CHAPTER 4. Evidence-Based Practice and Nursing Research
Susan Jane Fetzer
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Define evidence-based practice, nursing research, and research utilization.
2. Rank the strength of their contribution and list the major sources of evidence used to develop clinical practice guidelines.
3. Describe the link between research and the development of evidence-based practice.
4. Describe the nurse’s role in protection of patients from unethical or harmful research.
5. Identify the components of a research proposal.
6. Differentiate the research process from the quality assurance process.
7. Identify three areas of perianesthesia nursing practice that are in need of research.
8. Identify three methods of applying ambulatory perianesthesia research in practice.
I. DEFINITION OF EVIDENCE-BASED PRACTICE (EBP)
A. Problem-solving approach to clinical decision-making
B. Research utilization
1. Is one part of EBP
2. Assessment of single research report
3. Research study results will suggest change or support existing practice.
C. Requires search for best and latest evidence
1. Scientific evidence
2. Experiential evidence of patient and provider
D. Four components
1. Analysis of best research
2. Integrating clinical expertise
3. Integrating patient values and cultural needs
4. Integrating preferences of patient, family, and community
E. Approach is systematic and rigorous.
F. Requires synthesis of quality of evidence
G. Conscientious integration of evidence in practice
II. GOAL OF EBP
A. Implement effective nursing interventions
B. Provide quality cost-effective care
C. Reduce variations in practice
D. Improve patient outcomes
III. STIMULI FOR EBP INITIATIVES
A. Unusual or low-frequency clinical practice
B. Indicated when outcome of care differs between similar patient situations
C. Reference for developing nursing policies and procedures
IV. STEPS OF EBP
A. Assess need for practice change; formulate a clinical question.
1. Develop a problem-focused clinical question.
a. Derived from recurrent clinical problem
b. Encouraged by a quality improvement (QI) recommendation
c. Stimulated by a benchmarking report
2. Develop a knowledge-focused clinical question.
a. New practice is identified.
(1) Recently published research
(2) Scientific paper at conference
(3) Published clinical practice guideline
b. Unit is interested in maintaining competency.
3. Clinical question developed using PICO question format
a. P—population of interest
b. I—intervention of interest
c. C—comparison intervention
d. O—outcome
e. Example: in patients undergoing bowel resection [P], does prewarming to 38° C [I], compared with no prewarming [C], result in less postoperative hypothermia [O]?
B. Collect evidence.
1. Sources of evidence
a. Meta-analysis
(1) Collection of multiple quantitative studies on the research question
(2) Sample for analysis composed of the research studies identified
(3) Application of statistical techniques to combine results into one data set
(4) Determines strength of relationship between variables
(5) Highest level of evidence to determine practice effectiveness
(6) Example: a meta-analysis of studies of nurses’ job satisfaction
b. Systematic reviews
(1) Collection of evidence related to specific clinical issue
(2) Quantitative studies with similar methodology
(3) Rigorous search designed to ensure complete database
(4) Summary of findings provided
(5) Highest level of evidence to determine practice effectiveness
(6) Examples:
(a) Cochrane Database of Systematic Reviews
(b) Joanna Briggs Institute
c. Integrative literature reviews
(1) Similar to systematic review
(2) Includes qualitative and quantitative studies
(3) Draws narrative conclusions from summary of findings
(4) Provides understanding of state of the science
(5) Example: the relationship between nurse educational level and patient safety
d. Metasummary
(1) Synthesis of multiple qualitative studies
(2) Provides narrative understanding of selected phenomenon
e. Metasynthesis
(1) Similar to metasummary
(2) Develops a new theory or framework for topic
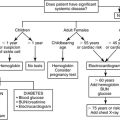
f. EBP guidelines
(1) General outline for specific course of action
(2) Systematically developed
(3) Recommendations supported by evidence
(4) Developed by experts who have evaluated evidence
(5) Goal is to translate evidence from research evaluations into practice
(6) Formats of guidelines
(a) Decision trees
(b) Algorithms
(c) Protocols
(d) Clinical pathways
(7) Sources of guidelines
(a) National Guideline Clearinghouse
(b) Agency for Healthcare Research and Quality
(c) PeriAnesthesia guidelines
(i) Normothermia
(ii) Postoperative nausea and vomiting
(iii) Pain and comfort
g. Original clinical studies
(1) Located through databases or indexes
(a) Cumulative Index to Nursing and Allied Health Literature
(b) PubMed
(2) Types of clinical studies
(a) Randomized controlled clinical trial (RCT)
(b) Quantitative studies
(i) Quasi-experimental
(ii) Correlational
(iii) Descriptive
(c) Qualitative studies
C. Evidence appraisal
1. Evidence appraised (critiqued) based on criteria
a. Merit
b. Feasibility
c. Utility
2. Evidence rated based on strength and quality
3. Strength of evidence
a. Level I—meta-analysis of multiple controlled studies; systematic review, evidence-based clinical guideline
b. Level II—single, well-designed RCT
c. Level III—quasi-experimental study, not randomized, single group
d. Level IV—well-designed, nonexperimental study: correlation, descriptive, qualitative
