CHAPTER 42. Orthopedic Care
Nancy Saufl
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Describe common orthopedic surgical procedures and their associated nursing interventions.
2. Describe the assessment and management of complications associated with orthopedic procedures.
3. Describe the pathophysiology and management of arthritic disorders.
4. Identify the various types of traction and the nursing care priorities for patients in traction.
5. Describe the treatment and nursing management of the patient with a fracture.
6. Identify the educational needs of the orthopedic patient.
I. ANATOMY AND PHYSIOLOGY
A. Skeletal system
1. System of living connective tissue, high in mineral content
a. Haversian system
(1) Nourishes bone tissue
(2) Made up of blood vessels and lymphatics
(3) Architectural unit of bone
b. Types of bone
(1) Cortical (compact) bone
(a) Dense, hard outer layer of bone
(b) Found in shafts of long bones
(c) Poor blood supply
(2) Trabecular (cancellous) bone
(a) Spongy, porous bone
(b) Found at ends of long bones and in vertebrae
(c) Rich blood supply
c. Types of cells
(1) Osteoblasts: form new bone
(2) Osteocytes: mature bone cell
(3) Osteoclast: resorb bone
2. Functions of the skeleton
a. Provides framework for the body
b. Provides attachment and leverage for muscles, facilitating movement
c. Protects vital organs and soft tissue
d. Manufactures red blood cells
e. Provides storage for:
(1) Minerals
(2) Calcium
(3) Phosphate ions
(4) Lipids
(5) Marrow elements
3. Divisions of skeleton
a. Axial: framework of head and trunk
b. Appendicular: framework of arms and legs
4. Classification of bones
a. Long bones
(1) Diaphysis: shaft of bone
(2) Epiphysis
(a) Ends of bone
(b) Helps with bone development
(c) Made of cancellous bone
(3) Metaphysis:
(a) Flared portion between diaphysis and epiphysis
(b) Growing part of bone
(c) Has richest blood supply
(4) Physis or epiphyseal plate: growth plate between epiphysis and metaphysis of immature bone
(5) Periosteum: connective tissue that covers bone
b. Short bones
(1) Sesamoid or accessory bones
(a) Carpals
(b) Tarsals
(c) Patella
(2) Primarily found in hands and feet
c. Flat bones
(1) Skull
(2) Ribs
(3) Pelvic girdle
d. Irregular bones
(1) Ossicles of ear
(2) Vertebrae
B. Tissue of musculoskeletal system
1. Connective tissue
a. Development
(1) Develops from mesenchymal cells
(2) Later differentiates into specialized connective tissue cell types
b. Types (three)
(1) Collagenous tissue
(a) Derived from dense fibrous connective tissue
(b) Constructed primarily of collagen fibers
(c) Tendons
(i) Dense fibrous connective tissue strands at the ends of muscles that attach muscles to bone
(ii) Characteristics: flexibility, strength, extensibility
(d) Ligaments
(i) Dense connective tissue bands that attach bone to bone and provide stability to joints
(e) Tendons and ligaments can withstand pulling forces.
(i) Activity
(ii) Joint motion largely affects ligaments.
(iii) Muscle contraction largely affects tendons.
(f) Fascia
(i) Made of connective tissue
(ii) Has many proprioceptive endings
(iii) Covers muscles; provides network of nerves, blood, and lymph vessels
(2) Cartilage: nonvascular tissue composed of collagenous and elastic fibers
(a) Hyaline cartilage—very elastic
(i) Found in:
[a] Trachea
[b] Synovial joints
[c] Larynx
[d] Nasal septum
[e] Ribs
(ii) Tends to get calcified in old age
(b) White fibrocartilage—thick, shock absorbing
(i) Found in:
[a] Symphysis pubis
[b] Between vertebrae
[c] Wrist and knee joints
[d] Ends of clavicle
(ii) Interarticular fibrocartilage—flattened fibrocartilaginous plates between articular surfaces of joints, such as
[a] Menisci of the knee
[b] Temporomandibular
[c] Sternoclavicular
[d] Acromioclavicular
[e] Wrist
[f] Knee joints
(iii) Connecting fibrocartilage—found in joints with limited mobility, such as the intervertebral disks
(iv) Circumferential fibrocartilage—rims surrounding sockets of articular surfaces such as the glenoidal labrum of the hip and the shoulder
(v) Stratiform fibrocartilage—forms a coating on osseous groove that tendons pass through
(c) Yellow or elastic cartilage—dense, more flexible and pliant than hyaline cartilage; strong
(i) Found in outer ear, epiglottis, and eustachian tube
(d) Synovial membrane—covers and lines joints; forms synovial fluid responsible for lubricating and nourishing articular cartilage
(3) Bone
(a) Osseous connective tissue
(b) Predominantly made up of
(i) Fibrous component called collagen
(ii) An amorphous component called calcium phosphate
(c) Highly porous and vascular
