CHAPTER 45. Plastic and Reconstructive Care
Theresa L. Clifford
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Describe the clinical management of burn injuries.
2. Describe the anatomy of skin.
3. Describe the physiology of wound healing.
4. Describe preoperative preparation of the plastic surgery patient.
5. Describe common plastic and reconstructive surgeries.
6. Describe common medical conditions affecting surgical outcomes.
7. Identify anesthesia administration concerns for the plastic surgery patient.
8. List psychological factors that affect the plastic surgery patient.
9. Identify nursing care for individual surgical procedures.
10. Evaluate postoperative management and patient education concerns for the plastic surgery patient.
I. OVERVIEW
A. Plastic and reconstructive surgery may be performed for a variety of reasons.
1. Physical appearance
2. Emotional well-being
3. Body image
B. Plastic surgery may be:
1. Elective
2. Cosmetic
3. Reconstructive
a. Correcting congenital or acquired abnormalities
b. Restore normal function and appearance.
C. Anesthetic needs vary on the basis of the complexity of the procedure.
1. Local anesthesia for simple lesion removal
2. Prolonged general anesthesia for complex reconstruction
D. Perioperative needs of the plastic surgery and burn patient.
1. Purpose
2. Procedure
3. Perianesthesia nursing care management
4. Patient education for specific surgical interventions
II. OVERVIEW OF BURNS
A. Determining severity of burn injury
1. Initial area of burn should be reassessed frequently after admission.
2. Size of percent of body surface involved (total body surface area [TBSA])
a. Rule of 9s (Figure 45-1)
(1) Body areas divided into equal multiples of 9
(2) Head and each arm equal 9%.
(3) Chest, back, and leg equal 18% each.
(4) Perineum equals 1%.
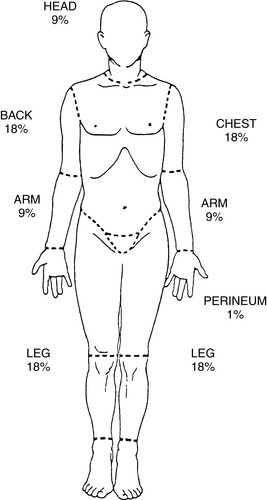 |
| FIGURE 45-1 ▪
The rule of 9s.
|
b. Berkow’s method, or Lund and Browder chart
(1) Used for children
(2) Adjusts for differences in body part sizes between adults and children
(a) Head in child younger than 2 years equals 18%.
(b) Each leg in child younger than 2 years equals 13%.
c. One percent method
(1) Used for quick assessment
(2) Palmar surface of patient’s hand equals approximately 1% TBSA.
(3) Not useful for large-area burns
d. Major burn injury
(1) Adults
(a) Greater than 25% TBSA: partial-thickness burn, age <40 years
(b) Greater than 20% TBSA: partial-thickness burn, age >40 years
(c) Greater than 10% TBSA: full-thickness burn
(2) Children
(a) Greater than 20% TBSA: partial-thickness burn
(b) Greater than 10% TBSA: full-thickness burn
(3) Other factors
(a) Burns of face, eyes, ears, hands, feet, and perineum
(b) Electrical burns
(c) Burns complicated by inhalation injury or major trauma
(d) Patients’ preexisting diseases may impact recovery (e.g., diabetes, congestive heart failure).
B. Depth of injury
1. Superficial injury (first degree)
a. Affects epidermis only
b. Appearance: skin intact, red, blanches
c. Painful
d. Healing time: 2 to 10 days
e. Causes: flash burns, sunburn
2. Partial-thickness injury (second degree)
a. Affects epidermis and part of dermis, leaving skin appendages intact
b. Levels
(1) Superficial partial-thickness: affects upper layers of dermis
(2) Deep partial-thickness
(a) Affects lower layers of dermis
(b) May convert to full-thickness injury
c. Appearance
(1) Superficial partial-thickness: red, moist, blistered, blanches
(2) Deep partial-thickness: deep red, moist, areas of white or yellow tissue, delayed capillary refill
d. Very painful
e. Healing time
(1) If affecting outer layers of dermis, 5 to 21 days
(2) If affecting deeper layers of dermis, 21 to 35 days
(a) May convert to full-thickness burn in first few days after burn
(b) May require skin grafting
f. Causes: scald, flame, chemicals
3. Full-thickness injury (third degree)
a. Affects epidermis and entire dermis and may extend to subcutaneous tissue, muscle, or bone
b. Appearance: hard, dry, leathery; color may be black, tan, white; nonblanching
c. Minimal to no pain
d. Healing time: requires excision and skin grafting
e. Causes: flame, scald, chemicals, electrical, contact with hot surfaces
C. Part of body involved
1. Specific areas of body have significant impact on healing, cosmetic appearance, and function.
2. Head, face, and chest burns significantly related to respiratory function
3. Hand, face, and feet burns significantly related to cosmetics and function
4. Perineal burns significantly related to infection
5. Circumferential burns significant because of compromised circulation
D. Burning agent
1. Scald
a. Most common type of burn, especially in children
b. Caused by immersion, splash, or steam
2. Flame and flash burns
a. Second most common type of burn
b. Commonly associated with smoke inhalation
c. Frequently full thickness in nature
d. From house fires, kerosene or gasoline ignition
3. Contact burns
a. Area burned is well defined in appearance in shape of item contacted.
b. May occur from hot metal, asphalt, or sand
4. Chemical burns
a. Less than 10% of all injuries
b. Acid or alkali
c. May be topical or ingested
d. More commonly from industrial accidents
5. Electrical
a. Least common
b. May cause significant internal or external damage
c. Direct current or alternating current
d. Alternating current more dangerous than direct current because of increased risk for cardiopulmonary arrest
e. Cataracts may occur 1 to 2 days to 3 years after burn.
f. May require extensive reconstructive surgery (e.g., myocutaneous flaps)
E. Age of burn patient
1. Higher mortality in patients younger than 2 years or older than 60 years
2. Thinness of skin in very young and very old makes injury more likely.
3. Changes in immune status alter ability to heal.
F. Preexisting medical conditions that impair healing process
1. Cardiovascular disease
2. Diabetes
3. Pulmonary disease: asthma, chronic obstructive pulmonary diseases
G. Other associated injuries at time of burn that might affect healing
1. Smoke inhalation
2. Traumatic injury (e.g., fractures, closed head injury)
3. Need for tracheostomy significantly increases mortality risk.
III. ANATOMY AND PHYSIOLOGY
A. Function of skin
1. Largest organ of the body
2. First line of defense against trauma and infection
3. Retention of body fluids
4. Regulation of body temperature
a. Vasoconstriction and vasodilation
b. Evaporation of water
5. Secretion and excretion
a. Secretion of oil from sebaceous glands to lubricate skin, preventing cracks and organism invasion
b. Excretion of water, sodium chloride, cholesterol, and urea from sweat glands
6. Metabolizes and produces vitamin D
7. Sensation and communication
a. Pressure, pain, touch, temperature
b. Reaction to environmental stimuli
8. Generates new skin
a. Contributes to self-image
B. Anatomy of skin
1. Properties of the skin
a. Accounts for one sixth of total body weight
b. Receives one third of resting cardiac output
2. Structure of skin
a. Epidermis
(1) Outermost layer—often tough and leathery
(a) Made up of five layers of keratinocytes
(i) Stratum corneum
[a] Layers of dead keratinized cells
[b] Layers
[1] Provide vapor barrier
[2] Protect body from microorganisms and chemical irritants
[c] A localized build-up of dead cells is a callus.
(ii) Stratum lucidum
(iii) Stratum granulosum
(iv) Stratum spinosum
(v) Stratum basale
[a] Regenerates epithelial covering
[b] Necessary for spontaneous healing
[c] Journey from stratum basale to stratum corneum takes 14 to 21 days.
(b) Surface and deepest layers most important in burn care
(c) Blood supplied by dermis
(d) Epidermis lines skin appendages
(i) Sebaceous glands
(ii) Sweat glands
(iii) Hair follicles
(e) New skin can be generated from lining of skin appendages even if epidermis is destroyed.
(f) Varies in thickness from 0.05 to 1.5 mm.
(i) Thickest at soles of feet, palms, scapula
(ii) Thinnest at eyelids
b. Additional epidermal cells
(1) Melanocytes
(a) Produce melanin, a pigment protecting skin from ultraviolet radiation
(b) Give skin its color depending on quantities of melanin
(2) Merkel cells
(a) Mechanoreceptors providing information on light touch sensation
(3) Langerhans’ cells
(a) Help fight infection by engulfing foreign material
c. Epidermal appendages
(1) Hair
(a) Traps air between hair and skin to regulate body temperature
(2) Nails
(a) Protect the distal end of digits
(3) Sweat and sebaceous glands
(a) Help to cool the body as well as reduce infections
d. Dermis—the layer of skin lying immediately under the epidermis; the true skin.
(1) Five main functions of the dermis
(a) Support and nourish the epidermis
(b) Accommodate epidermal appendages
(c) Support infection control
(d) Support thermoregulation
(e) Provide sensation
(2) Two layers
(a) Papillary layer
(i) Composed of fibrous connective tissue made of collagen and elastin
(ii) Contains numerous capillaries, lymphatics, and nerve endings
(b) Reticular layer
(i) Densely arranged connective tissue increasing structural support for the skin
(3) Hypodermis—subcutaneous tissue
(a) Functions to:
(i) Store fat for energy
(ii) Cushion
(iii) Insulate
(b) Contains fascia to facilitate structural movement
(c) Attached to dermis by collagen
e. Deeper tissues
(1) Muscles
(2) Tendons
(3) Ligaments
(4) Bones
C. Physiology of wound healing
1. An alteration in the integrity and function of tissues in the body
2. Intentional wounds from surgical procedure
3. Unintentional wounds include accidental trauma such as a motor vehicle crash or by persistent forces such as that which causes pressure ulcers
4. Terms describing wounds include:
a. Abrasion
b. Avulsion
c. Contusion
d. Laceration
e. Puncture
D. Process of wound healing
1. Inflammation
a. Vascular response—hemostasis for bleeding control
(1) Injury causes blood cells to enter wound and release coagulation factors to promote platelet aggregation and seal the vessel walls.
(2) Thromboplastin is released from injured cells, activating the clotting cascade.