e. Level V—case report, program evaluation data
f. Level VI—expert opinion, nationally known authorities
4. Quality of evidence
a. A—well-designed study
b. B—observational study or controlled trials with less consistent results
c. C—dramatic results but lacks controlled trial, evidence not consistent
d. D—study has major flaw, findings suspect
5. Evidence summarized
a. Narrative summary
b. Table of evidence
D. Integrate evidence into practice recommendations.
1. Practice guidelines
a. General outline for specific course of action
2. Practice protocols
a. Specific actions for direct application of an intervention
E. Implement practice change.
1. Pilot study or demonstration project
2. Evaluate need for change.
a. Adopt a practice change based on evidence.
b. Adapt a practice change based on evidence and setting characteristics.
c. Reject a practice change for nonapplicability to the situation.
3. Rogers’ Theory of Diffusion of Innovation
a. Guide for implementing changes in practice based on research
b. Five-stage process
(1) Knowledge—first awareness of innovation
(2) Persuasion—attitude formation toward innovation
(3) Decision—determination to adopt or reject innovation
(4) Implementation—using innovation in practice
(5) Confirmation—reconsider adoption or rejection of innovation
F. Evaluate and monitor practice change.
1. QI monitoring
2. Conduct an original research study.
V. DEVELOPING AN EVIDENCE-BASED CULTURE
A. Creation of environment that allows questions of current practices and actions
B. Policies and procedures supported by literature citations
C. Research committee is active.
1. Inservice staff
a. Promote positive attitude toward EBP.
b. Methods of critical appraisal
c. Accessing databases
d. Steps of the research process
e. Grading evidence
2. Facilitate journal clubs.
3. Change agents for EBP
a. Champion a positive attitude toward research.
b. Identify clinical practice questions.
D. Resources needed to support EBP culture
1. Time to reflect on practice
2. Time to access and review evidence
3. Consultants with research expertise
4. Access to databases
5. Authority to implement change
VI. DEFINITION OF NURSING RESEARCH
A. Research: process of applying the scientific method designed to develop or contribute to generalizable knowledge
B. Scientific method: controlled, systematic process for conducting studies in which data are collected under constant conditions to decrease error so that all data are collected in the same manner
C. Nursing research: process of applying the scientific method to answer questions about nursing education, nursing practice, and nursing administration
VII. GOALS OF PERIANESTHESIA NURSING RESEARCH
A. Maximize perianesthesia patient outcomes from nursing interventions.
B. Validate a unique body of perianesthesia knowledge that impacts perianesthesia nursing.
C. Maximize the effectiveness and efficiency of perianesthesia nursing care delivery.
VIII. OBJECTIVES OF PERIANESTHESIA NURSING RESEARCH
A. Validate interventions used by perianesthesia nurses.
B. Uncover perianesthesia phenomena not previously realized.
C. Develop and test theories able to explain, predict, and control perianesthesia nursing practice and patient outcomes.
D. Substantiate the unique contribution of perianesthesia nurses as health care providers.
IX. DEVELOPING AND PLANNING A RESEARCH STUDY
A. Phases of a research study
1. Proposal development
2. Institutional review board (IRB) approval
3. Data collection
4. Analysis
5. Communication of findings
B. Proposal development
1. A proposal is the plan the researcher intends to implement to solve the research problem by answering the research question or supporting the research hypothesis.
