CHAPTER 46. Podiatric Care
Lynda Marks
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Identify the skeletal structure of the foot.
2. Describe specific physical and psychosocial assessment for podiatric patients.
3. Describe operative procedures of the foot.
4. Describe perianesthesia care to be provided to patients having surgical procedures on the foot.
I. ANATOMY AND PHYSIOLOGY
A. Bony structure—7 tarsal, 5 metatarsal, 14 phalanges (Figure 46-1)
1. Tarsals—seven bones of the ankle, hindfoot, and midfoot
a. Talus—irregularly shaped bone
(1) Located between bimalleolar fork and tarsus
(2) Ligament attachments, no tendons
b. Calcaneus—largest bone in foot
c. Cuboid—wedge shaped
d. Scaphoid (navicular)—bound with ligaments
e. Three cuneiforms
(1) Interposed between scaphoid, first three metatarsals, and cuboid
(2) Wedge shaped
2. Metatarsals—five
a. First toe (great toe)
b. Four lesser toes
c. Articulates with three cuneiforms
d. Form tarsometatarsal or Lisfranc’s joint
3. Phalanges
a. Great toe—proximal and distal
b. Lesser toes (2, 3, 4, 5)—proximal, middle, distal
4. Sesamoids
a. Small, round bones
b. Embedded (partially or totally) in substance of corresponding tendon
c. Pressure-absorbing mechanism
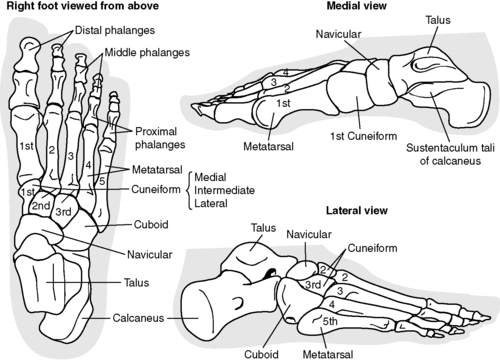 |
| FIGURE 46-1 ▪
Bones of the right foot.
(Redrawn from Jacob S, Francone C: Elements of anatomy and physiology, ed 2, Philadelphia, 1989, WB Saunders.)
|
B. Arches
1. Formed by bony structure
2. Longitudinal (lengthwise) arches
a. Medial longitudinal arch—formed by calcaneus, talus, navicular, three cuneiforms, and first three metatarsals
b. Lateral longitudinal arch—formed by calcaneus, cuboid, and fourth and fifth metatarsals
3. Transverse—across the ball (top) of the foot
C. Muscles, ligaments, and tendons; nerves (multiple structures)
II. ASSESSMENT PARAMETERS (PROCEDURE SPECIFIC)
A. Structural disorders—causes
1. Weakness of muscles, ligaments, and tendons
2. Imbalance between bone support and supporting structure
3. Constant wear, rub
B. Identified disorders (Table 46-1 for podiatric definitions)
1. Hallux valgus (also called bunion): deformity of the foot involving the first metatarsal and great toe (hallux)
a. Lateral angulation of great toe
b. Progresses, resulting in medial deviation of first metatarsal
c. Often accompanied by multiple disorders and symptoms; commonly affects lesser toes
d. Occurs in females nine times more often than males; may be congenital or as a result of rapid growth
e. Symptoms
(1) Adults—pain or dull ache over metatarsal head
(2) Adolescents—chief complaints are unrelenting pain, altered body image; may have family history.
f. Radiographs show exostosis with subluxation or dislocation of first metatarsal head.