(3) Platelets release growth factors required for tissue development during the subsequent phases of healing.
b. Cellular response—combating infectious processes
(1) Histamines are released from mast cells to cause vasodilation and increased capillary permeability to bring needed nutrients, chemical, and white blood cells (WBCs) to the injured area.
(2) Epithelialization occurs; WBCs cleanse wound (phagocytosis).
(3) Stage of exudate and wound drainage
(4) Stage lasts from time of initial injury up to 4 days.
2. Proliferation
a. Four major events occur.
(1) Neovascularization (angiogenesis)
(a) Formation of new blood vessels in order to reestablish perfusion
(2) Epithelialization
(a) Migration of epithelial cells across the wound
(3) Collagen formation
(a) Collagen fibers add strength to the healing wound.
(4) Granulation tissue formation and contracture
(a) Temporary network of connective tissue formed to fill in wounds
(b) Wound margins begin to move towards the center of the wound.
b. Begins several days after an injury and lasts several weeks
3. Remodeling and maturation
a. Collagen fibers are remodeled, and scar matures.
(1) Becomes flat, thin, silver in color
(2) Stage lasts 1 to 2 years.
E. Comorbidities affecting wound healing
1. Local factors
a. Healing affected by vascularity, tissue tension and motion relative to wound location
b. Dimensions of wound (shape, size, depth)
c. Temperature of wound (normothermic wounds heal better)
d. Desiccation or dehydration of wound
e. Presence of necrotic tissue, foreign bodies, or infection
f. Incontinence or other chronic skin irritants
g. Mechanical trauma such as prolonged or excessive pressure or friction to surface of wound
h. Use of cytotoxic products near wound
i. Dead space—accumulation of air or fluid slows healing, promotes infection.
2. Age
a. Children heal rapidly.
b. Geriatric patients heal slower because of:
(1) Decreased circulation
(2) Higher incidence of chronic illnesses
3. Activity limitations
a. Increase risk of skin breakdown and delayed repair
4. Nutrition
a. Malnutrition, dehydration, and vitamin deficiency slow healing process.
b. Large healing demands require large nutritional reserves.
5. Behavioral risk taking
a. Nicotine—causes poor healing because of:
(1) Oxygen deprivation
(2) Peripheral vasoconstriction
(3) Increased platelet aggregation leading to “tough” clots
b. Alcohol abuse can lead to poor nutrition.
6. Psychological stress
a. Corticosteroids decrease inflammatory response.
b. Catecholamines suppress microcirculation.
7. Medications
a. Chronic use of:
(1) Aspirin-containing products
(2) Steroids
(3) Nonsteroidal anti-inflammatory drugs (NSAIDs)
b. Chemotherapy and other immunosuppressive drugs
8. Immunosuppression
a. History of cancer, human immunodeficiency virus, hypothyroidism, etc.
9. Comorbidities
a. Diabetes
(1) Peripheral macrovascular and microvascular changes
(2) Poor glycemic control
(3) Loss of sensation and neuropathies
(a) Impaired ability to recognize continued tissue damage
(4) Impaired oxygenation and perfusion
(5) Slowed epithelialization and wound contraction
(6) Impaired phagocytosis
b. Peripheral vascular disease
(1) Impaired blood flow such as in venous stasis or anemia
c. Pulmonary disease
(1) Hypoxemia causes tissue hypoxia, which will divert necessary oxygen and nutrients from tissues.
d. Obesity (>20% ideal body weight)
(1) Increased incidence of wound dehiscence and infection
(2) Poorly vascularized adipose increases risk of ischemia.
e. History of bleeding disorders
F. Physiologic changes after burn injury
1. Burn shock
a. Massive fluid and protein shifts from intravascular space to interstitium
(1) Vasodilation, increased capillary permeability, and altered cell membrane at injury site
(2) Hypovolemic shock occurs because of volume loss.
(3) Edema of tissues occurs from increased capillary permeability.
b. Hypovolemia stage lasts for first 48 hours after injury.
c. Sodium and protein lost from intravascular space into interstitium
2. Hypothermia
a. Loss of water and heat by evaporation
b. Loss of skin’s ability to vasoconstrict or vasodilate in response to environmental temperature
3. Cardiovascular
a. Decreased cardiac output related to hypothermia, uncompensated hypovolemia, and release of myocardial depressant factor
b. Catecholamine release from stress response causes vasoconstriction and increases systemic vascular resistance.
c. Potential for decreased organ perfusion exists.
4. Pulmonary
a. Potential airway obstruction from edema of face and neck
b. Decreased chest wall compliance if chest expansion is impaired by chest burns
c. Bronchopulmonary mucosal damage from smoke inhalation
5. Metabolic
a. Hypermetabolic state occurs as result of stress response.
b. Patient develops catabolic state.
6. Immunologic
a. Postburn immunosuppression occurs from changes in humoral and cell-mediated immunity.
b. Loss of skin as first line of defense
7. Hematologic
a. Potential red blood cell hemolysis from thermal injury
b. Decreased coagulation ability from loss of clotting factors into interstitium
8. Gastrointestinal
a. Development of paralytic ileus
b. Prone to stress ulcer development
9. Renal failure
a. Related to inadequate fluid resuscitation
b. Related to myoglobinuria from muscle damage in electrical and severe flame burns
IV. ASSESSMENT
A. Local procedures
1. Complete blood cell count
2. Prothrombin time (PT)/partial thromboplastin time (PTT) with a history of bleeding or easy bruising
3. Additional tests as appropriate depending on the patient’s medical history and physical exam
B. General anesthesia
1. Complete blood cell count
2. Chemistry profile
3. Electrocardiogram (ECG) in adults older than 45 years or with known cardiac condition
4. Pulmonary function testing if necessary
5. Chest x-ray film (in adults or in children with pulmonary pathologic findings)
6. Bleeding profile:
a. PT
b. PTT
c. International normalized ratio (INR)
7. Pregnancy testing as indicated or desired
C. Psychological considerations
1. Body image—the mental picture we possess of our own body
a. Body image is a changing dynamic entity influenced by internal and external factors.
b. Body image is a component of how we feel about ourselves.
c. Most patients undergo elective cosmetic surgery because of body image dissatisfaction.
2. Motivation for plastic surgery
a. Internal motivation—surgery to change physical appearance of oneself
b. External motivation—surgery to change physical appearance at recommendation of others
c. Patients who are internally motivated are most pleased with surgical outcomes.
d. History of repeated surgeries
e. Patients who are dissatisfied with results may:
(1) Request or undergo repeat procedures
(2) Experience
(a) Depression
(b) Isolation
(c) Coping disturbances
(d) Self-destructive behaviors
f. Rule out body dysmorphic disorder—preoccupation with an aspect of one’s appearance.
3. Preoperative psychological assessment
a. Determine mental status and mood.
(1) Poor outcomes associated with history of depression and/or anxiety
(2) Patients with personality disorders also have poor postoperative outcomes.
b. Understand patient’s perception of body deformity.
c. Understand patient’s expectation of surgical outcome.
d. Explore significant other’s feelings regarding procedure.
e. Assess postoperative support and coping mechanisms.
4. Integration of surgical changes into body image
a. Patients may progress through the stages of grieving.
b. Changed physical appearance slowly integrates into body image and then self-concept.
c. Some patients never integrate changes into body image; may request more surgery or require counseling.
5. Nursing care related to body image
a. Encourage patient to verbalize feelings.
b. Reassure patient that it is normal to desire physical attractiveness.
c. Support the stages of grieving.
d. Be nonjudgmental with verbal and nonverbal communication.
6. Determine patient’s expectations of surgery.
a. Expectations realistic?
(1) Poor outcomes associated with unrealistic expectations
b. Motivation for surgery?
c. Reinforce that immediate results may not meet patient’s expectations because of swelling, color changes, and suture lines.
d. Family expectations
e. Reinforce that long-term results may not meet expectations.
7. Impact of deformity on patient’s self-perception
a. How does patient view it as changing his or her life?
b. How important is it to be attractive?
c. Effect of others’ reactions on patient
8. Psychological evaluation and/or therapy may be appropriate before procedure.
V. PERIOPERATIVE CONCERNS
A. Preprocedural teaching
1. Preemptive medications should be reviewed with patient.
2. NPO (nothing by mouth) instructions
3. Review any over-the-counter medications and herbal remedies patient uses to determine whether any need to be stopped.
4. Encourage patient to stop smoking before surgery.
5. Encourage to wear loose, button-up clothing with preferably slip-on shoes for comfort.
6. Have patient arrange for a ride and home care support.
B. Procedural concerns
1. Primary goals for plastic surgery procedures
a. Provide cosmetically acceptable results.
b. Restore function.
c. Promote healing with minimal scarring.
d. Prevent infection.
2. Many procedures are carefully planned before surgery using photography, computerized imaging, and so forth.
3. Patient positioning requirements
a. Provide comfortable access to surgical field.
(1) Optimal position on table to allow for repositioning during procedure to evaluate results (e.g., mammoplasty)
b. Prevent nerve compression from improper positioning.
(2) Careful positioning
(3) Padding of pressure points
4. Promote venous drainage.
a. Use of sequential compression devices (SCDs) and thromboembolism deterrent stockings (TEDS), for example
5. Provide for greatest hypotensive advantages (reduction of bleeding) if deliberate hypotensive technique is used.
6. Incision placement
a. Incisions placed so that scar lines lie parallel to existing skin lines or behind hairline
b. Skin lines represent areas with minimal tension.
c. Cosmetic effect better if tension is minimized
d. Frequently found under long axis of muscle
7. Hemostasis
a. Must be obtained and maintained to promote good cosmetic effect
b. Bleeding under skin potentiates:
(1) Inflammation
(2) Infection
(3) Pressure
(4) Dehiscence
c. Achieved with:
(1) Ligation
(2) Electrocautery
(3) Pressure
8. Instrumentation
a. Microinstrumentation for nontraumatic repair
b. Use of operating microscope
(1) Provides three-dimensional view (stereoscopic) that must be clearly seen by surgeon and assistants
(2) Careful movements in vicinity of operating table
(3) May require separate instrument tables for donor and recipient sites
c. Lasers
(1) LASER: acronym for light amplification by stimulated emission of radiation
(2) Carbon dioxide (CO 2) laser, argon laser, and neodymium:yttrium-aluminum-garnet (Nd:YAG) laser may be used in aesthetic (cosmetic) surgery.