2. Proposal precedes the implementation of a research study
a. Assists the researcher to think through all steps in a study so nothing is missed
b. Allows the researcher to make changes before investing time and money in procedures that may not be appropriate
c. Encourages researcher to plan study with such clarity that it can be replicated (e.g., reproduced with another group)
d. Provides an opportunity for peer review that allows constructive criticism from others who are knowledgeable about topic and research process for purpose of improving the study
e. Proposal reviewed by the human subjects committee or IRB before data collection
X. COMPONENTS OF A RESEARCH PROPOSAL
A. Introduction and problem statement (Box 4-1)
1. Introduction: defines problem and provides background information so reader can understand why study needs to be conducted
2. One to two paragraphs at the beginning of a research proposal that introduces the topic to the reader
3. Problem statement: description of a dilemma or situation
a. Dilemma or situation requires resolution by scientific inquiry and the development of new knowledge.
b. Situation has not been satisfactorily resolved by past research studies.
c. Dilemma exists because of a knowledge gap in the nursing literature.
d. Example of perianesthesia nursing introduction and problem statement:
4. Perianesthesia topics that can be developed into research problems
a. Preoperative examples:
(1) Effectiveness of take-home preoperative video on patient compliance with preoperative regimen
(2) Completeness of data provided by patient for preoperative database
(3) Appropriate scheduling of preadmission visits
b. Phase I examples:
(1) Role of registered nurse during conscious sedation
(2) Speed of patient rewarming on pain management
(3) Role of PACU visitation on patient, family, and staff
c. Phase II examples:
(1) Validity of discharge criteria for regional anesthesia patients
(2) Effectiveness of postoperative telephone calls in measuring patient outcomes
(3) Use of bladder scanner to determine postoperative voiding necessity
BOX 4-1
EXAMPLE OF A PERIANESTHESIA NURSING INTRODUCTION AND PROBLEM STATEMENT
Pain is a common problem in the post anesthesia care unit (PACU) resulting in negative consequences for the patient. Length of stay in the PACU contributes to total cost of the surgical experience. Unrelieved pain is one of the most common causes of delayed stay in the PACU, therefore, contributing to higher cost.
Traditionally medications have been used to provide pain relief in the PACU. The effect of medications differs from person to person because of great variability in personal responses to pain. Experts have suggested that a combination of pharmaceutical and nonpharmaceutical therapies have the greatest potential for providing optimal pain relief. Music and quiet conversation by staff have the potential to provide pain relief and improve patient satisfaction with the PACU experience. The effect of music with noise control in the PACU on pain reports is not known.
B. Purpose statement
1. Provides a direction the researcher will take to solve the research problem
2. Includes the extent of the research project and the clinical context in which the researcher is interested
3. Presents one sentence that clarifies and provides the specific reason for the research
4. Example of perianesthesia nursing purpose statement:
a. The purpose of the study was to investigate the effect of soothing music and control of noise on patients’ perceived pain in PACU.
5. Perianesthesia purpose statements related to research problems
a. Preoperative examples:
(1) The purpose of the study is to determine the effectiveness of a take-home preoperative video on patient compliance with the preoperative regimen.
(2) The purpose of the study is to describe the completeness of the data provided by the patient for the preoperative database.
(3) The purpose of the study is to determine the most appropriate scheduling of preadmission visits.
b. Phase I examples:
(1) The purpose of the study is to describe the role of the registered nurse during moderate sedation and analgesia.
(2) The purpose of the study is to determine the relationship between the speed of patient rewarming and perceived pain.
(3) The purpose of the study is to determine the difference between scheduled and open PACU visitation on patient satisfaction.
c. Phase II examples:
(1) The purpose of the study is to determine the validity of temperature as a discharge criterion for regional anesthesia patients.
(2) The purpose of the study is to determine the effectiveness of postoperative telephone calls in measuring patient satisfaction.
(3) The purpose of the study is to determine the relationship between bladder scan volume and postoperative voiding urgency after spinal anesthesia.
C. Review of literature
1. Presents and clarifies what has been previously written or studied on the proposed topic
2. The researcher seeks out available solutions to the research problem in the existing literature before planning the study.