2. Muscular system
a. Made up of muscle cell bundles
b. Possess rich vascular supply
c. Covered by fascia
d. Attached to bone by tendons
e. Produces bodily movement by contraction
f. Controlled by complex interaction with the central nervous system
3. Joints: articulations where bones or two bone surfaces come together
a. Diarthrosis—freely movable synovial joint
(1) Uniaxial—move in one axis and only one plane
(a) Hinge—knee, elbow, finger, toe
(b) Pivot—radial head
(2) Biaxial—moves around two perpendicular axes, in two perpendicular planes
(a) Saddle—base of the thumb
(b) Condyloid—distal radius and wrist bones
(3) Multiaxial—moves in three or more planes and around three or more axes
(a) Ball and socket—hip, shoulder
(b) Gliding—vertebral joints
b. Amphiarthrosis—limited movement
(1) Symphysis pubis, intervertebral
c. Synarthrosis—immovable
(1) Sutures—fibrous tissue between skull bones
(2) Syndesmosis—ligament connecting bones’ distal radius and ulna, distal tibia and fibula
(3) Gomphosis—fibrous membrane connects to bone, tooth, and mandible or maxilla
(4) Range of motion—degree of movement of a joint (Figure 42-1)
(a) Angular—changes the size of angles between articulating bones
(i) Flexion—shortens the angle by bending forward
(ii) Extension—lengthens the angle by bending backward
(iii) Abduction—movement away from the midline
(iv) Adduction—movement toward the midline
(v) Plantar flexion—increases the angle between the foot and the front of the leg by bending the foot and toes down and back
(vi) Dorsiflexion—decreases the angle between the foot and the back of the leg by bending the toes and foot upward
(vii) Hyperextension—stretching a part beyond its normal anatomical limits
(b) Circular—movement around an axis
(i) Rotation—moving or pivoting a bone around its axis (side to side of the head)
(ii) Circumduction—movement that resembles a cone shape; the distal part is a wider circle (winding up to throw).
(iii) Supination—palm turns upward while forearm rotates outward.
(iv) Pronation—palm turns downward while forearm rotates inward.
(c) Gliding—moving one joint surface over another with no circular or angular movement
(d) Miscellaneous movements
(i) Elevation—moving upward, lifting
(ii) Depression—moving downward, lowering
(iii) Inversion—sole of the foot turns inward.
(iv) Eversion—sole of the foot turns outward.
(v) Protraction—moving a part forward, such as the jaw or shoulder
(vi) Retraction—moving a part backward
(vii) Opposition—moving parts together (finger and thumb)
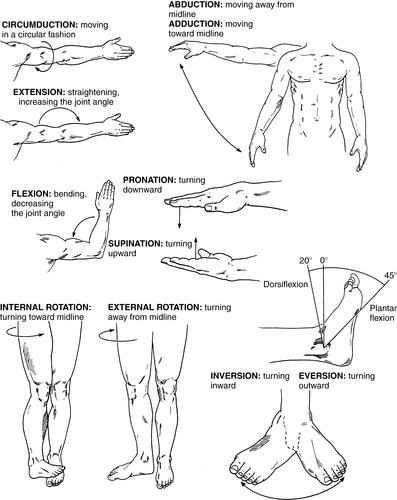 |
| FIGURE 42-1 ▪
Joint movements.
(From Maher AB, Salmond SW, Pellino TA: Orthopaedic nursing, Philadelphia, 2002, WB Saunders.)
|
II. PATHOPHYSIOLOGY OF THE MUSCULOSKELETAL SYSTEM
A. Common congenital and developmental abnormalities
1. Joint dysplasia
a. Incomplete formation of diarthrodial joint
b. May lead to chronic subluxation or dislocation of joint
c. Developmental dysplastic hip, including congenital dislocated hip; may lead to early secondary osteoarthritis (OA)
2. Torsional problems of the long bones
a. Deformity related to abnormal development of bone
(1) Metatarsal adductus: metatarsal deviated medially
(2) Tibial torsion: tibia rotated externally or internally
(3) Femoral anteversion: leads to intoeing with internal or external rotation of leg
b. In extreme cases, may require surgical intervention
3. Clubfoot
a. Anomaly characterized by inversion of foot and forefoot, adduction, and equinus
b. Classified as fixed or rigid
4. Osteogenesis imperfecta (“brittle bone disease”)
a. Genetic disease characterized by:
(1) Defect in collagen synthesis
(2) Generalized osteopenia
(3) Metabolical abnormalities
b. Classified according to severity: types I to III
5. Legg-Calve-Perthes disease
a. Idiopathic avascular necrosis of femoral head—flattening of femoral head
b. Seen in school-aged children
c. May lead to:
(1) Residual deformity of femoral head
(2) Fracture
(3) Early secondary OA
6. Slipped capital femoral epiphysis
a. Disruption of growth plate leading to posterior displacement of femoral head on the femoral neck
b. Seen in preteen and teenage children
c. May lead to avascular necrosis of the femoral head, limb shortening, or early secondary OA
7. Scoliosis
a. Lateral curvature of spine with vertebral rotation
b. Classified according to causative factors
(1) Idiopathic
(a) Unknown origin: accounts for 90% of cases
(b) Most frequent in children 10 to 12 years of age
(c) Occurs 10 times more frequently in females
(d) Familial pattern may be present.