(3) Uses
(a) Removal of professional tattoos and traumatic scars
(b) Obliteration of blood vessels
(c) Removal of skin lesions and cancers
(d) Alternative for skin resurfacing (CO 2 laser)
(i) Laser blepharoplasty
(4) Precautions
(a) Warning signs should be posted indicating that a laser is being used.
(b) Skin preparation solution may not contain combustible agents.
(c) Surgical drapes around the site must be kept wet.
(d) Proper eye protection for everyone must be provided.
d. Endoscopy
(1) Endoscope requires body cavity for insertion of scope and visualization.
(a) No natural cavities in plastic surgery operative areas
(i) Cavity created by use of umbrella or balloonlike retractor on soft tissues
(b) Uses
(i) Endoscopic forehead lift
(ii) Facelift
(iii) Augmentation or reduction mammoplasty
(iv) Abdominoplasty
C. Anesthesia concerns
1. Selection of anesthetic routes and agent
a. Local anesthesia
(1) Suitable for minor plastic surgical procedures (e.g., skin lesions, rhinoplasty)
(2) Often used for outpatients or office patients
(3) Indicated for procedures that require patient participation (e.g., patients may need to open and close eyes during blepharoplasty)
(4) Selection of agent that lasts 50 to 100 minutes longer than anticipated length of surgery
b. Regional anesthesia
(1) Suitable for procedures localized to extremity
(a) Axillary, plexus blocks for upper extremities
(b) Sciatic block for feet
(c) Lumbar epidural or spinal for leg procedures
c. General anesthesia
(1) Suitable for long procedures, pediatrics, and anxious patients
(2) Long plastic procedures generally require lighter general anesthesia.
(3) Selection of inhalation agents
(a) Agents that do not sensitize the heart to catecholamines because of large doses of epinephrine used in plastic procedures (e.g., isoflurane)
(b) Agents that are less likely to precipitate coughing and laryngospasm, particularly in procedures of face and neck
(c) Length of time required for elimination for short procedures (e.g., enflurane is rapidly eliminated if used in procedures that last less than 40 minutes)
(d) Inducing deliberate hypotension
(i) Selection of agents that induce hypotension
[a] Reduces blood loss
[b] Improves visibility at surgical field
(ii) May be accomplished with volatile agents alone or in combination with:
[a] Ganglionic blocking agents
[b] Vasodilators
[c] Alpha-blockers
[d] Beta-blockers
(iii) Used for reconstruction of head and neck
(iv) Hypotension onset and reversal performed slowly to prevent rapid blood pressure fluctuations (e.g., perfusion to organ is maintained)
2. Intraoperative management
a. Airway management
(1) Method of intubation (oral or nasal) depends on access to surgical field.
(a) Nasal intubation for oral procedures
(b) Use of oral or nasal Ring-Adair-Elwyn (RAE) tube for cleft lip and palate repair (endotracheal tubes with sharp curves that promote access to field by surgeon)
(c) Intubation may be difficult and require fiberoptic bronchoscope in patients, particularly children, with maxillofacial deformities.
(2) Ensure vigorous spontaneous breathing before extubation in patients with maxillofacial surgery.
(3) Esophageal or precordial stethoscope to assess ventilation
(4) Monitor oxygenation.
(a) Transcutaneous oxygen measurement
(b) Direct arterial blood gas measurement
(c) Pulse oximetry
(5) Carbon dioxide monitoring; end-tidal carbon dioxide
(a) Elevated carbon dioxide levels result in vasodilation, which increases bleeding and intracranial pressure.
b. Cardiovascular management
(1) ECG monitoring (including ST-segment analysis) for patients at risk for coronary ischemia
(a) From use of epinephrine
(b) As result of deliberate hypotensive technique
(2) Direct or indirect blood pressure monitoring
(a) Large blood loss common in plastic procedures
(i) Crystalloids
(ii) Colloids
(iii) Blood products
(b) Significant hypotension may result in graft or flap failure.
(3) Positioning and position change
(a) Anesthetic agents affect vascular homeostasis and reflect pressure control mechanisms.
(b) Position changes during procedure may be necessary.
(i) To access donor and recipient sites
(ii) To evaluate cosmetic result of procedure (e.g., mammoplasty)
(c) Minimizing excessive hypotension
(i) Slow, careful movement of patient
(ii) Maintain light anesthesia.
(4) Emergence from anesthesia
(a) Smooth emergence desired to prevent thrashing that may disrupt delicate suture lines
(b) Prevent excessive coughing, particularly in head and neck procedures.
(c) Minimize nausea and vomiting.
VI COSMETIC BODY PROCEDURES
| Augmentation Mammoplasty |
| Rhinoplasty |
| Liposuction/Fat Transfer* |
| Blepharoplasty |
| Abdominoplasty |
| *Most widely performed procedure worldwide. |
A. Abdominoplasty
1. Purpose
a. Surgical correction of deformities of anterior abdominal wall
b. Removal of apron deformities (panniculus)
c. Repair of muscle wall from previous abdominal surgeries
d. Improve body shape
e. Also known as a “tummy tuck”
2. Procedure
a. Surgical removal of loose and redundant tissue of the abdomen
b. Involves skin, fascia, and adipose tissue
c. May include closure of abdominal wall muscles
3. Perianesthesia care
a. Anesthesia: general
b. Patient selection important for ambulatory abdominoplasty
(1) Must stay within close proximity to surgery center
(2) Patient must be motivated.
(3) Home support must be adequate.
c. Maintain good pain control so patient can ambulate, cough, and deep breathe.
d. Control nausea so pain medications will be tolerated.
e. Maintain correct positioning.
(1) Head of bed elevated
(2) Pillow under knees
(3) Use pillow splint for coughing and moving.
(4) Walk in stooped position for 1 week.
f. Empty drains as needed.
(1) Two Jackson-Pratt drains not unusual
(2) Empty and record drainage.
(3) Maintain patency of drains.
(a) Clots can be a sign of hematoma formation.
g. Patient will wear a compression girdle for 2 to 3 weeks.
4. Patient education
a. Review instructions with patient and caregiver.
(1) Demonstration for positioning and moving
(2) Activity restrictions: no straining, lifting, exercising for 4 to 6 weeks
(3) Drain-emptying demonstration
(4) Hematoma assessment
(5) Pain management techniques
(6) Keep compression garment on as directed.
(7) Report signs and symptoms of infection.
B. Buttock, thigh, upper arm lifts
1. Purpose
a. Eliminate loose and sagging skin.
b. Improve appearance and boost self-confidence.
2. Procedure
a. Excision of redundant skin and tissue
b. Excisional surgery can be performed in conjunction with liposuction.
3. Perianesthesia care
a. Anesthesia: local or general
b. Maintain good pain control so patient can ambulate, cough, and deep breathe.
c. Monitor drains if used.
(1) Maintain patency of drains.
(2) Clots can be a sign of hematoma formation.
d. Patient will wear a compression girdle for 2 to 3 weeks.
4. Patient education
a. Review instructions with patient and caregiver.
(1) Demonstration for positioning and moving
(2) Activity restrictions: no straining, lifting, exercising for 4 to 6 weeks
(3) Drain-emptying demonstration
(4) Hematoma assessment
(5) Pain management techniques, including cold compress applications (avoid aspirin)
(6) Keep compression garment on as directed.
(7) Report signs and symptoms of infection.
C. Liposuction and fat transfer
1. Purpose
a. To remove pockets of adipose tissue for body contouring
b. Reimplantation of fat for tissue augmentation (liposhifting)
2. Procedure
a. Removal of adipose tissue with suction-assisted device from face, neck, abdomen, thighs, buttocks, flanks, and extremities
b. Small (1-2 cm) incisions used to minimize scarring
c. Adipose tissue aspirated using crisscross technique
d. Compression dressing applied to collapse tunnels created
e. Accurate volume loss recorded to monitor for hypovolemia and third spacing
3. Perianesthesia care
a. Anesthesia: general or local
(1) More procedures being done with local anesthesia, allowing for better positioning and cooperation by awake patients
b. Preprocedure, patient is marked in standing position.
c. Often performed on outpatient basis unless more than 2500 mL of fat is removed
(1) Admit for fluid replacement.
d. Medicate for pain.
e. Usually described as mild to moderate
f. Maintain fluid balance.
g. Observe for hypovolemia.
(1) Replace fluids as indicated by clinical signs and symptoms.
(2) Autologous blood should be available when high blood loss is expected.
(3) Estimated blood loss will be decreased with the tumescent technique versus the nontumescent technique.
(a) Tumescent technique
(i) Involves infusion of saline, lidocaine, and epinephrine into area to be suctioned
(ii) Lipolysis is improved and blood loss is decreased.
(iii) Third spacing can occur with removal of large volumes of adipose tissue.
h. Assess for hematoma and seroma formation.
i. Compression applied with compression garment or ACE wraps
(1) Keep dressings flat and smooth for even contouring.
4. Patient education
a. Instruct patient to push fluids to cover third-space fluid shifts.
b. Patient should avoid aspirin-containing products.
c. Compression garment will be worn for 24 hours to several weeks (physician preference).
d. Activity
(1) Rest; minimal activity for first week
(2) Avoid strenuous activity for 1 month.
e. Observe for hematoma and seroma formation.
f. Bruising and swelling expected
g. Female urinal can aid in elimination while compression garment is worn.
h. Instruct patient to protect bedding the first 24 hours because copious serous-sanguineous drainage is not unusual.
i. Sponge bathing may be required while patient is restricted to compression garment.
D. Body contouring
1. Purpose
a. Increasing popularity of weight loss surgeries to remove excess skin primarily from the abdomen, back, upper arms, breasts, inner and outer thighs
b. Excess skin can cause chafing, moisture retention, skin infections, musculoskeletal and postural strains.
c. Improve sense of well-being and accomplishment
2. Procedure
a. Contouring will depend on the presence of excess and redundant tissue.
b. Procedures often done in combination
(1) Abdominoplasty
(2) Mastopexy
(3) Mammoplasty
(4) Brachioplasty
(5) Thigh lift
(6) Mons reduction
(7) Liposuction
(8) Buttock augmentation
c. Surgery usually planned once weight loss has plateaued for 12 to 24 months
3. Perianesthesia care
a. Anesthesia: general
b. Surgery times can vary from 2 to 10 or more hours.