3. Includes a written summary of previous research related to the study problem and purpose
4. Provides the reader with a comprehensive background on the research topic
5. Types of literature
a. Research-based literature—qualitative or quantitative research studies that follow steps of the scientific method found in nursing and nonnursing journals
b. Theoretical—opinions or empirical experience articles found in nursing and non-nursing journals
c. Research-based literature preferred
6. Literature review breadth and depth
a. Breadth—wide variety of topics because area of research not well defined
b. Depth—focused review on single concept when area of research is extensively documented in existing literature
D. Research question
1. Study purpose narrowed down further to focus on one or two research questions and/or hypotheses
2. Research question
a. Definition: an interrogative statement posed by the researcher when little is known about the topic
b. Used when there is insufficient current research to predict a relationship between two characteristics (variables) or an effect of one variable on another
c. Components include the group to be studied and the characteristics (variables) under investigation.
3. Perianesthesia nursing research questions
a. Preoperative examples:
(1) What preoperative information do cataract patients retain?
(2) How do parents describe the effect of pediatric preoperative tours on the child’s behavior?
(3) What are the characteristics of patients who do not comply with fasting limits (e.g., nothing by mouth [NPO]) preoperatively?
b. Phase I examples:
(1) What are the educational characteristics of RNs administering conscious sedation?
(2) What is the older nurse’s experience of being on-call?
(3) How long does it take an elderly patient to regain movement after spinal anesthesia?
c. Phase II examples:
(1) What is the effect of ketorolac on discharge temperature of elderly patients?
(2) What is the most frequent reason for inability to contact patients by phone for discharge follow-up?
(3) What are the factors associated with the ambulatory perianesthesia nurse’s proficiency with cardiopulmonary resuscitation?
E. Research hypothesis
1. Definition: a formal declaration of an expected relationship or cause and effect between two characteristics (variables) made by the researcher based on established theory and/or past research
2. Statement that offers a potential solution to the research problem that can be supported by the existing literature and the researcher’s experience
3. Always determined before the study and offers a framework for the research methodology
4. Components of a hypothesis
a. Group being studied
b. Characteristics (variables) being studied
c. The direction of the expected relationship (e.g., positive, negative, increased, decreased)
5. Perianesthesia nursing research hypotheses
a. Preoperative examples:
(1) Cataract patients who are provided with face-to-face preoperative education will remember more information than cataract patients who are given an audiovisual preoperative video.
(2) Patients scheduled for breast biopsy will report more anxiety if the time between preadmission interview and day of surgery is longer than 3 days.
(3) There is a positive relationship between patient educational level and compliance with NPO guidelines.
b. Phase I examples:
(1) There will be a positive relationship between the PACU nurse’s years of experience and comfort with administering moderate sedation and analgesia.
(2) Patients who receive intravenous ketorolac preoperatively will report less postoperative pain than patients who receive intravenous ketorolac intraoperatively.
(3) Patients who receive supplemental oxygen during postoperative transport to PACU will report less nausea than patients who do not receive supplemental oxygen.
c. Phase II examples:
(1) Discharge assessment phone calls placed after 5 pm will be more successful than phone calls placed before 5 pm.
(2) There is a negative relationship between duration of preoperative NPO status and ability to void before discharge in cystoscopy patients.
(3) Pediatric patients who participate in preoperative pediatric tours will recover faster than patients who do not participate.
F. Research variables
1. Definition: any quality or characteristic that is likely to change and/or is observed or measured by the researcher
2. Independent variable (IV): a characteristic selected by the researcher and believed to affect another characteristic (i.e., dependent variable [DV])
3. DV: the characteristic believed by the researcher to change when the IV is changed
4. IV is the cause or antecedent; DV is the effect or outcome.
5. Demographic variables are characteristics of the group (e.g., patients, providers, units) being measured (i.e., gender, age, type of anesthesia, type of surgery, education, phase).
6. IV, DV, and demographic variables require definition and measurement by the researcher; other characteristics, which may impact the research study, should be controlled.