2. Hallux varus
a. First metatarsal deviates medially, and the great toe deviates laterally.
b. Condition may start in late childhood or early adult life.
c. More common in females
d. May be agitated by improperly fitting footwear
3. Hallux rigidus—“stiff big toe”
a. Painful stiffness of first metatarsophalangeal joint of the toes when walking; toe becomes rigid.
b. Caused by arthritis
4. Corns—conical thickening of skin in areas of constant irritation
5. Bursal hypertrophy—inflammation of the joint
6. Digital deformity
a. Mallet toe—congenital abnormality of the distal interphalangeal joint, usually genetic
(1) Flexion posture of the distal interphalangeal joint
(2) Most commonly affects second toe
(3) Associated with a long digit
(4) Caused by pressure at tip of toes
(5) Occurs in persons with peripheral neuropathy; no known reason
b. Varus toes
(1) Curly or overlapping toes
(2) Flexion and varus rotation
(3) Commonly affects third, fourth, and fifth toes
c. Hammer toe deformity
(1) Affects one of the lesser four toes (commonly second toe)
(2) Hyperextension at metatarsophalangeal joint, flexion at proximal interphalangeal joint
(3) Etiology unknown
d. Clawtoe
(1) Hyperextension of metatarsophalangeal joint with flexion of the proximal interphalangeal joint
(2) Associated with cavus foot deformity and neuromuscular conditions
7. Interdigital deformity (Morton’s neuroma)
a. Benign enlargement of third common digital branch at site of bifurcation of interdigital nerves (medial plantar nerve)
b. Frequently between and distal to third and fourth metatarsal heads
c. Symptoms and common findings
(1) Pain in plantar forefoot area (sharp, dull, throbbing, or burning sensation)
(2) Swelling of plantar metatarsal
(3) Affects females more than males
(4) Overweight person
8. Pes planus (flatfoot)
a. Loss of normal medial longitudinal arch
b. Initial treatment is conservative therapy with shoes, arch supports.
c. Surgical treatment with onset of disabling pain
d. Correction procedures include Miller, Durham flatfoot plasty, triple arthrodesis, calcaneal displacement osteotomy.
9. Pes cavus (hollow foot, clawfoot)
a. Occurs with neuromuscular conditions such as spina bifida, cerebral palsy, muscular dystrophy, congenital clubfoot
b. Muscular weakness in foot
c. Several procedures required for repair
(1) Soft tissue release, decrease contracture
(2) Tendon transfer to correct muscle imbalance
(3) Osteotomy—incision into a bone
(4) Arthrodesis—surgical immobilization or fusion of a joint
| Arthrodesis | Surgical immobilization or fusion of a joint |
| Arthrolysis | Surgical procedure in which mobility is restored to an ankylosed (fused/immobile) joint |
| Arthroplasty | Surgical repair or reformation of a joint |
| Arthrotomy | Incision into a joint |
| Bunion | Enlargement and inflammation of the joint bursa at the base of the great toe, usually causing the toe to displace laterally; usual etiology is long-term wearing of tight-fitting shoes. |
| Capsulotomy | Incision into the joint capsule |
| Exostosis | A bony growth on the surface of a bone, also called “osteoma” or “hyperostosis” |
| Hallux | The great toe |
| Hallux valgus | Displacement of the great toe laterally toward the other toes; often coexists with a bunion, but often the two terms are inaccurately used synonymously. |
| Hammer toe | A deformity in which there is dorsiflexion of the metatarsophalangeal joint (joint between the foot and the toe) or plantar flexion of interphalangeal (IP) joints. |
| Mallet toe | A deformity in which the most distal IP joint is involved. |
| Morton’s neuroma | Interdigital nerve entrapment within a metatarsal interspace that causes pain, particularly with weight-bearing |
| Osteotomy | Incision into a bone |
| Plantar | Regarding the sole of the foot |
| Tenotomy | Incision of a tendon, often used to correct hammer toe |
III. ELECTIVE OPERATIVE PROCEDURES
A. Treatment of disorders
1. Determined by the degree of involvement
2. Goals toward alignment, shortening, stabilization
3. Multiple procedures may be indicated.
B. General intraoperative care
1. Tourniquet application
2. Operative site cleansing (including clipping of hair and cleaning toenails)
3. Provision of sterile instruments, supplies
4. Availability of implants including joint replacement, K-wire (pins), screws
C. Procedures
1. Arthrodesis
a. Excision of bone wedges with fusion
b. Indicated for severe compromise of muscle function; digital and metatarsophalangeal joint stability inadequate
c. Treatment for hallux valgus
(1) Method: divide tendon, resect cartilage, provide stability to joint with K-wire or other means.