(1) Increased risk for pressure ulcers in the operating room
(2) Deep vein thrombosis
(3) Pulmonary emboli
c. Increased risks associated with weight loss surgery
(1) Protein and/or vitamin deficiencies interfering with wound healing
(2) Residual comorbidities such as diabetes, sleep apnea
(3) Persistent or unhealed skin irritation and infections
(4) Unresolved psychological component to weight management and eating disorders
(5) Medication risks
(a) Avoid because of increased risk for ulcers and bleeding
(i) NSAIDs
(ii) Aspirin
(iii) Cyclooxygenase-2 inhibitors
(b) Avoid
(i) Tetracycline
(ii) Macrolides
(iii) Oxycodone
4. Patient education
a. Review instructions with patient and caregiver.
(1) Demonstration for:
(a) Positioning and moving
(b) Early ambulation
(2) Activity restrictions: no straining, lifting, exercising for 4 to 6 weeks
(3) Drain-emptying demonstration
(a) Hematoma assessment
(b) Foley care if necessary
(4) Pain and comfort management techniques, including cold compress applications, elevation of affected extremities, nausea control
(5) Keep compression garment on as directed.
(6) Report signs and symptoms of infection.
E. Spider vein therapy
1. Purpose
a. To treat spider veins (telangiectasia) and varicose veins
2. Procedure
a. Sclerotherapy
(1) Injection of chemical agents to eliminate unsightly veins
(2) Three categories of agents
(a) Detergents
(b) Osmotic agents
(c) Chemical irritants
b. Other treatment options include
(1) Laser surgery
(2) Electrodesiccation
3. Perianesthesia care
a. Anesthesia: local
b. Observe for itching and burning at injection site.
4. Patient education
a. Keep compression bandages on as directed.
b. Early return to walking regimens encouraged to promote aerobic circulation
c. Mild analgesics may be required initially for cramplike discomfort.
d. Reinforce with patient that area will “look and feel worse before it gets better.”
VII. COSMETIC BREAST AND CHEST PROCEDURES
A. Augmentation mammoplasty
1. Purpose
a. To improve body image and self-confidence
b. To modify shape of breast to:
(1) Increase breast size
(2) Correct surgical defects with the use of a prosthesis
2. Procedure
a. Insertion of prosthetic devices (e.g., tissue expanders that are inflated with normal saline)
b. Prosthesis placed under the pectoral muscle or mammary tissue through an inframammary, axillary, areolar incision, or endoscope
(1) Submammary: beneath breast tissue on anterior surface of pectoralis muscle
(2) Submuscular: beneath pectoralis major and serratus anterior muscles
3. Perianesthesia care
a. Anesthesia: general or local with monitored anesthesia care (MAC)
b. Assess for hematoma.
(1) Palpate superior aspect of pectoralis muscle over the third rib to the clavicle.
(2) Breast size should remain equal.
c. Assess for signs of pneumothorax.
(1) More common with axillary incision
(2) Have chest tube and drainage setup available.
(3) Auscultate lung sounds.
d. Provide pain relief.
(1) Pain is moderate to severe.
(2) Prosthesis beneath chest muscle is more painful.
(3) Multimodal drug therapy effective
(a) Preemptive oral narcotics
(b) Toradol and narcotics intravenous (IV) or oral
(c) Local anesthesia in wounds
(d) Muscle relaxants for spasm
(e) Ice may be helpful for pain control.
e. Prevent and treat nausea so oral pain medications can be tolerated.
4. Patient education
a. Observe for hematoma.
b. ACE wrap or soft-support bra may be worn for 1 week.
c. Observe for capsule formation.
(1) May occur months after surgery
d. Massage instructions per physician preference
(1) Massage usually begins within first 2 weeks.
(2) Massage keeps prosthesis mobile in pocket.
(3) Postmassage ice packs helpful
e. Activity
(1) Restrict arm activity for 3 to 4 weeks.
B. Pectoral implantation
1. Purpose
a. To provide an athletic chest contour for male patients
b. To treat underdevelopment of muscles of one side of chest as a result of congenital defects or injury
2. Procedure
a. Small transaxillary incisions made
b. Implants inserted under pectoralis muscles
c. Can be done endoscopically to minimize risk of bleeding and infection
3. Perianesthesia care
a. Similar to breast augmentation surgery
b. Usually no drains required
c. Assess for hematoma formation.
4. Education
a. Pain is usually mild to moderate soreness.
b. Normal activity can be resumed within a week, but strenuous exercise should be restricted for at least 6 weeks.
C. Gynecomastectomy
1. Purpose
a. To improve self-confidence and body image
2. Procedure
a. Removal of excessive breast tissue in male patient
b. May combine excision of excess skin and tissue with liposuction
3. Perianesthesia care
a. Anesthesia: general or local (for small excision)
b. Assess for hematoma formation.
c. Maintain patency of drains (Jackson-Pratt not unusual).
d. Pain usually described as moderate
4. Education
a. Observe for hematoma.
b. Provide instruction and demonstration of drain care.
c. Usually removed after 48 hours
d. Arm activity limited for 1 month
e. ACE wrap or compression vest usually worn for compression
D. Mastopexy
1. Purpose
a. Reshaping (uplifting) of redundant, sagging breast skin
b. Generally less than 300 g of tissue removed
2. Procedure
a. Incisions usually placed in the inferior pedicle, maintaining nerve innervation to the nipple
3. Perianesthesia care
a. General anesthesia most common
b. Usually same-day procedure
c. Position supine or semi-Fowler’s for comfort.
d. Assess for hematoma formation.
e. Maintain patency of drains if used (rarely).
f. Pain usually described as mild
4. Education
a. Observe for hematoma.
b. Surgical support bra may be worn.
c. Inform patient about potential for scarring.
VIII. COSMETIC HEAD AND NECK PROCEDURES
A. Blepharoplasty
1. Purpose
a. To repair or reconstruct upper or lower eyelid to correct “baggy” appearance
b. To provide patient with a more youthful and less fatigued look
c. To improve vision fields
2. Procedure
a. Surgical removal of redundant skin and adipose tissue with shortening of muscles of upper and lower eyelids
b. Incisions placed in the crease of the upper lid and in the lower lid below lash margin
c. Surgical incisions may be done with laser or scalpel.
3. Perianesthesia care
a. Anesthesia: local
b. Assess for signs of retrobulbar hematoma formation.
(1) Signs of medical emergency
(a). Pressure behind eye
(b). Loss of vision
(2) Observe for:
(a). Pallor, ecchymosis, firmness, or complaints of pain or tightness around eyes
(b). Proptosis: forward displacement or bulging eye
c. Maintain normal blood pressure.
(1) Retards hematoma formation
(2) Avoid straining, lifting, bending at least 1 week.
(3) Elevate head of bed.
d. Pain usually described as mild to moderate
(1) Control with moderate strength narcotics (codeine or hydrocodone usually effective).
(2) Ice packs provide pain control and decrease swelling.
4. Education
a. Activity
(1) Avoid activities that will increase blood pressure.
(2) Keep head elevated.
(3) Limit reading and television for 48 hours.
b. Observe for hematoma formation.
c. Use ice or cool, moist compresses as ordered.
(1) Keep cloth between ice bag and skin.
(2) Frozen peas in the bag work well.
d. Eyes may be dry and lashes crusty with bloody drainage.
e. Expect periorbital ecchymosis and swelling.
(1) Mild blurring expected
(2) Call immediately for loss of vision or pressure behind eye.
(3) Use sterile saline drops to moisten eyes and separate lashes.
f. Sutures usually removed in 5 days or surgeon preference
B. Genioplasty and mentoplasty
1. Purpose
a. Surgical reshaping of chin
b. Modifications in mandible or insertion of prosthesis
c. May be performed in conjunction with rhinoplasty to provide a balanced facial profile
2. Procedure
a. Incisions placed inside mouth or beneath chin
3. Perianesthesia care
a. Maintain dressing.
b. Liquid or soft diet
c. Meticulous oral hygiene if oral incisions placed
4. Education
a. Minimize facial movements.
b. Offer suggestions for nutritional alternatives.
c. Meticulous oral hygiene if oral incisions placed
C. Otoplasty
1. Purpose
a. Surgical reshaping or repositioning of ears
b. To correct prominent or malformed ears (i.e., microtia)
c. To improve body image and self-confidence
d. May be performed on children after 6 years of age, when ears have reached most of their adult size
2. Procedure
a. Reshaping of cartilage and skin of the outer ear
b. May require harvesting cartilage from ribs
3. Perianesthesia care
a. Anesthesia: local or general, depending on age of patient
b. Frequently a procedure for school-age children
c. Assess for hematoma formation.
(1) Use severe pain as an indicator because of bulky head dressing.
d. Maintain patency of any drains.
e. Medicate for pain with oral narcotics.
(1) Usually described as moderate pain
f. Children have usually suffered teasing because of ears.
(1) Assure them that surgical outcome is good.
4. Education
a. Activity
(1) Elevate head with two pillows.
(2) No strenuous activity for 2 to 4 weeks
b. Ears will be sensitive to cold and swell in heat for 3 to 6 months.
c. Observe for hematoma.
d. Teach drain care.
e. Bulky head dressing usually worn for 1 week
D. Rhytidoplasty, rhytidectomy, browlift
1. Purpose
a. To remove wrinkle and facial laxity giving a more rested, youthful appearance
b. To tighten loose tissue in face
(1) May involve skin, fat, subcutaneous tissue, and muscle
2. Procedure
a. Standard incisions placed in temporal area behind hairline
b. Additional procedures may be performed in conjunction with rhytidectomy.
(1) Tightening of underlying fascia in the superficial musculoaponeurotic system
(2) Blepharoplasty, browlifting, chemical peel, suction-assisted lipectomy or lipolysis
c. Rhytidectomy—facelift
(1) Tightening of all tissue of the face and neck with excision of redundant tissue
d. Coronal browlift
(1) Tightening the tissue of the forehead and brow with excision of redundant tissue
e. Endoscopic surgery of the head and neck
(1) Face, neck, and browlift may be performed with the endoscopic technique when redundant tissue excision is not required.
(2) Endoscopic techniques generally involve minimal bleeding.
3. Perianesthesia care
a. Anesthesia: MAC or general
b. Assess for hematoma formation.