7. IV and DV are found in the purpose statement and the research question or the hypothesis.
8. Perianesthesia nursing variables of interest
a. Preoperative examples:
(1) Type of preoperative teaching strategy (e.g., face to face, video)
(2) Timing of preadmission visits (e.g., 2 days before surgery, day of surgery)
(3) Preoperative temperature
b. Phase I examples:
(1) Postoperative temperature
(2) Report of nausea
(3) Oxygen saturation
c. Phase II examples:
(1) Duration of time to discharge
(2) Bladder volume
(3) Report of pain
d. Examples of demographic variables—patients:
(1) Age
(2) Gender
(3) Surgical procedure
e. Examples of demographic variables—providers:
(1) Years of experience
(2) Certification status
(3) Educational background
f. Examples of demographic variables—units:
(1) Phase of recovery provided
(2) Number of beds
(3) Types of patients (e.g., specialty unit, general unit)
9. Examples linking IV and DV of interest:
a. Type of teaching strategy (IV) and preoperative knowledge using a posttest score (DV)
b. Time of preadmission visit (IV) and anxiety behavior (DV)
b. Type of health care provider (IV) and patient satisfaction (DV)
c. Warming device (IV) and postoperative temperature (DV)
d. Intravenous fluid administration volume (IV) and time to postoperative void (DV)
e. Certification of RN provider (IV) and amount of conscious sedation administered (DV)
f. Use of ketorolac (IV) and postoperative pain (DV)
g. Postoperative phone call (IV) and patient satisfaction (DV)
h. Use of pediatric tours (IV) and child anxiety behavior upon discharge (DV)
G. Methodology
1. Definition: the blueprint or plan taken by the researcher to collect the data required to answer the research question or support the research hypothesis
2. Includes all procedures required to collect the research data: design, sample, setting, instrument, procedure, data analysis
3. Includes rationales for decisions on how, when, and where data are collected, as these decisions may affect the research results
4. Researcher designs the methodology so that the findings will have implications for nursing in general, not just the group being studied (e.g., generalizability).
5. Research design
a. Definition: the approach the researcher will use to collect the data
(1) Qualitative
(2) Quantitative
b. Depends on the purpose of the study and the research question or hypothesis
c. Qualitative research design
(1) Focuses on the experience from the perspective of the patient
(2) Emphasizes the holistic approach to the patient
(3) Seeks to examine meaning of and insight into a patient’s experience
(4) Used when previous research on the topic is limited or absent
(5) Data collected using words and narratives of patients
(6) Topics using qualitative research designs in perianesthesia nursing
(a) Preoperative examples:
(i) Experience of waiting for surgery
(ii) Patient’s account of preadmission screening
(iii) Narrative response to advanced directive questions before surgery
(b) Phase I examples:
(i) Patient’s account of the experience of postanesthetic shivering
(ii) One patient’s account of midazolam-induced amnesia
(iii) Experience of parents during the child’s surgery
(c) Phase II examples:
(i) A narrative response to inquiry about satisfaction with caregivers
(ii) Patients’ experience with postdischarge nausea
(iii) Parental satisfaction with discharge instructions
d. Quantitative research design
(1) Focuses on understanding one part of the patient’s experience
(2) Emphasis placed on one or two selected variables of interest to the researcher
(3) Used when a variable is in need of description (e.g., descriptive research), a relationship is being examined (e.g., correlational research), or cause and effect is being tested (e.g., experimental research)
(4) Data collected for quantitative research can be reduced to numbers for statistical analysis.
(5) Topics using quantitative research designs in perianesthesia nursing
(a) Preoperative examples:
(i) Characteristics of patients who fail to follow preoperative instructions (descriptive research)
(ii) Effect of pediatric tours on parental anxiety (experimental research)
(iii) Relationship between NPO duration and preoperative blood pressure (correlational research)
(b) Phase I examples:
(i) Relationship between fluid volume replacement intraoperatively and incidence of postoperative nausea (correlational research)
(ii) Incidence of hypothermia among elderly patients (descriptive study)
(iii) Effect of Reiki therapy on report of postoperative pain (experimental study)
(c) Phase II examples:
(i) Effect of ketorolac on discharge temperature (experimental research)
(ii) Incidence of postdischarge nausea (descriptive research)
(iii) Relationship between admission temperature and discharge temperature (correlational research)
6. Research sample
a. Definition: the individuals (i.e., patients, nurses, and family members) who agree to participate and provide data for the research study
b. Individuals who provide data referred to as participants (qualitative design) or subjects (quantitative design)
c. Sample selected from the population of all individuals with the characteristic of interest
d. Sample selected so that the individuals are representative of all the individuals who are known to have the variable(s) of interest to the researcher
e. Sample size
(1) Qualitative design: data collected from participants until data saturation is obtained
(2) Quantitative design considerations
(a) Number of variables being studied
(b) Type of variables being studied
(c) Statistical analysis selected
(d) Ability of the instrument measuring outcome variable to detect differences
(3) Power analysis (statistical calculation) used to determine number of subjects
f. Types of sampling methods
(1) Simple random sample
(a) Random selection of study subjects from population of interest using flip of a coin or random numbers table
(b) Example: sample randomly selected from the population of thyroidectomy patients because it would be difficult and costly to study all patients in this category
(2) Stratified random samples
(a) Dividing subjects into layers or strata on the basis of specific attributes
(b) Example: PACU nurse wishes to study implementation of PACU standards of practice; hospitals are stratified by geographic location (east, west, north, south) and bed size (<100, 100–300, >300).