(2) Congenital
(a) Develops in early embryonic life (6-8 weeks)
(b) Malformation of spine occurs, resulting in hemivertebrae or failure of segmentation of vertebrae.
(3) Neuromuscular
(a) Neuropathic (paralytic): associated with spina bifida, poliomyelitis, or cerebral palsy
(b) Myopathic: associated with muscular dystrophy
(4) Additional types of scoliosis
(a) Acquired—seen in:
(i) Rheumatoid arthritis
(ii) Rickets
(iii) Spinal cord tumors
(iv) Neurofibromatosis
(b) Traumatic: resulting from vertebral fracture after radiation
B. Metabolical bone disease
1. Osteoporosis
a. Common disorder characterized by a generalized reduction in the mass and strength of bone, leading to high risk for fracture
b. Rate of bone resorption greater than rate of bone formation
c. Multiple risk factors
(1) Prevalent with Caucasian, Asian, or Hispanic/Latino people
(2) Small skeletal frame
(3) Estrogen deficiency or postmenopausal condition
(4) Inactivity or immobility
(5) High caffeine or alcohol consumption
(6) Low-calcium or high-protein diet
(7) Female
(8) Older age
(9) Family history
(10) Certain medications (i.e., steroids, some anticonvulsants)
d. Fractures common and may be induced by minor trauma
(1) Wrists
(2) Femoral head
(3) Vertebrae
(4) Pelvis
2. Paget’s disease (osteitis deformans): chronic disorder that typically results in enlarged and deformed bones
a. Excessive breakdown and formation of bone tissue causes the bone to weaken.
b. Slow, progressive disease caused by initial bone resorption, followed by period of reactive bone formation
c. New bone is:
(1) Thicker
(2) Softer
(3) Has reduced strength
(4) Highly vascular
3. Rickets
a. Abnormal calcification of bone seen in childhood, leading to soft and deformed bones
b. Related to deficiency in vitamin D caused by:
(1) Nutritional deficit
(2) Inability to absorb or use vitamin D
4. Osteomalacia
a. Demineralization of bone in the adult leading to soft, deformed bones (“adult rickets”)
b. Related to inadequate supply of calcium or phosphorus caused by:
(1) Nutritional deficit
(2) Absorptive problem
C. Neoplastic disorders
1. Primary bone or soft tissue tumors
a. Benign or malignant tumors
(1) Bone
(2) Cartilage
(3) Connective tissue
(4) Vascular tissue near bone
b. May lead to local bone destruction and weakening of the tissue
c. Relatively uncommon
2. Bone metastasis
a. Spread of malignancy from a primary site of origin to bone
b. Lytic or blastic lesions may lead to:
(1) Bone destruction
(2) Weakening
(3) Impending or actual fracture
c. Frequent sequelae of common malignancies
(1) Breast
(2) Prostate
(3) Lung
(4) Kidney
(5) Thyroid
(6) Bladder
D. Infection
1. Bone or joint tuberculosis
a. Infection of bone or joint by Mycobacterium tuberculosis, leading to cartilage or bone destruction
b. Weight-bearing joints and vertebral bodies most common sites
c. May require surgical drainage of abscesses in addition to aggressive pharmacological treatment
2. Osteomyelitis
a. Microbial invasion of bone leading to acute or chronic infection
b. Classified according to method of microbial invasion
(1) Hematological: acute or chronic infection spread to the bone through circulatory system
(a) More common in children
(b) More easily treated in children because of higher vascularity of their bones and supportive tissues
(2) Contiguous: infection of the bone by direct extension of bacteria from infected soft tissue or surgical site
(a) More common in adults older than 50 years
(b) Risk factors include orthopedic surgeries or soft tissue trauma.
(3) Traumatic: infection of the bone by direct contamination with environmental or bodily microbes
(a) More common in young males and children
(b) Risk factors include penetrating wounds, intramedullary rods, and open fractures.
3. Septic arthritis
a. Microbial invasion of the synovial membrane, commonly bacterial in origin, leading to joint infection
b. Joint infection usually accompanied by signs and symptoms of systemic infection
c. May lead to destruction of articular cartilage and early secondary OA
E. Arthritic disorders
1. OA (degenerative joint disease or osteoarthrosis)
a. Progressive noninflammatory disorder of diarthrodial joints characterized by loss of articular cartilage, marginal osteophytes (spurs), subchondral cysts, and sclerotic changes
(1) Most common form of arthritis
(2) Primarily affects weight-bearing joints: hips, knees, spine, shoulders, interphalanges
b. Classified by causative factor
(1) Primary OA
(a) Cause unknown
(b) Increased with:
(i) Obesity
(ii) History of repetitive trauma to joint
(iii) Age
(2) Secondary OA
(a) Related to preexisting factors
(b) Seen after trauma to:
(i) Joint
(ii) Dysplasia
(iii) Other pediatric or congenital disorders of the joint
(iv) Sepsis
(v) As a result of a primary disease involving the joint such as hemophilia
c. Clinical findings
(1) Asymmetric distribution
(2) Pain or stiffness in joint, especially with weight-bearing activities
(3) Crepitation of joint
(4) Deformity of joint or decrease in range of motion
(5) Possible swelling and warmth of joint
(6) Gait disturbance (limp)
d. Conservative treatment
(1) Reduction of risk factors
(a) Weight loss if needed
(b) Decrease in weight-bearing activities
(2) Gait rest devices (cane, crutch)
(3) Local application of heat or cold
(4) Pharmacological therapy (Box 42-1)
BOX 42-1
PHARMACOLOGICAL THERAPY
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Initial drug of choice for mild to moderate pain
NSAIDs inhibit prostaglandin formation through the cyclooxygenase (Cox) enzyme.