(1) Palpate neck, forehead, and check frequently.
(2) Bulky dressings common
(a) Assess for absence of increasing tightness, difficulty breathing, or swallowing.
(b) If any question of hematoma, notify surgeon so dressing can be taken down.
c. Maintain patency of drains.
(1) May have Jackson-Pratt or Penrose
d. Maintain normal blood pressure.
(1) To prevent hematoma formation
(2) Manage pain before it increases blood pressure.
(3) Treat uncontrolled hypertension with antihypertensives if pain management not the cause.
e. Prevent nausea and vomiting.
f. Provide calm, reassuring environment to decrease anxiety.
g. Maintain comfort.
(1) Pain can be considered moderate to severe for facelift.
(2) Browlift pain usually described as severe headache
(3) Begin medications before all local anesthesia has resolved.
(4) Combination of oral and IV narcotics may be required.
(5) Toradol very effective but contraindicated by some physicians because of bleeding potential
(6) Cold compresses or ice can be effective.
h. Positioning
(1) Elevate head of bed to decrease swelling.
(2) Avoid activities that increase blood pressure.
(3) Avoid turning head side to side or nodding.
i. Assess cranial nerve VII.
(1) Temporary numbness of ears and cheeks are normal sequelae.
(2) Ask patient to smile, frown, wrinkle forehead and nose.
(3) Assess facial symmetry.
(4) Assess sensation of earlobes.
(a) If facial nerve damaged, it will regenerate with time.
4. Education
a. Activity
(1) Avoid strenuous activity for 1 month.
b. Elevate head and torso with two pillows at bedtime.
c. Observe for hematoma formation.
(1) Drain care demonstration
(2) If drains present, usually removed in 24 hours
d. Hair washing per physician
(1) Usually after sutures are removed in 1 week
e. Soft diet with little chewing
f. Appropriate use of pain medications and ice for pain control
g. Signs to report
(1) Increased facial pain or unilateral numbness
(2) Signs and symptoms of infection
E. Rhinoplasty
1. Purpose
a. Surgical reshaping of nose
b. To improve body image and self-confidence
2. Procedure
a. Excision of fat, cartilage, and skin with fracturing of nasal bones to reshape the nose
3. Perianesthesia care
a. Anesthesia: general or MAC with local anesthesia
b. Provide comfort measures.
(1) Pain usually described as moderate but may be severe
(2) Medicate with oral or IV narcotics as needed.
(a) NSAIDs can be helpful.
(b) Begin medications before local anesthesia resolves.
(c) Ice mask to reduce swelling and pain
c. Provide calm, reassuring environment.
d. Patient may have packing in both nares.
(1) Maintain nasal packing, and avoid removal of clots from nose.
(2) Change “drip pad” as needed.
(3) Avoid pressure to nose, including glasses.
(4) Sneeze through mouth.
(5) Inability to breathe through nose can be anxiety producing.
(a) Provide reassurance.
(6) Mouth will be very dry.
(a) Give frequent mouth care.
e. Position patient with head of bed elevated.
f. Prevent postoperative nausea and vomiting.
(1) Encourage patient to expectorate any postnasal bloody secretions.
(2) Medicate with antiemetics as needed.
4. Education
a. Activity
(1) No strenuous activity for 1 month
(2) No flexing from waist
(3) No flexing head
b. Nasal packing usually removed in 24 to 72 hours
c. Continue ice mask at home.
(1) Swelling and bruising may be worse on second or third postoperative day.
d. Use humidifier at home to prevent drying of mucous membranes.
e. Force fluids.
F. Skin enhancement and minimally invasive procedures
1. Purpose
a. To remove signs of aging and give a youthful appearance
b. Use of chemical agents to remove or destroy tissue to improve tone and texture of skin
c. Removal of facial epidermis and part of superficial dermis to correct skin defects
(1) Acne or depressed scarring
(2) Wrinkles
(3) Irregular skin pigmentation
2. Procedures
a. Chemical peels
(1) Phenol: creates a controllable superficial thickness burn
(2) Trichloroacetic acid: medium depth peel causing temporary blanching of skin
(3) Alphahydroxy acid (“fruit peel”): better choice for “sensitive” skin because it causes less irritation and photosensitivity postapplication
(4) Retin A: common topical treatment for acne
b. Dermabrasion
(1) Helpful for skin resurfacing: to make skin smoother, improve mild pigmentation problems, reduce pore size and treat acne, and give skin a smoother contour
(2) Uses sanding with microparticles or rotating wire brushes on skin
c. Collagen injections: injections of autologous or bovine collagen to enhance or remodel skin and tissue appearance
(1) Scar revisions
(2) Lip enhancement
(3) Minor facial corrections
d. Laser hair removal
e. Soft tissue filling: hyaluronic acid
3. Perianesthesia care
a. Anesthesia: usually local, general if combined with total facial resurfacing
b. Provide comfort measures.
(1) NSAIDs helpful
(2) Pain can be mild to moderate.
(a) Ice to affected area or cold gel mask decreases discomfort and swelling.
c. Elevate head of bed.
d. Continue prophylactic antibiotics and antiviral agents as ordered.
e. Skin care will vary according to physician preference.
4. Education
5. Activity
a. Elevate head of bed.
b. Minimize facial movement to decrease cracking of dead tissue.
6. Skin and dressing care per physician’s preference
a. Avoid picking or scratching of skin.
b. Expect erythema.
c. Expect mild weeping serous fluid.
7. Continue antiviral and antibiotic agents if ordered.
a. Application of antibiotic or hydrocortisone ointments or powders if indicated
8. Observe and report any signs of infection.
9. Encourage patient to call office with any questions on skin care.
10. Instruct patient to avoid sun while skin is healing.
a. When healed, use at least a sun protection factor (SPF) 15 sunscreen.
11. Instruct patient to notify physician if any hyperpigmentation changes are noted.
a. Face will remain pink for 4 to 6 weeks.
b. Camouflage makeup is helpful.
G. Laser resurfacing
1. Purpose
a. To remove signs of aging and give a youthful appearance
b. Removal of facial epidermis and part of superficial dermis to correct skin defects
(1) Acne or depressed scarring
(2) Wrinkles and sun-damaged skin
(3) Irregular skin pigmentation: freckles, liver spots, keratoses
2. Procedure
a. Short blasts of invisible light vaporize a thin layer of epidermis.
(1) CO 2 and erbium:yttrium-aluminum-garnet (Er:YAG) lasers remove the epidermis.
(2) Nd:YAG penetrates more deeply to dermis.
(3) Pulsed-dye laser and intense pulse light both stimulate collagen growth and improve skin’s appearance with less blanching.
b. The deeper the laser penetrates, the more lines and wrinkles will be removed.
c. Penetration that is too deep will cause scarring.
d. Contraindicated in dark-skinned people
3. Perianesthesia care
a. Anesthesia: local or general
b. Provide comfort measures.
(1) Medicate with narcotics as needed.
(a) NSAIDs helpful
(2) Pain can be mild to severe.
(a) Ice to affected area or cold gel mask decreases discomfort and swelling.
c. Elevate head of bed.
d. Continue prophylactic antibiotics and antiviral agents as ordered.
e. Provide nourishment through a straw.
f. Full face resurfacing will cause swelling around mouth.
g. Child’s toothbrush can assist with mouth care.
h. Skin care will vary according to physician preference.
(1) Open technique (no dressing)
(a) Cool saline compresses on the face for first night
(b) On day 1, four times per day, vinegar and water soaks with gentle removal of crusts
(c) Frequent application of petroleum jelly or antibiotic based ointment
(d) Goal is to keep skin soft, pink, and free of crusts.
(e) Soaks continued until crusting ceases (7-10 days), then a moisturizer used
(2) Closed technique
(a) Flexan (biomembrane dressing) applied to the affected area
(i) Any exposed areas treated with the open technique
(ii) Flexan dressing changed according to physician’s preference
(b) N-terface dressing can be applied to affected areas.
(i) Held in place with tube gauze and 4 × 4-inch bandages to absorb drainage
(ii) Soaks may be done through the dressing, and application of petroleum jelly or other lubricant is put on over the dressing.
(iii) Changed according to physician’s preference
4. Education
a. Activity
(1) Elevate head of bed.
b. Skin and dressing care per physician’s preference
(1) Laser resurfacing patients require reassurance and reinforcement of skin care instructions.
(2) Avoid picking or scratching of skin.
(3) Expect erythema.
(4) Expect weeping serous fluid.
c. Continue antiviral and antibiotic agents as ordered.
(1) Application of antibiotic or hydrocortisone ointments or powders if indicated
d. Observe and report any signs of infection.
e. Encourage patient to call office with any questions on skin care.
f. Instruct patient to avoid sun while skin is healing.
(1) When healed, use at least an SPF 15 sunscreen.
g. Instruct patient to notify physician if any hyperpigmentation changes are noted.
(1) Face will remain pink for 4 to 6 weeks.
(2) Camouflage makeup is helpful.
h. Pain management
IX. GENERAL RECONSTRUCTIVE PROCEDURES
| Skin Lesions/Tumor Removal |
| Laceration Repair |
| Scar Revisions |
| Hand Surgery |
| Reduction Mammoplasty |
A. Skin lesions/tumor removal
1. Purpose
a. Removal of skin lesions whether benign or malignant
b. Benign skin lesions
(1) Nevus
(a) Most common skin lesion
(i) Round
(ii) Brown or black
(iii) Flat or raised
(iv) With or without hair
(b) Three types
(i) Intradermal
(ii) Junctional
(iii) Compound
[a] Most need no treatment unless a change is noted or if there is constant irritation.
[b] Junctional may convert to malignant melanoma.
c. Malignant skin lesions
(1) Basal cell carcinoma
(a) Most common skin cancer
(b) May be nodular with an ulcerated center or crusted, dermatitis-like
(2) Squamous cell carcinoma
(a) Begins as a red papule
(b) Progresses to an area that ulcerates, then crusts
(c) Invades underlying tissue
(3) Malignant melanoma
(a) Suspicious lesions with:
(i) Change in size
(ii) Change in color (brown to black)
(iii) Change from smooth to rough
(iv) Irregular borders
(v) Change in sensation
(vi) Satellite lesions
2. Procedure
a. Simple excision
b. Laser therapy
c. Wide excision, possible flap graft, node dissection, radiation, topical chemotherapy, or cryosurgery
3. Perianesthesia care
a. Anesthesia: local or general
b. Provide reassurance, and allow patient to verbalize any fears or concerns regarding body image, diagnosis, and so forth.
c. Elevate extremities.
d. Monitor dressings and assess for hematoma.
e. Position for comfort.