(3) Systematic random sampling
(a) Random selection of sample from a list or membership roster
(b) Example: American Society of PeriAnesthesia Nurses (ASPAN) membership roster (population of PACU nurses) used to obtain a sample of PACU nurses for a study on attitudes toward research
(4) Cluster sample
(a) Selection of a cluster of institutions in a geographic area
(b) Example: sample of patients selected from several PACUs from several hospitals in a metropolitan area
(5) Convenience or accidental sample
(a) Obtaining subjects within readily available location or handy population
(b) Example: PACU nurse studies effect of music therapy on pain in first 50 adult perianesthesia patients having orthopedic surgery who agree to participate.
(c) Problem with convenience samples: Patients studied may not be representative of all patients admitted to all PACUs in all states.
(6) Purposive sample
(a) Selected intentionally on the basis of a particular attribute and frequently used in instrument development
(b) Example: PACU nurse testing the ability of a new questionnaire to measure attitudes of ambulatory surgical patients’ families regarding family visits in PACU would purposefully ask surgical patients’ family members to participate in study. (Note: Families studied may not be representative of all types of ambulatory surgical patients’ families.)
g. Sample criteria
(1) Researcher makes decision on demographic characteristics of participants or subjects for the study.
(2) Inclusion criteria—demographic characteristics the researcher desires
(3) Exclusion criteria—demographic characteristics that will make the participant or subject ineligible for the study
(4) Examples of selection criteria for perianesthesia nursing research sample:
(a) Fifty male patients having regional anesthesia for herniorrhaphy
(b) All cataract patients requiring conscious sedation during the month of June
(c) Every other adult patient requiring general anesthesia who is not allergic to aspirin
(d) Children from 3 to 7 years of age who are accompanied by a parent
(e) Registered nurses who have been members of ASPAN for at least 10 years
7. Research setting
a. Definition: location or environmental condition under which the study data are collected
b. A description of the setting allows the reader to determine whether the research environment is similar to the reader’s environment and whether the findings are applicable to the reader’s practice.
c. Examples of a perianesthesia nursing research setting:
(1) Waiting area of preadmission testing department
(2) Phase I PACU of a rural acute care facility with four operating suites and six postanesthesia bays
(3) Hospital-based surgery center caring for 30 pediatric surgical cases per week
(4) Operating room with temperature controlled at 60° F and humidity of 75%
(5) Waiting area of the surgeon’s office
(6) Patient’s home
8. Research instrument
a. Definition: any device (e.g., monitor, questionnaire, interview) that produces or records data required by the research project
b. Selection of the instrument depends on the variable being studied, the availability of the instrument, the expertise of the researcher, and the subject’s capabilities.
c. The instrument should be able to actually measure what the researcher intends (i.e., be a valid representation of the variable).
d. The instrument should be able to collect consistent measurements of the variable being studied (i.e., be a reliable representation of the variable).
e. The researcher describes the instrument clearly before the data are collected.
(1) Reports or establishes the instrument’s reliability
(2) Reports or establishes the instrument’s validity
(3) Describes the nature of the instrument (e.g., number of questions, type of questions, type of device)
(4) Provides rationale for selection of the instrument
(5) Provides reference for instrument and any previous study using the instrument
f. Examples of perianesthesia nursing research instruments:
(1) Visual Analog Pain Scale
(2) Tympanic thermometer in core mode
(3) Speilberger’s State–Trait Anxiety Questionnaire
(4) Postanesthesia discharge criteria modified by Aldrete
(5) Written posttest on care of surgical dressing
9. Research procedure
a. Definition: description of the steps taken to implement research data collection, including the selection of the sample, the identification of the setting, the administration of the research instrument, and any protocols for the IV
b. Procedure provided with sufficient detail to allow the study to be replicated (repeated with a different group of participants) by other researchers.
c. Procedure described in chronological order of implementation
10. Data analysis methods
a. Definition: procedures used to analyze the data
b. Qualitative analysis will include ways in which the researcher will determine themes.
c. Quantitative analysis
(1) Descriptive procedures, correlational procedures, or tests of hypotheses
(2) Based on the type of data collected and the format of hypothesis
(3) Statistical experts consulted to determine appropriate statistical procedures
XI. ETHICAL ISSUES IN NURSING RESEARCH
A. The researcher is required to protect the vulnerable patient from harmful effects and to ensure that benefits to participants outweigh risks of participating in the research.