This enzyme exists in two isoforms, Cox-1 and Cox-2:
▪ Primary therapeutic effect of NSAIDs exhibited by blocking Cox-2.
▪ Celecoxib, (Celebrex)—100 to 200 mg orally twice per day
▪ Meloxicam, (Mobic)—7.5 to 15 mg orally daily (structurally related to piroxicam; selectively inhibits Cox-2 over Cox-1)
▪ Ketorolac, (Toradol)—10 mg orally every 4 to 6 hours or 30 mg IV or IM every 6 hours; if older than 65 years, 15 mg IV or IM every 6 hours
▪ Fenoprofen, (Nalfon, Fenopron)—300 to 600 mg orally three or four times per day to a maximum of 3.2 g daily
▪ Nabumetone, (Relafen, Relifex)—1000 mg orally daily or twice per day with maximum of 2000 mg per day
▪ Piroxicam, (Feldene, Pirox)—20 mg orally daily
▪ Sulindac, (Clinoril, Novo-Sundac)—150 to 200 mg orally twice per day with maximum daily dose of 400 mg
▪ Naproxen, (Anaprox, Aleve)—250 to 500 mg orally twice per day with maximum daily dose of 1.5 g
▪ Ketoprofen, (Orudis, Actron)—75 mg three times per day or 50 mg four times per day or 200 mg as extended-release form; maximum daily dose 300 mg, or 200 mg as extended-release form
Possible side effects:
▪ Abdominal pain
▪ Heartburn
▪ Ulcers
▪ Bleeding
▪ Renal failure
▪ Decreased liver function
Opioids
Added to NSAIDs for mild to moderate pain; adult dosage guidelines:
▪ Codeine—15 to 60 mg orally every 4 to 6 hours as needed with maximum daily dose of 360 mg
▪ Hydrocodone bitartrate, Lortab, Lorcet, or Roxicet combined in varying strengths with acetaminophen, 500 to 650 mg
▪ Oxycodone hydrochloride, Percodan, or Percocet combined in varying strengths with aspirin, 325 mg, or acetaminophen, 500 to 650 mg
▪ Propoxyphene hydrochloride, Darvon—65 mg orally every 4 hours, as needed with maximum daily dose of 390 mg
For persistent pain, stronger opioid added along with antidepressants or antianxiety drugs to increase tolerance for pain:
▪ Antidepressants helpful in reducing neuropathic pain
▪ Neurontin (Gabapentin)—originally developed for treatment of epilepsy; now widely used to relieve pain, especially neuropathic pain and postoperative chronic pain
IM, Intramuscular; IV, intravenous.
e. Nutritional supplements: glucosamine and chondroitin
(1) Substances found naturally in the body and believed to play a role in:
(a) Cartilage formation
(b) Cartilage elasticity
(2) Widely used as dietary supplement in the treatment of OA
(3) Some studies have shown that some people with mild and moderate OA taking glucosamine/chondroitin have reported pain relief similar to that of nonsteroidal anti-inflammatory drugs (NSAIDs).
(4) Some research has indicated that the supplements might slow down cartilage damage in patients with OA.
f. Disease-modifying drugs
(1) Current focus of pharmacological research
(a) Pentosan
(b) Enzyme inhibitors
(i) Doxycycline
(ii) Collagenase inhibitors
(iii) Lipids
(iv) Growth hormones
g. Topical analgesics
(1) Inexpensive, safe, effective
(2) Application by massage releases endorphins.
(3) NSAIDs
(a) Salicylate
(b) Benzydamine
(c) Diclofenac
(d) Ibuprofen
(e) Indomethacin
(f) Ketoprofen
(g) Felbinac
(h) Capsaicin
h. Intra-articular injections
(1) Corticosteroids
(2) Local anesthetics
(3) Viscosupplements (hyalgan products)
i. Surgical options
(1) Arthroscopy: diagnostic, for removal of loose bodies, and for treatment
(2) Joint fusion (arthrodesis)
(3) Osteotomy: option in early arthritis accompanied by deformity
(4) Resection arthroplasty
(5) Hemiarthroplasty: replaces one half of the joint with an artificial surface and leaves the other part in its natural (preoperative) state
(a) Most commonly performed on the hip after fracture of neck of femur
(b) Partial knee replacement (hemiarthroplasty, unicompartmental) may be performed on patient whose disease is limited to a single compartment (i.e., medial or lateral).
(i) The unicompartmental knee replacement is less invasive.