4. Education
a. Teach patient proper dressing and wound care per physician preference.
b. Protect healing incisions from sun.
c. Minimize activity of affected areas for 1 to 2 weeks.
d. Encourage proper follow-up care to monitor for new lesions.
B. Laceration repair and scar revisions (Z-plasty, V-plasty)
1. Purpose
a. Repair skin lacerations (dog bites most common).
b. Remove or reduce scar tissue.
2. Procedure
a. Z-plasty
(1) Use of Z-shaped incision to remove scar tissue
(2) Requires tissue with elasticity
b. V-plasty
(1) Used to repair skin defects
(2) Two triangular flaps of adjacent skin transposed
c. Laser therapy can be used.
d. All procedures can be offered in combination.
3. Perianesthesia care
a. Anesthesia: local or general
b. Wound and dressing assessments to observe for hematoma formation
c. Analgesia as required
d. Minimal activity involving operative site to reduce tension on operative sutures
4. Education
a. Signs and symptoms of infection
b. Activity restrictions
c. Pain management
C. Hand surgery
1. Purpose
a. To correct deformities of the hand
b. To restore function
2. Procedures
a. Ganglionectomy: excision of painful fluid-filled cyst attached to a joint capsule or tendon
b. Palmar fasciectomy: release of flexion contractures of metacarpophalangeal joints
c. Carpal tunnel release: decompression of the carpal tunnel releasing pressure on the median nerve
(1) May be done open or endoscopically
d. Trauma repair: may involve open reduction with internal fixation of fractures or microvascular surgery
3. Perianesthesia care
a. Anesthesia: local, axillary or bier block, general
b. Assess extremity for circulation and neurological status.
c. Include sensory, motor, color, and capillary refill.
d. Apply temporary sling after axillary block.
e. Elevate extremity above level of heart using pillows.
f. Provide adequate analgesia.
g. Consider multimodal therapies.
h. Maintain patency of drains.
4. Education
a. Activity restrictions as directed
b. Maintain elevation of affected limb.
c. Observe for changes in circulation and neurological status.
d. Teach signs and symptoms of infection.
D. Cleft lip and palate
1. Purpose
a. Repair of congenital cleft lip or palate defects
b. Repair of congenital defects from early closure of sutures (craniosynostosis)
c. Repair of congenital maxillofacial deformities
d. Obtain nostril symmetry and Cupid’s bow of upper lip, and repair lip muscle.
(1) Commonly performed when child (rule of 10s)
(a) At least 10 weeks old
(b) Weighs at least 10 lb (4500 g)
(c) Has a hemoglobin of 10 g/dL
2. Procedure
a. May require extensive skeletal reconstruction
b. May be performed in staged procedures
3. Perianesthesia care
a. Anesthesia: general
b. Position side to side, never prone.
c. Avoid crying and restlessness that strain suture lines.
(1) Allow parents to hold the child.
(2) Offer cool compresses to suture areas to reduce swelling and promote comfort.
d. Monitor for bleeding.
(1) Swelling or hematoma at lip
(2) Excessive swallowing
e. Maintain in elbow extension splints to protect incisions.
f. Gentle oral suctioning with soft-tip catheter
g. Provide mist humidifiers if possible to keep airway moist.
h. Maintain elevation of head of bed to decrease intracranial pressure.
i. Place on seizure precautions.
j. Minimize activities that increase intracranial pressure.
(1) Crying in children
(2) Straining
k. Medicate to provide comfort but not enough to mask neurologic symptoms.
4. Education
a. Feeding routines by physician preference
b. Pain management
E. Microvascular surgery
1. Purpose
a. Generally used to replant severed body parts
2. Procedure
a. Tedious anastomosis of severed blood vessels, nerves, and other injured structures
b. Reconstruction of absent digits using transplanted body parts
c. Example: reconstruction of absent finger using patient’s toe
3. Perianesthesia care
a. Procedure-specific care
b. Special attention given to observation of skin color at operative site
(1) White indicates no blood is perfusing to area because of arterial obstruction.
(2) Pink is normal.
(3) Blue indicates hypoxemia in tissues.
(4) Dark blue to black indicates impending tissue infarct from venous obstruction.
c. Often require posttraumatic counseling
4. Education
a. Procedure-specific and site-specific patient education to include but not be limited to activity, pain management, and wound care
F. Genitourinary/gender reassignment
1. Purpose
a. Surgical interventions for “intersex” children
b. Most frequent disorder is genital ambiguity (congenital adrenal hyperplasia).
c. Highly controversial circumstance concerning the appropriate developmental stage to pursue intervention
d. Sex reassignment surgery for transsexual individuals
2. Procedure
a. Surgical restructuring of genitalia
b. Feminizing genitalia involves clitoral reduction and/or vaginoplasty.
c. Penile reconstruction
3. Perianesthesia care
a. Same as any major genitourinary procedure
4. Education
a. Patients and family require extensive counseling and education regarding treatment options and to address any underlying issues of self-esteem and psychological stress.
X. BREAST RECONSTRUCTIVE PROCEDURES
A. Reduction mammoplasty
1. Purpose
a. Removal of excess breast mass to decrease neck, back, and shoulder pain
b. To improve body image and self-confidence
c. May be performed to correct severe asymmetry as in Poland’s syndrome
2. Procedure
a. Surgical excision of redundant breast tissue and skin with recontouring of breast shape
b. Areolar transplantation can be done through free tissue transfer to pedicle.
c. On occasion, areola may be replaced as free graft, resulting in loss of breast-feeding abilities and sensation.
3. Perianesthesia care
a. Anesthesia: general
b. Assess for hematoma.
(1) Palpate superior aspect of pectoralis muscle over the third rib to the clavicle.
c. Drains may be used postoperatively.
(1) Monitor drainage.
(2) Reinforce to keep clothing and bedding dry.
d. Treat pain.
(1) Usually described as moderate
(2) May need IV narcotic on emergence
(3) Control with strong narcotics at home (e.g., oxycodone for first day or two).
e. Surgical bra or compression dressing applied postoperatively to maintain new breast contour and decrease fluid accumulation; compression bra
(1) Tube gauze over bra assists in holding reinforcement ABD pads in place.
f. Prevent and treat nausea and vomiting.
(1) Vomiting can cause hematoma formation.
g. Provide aggressive fluid replacement for blood loss.
(1) Usual blood loss, 400 mL
(2) Replace with crystalloid or colloid as needed.
(3) Some patients may require hospitalization if symptomatic after blood loss and fluid replacement.
4. Education
a. Observe for hematoma formation.
b. Activity
(1) No heavy lifting or strenuous activity for 1 month
(2) No pushing self up with arms
(3) Instruct patient and caregiver on how to make position changes.
c. Usually a return appointment in 24 hours for drain removal
d. Steristrips or sutures may be removed in 1 week.
e. Compression bra for 2 to 3 weeks
(1) Demonstrate how to reinforce dressing.
B. Breast reconstruction
1. Purpose
a. Breast reconstruction after wide local excision and mastectomy for breast cancer to achieve breast symmetry
b. Repair of traumatic injury
c. Repair of defects from cancer treatment
2. Procedure
a. Insertion of breast implants
(1) Creation of a pocket space under remaining breast tissues into which a soft prosthetic breast implant can be placed
(2) Pocket can be created by means of inflatable tissue expander used to gradually increase the volume of pocket space to receive prosthesis.
b. Transplantation of skin, muscle, and blood supply from autologous donor site to repair congenital or acquired tissue defects
(1) Flaps or tissue transfer
(a). At time of procedure, absence of infection required at recipient site
(b) Donor muscle or skin for flap selected to appropriately fit defect and minimally impact patient’s activity and function after removal
(i) Muscle size will decrease at recipient site after denervation.
(c) Pedicle flap (delayed) selected to reach defect comfortably
(d) Preparation of recipient vessels
(i) Devitalized tissue carefully removed
(ii) Selection of recipient blood vessels that have been minimally impacted by trauma of defect
(e) Anastomosis of vessels
(i) Avoid twisting of vessels.
(ii) Vessels must be delicately handled.
(iii) Use of heparin-containing irrigating solutions
(2) Types of flaps
(a) Delayed flap
(i) Donor tissue attached to recipient site without being separated from its blood supply
(ii) Remains attached to donor site (by pedicle) until recipient circulation is established
(b) Local flaps
(i) Moved from location immediately adjacent to defect
(ii) Maintains blood supply from original source
(c) Free flap
(i) Entire tissue and blood supply detached from donor site
(ii) Requires prolonged microsurgery (6-12 hours)
(3) Common sources of flaps
(a) Skin flaps
(i) Consists of skin and subcutaneous tissue
(ii) May be placed to a remote area by means of pedicle
(iii) May be advanced into a defect close to donor site or moved at a pivotal point and rotated into tissue defect
(iv) Sources
[a] Temporalis fascia: may be used to cover dorsum of hand or foot
[b] Lateral forearm: skin and fascia used to cover areas requiring a thicker coverage
[c] Omentum: for areas that require pliable tissue (e.g., frontal sinuses)
(b) Muscle and myocutaneous flaps
(i) Movement of muscle with or without skin to cover defect
[a] Local transfer
[b] Free transfer
(ii) May require additional skin grafting at recipient site
(iii) Sources
[a] Latissimus dorsi
[b] Pectoralis major
[c] Tensor fascia lata
[d] Rectus abdominus
[e] Gluteus maximus
[f] Gracilis
3. Perianesthesia care
a. Anesthesia: general
b. Monitor for and prevent factors that promote vasospasm and thrombosis.
(1) Hypothermia
(a) Results in vasoconstriction
(b) Arterial flow compromised
(c) Use warming blankets, lights, warmed fluids, increased room temperature.
(2) Hypotension
(3) Hypovolemia
(a) Large blood loss may have occurred.
(b) Replacement with crystalloids and colloids
(c) Excessive red blood cell replacement may raise hematocrit, causing sluggish capillary flow.
