can run in the background, quietly labeling tiles, generating heatmaps or calculating scores before the pathologist even opens the case. In some implementations, a worklist view will show which cases have AI flags, which ones appear straightforward and which ones need a closer look. That kind of triage is particularly helpful in high-volume services such as prostate biopsies, breast screening or dermatopathology.
Digital pathology also enables true telepathology. Subspecialists can review complex cases from home or from another hospital, without waiting for physical slides to be shipped. Tumor boards can project digital slides in the conference room, with AI overlays available when needed to clarify margins or highlight micrometastases. For teaching hospitals, residents can review the exact same images as their attendings, even if they are not in the same room.
There are also quality and safety benefits. Consistent digital images make it easier to standardize stain appearance and to detect subtle drifts in processing over time. Studies on color calibration and scanner variability show that standardization improves both human and AI performance, which ultimately protects patients from misinterpretation.
Adoption challenges and how labs are working through them
For all the enthusiasm, digital pathology and AI are not trivial to implement. Labs need to think beyond buying a scanner. They must plan for storage, network bandwidth, image management, information security, validation protocols and integration with existing systems.
Regulatory guidance now exists for how to validate whole slide imaging for primary diagnosis and how to incorporate AI into clinical workflows, but each laboratory still has to do the practical work of proving that digital reads are at least as reliable as their prior microscope-based process.
Data quality is another real concern. AI models trained on one scanner, one lab protocol or one population may not perform as well elsewhere. That has led to a focus on multi-center datasets, robust color normalization and continuous performance monitoring. Many laboratories are starting small, with well defined use cases and close human oversight, before expanding AI to more complex tasks.
Underneath all of this sits a simple reality. Digital pathology and AI only reach their potential if they are tightly connected to the rest of the lab infrastructure. That is where a modern laboratory information system becomes central.
Why the LIS sits at the center of digital pathology
A pathology laboratory information system is more than a reporting tool. It manages specimen accessioning, barcoding, tracking through the gross room and histology bench, slide labeling, case assembly, result reporting and interfaces with the electronic health record. In a digital environment, it also needs to coordinate with scanners, image management systems and AI services.
When the LIS is properly integrated, a pathologist can open a case from the worklist and immediately see everything in one place: clinical information, prior history, digital slides, AI results and any ancillary testing that has been ordered. The LIS ensures that the right images are linked to the right patient and specimen, that orders and results flow correctly and that the audit trail is clear for regulatory review.
Without that level of coordination, digital pathology can become a collection of disconnected tools. Scanners may sit underused, AI models may run on test servers and the daily workflow may still revolve around manual tracking and phone calls.
How NovoPath helps enable digital pathology
This is where comprehensive platforms like NovoPath come into play. NovoPath is designed specifically as a pathology focused LIS that supports anatomic, clinical, molecular and digital workflows within a single environment.
From a practical standpoint, that means the same system handling accessioning and specimen tracking can also coordinate digital slide viewing, image-based workflows and downstream analytics. NovoPath has a long history of integrating with whole slide imaging systems and digital pathology solutions, allowing images and metadata to flow seamlessly between the scanner, image management layer and the LIS.
For laboratories that are starting or scaling their digital pathology programs, this kind of integration matters in a very tangible way. Pathologists can launch digital slides for a case directly from the LIS, review AI overlays where they are available, finalize reports and push structured data back into the EHR, all within a workflow that feels familiar rather than experimental.
NovoPath’s focus on interoperability also supports broader enterprise goals. Its integration capabilities help tie pathology data into larger healthcare networks, making it easier to share results with oncology teams, radiology systems and population health platforms. For organizations that see AI as a long term strategic priority, having a LIS that already understands digital pathology and can support large structured datasets is a significant advantage.
What comes next for pathology teams
Looking ahead, the line between traditional pathology and computational pathology will keep getting thinner. Foundation models trained on massive slide collections are already demonstrating impressive performance across multiple cancer types. New platforms are emerging that let pathologists build and validate their own AI tools without needing to write code, which should broaden access beyond a handful of academic centers.
In day to day practice, the likely future is a partnership model. Pathologists will continue to interpret complex patterns, reconcile discordant findings and communicate nuanced diagnoses to clinicians. Digital pathology and AI will sit alongside them, handling repetitive measurement, surfacing patterns that are easy to miss with the naked eye and making it possible to share expertise across distance and time zones.
For that vision to work, the underlying digital infrastructure has to be strong. Labs will need scanners that produce reliable images, AI tools that are validated in real clinical settings and LIS platforms, like NovoPath, that are built to orchestrate the entire workflow from specimen to report. When those elements come together, pathology becomes faster, more consistent and better connected to the rest of patient care.
The glass slide and microscope are not disappearing overnight. They are being joined by a powerful set of digital tools that can extend the reach of pathologists and improve the clarity of their work. As digital pathology and AI continue to mature, laboratories that invest thoughtfully in technology, workflows and information systems will be best positioned to deliver timely, high quality diagnoses for the patients who depend on them.