d. Triple arthrodesis—subtalar joint, talonavicular joint, tarsometatarsal joint
(1) Treatment for equinus deformity, cavus deformity, flatfoot, or forefoot cavus
2. Arthroplasty
a. Resection or replacement of bony structure of joint
b. Indicated for alleviation of pain and correction of digits with flexor to rigid deformity caused by:
(1) Inflammatory arthritis
(2) Degenerative arthrosis
(3) Congenital deformity
(4) Flail toes
(5) Revision of previous surgery
c. Keller resection arthroplasty:
(1) Tissues released around the joint
(2) Articular surface exposed
(3) Medial eminence resected
(4) Implant (K-wire) seated
(5) Capsulorrhaphy completed
3. Bunion procedures
a. Revision of soft tissue structures and/or bone to correct deformity
b. Soft tissue procedures correct muscle imbalance: McBride, DuVries, Mann, Silver.
c. Soft tissue and bone procedure: Keller resection arthroplasty, Chevron osteotomy, Akin procedure
d. Purpose: simple treatment of hallux valgus causing impaired function and/or pain; cosmetic improvement
4. Capsulotomy
a. Incision of capsule
b. Treatment of equinovarus foot
c. Performed in conjunction with other procedures
d. Method: incision through superficial fascia, expose joint, incise capsule
5. Endoscopic plantar fasciotomy
a. Operative tissue repair using a less invasive procedure
b. Completed using fluoroscopy
c. Procedure: stab incision, blunt dissection to create a channel, pass a trocar, release the plantar fascia
d. Open procedure more invasive; appropriate procedure for fascia release
6. Exostectomy
a. Resection of lateral prominences (callus) of toes
b. Commonly fifth toe
7. Hammer toe repair
a. Abnormal flexion posture of the proximal interphalangeal joint of one of the lesser four toes
b. Second toe most frequently affected
c. Metatarsophalangeal joint
d. Stage of deformity depends on joint involvement and degree of contracture.
e. Treatment
(1) Soft tissue procedures: Girdlestone, Taylor, Parrish, Mann, Coughlin
(2) Soft tissue and bone procedures
8. Mallet toe repair
a. Flexion posture of the distal interphalangeal joint
b. Second toe most frequently affected
c. Etiology
(1) Pressure at tip of toes, possibly caused by shoes
(2) Persons with peripheral neuropathy; no known reason
d. Treatment
(1) Flexor tenotomy at distal interphalangeal flexion crease
(2) Subtotal or total resection of middle phalanx
9. Osteotomy
a. Removal or addition of a bone wedge
b. Extra-articular or intra-articular
c. Extra-articular most commonly in the calcaneus for cavovarus heel
d. Metatarsal osteotomy for plantar calluses, hallux valgus: many types including wedge resection, Chevron, “Z,” Reverdin, Mitchell
e. Mitchell osteotomy: capsular incision, medial eminence removed, drill holes offset, and suture passed; double osteotomy completed with excision of bone between, capital fragment displaced, and suture tied; medial capsulorrhaphy completed
10. Tenotomy
a. Incision of tendon: eliminates tendon function, relieves contracture
b. Completed in conjunction with other procedures
IV. PERIANESTHESIA PRIORITIES
A. Preoperative (Box 46-1)
1. Support system
a. Available assistance
b. Impaired mobility related to other disease processes
2. Awareness of procedure and expected outcomes
a. Procedure to be performed
b. Anesthetic type
(1) General anesthetic
(2) Ankle block with intravenous conscious sedation
(a) Procedure for block
(b) Sensory deficit—length and precautions
c. Complications
(1) Loss of function, muscular imbalance
(2) Neurovascular compromise, swelling
BOX 46-1
KEY PATIENT EDUCATIONAL OUTCOMES
Patient Will:
Demonstrate proper use of supportive devices (crutches, walker, walking shoe).