(4) Agents that increase vasoconstriction and vasospasm (e.g., nicotine, caffeine)
c. Maintenance of normal body temperature
(1) Warmed IV and irrigating fluids
(2) Room temperature regulation
(3) Warming blankets
d. Assess condition of flap.
(1) Skin temperature
(a) Should be warm to touch
(b) Coolness reflects reduced blood flow.
(2) Capillary refill
(a) Blanching within 2 seconds
(b) Rapid blanching may indicate venous engorgement.
(c) Delayed blanching may indicate arterial insufficiency.
(d) Arterial and venous flow may be obtained by Doppler ultrasonography and are marked by surgeon with a marker or suture.
(e) Venous congestion frequently results in failure before arterial insufficiency.
(3) Color
(a) Normally white or gray immediately postoperatively
(b) Increasingly pale flaps suggest arterial insufficiency.
(c) Bluish color suggests venous congestion.
(d) Color of flap may be different from other skin in recipient area if obtained from tissue far removed.
(4) Edema
(a) Slight swelling expected
(b) Significant swelling may indicate hematoma or venous congestion.
(5) Monitor drainage from drains every 30 to 60 minutes.
(a) Gentle continuous suction
(b) Greater than 50 mL/hr is problematic.
(6) Monitor muscle donor site for bleeding.
(7) Antiplatelets or anticoagulants may be used to decrease platelet aggregation and thrombosis.
(a) Low–molecular weight dextran
(b) Heparin drip
(c) Aspirin
(8) Flap failure usually caused by inadequate circulation or infection
(a) Prevent patient from lying on operative site.
(b) Prevent compression of operative site by blankets.
(9) Patient care for patient with tissue expander or prosthetic implant same as augmentation mammoplasty
(a) When expansion complete:
(i) Prosthesis inserted
(ii) Nipple reconstruction done
(iii) Nipple tattoo or graft reconstruction
(b) Pain can be severe with initial insertion of expander.
(c) Anesthesia: general
(d) Psychological support crucial because patients have had multiple procedures and cancer diagnosis
4. Education
a. Observe for hematoma formation.
b. Report deflation of tissue expander.
(1) Could mean rupture
c. Limit arm activity for 1 month.
d. Frequent appointments required for inflation of expander with saline
XI. COMMON SURGICAL BURN PROCEDURES
A. Escharotomy
1. Indicated for circumferential full-thickness burns
a. Burn eschar acts as tourniquet.
(1) Decreases arterial flow
(2) Causes venous congestion
b. Common sites are extremities or trunk.
2. Linear incisions placed extending through burn eschar down to superficial fascia, releasing constriction
3. May be performed with or without anesthesia
a. Nerve endings in eschar dead
b. Premedication to relieve anxiety and discomfort
B. Excision and skin grafting
1. Goal is to restore function and maximize cosmetic appearance.
a. Performed in burns with limited or inability to heal
b. May require grafting months to years after injury to revise scar tissue
c. Principles of grafting similar for burns and nonburn wounds requiring skin coverage
2. Nonviable tissue removed
3. Graft sources
a. Autograft
(1) Patient’s own skin used
(2) Permanent
b. Cultured autologous human epithelium
(1) Biopsy of patient’s skin obtained
(2) Skin grown in petri dish and then grafted to patient
c. Homograft (allograft)
(1) Skin obtained from another human
(2) Fresh cadaver
(a) Provides a temporary covering to excised tissue awaiting permanent grafting
(b) May be placed over a widely meshed autograft to promote graft take
(c) Patient will eventually reject.
(3) Processed human dermis (AlloDerm)
(a) Donated skin processed to remove components that cause rejection
(i) Epidermis removed
(ii) Cells that contain antigen targets for rejection removed
(iii) Tissue (dermal matrix) freeze-dried for storage
(b) Procedure
(i) Wound excised
(ii) AlloDerm applied to wound bed
(iii) Thin autograft applied over AlloDerm
d. Skin substitutes
(1) Integra
(a) Bilaminate skin substitute
(i) Dermal analogue of collagen fibers
(ii) Epidermal analogue is Silastic membrane.
(b) Applied to excised wound
(i) Dermal analogue develops vasculature.
(ii) Silastic membrane removed after dermal vascularity established (approximately 2 weeks)
(iii) Thin autograft applied after Silastic membrane removed
(c) Requires a two-step process
(i) Excision and application of Integra
(ii) Removal of Silastic membrane and autograft
(2) Biobrane
(a) Synthetic polymer dressing
(b) Porcine collagen base with nylon covering
(c) Placed over excised tissue
(d) Patient’s dermis binds with collagen base.
(e) Biobrane removed after dermal healing
(f) Patient must have capacity for dermal regeneration.
(g) May be placed over donor sites
e. Heterograft (xenograft)
(1) Tissue from another species, usually pigskin
(2) Temporary covering over excised wounds
C. Primary closure
1. May be used for small burns
2. Burn tissue excised and closed primarily
XII. INTRAOPERATIVE CONSIDERATIONS FOR THE BURN PATIENT
A. Surgical concerns
1. Minimize physiological stress experienced by patient.
a. Limit operative time to 2-hour to 3-hour sessions.
b. Limit excision to 20% of total body surface at any one operative session.
2. Selection of donor sites
a. Preferred sites: thighs, buttock, abdomen, back, scalp
b. Best color match if skin obtained from area near burn
3. Types of grafts
a. Split-thickness skin graft
(1) Donor skin contains epidermis and part of dermis.
(2) Thickness: 0.012-inch
(3) Graft “takes” as capillaries grow in from granulation bed into graft (begins to occur after 48 hours).
(4) Donor site reepithelializes in 10 to 14 days and may be ready as donor site again in 21 days (scalp donor sites may heal in 7 days).
b. Full-thickness graft
(1) Entire epidermis and dermis used as donor
(2) Used to cover deep defects, tendons, bone
(3) Requires split-thickness skin graft on donor area from which full-thickness skin was removed
(4) Less hyperpigmentation and contractures than with split-thickness skin graft
c. Mesh graft
(1) Split-thickness skin graft in which donor skin is passed through mesher to produce slits in skin
(2) Allows for donor skin to be stretched covering large area
(a) May be meshed 1.5 to 3 times original size
(b) Useful in large burns
(3) Meshing helps prevent fluid or blood from accumulating under graft, which prevents “take.”
(4) Less cosmetically perfect than sheet graft
d. Sheet graft
(1) Split-thickness skin graft placed on wound without meshing
(2) Provides better cosmetic result, especially for hands, face, and neck
(3) Fluid and blood can accumulate under graft, affecting “take.”
4. Burn wound excision
a. Tangential (sequential) excision
(1) Sequential removal of tissue until viable dermis reached
(2) Provides optimal functional and cosmetic result
(3) Large blood loss may occur.
(4) May be difficult to determine endpoint of excision—too much or too little may be excised
b. Fascial excision
(1) Used in deep full-thickness burns that may extend into fat or underlying tissues
(2) Tissue sharply dissected to fascia
(3) Blood loss less than if tangentially excised
(4) Easier to determine endpoint of excision
(5) Risk of injury to nerves, joints, tendons
(6) Results in cosmetic defects
5. Control of bleeding
a. Patient may have considerable blood loss.
b. Controlled with thrombin, epinephrine soaks, electrocautery
c. Hemostasis must be obtained before graft is placed.
6. Factors promoting graft “take”
a. Hemostasis
b. Graft secured and immobilized
c. Prevention of infection
d. Good nutrition
B. Anesthesia concerns
1. Anesthetic agents
a. Pharmacokinetics may be altered because of physiological changes that occur after major burn injury.
b. Serum protein levels decrease, making agents that bind to albumin more pharmacologically active.
c. Narcotic anesthesia amounts may be high because of developed tolerance.
d. Amount of cardiac depression must be weighed if inhalation agents are used.
e. Increased sensitivity to depolarizing neuromuscular blocking agents occurs and may result in hyperkalemic response.
(1) Succinylcholine use contraindicated because of hyperkalemic response
f. Hyposensitivity to nondepolarizing neuromuscular blocking agents
2. Ventilatory needs
a. Intubation may be difficult because of burns of face and neck or limited oral mobility, requiring use of fiberoptic bronchoscope.
b. Hypermetabolic response results in increased oxygen consumption and carbon dioxide production.
c. Chest wall compliance may be decreased if chest burns are present.
d. Ventilation-perfusion mismatches may occur with pulmonary injuries.
e. Patient may need increased minute ventilation because of hypermetabolic state and positive end-expiratory pressure.
f. Monitor oxygen saturation and end-tidal carbon dioxide.
3. Prevention of hypothermia
a. Room temperature maintained at 85° F
b. Use of warming blankets and warmed fluids
c. Temperature monitoring
d. Warmed inspired gases
4. Maintaining hemodynamic stability
a. May be prone to hypotension because of position changes as donor skin is obtained and burn wound prepared
b. Fluid loss through evaporation and bleeding
(1) Replacement with red blood cells and fresh frozen plasma
(2) Crystalloids to maintain adequate urine output without giving excess salt
5. Fluid resuscitation criteria
a. Calculated fluid requirements for first 24 to 48 hours after injury
b. Thermal injuries uncommonly taken to operating room during burn shock period (first 24-48 hours)
(1) Early excision after 24 hours to begin wound coverage to decrease metabolic rate and decrease wound infection
c. Calculated requirements (Parkland formula)
(1) Over first 24 hours: 4 mL/kg per TBSA percent of injury
(a) One half of calculated requirements given over first 8 hours from time of injury
(b) One half of calculated requirements given over next 16 hours
(2) Fluids adjusted to maintain urinary output
(a) Adult: 0.5 to 1 mL/kg per hour
(b) Children: 1 to 2 mL/kg per hour
d. Fluids used
(1) Isotonic crystalloid
(a) Normal saline
(b) Lactated Ringer’s
(2) Hypertonic saline may be used.
(a) Increases osmotic pull back to intravascular space
(b) Decreases total fluid requirements and assists to minimize edema formation
(3) Colloids rarely used in first 12 hours after burn injury because of increased capillary permeability
(4) Care taken to avoid pulmonary edema and worsening of fluid shifts from overaggressive fluid resuscitation
e. Electrical injury fluid requirements
(1) More difficult to estimate fluid needs
(2) Injury greater internally than what is seen externally
(3) Calculate on basis of Parkland formula.