(ii) The small incision does not interfere with the main muscle control of the knee.
(c) Shoulder hemiarthroplasty may be indicated in select patients with OA or posttraumatic disorders, providing pain relief and functional improvement.
(6) Total joint replacement: arthritic or damaged joint removed and replaced with a prosthesis (artificial joint)
(7) Hip resurfacing: type of hip replacement that replaces the two surfaces of the hip joint, conserving bone (head of femur preserved)
2. Rheumatoid arthritis
a. Chronic systemic inflammatory disease potentially affecting multiple organs and joints; also considered an autoimmune disorder
(1) Extra-articular manifestations
(a) Cardiovascular changes: fibrinous pericarditis, cardiac myopathy, vasculitis
(b) Pulmonary changes: pulmonary nodules, pleuritis, pulmonary fibrosis, pleural effusion
(c) Neurological: peripheral neuropathy, carpal tunnel syndrome, nerve entrapment
(d) Gastrointestinal: bowel and mesenteric vasculitis, malabsorption, enlarged spleen
(e) Ocular: scleritis, episcleritis, Sjögren’s syndrome
(f) Integument: rheumatoid nodules, vasculitic skin lesions, purpura
(g) Hematological: anemia, thrombocytopenia, granulocytopenia, increased sedimentation rate
(h) Constitutional: fatigue, malaise, fever
(2) Articular manifestations
(a) Synovial proliferation
(b) Pannus formation
(c) Destruction of articular cartilage, with cartilage erosion, bone cysts, and osteophytes
(d) Tendon and ligament scarring and shortening with ligamentous laxity, subluxation, and contracture
b. Causative factors
(1) Etiology unknown
(a) Infectious
(b) Traumatic
(c) Stress related
(2) Genetic predisposition exists.
(3) Seen in all ages, affecting females to males 3:1
c. Clinical manifestations (musculoskeletal)
(1) Polyarticular symmetric joint distribution
(a) Can affect any synovial joint
(b) Most severe changes in weight-bearing joints
(2) Joint swollen, erythematous, and warm to touch
(3) Joint pain, stiffness, and possible contracture
(4) Joint deformity, laxity, or subluxation
(a) Deformities of knees, feet, phalanges possible
(b) Subluxation of cervical vertebrae
(5) Muscle atrophy
d. Conservative treatment
(1) Joint protection techniques
(a) Weight loss if needed
(b) Decrease in weight-bearing activities
(c) Use of large, more proximal joints in more activities
(2) Gait rest devices (cane, crutch)
(3) Program of rest and exercise
(4) Application of cold and heat
(a) Use ice for first 48 to 72 hours postoperatively.
(i) Specific duration of treatment for ice is 20 minutes “on” followed by one hour “off.”
(b) Next alternate ice with heat
(c) Finally use strictly heat.
(i) Duration of treatment for heat is 15 to 20 minutes “on” followed by a minimum of one hour “off.”
(5) Splinting or bracing of joint
(6) Pharmacological therapy (see Box 42-1)
(a) Oral NSAIDs (see OA)
(b) Oral analgesics
(c) Oral corticosteroids
(d) Oral or parenteral gold therapy
(e) Oral remittive agents: chloroquine phosphate
(f) Oral immunosuppressives: methotrexate, cyclophosphamide, azathioprine
(g) Intra-articular injection of steroid or local anesthetic
e. Surgical options
(1) Fusion of cervical spine or small joints (e.g., wrist)
(2) Synovectomy
(3) Osteotomy
(4) Tendon repair or transfer
(5) Hemiarthroplasty
(6) Total joint replacement
F. Traumatic disorders
1. Strain
a. Musculotendinous injury caused by overstretching, repetitive stress, or misuse
b. Classified according to degree of injury to musculotendinous unit
(1) First degree: mild stretching or injury
(2) Second degree: moderate stretching or tearing
(3) Third degree: severe stretching, leading to rupture of the body or insertion site of the musculotendinous unit
2. Sprain
a. Ligamentous injury caused by overstretching or overuse
b. Classified according to degree of injury to ligament
(1) First degree: mild injury involving tear of few ligamentous fibers
(2) Second degree: moderate injury with tearing of up to one half of ligamentous fibers
(3) Third degree: severe injury leading to rupture of the body of the ligament or from its bony attachment
3. Dislocation or subluxation
a. Disruption of the contact of articulating surfaces of a joint caused by force to joint or development abnormality
(1) Dislocation: complete disruption of joint
(2) Subluxation: partial disruption of joint
b. Most common in shoulder joint
c. May be accompanied by soft tissue injury, including nerve palsy
d. Recurrent dislocation may necessitate surgical repair of soft tissue or reconstruction of joint.
4. Fracture (Figure 42-2)
a. Disruption of normal continuity of a bone, often accompanied by soft tissue trauma
b. Classification of fractures
(1) Severity of fracture
(a) Compound (open): bone is broken with communication of the fracture site with an external wound.
(b) Simple (closed): bone is broken with skin intact.