B. Ethical research behaviors include objectivity, cooperation with institutional guidelines, integrity, and honesty.
C. Any research on human subjects requires review and approval by an IRB or human subjects committee before collecting data.
1. Composition of the IRB includes nurses, physicians, and other health care professionals; clergy, community members, attorneys, and ethicists also participate on the IRB.
2. IRB independently determines the ethical implications of the research methodology.
3. IRB determines the requirements for participant’s informed consent either in writing or verbally.
XII. COMMUNICATING THE RESULTS OF A RESEARCH PROJECT
A. Upon completion of data collection, the researcher includes in the report findings, discussion of findings, conclusions, implications, and recommendations.
B. Findings
1. A demographic summary of the sample is provided.
2. Results of the data analysis are provided in the order of the research questions or hypotheses.
3. Tables are used to illustrate findings.
4. Statistical notations are used to describe findings (e.g., P= .001).
C. Discussion of findings
1. An interpretation of the findings
2. Related research that supports or refutes the study findings is discussed from the perspective of the researcher’s findings.
3. Examples of perianesthesia nursing research findings:
a. Findings from this study indicated that face-to-face preoperative instructions improve posttest scores significantly more than video teaching did.
b. Findings of this study revealed that 2 days before surgical intervention is the appropriate time for a preadmission interview.
c. Findings from this study did not identify a difference in patient satisfaction between care delivered by unlicensed providers and licensed providers.
d. Findings from this study indicated no difference in postoperative temperature between patients who received ketorolac and patients who received acetaminophen.
e. Findings from this study showed that postoperative follow-up phone calls made in the afternoon were more successful than those made in the morning.
D. Conclusions
1. Definition: one or two specific statements of new knowledge that have been revealed by the research findings
2. The conclusion attempts to answer the research problem presented at the beginning of the study.
3. Examples of perianesthesia nursing research conclusions:
a. The findings of the study support the conclusion that patients who receive face-to-face preoperative teaching learn better.
b. The conclusion of this study is that the timing of preoperative visits can impact patient anxiety related to their surgical experience.
c. The conclusion of this study is that level of patient education is a predictor of compliance with NPO guidelines.
d. The research findings support the conclusion that pediatric preoperative tours reduce parental anxiety but have no effect on the child’s anxiety before discharge.
e. The findings of the study support the conclusion that patients who receive preoperative analgesics have less postoperative nausea.
E. Implications and recommendations
1. Definition: suggestions offered by the researcher as to ways the research conclusions could be used in nursing practice, nursing education, nursing administration, or by future researchers
2. Implications for practice translate the research findings into usable interventions to improve patient outcomes.
3. At least one implication is reported for each research conclusion.
4. Examples of perianesthesia nursing research implications:
a. The study suggests that preoperative teaching be conducted by trained perianesthesia nurses during individualized face-to-face sessions.
b. The study findings suggest that preadmission visits should be scheduled a maximum of 2 days before the day of surgery.
c. The study findings recommend that NPO guidelines be explained based on the patient’s educational level.
d. The study findings suggest that parental tours may be just as effective as pediatric tours in reducing postoperative anxiety behaviors of children.
e. The researcher recommends that the study be repeated using male and female patients of a wide range of ages.
XIII. QI AND THE RESEARCH PROCESS
A. QI (e.g., quality assurance, total QI, and total quality management) projects are designed to measure performance against preestablished criteria (see Chapter 9).