(4) Adjust fluids to maintain urinary output of 75 to 100 mL/hr in adults or 2 to 3 mL/kg per hour in children.
(5) Add sodium bicarbonate to alkalinize urine, promoting myoglobin excretion.
(6) Administer mannitol to increase urinary flow, promoting myoglobin excretion.
f. Inadequate fluid resuscitation is primary cause of death in first 24 to 48 hours after injury.
XIII. POSTOPERATIVE CONCERNS FOR THE BURN PATIENT
A. Airway and ventilatory needs
1. Upper airway injuries
a. Caused by heat injury to oronasopharynx and vocal cords
b. Swelling usually peaks 48 hours after injury.
c. Edema may lead to obstruction.
d. Intubation performed early, often prophylactically
e. If patient is extubated postoperatively, observe for signs of obstruction (e.g., stridor, tachypnea, increased work of breathing, low arterial oxygen saturation [Sa o2], low mixed venous oxygen saturation [Sv o2]).
f. Secure endotracheal tube.
(1) Use ties in patients with face burns.
(2) Tape will not adhere.
(3) Avoid pressure on burned nose or ears.
(4) Monitor ties for constriction as facial swelling increases.
2. Lower airway injuries
a. Injuries below glottis caused by chemical irritants released from smoke
b. Lower airway damage results in:
(1) Increased airway irritability, laryngospasm, bronchospasm
(2) Bronchiolar edema and impaired airway flow
(3) Increased mucus production caused by chemical irritants
(4) Damage to epithelial lining of bronchial tree and alveolar cells
c. Management considerations
(1) Frequent assessment of respiratory function and airway patency
(a) Respiratory effort
(b) Chest wall expansion and symmetry
(c) Monitor oxygenation with pulse oximeter and arterial blood gases.
(d) Monitor end-tidal CO 2
(2) Assess need for bronchodilator therapy.
(3) Assess chest expansion.
(a) Constriction of nonexcised chest burns
(b) Constriction of chest dressings
(4) Deep breathing and coughing to facilitate mucus mobilization
(5) Provide for oxygen and ventilatory needs.
(a) May need increased minute ventilation (rate or tidal volume or both) because of hypermetabolic state
(b) Humidified oxygen
(c) Prevent oxygen administration device from applying pressure if grafts have been placed on face or neck.
B. Circulatory function
1. Blood and fluid loss may be significant.
2. Monitor for signs of hypovolemia.
a. Tachycardia
b. Decreased blood pressure and presence of pulsus paradoxus
c. Delayed capillary refill
d. Monitor urinary output.
(1) Maintain 30 to 50 mL/hr in adults.
(2) Maintain 1 to 2 mL/kg per hour in children.
3. Provide fluid replacement.
a. Isotonic or hypertonic crystalloids
b. Colloids: red blood cells, fresh frozen plasma, albumin
4. Monitor circulatory function distal to burn.
a. Distal to escharotomy sites every 15 to 30 minutes
b. Assess circulatory compromise caused by constricting dressings or splints.
c. Assessment
(1) Pulses
(2) Capillary refill
(3) Movement and sensation
(4) Color
C. Infection
1. Thorough hand washing and gloves are essential.
2. Prevent cross-contamination with other patients.
3. Isolation precautions, including gown, mask, and gloves, may be necessary in large burns.
4. Aseptic wound technique
5. Frequent change of invasive catheters
D. Temperature control
1. Assess body temperature every 30 minutes.
2. Warm fluids and blood products before infusion.
3. Use heat shields or warming blankets.
4. Adjust room temperature to 75° F to 85° F.
5. Monitor for ST-segment changes caused by myocardial ischemia.
E. Wound care
1. Monitor graft and donor sites for bleeding.
a. Grafts will fail if blood collects beneath them.
b. Dressings usually not changed for first few days
2. Monitor status of sheet grafts that do not have dressing.
a. Assess for fluid and blood collection under graft.
(1) Aspiration of fluid using syringe and small-gauge needle
(2) Removal of fluid by “rolling” fluid to edges of graft with cotton-tipped applicator
b. Avoid pressure or shearing.
c. Antimicrobial ointment may be applied to edges and seams of graft.
3. Maintain joint immobility if graft is over joint.
4. Elevate grafted extremities to minimize edema and promote venous return.
F. Pain control
1. Pain usually more severe at donor site than at grafted areas
2. May have high analgesic needs because of previous narcotic needs during wound care
3. IV administration preferred over intramuscular in large burns because of poor absorption
4. Avoid aspirin-containing products.
G. Emotional support for patient and family
1. Patient and family must deal with change in physical appearance from first day after injury.
2. Ongoing emotional support required
a. Change in physical appearance
(1) Long-term results may be uncertain.
(2) Must begin to adjust to fact that even with the best cosmetic results, patient will never look the same again
b. Possible changes in function if severe burns of extremities, hands, feet, face
3. Surgical procedure may be the first or one of many.
a. Expectations of each may differ.
b. May view regrafting as a setback because of graft failure or poor cosmetic result
4. Provide support appropriate to stage of adjustment that patient or family is experiencing.
5. Use additional health care workers to assist in support (e.g., child life specialists, clergy, mental health practitioners, social worker).
6. Priorities of care: life, limbs, looks (in that order)
H. Discharge instructions for the ambulatory skin graft patient
1. Maintain dressing dry and intact.
a. Donor site dressing may exhibit some bloody drainage.
b. Avoid getting dressings wet.
2. Keep grafted area immobile.
a. Avoid activities that would cause sheer.
b. Grafts over joint must remain immobile—may have splints in place.
c. Reinforce weight-bearing status or crutch walking for lower extremity grafts.
d. Elevate grafted extremity to limit edema.
3. Pain management
a. Reinforce that donor site may be more painful.
b. Instruct on use of prescribed analgesia.
4. Notify physician of:
a. Temperature >38.5° C (101.3° F)
b. Numbness, paresthesia of grafted extremity
c. Pain that is not controlled by analgesia
d. Bleeding of graft or donor site
5. Reinforce follow-up instructions.
a. Dressing usually changed and graft evaluated 3 to 5 days after grafting
BIBLIOGRAPHY
1. American Society of Plastic Surgeons, 2006 Quick facts: Cosmetic and reconstructive plastic surgery trends. ( 2008) ; Available at:http://www.plasticsurgery.org/media/statistics/loader.cfm?url; = /commonspot/security/getfile.cfm&PageID = 23625″>www.plasticsurgery.org/media/statistics/loader.cfm?url = /commonspot/security/getfile.cfm&PageID = 23625. Accessed December 10.
2. Bosch, J.A.; Engeland, C.G.; Cacioppo, J.T.; et al., Depressive symptoms predict mucosal wound healing, Psychosom Med 69 (7) ( 2007) 597–605.
3. Bowser, A., Lipo innovations: Female breast reduction, ‘plasty’ alternatives expand, Dermatology Times 26 (2) ( 2005) 84.
4. Bryant, R., Early pioneer describes autologous fat transfers, Dermatology Times 26 (2) ( 2005) 85–86.
5. Dell, D.D.; Weaver, C.; Kozempel, J.; et al., Recovery after transverse rectus abdominis myocutaneous flap breast reconstruction surgery, Oncol Nurs Forum 35 (2) ( 2008) 189–196.
6. Dittmann, M., Plastic surgery: Beauty or beast?Monitor on Psychology 36 (8) ( 2005) 30.
7. Dugas, B., Choosing the right peel for your patient, Plast Surg Nurs 27 (2) ( 2007) 80–84.
8. Figueroa-Haas, C.L., Effect of breast augmentation mammoplasty on self-esteem and sexuality, Plast Surg Nurs 27 (1) ( 2007) 16–36.
9. Guttman, C., Survey: Chemical peels remain mainstay in dermatologic surgery armamentarium, Dermatology Times 29 (1) ( 2008) 72.
10. Hackenschmidt, A., Burn trauma priorities for a patient with 80% total body surface area burns, J Emerg Nurs 33 (4) ( 2007) 405–408.
11. Hainsworth, T., Risks and benefits associated with cosmetic procedures, Nurs Times 102 (11) ( 2006) 23–24.
12. Hill, O.; White, K., Exploring women’s experiences of TRAM flap breast reconstruction after mastectomy for breast cancer, Oncol Nurs Forum 35 (1) ( 2008) 81–88.
13. Hilton, L., In search of the perfect filler, Dermatology Times 25 (8) ( 2004) 39–48.
14. Iverson, R.E.; Lynch, D.J., ASPS Task Force on Patient Safety in Office-based Surgery Facilities: Patient safety in office-based surgery facilities: II. Patient selection, Plast Reconstr Surg 110 (7) ( 2002) 1785–1790.
15. Myers, B.A., Wound management: Principles and practice. ed 2 ( 2008)Prentice Hall, Upper Saddle River, New Jersey.
16. Nash, K., Liposuction: Safety paramount; not every patient a candidate, Dermatology Times 28 (2) ( 2007) 10–11.
17. Rasberry, C.N., Battling body image: Confessions of a health educator, J Am Coll Health 56 (4) ( 2008) 423–426.
18. Robles, T.F., Stress, social support, and delayed skin barrier recovery, Psycosom Med 69 (8) ( 2007) 807–815.
19. Sattler, G., Advances in liposuction and fat transfer, Dermatol Nurs 17 (2) ( 2005) 133–139.
20. Sicoutris, C.P.; Homes, J.H., Fire and smoke injuries, Crit Care Nurs Clin North Am 18 (3) ( 2006) 403–417.
21. Sobralske, M., Primary care needs of patients who have undergone gender reassignment, J Am Acad Nurse Pract 17 (4) ( 2005) 133–138.
22. Venes, D., Taber’s cyclopedic medical dictionary. ed 20 ( 2005)FA Davis, Philadelphia.
23. Wagner, K.D.; Johnson, K.L.; Kidd, P.S., High acuity nursing. ed 4 ( 2005)Prentice Hall, Upper Saddle River, New Jersey.
24. Warner, D.O., Perioperative abstinence from cigarettes: Physiologic and clinical consequences, Anesthesiology 104 (2) ( 2006) 356–367.
25. Zuelzer, H.B.; Baugh, N.G., Bariatric and body-contouring surgery: A continuum of care for excess and lax skin, Plast Surg Nurs 27 (1) ( 2007) 3–13.