Describe proper dosing procedure for prescribed analgesic medication(s) and report uncontrolled pain.
Report excessive drainage on dressings.
Describe signs and symptoms of infection and report findings to physician immediately.
Report any neurological or circulatory impairment.
Describe understanding of need for limited mobility for 6 to 8 weeks.
B. Phase I
1. Predisposing factors
a. Congenital, acquired, or traumatic
b. Older adults and children included in the spectrum
c. Existing conditions
(1) Neuromuscular disease
(2) Neuropathy
(3) Diabetes
(4) Arthritis
d. Previous procedures or anticipated future procedures (bilateral treatment needs)
2. Condition of foot: appearance and sensation
a. Soreness, tenderness, edema
b. Temperature equal on each foot
c. Note presence of pins.
3. Color
a. Blanching of nail beds
b. Capillary refill
4. Vascular status
a. Presence of dorsalis pedis pulse on dorsal center of metatarsal area of each foot
b. Poor vascularity may impede healing.
5. Goals of procedure
a. Pain relief
b. Return or improvement of mobility
c. Cosmetic improvement
d. Extent of procedure influences outcome.
C. Phase II
1. Neurovascular status
a. Sensation in affected and opposite extremity
b. Pulses
c. Coloration, blanching of nail beds, capillary refill
2. Preventive measures
a. Elevation of extremity
b. Ice therapy if ordered by physician, being careful not to place ice over the toes
D. Extended observation/discharge home
1. Ambulation and mobility
a. Home care availability
b. Sensory deficit with use of ankle block up to 8 hours
c. Support devices—crutches, walker, walking shoe, boot
(1) Proper fit
(a) Walking shoe long enough to protect toe, short enough to prevent tripping
(2) Return demonstration of use
d. Non–weight-bearing ambulation 3 to 5 days
e. Limited mobility 6 to 8 weeks (longer depending upon procedure)
2. Wound care
a. Incision site clean, dry
(1) Report bleeding, discharge.
(2) Protect K-wire(s) if used.
(a) Clean around site with alcohol daily.
(b) Removal time depends on procedure; possibly 6 to 8 weeks.
b. Dressings remain intact, clean, dry (use protective waterproof cover for showering).
c. Soft tissue procedures
(1) Bulky, soft dressing for support
(2) Three to 6 weeks with bandages in place (more involved procedures, longer bandage remains)
(3) Compression dressing after 2 to 4 weeks
d. Soft tissue and bone procedures
(1) Six to 8 weeks with bandages in place, guarded ambulation
(2) External support several additional weeks
(3) If bone graft used, may immobilize 3 to 6 months
e. Skin care beneath cast, dressing
3. Return of function
a. Pain management
(1) Nonsteroidal anti-inflammatory medications
(a) Pain after foot surgery intense
(b) Evaluate medication interactions.
(2) Elevation of extremity
(3) Ice therapy if ordered by physician, being careful not to place ice over the toes
b. Ambulation to tolerance
c. Preventive measures
(1) Eliminate pressure, rub on toes from footwear.
BIBLIOGRAPHY
1. Black, J.; Hokanson Hawks, J., Medical-surgical nursing: Clinical management for positive outcomes. ed 7 ( 2004)Saunders, St Louis.
2. Burden, N.; Dawes, B.; O’Brien, D.; et al., Ambulatory surgical nursing. ed 2 ( 2000)WB Saunders, Philadelphia.
3. Lippincott manual of nursing practice. ed 8 ( 2006)Lippincott Williams & Wilkins, Ambler.
4. McGlamery, E.D.; Banks, A.S.; Downey, M.S., Comprehensive textbook of foot surgery. ed 2 ( 2001)Lippincott Williams & Wilkins, Baltimore.
5. Pudner, R., Nursing the surgical patient. ed 2 ( 2005)Bailliere Tindall, Edinburgh, Scotland.
6. Rothrock, J.C., Alexander’s care of the patient in surgery. ed 13 ( 2007)Mosby, St Louis.