(c) Complete: continuous fracture line through entire section of bone
(d) Incomplete: break in continuity of one side of cortex only, as in the “greenstick” fracture
(e) Displaced: edges of fractured bone not aligned, with higher risk for neurovascular damage
(f) Nondisplaced: edges of fractured bone remain aligned.
(g) Impacted: fractured bone fragment forcibly driven into an adjacent bone (“telescoped”)
(h) Avulsion: separation of small fragment of bone at site of a ligament or tendon attachment
(2) Direction of line of fracture
(a) Longitudinal (linear): fracture line runs parallel to axis of bone.
(b) Oblique: fracture line runs at a 45 ° angle to axis of bone.
(c) Spiral: fracture line encircles bone shaft.
(d) Transverse: fracture line runs at a 90 ° angle to longitudinal axis of bone.
(e) Comminuted: multiple fracture lines divide bone into multiple fragments.
(3) Etiology of the fracture
(a) Stress (fatigue): fracture occurs as result of repetitive microtrauma or an excessive musculotendinous pull that exceeds the strength of the bone.
(b) Pathological (spontaneous): fracture through an area of disease-weakened bone, usually related to minor trauma
(c) Compression: fracture resulting from compressive force
(4) Fractures by name
(a) Pott’s fracture: fracture at distal fibula associated with severe tibiofibular disruption
(b) Colles’ fracture: fracture of distal radius within 1 inch of joint in a characteristic manner
c. Etiology of fractures: fractures occur when bone subjected to more stress than it can absorb.
d. Predisposing factors for fractures: factors that reduce bone strength or forces that exceed bone strength
(1) Age: extremes in age
(2) Nutritional deficiency: diet low in calcium, low in vitamin D, or high in protein
(3) Metabolical diseases
(4) Inactivity or immobility: bone remains strongest under stress (“Wolff’s Law”).
(5) Physical abuse or trauma
e. Fracture healing: healing maximized when bone edges approximated
(1) Hematoma forms at site of fracture (first 24 hours).
(2) Leukocytes infiltrate site, followed by macrophages.
(3) Fibrous matrix of collagen proliferates at site.
(4) Highly vascular “callus” forms.
(5) Callus converts to loosely woven bone.
(6) Callus calcifies and remodels (full fracture “union”).
f. Goals of fracture management
(1) Reduce fracture to normal anatomical alignment.
(2) Promote bone healing.
(3) Maintain extremity function.
g. Methods of fracture reduction
(1) Closed reduction: reduction achieved without surgical intervention
(a) Continuous traction: skin or skeletal
(b) Manual traction
(c) Splints or casts
(d) External fixation
(2) Open reduction and internal fixation
(a) Allows visualization of fracture site
(3) Repair with:
(a) Pins
(b) Rods
(c) Nails
(d) Wire
(e) Screws
(f) Plate and screw combinations
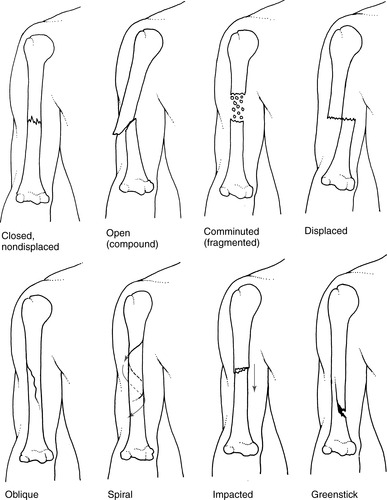 |
| FIGURE 42-2 ▪
Types of fractures.
(From Ignatavicius DD, Workman ML: Medical surgical nursing, ed 4, Philadelphia, 2002, WB Saunders.)
|
III. COMMON THERAPEUTIC DEVICES
A. Casts
1. Purpose
a. Provide temporary immobilization.
b. Prevent or correct deformities.
c. Support bone and soft tissue during healing process.
d. Promote early weight bearing.
2. Types of casts
a. Short extremity cast
(1) Applied for stable fractures or tertiary sprains
(2) May be weight bearing versus non–weight bearing
b. Long extremity cast
(1) Applied for stable or unstable fractures
(2) Immobilizes joint to protect soft tissue injuries: Achilles tendon rupture
c. Cylinder cast
(1) Applied to treat stable fractures of long bones
d. Body cast
(1) Immobilizes spine (e.g., postoperative spinal fusion)
(2) Corrects deformities (e.g., scoliosis)
e. Spica cast
(1) Immobilizes complex joint: shoulder, hip, thumb
(2) Prevents dislocation of complex joint while promoting soft tissue healing
3. Materials
a. Plaster of Paris
(1) Applied by wrapping wet plaster strips
(2) Easily molded
(3) Heavier weight
b. Fiberglass—most common
(1) Applied by wrapping wet plastic roll
(2) More difficult to mold
(3) Lightweight
c. Fiberglass-free, latex-free polymer
(1) Use in latex allergy or latex-sensitive patients.
d. Hybrid
(1) Combination of plaster of Paris and fiberglass
e. Polyester and cotton knit
f. Thermoplastic
(1) Fabric tape composed of polyester polymer
4. Early postcasting care
a. Promote cast drying.