B. Purpose of QI project is to solve an institutional problem or improve or evaluate current practice.
C. Goal of QI
1. Improve systems and processes
2. Improve outcome
D. QI projects do not follow all the steps of the research process (Table 4-1).
| Characteristic | Research | Quality Improvement |
|---|---|---|
| Seeks to solve a problem | Yes | Yes |
| Seeks to develop new knowledge | Yes | No |
| Requires defining the problem | Yes | Yes, but problem may be to examine current practice for improvement areas |
| Requires a purpose statement | Yes | No |
| Requires a question or hypothesis to be answered | Yes | No |
| Project supported by outside literature | Yes | No |
| Sample representative of population | May be, if using quantitative methods | No, sample of convenience |
| Sample size important | Yes | No |
| Setting described for replication | Yes, important for future researchers | No, setting is institution specific |
| Instrument has preestablished validity and reliability | Yes, validity and reliability strengthen study | Not needed, frequently an institution-created tool is used |
| Procedure clearly described | Yes, permits replication | Not necessary because one person is collecting data |
| Multiple methods used for data analysis depending on type of question or hypothesis | Yes, use of themes, descriptive, correlational, and effect statistics | No, data analyzed using descriptive statistics (mean, percentage) |
| Institutional review board approval required | Yes, mandatory | No, permission to survey granted by institution’s administration |
| Findings, discussion, conclusion, recommendations follow from question or hypothesis | Yes, findings presented as generalizable results | No, findings discussed in light of improvement of quality and lessons learned |
| Publication in peer-reviewed journal | Yes, results disseminated to encourage knowledge development | No, results shared with internal stakeholders |
E. Framework of QI
1. Plan
2. Do
3. Study
4. Act
XIV. DISSEMINATING RESEARCH FINDINGS
A. Research findings can be disseminated in a variety of venues.
1. Poster displays at national and local conferences and meetings of professional organizations
2. Oral presentations at national and local conferences
3. Local and national publications
a. Specialty journals: Journal of PeriAnesthesia Nursing, Breathline
b. Clinical journals: Association of periOperative Registered Nurses Journal, American Journal of Critical Care, American Association of Nurse Anesthetists Journal
c. Research journals: Nursing Research, Applied Nursing Research, Western Journal of Nursing Research
XV. PROFESSIONAL RESPONSIBILITY FOR EBP AND RESEARCH
A. Nurses have a professional responsibility to practice in accordance with the most current evidence.
B. Nurses have a professional responsibility to maintain current practice by reading, discussing, and participating in nursing research.
C. Research utilization should be included in all professional job descriptions.
D. Perianesthesia nurses participating in nursing research are responsible for:
1. Being aware of the research purpose and methodology
2. Validating that the research project has undergone IRB review
3. Advocating for the participant’s informed consent
4. Supporting the research data collection procedure where possible
BIBLIOGRAPHY
1. Agency for Healthcare Research and Quality, Available at:www.ahrq.gov; Accessed November 19, 2008.
2. American Society of PeriAnesthesia Nurses, Available at:www.aspan.org; Accessed November 19, 2008.
3. Brown, S.J., Evidence-based nursing: The research-practice connection. ( 2008)Jones & Bartlett, Philadelphia.
4. Burns, N.; Grove, S.K., Understanding nursing research: Building an evidence-based practice. ed 4 ( 2006)Saunders, Philadelphia.
5. Fetzer, S.J.; Vogelsang, J., Research primer for perianesthesia nurses. ( 2001)American Society of PeriAnesthesia Nurses, Thorofare, NJ.
6. Macnee, C.L.; McCabe, S., Understanding nursing research. ed 2 ( 2008)Lippincott, Philadelphia.
7. McSherry, R.; Artley, A.; Holioran, J., Research awareness: An important factor for evidence-based practice?Worldviews Evid Based Nurs 3 (3) ( 2006) 103–115.
8. National Guideline Clearinghouse, Available at:www.guideline.gov; Accessed November 19, 2008.
9. Ridley, R.T., The relationship between nurse educational level and patient safety: An integrative review, J Nurs Educ 47 (4) ( 2008) 149–156.
10. Shertzer, K.E.; Keck, J.F., Music in the PACU environment, J Perianesth Nurs 16 (2) ( 2001) 90–102.
11. The Cochrane Collaboration, Cochrane collection, Available at:www.cochrane.org/reviews/; Accessed November 19, 2008.
12. The Joanna Briggs Institute, Available at:www.joannabriggs.edu.au/about/home.php; Accessed November 19, 2008.
13. Zangra, G.A.; Soeken, K.L., A meta-analysis of studies of nurses’ job satisfaction, Res Nurs Health 30 (4) ( 2007) 445–458.