(1) Plaster of Paris: may take 24 hours or greater to dry
(a) Leave cast uncovered and open to air.
(b) Use fans to aid drying of large casts.
(c) Position casted part on pillow or smooth surface.
(d) Move cast on pillow or with palms to avoid plaster indentation.
(e) Advise patient to expect feeling of warmth as cast dries.
(2) Fiberglass: dry within 30 minutes
(a) Blot moisture from surface with paper towel.
(b) Use blow dryer on cool or warm setting to aid drying of cast and skin.
b. Potential complications
(1) Skin breakdown
(2) Neurovascular compromise
(3) Compartment syndrome
(4) Fracture misaligned
(5) Superior mesenteric artery syndrome
(a) Only seen in body spica casts
(b) A decreased blood supply to bowel
(i) Resulting from compression of mesenteric artery
(ii) Causes necrosis to gastrointestinal tract and hemorrhage
(c) Symptoms
(i) Pain, distention, pressure in abdomen
(ii) Bowel obstruction
(iii) Nausea and vomiting
(iv) Presenting symptoms may appear days or weeks after cast applied because of retroperitoneal fat loss after patient immobilized.
(d) Postcasting care
(i) Prevent complications related to ineffective breathing pattern with body or spica cast.
[a] Note rate and quality of respirations.
[b] Reposition patient in more upright position if possible.
[c] Teach relaxation techniques, deep controlled breathing.
[d] Cut a window in the cast, bivalve or remove cast.
[e] Place nasogastric tube to decompress stomach.
[f] Patient receives nothing by mouth (NPO), receiving intravenous (IV) fluids.
[g] Prone position optimal
[h] Ligament of Treitz released surgically
c. Protect skin.
(1) Remove loose particles of plaster or plastic from cast edges and skin.
(2) Cover edges of cast to prevent skin irritation, especially important in personal area.
(a) Turn edge of skin liner (stockinette) over cast edge and secure with tape.
(b) If stockinette not used, “petal” edge with Transpore tape or moleskin.
(c) Insert diaper at buttocks to prevent soiling in children with body or spica cast.
(3) Instruct patient to avoid putting any object between cast and skin.
d. Reduce postoperative or postinjury swelling.
(1) Elevate extremity on pillow above level of heart.
(2) When cast dry, apply ice to area of injury or fracture.
e. Assess neurovascular status of extremity.
(1) Perform integrated bedside assessment of extremity (Box 42-2).
BOX 42-2
INTEGRATED BEDSIDE ASSESSMENT OF EXTREMITY
Assessment of Neurovascular Status
Pain
Edema
Color
Capillary refill
Pulses
Temperature
Sensation
Motion
(2) Note amount and change in bloody drainage on cast and in dependent areas.
B. Traction
1. Definition: application of pulling force in the presence of a counterforce
2. Purpose
a. Aligns fragments of displaced bones, preventing further soft tissue injury
b. Reduces muscle spasm
c. Maintains limb length
d. Maintains alignment of limb while resting soft tissue
e. Reduces contracture and deformity
3. Types of traction
a. Skin traction
(1) Traction force applied via wraps, straps, or prefabricated boots secured to body (e.g., Russell’s or Buck’s traction)
(2) Uses
(a) Short-term immobilization of stable fractures (e.g., Buck’s traction for proximal femoral fractures)
(b) Intermittent traction (e.g., cervical neck traction)
(3) Techniques of application
(a) Traction applied at bedside by trained individual
(b) “Customized” devices applied using Webril and moleskin
(c) Prefabricated devices (e.g., boots)
(d) Traction weight generally no more than 10 lb (4.5 kg)
b. Skeletal traction
(1) Traction applied directly to bone through transcortical or pericortical wires or screws (e.g., halo traction)
(2) Uses
(a) Long-term immobilization of fractures (commonly >1 week)
(b) Short-term to long-term immobilization of unstable fractures of long bones or pelvis
(3) Techniques of application
(a) Traction applied at bedside or in operative suite
(b) Local anesthetic applied to skin and injected into periosteum
(c) Sedation and analgesia commonly used with pediatric patients
(d) Amount of weight to traction according to patient’s body weight and complexity of fracture, usually 15 to 40 lb
(e) Use of portable x-ray to confirm fracture reduction
c. Manual traction
(1) Temporary traction applied by manual pull on extremity
(2) Uses
(a) Maintenance of alignment and position of extremity when skin or skeletal traction is being readjusted
(b) Short transport of patient
(c) Dislocation or relocation of joint, casting of extremity, and reduction of fracture
(3) Techniques of application: firm manual pull placed on extremity while taking care to avoid pressure on bony prominences
4. Nursing care of patient in traction
a. Maintain traction apparatus to ensure proper alignment of body.
(1) Reposition patient in neutral alignment, usually supine.
(2) Obtain specific orders for:
(a) Amount of traction pull
(b) Position of extremity in bed
(c) Head of bed—elevating head of bed decreases counterforce of body.
(3) Readjust skin traction if device dislodged.
(4) Apply manual traction to extremity whenever skeletal traction interrupted.
(5) Avoid heavy coverings (blankets) over extremities, which may disrupt traction.
(6) Inspect traction apparatus carefully every shift to ensure:
(a) Bolts are tight on frame.
(b) Knots are tight.
(c) Weights are free hanging.
b. Assess skin integrity.
(1) Inspect pressure points between skin and apparatus.
(2) Inspect bony prominences of body in bed.
(3) Note redness, swelling, abrasion, pain caused by pressure.
c. Assess for neurovascular compromise.
(1) Perform integrated bedside assessment of extremity (see Box 42-2).
(2) Compare affected with nonaffected side.
(3) Note potential problems caused by disrupted traction or inappropriately sized devices (e.g., boots).
d. Assess for complications related to skeletal pin.
(1) Note:
(a) Redness
(b) Purulent drainage
(c) “Tenting” of skin surrounding pin
(d) Pain at insertion of skeletal pin
(2) Note signs and symptoms of infection in patient with long-standing traction.
C. External fixator
1. Definition: method of rigid fixation applied using percutaneous pins and wire in bone that attach to a portable external frame
2. Purpose
a. Reduces fractures, especially complex or open fractures
b. Permits care of soft tissue wounds associated with fractures
c. Corrects bony deformity
d. Stabilizes fractures with delayed union or nonunion
e. Stabilizes arthrodesis (fusion) of a joint
3. Types of external fixators
a. Simple
(1) One or two bars on side(s) of limb (e.g., unilateral or bilateral frame)
(2) Used to treat less complex fractures
b. Complex
(1) Multiple bars or semicircular rings placed in three-dimensional configuration around limb
(a) Triangular
(b) Quadrilateral
(c) Semicircular
(d) Circular frame
(2) Used to treat more complex fractures, often accompanied by soft tissue trauma
4. Nursing care of patient with external fixator
a. Maintain external fixator.
(1) Inspect device carefully every shift to ensure that bolts are tight on frame, with no movement of fixator pieces.
(2) Move device and limb using pillow beneath extremity or by grasping longitudinal bars on each side of limb.
b. Assess for neurovascular compromise.
(1) Perform integrated bedside assessment of extremity (see Box 42-2).
(2) Compare affected with nonaffected side.
c. Assess for complications related to skeletal pin.
(1) Note redness, purulent drainage, or pain at pin site.
(2) Note signs and symptoms of infection in patient with long-standing device.
(3) Note changes in sensorimotor status.
D. Assistive devices
1. Definition: devices prescribed to assist in mobility by providing support to an injured or weakened lower extremity by redistributing weight to the upper extremities
2. Purpose
a. Promote healing of traumatically fractured bones.
b. Promote healing of surgically osteotomized bones.
c. Support weakened or injured soft tissue.
3. Weight-bearing prescription
a. Non–weight bearing (NWB): affected extremity should not touch floor.
b. Touch-down weight bearing (TDWB): foot rests on floor with no weight.
c. Partial weight bearing (PWB): 30% to 50% of body weight placed on affected extremity
d. Weight bearing as tolerated: as much weight as patient can tolerate without extreme pain
e. Full weight bearing: full weight should be placed on affected extremity.
4. General instructions for patients
a. Take small, controlled steps at all times.
b. Wear sturdy walking shoes with nonskid soles.
c. Avoid wet or snowy areas.
d. Remove from path of walking:
(1) Throw rugs
(2) Electrical cords
(3) Excess furniture
(4) Other obstructions
e. Stand erect, looking forward when walking.
f. Lead with strong, unaffected leg.
5. Types of assistive devices
a. Crutches
(1) Selection criteria: prescribed for persons with good coordination, balance, and upper body strength
(2) Types of crutches
(a) Axillary: most common crutch where
(i) Weight is placed on wrist and by tricep contraction.
(ii) Consists of a central post, handgrip, and axillary pad
(b) Platform: crutch used to distribute weight to forearm
(i) Consists of a central post and forearm platform
(ii) Reduces stress on arthritic wrist or fingers
(c) Canadian or Lofstrand: crutch used to distribute weight to wrist and hand; consists of a central post with a band that fits around the forearm
(3) Proper fit of axillary crutches
(a) Instruct patient to stand erect while wearing comfortable walking shoes.
(b) Raise or lower central post so that two or three fingers can be inserted between the axilla and axillary pad.
(c) Raise or lower handgrips so that elbows are bent 20 ° to 30 °.
(4) Crutch gaits
(a) Two-point gait: patient advances one crutch at the same time as the contralateral leg in alternating fashion (common with PWB).
(b) Three-point gait: patient advances both crutches along with affected leg (common in PWB, TDWB, and NWB).
(c) Four-point gait: patient advances right crutch, left foot, left crutch, right foot, with three “points” on ground at all times (used only in patient with high disability).
(5) Stair climbing
(a) Climbing up stairs
(i) Patient holds banister on affected side and both crutches in contralateral hand.
(ii) Patient steps up with unaffected leg.
(iii) Patient follows with crutches and affected leg to same stair.
(b) Climbing down stairs
(i) Patient holds banister on affected side and both crutches in contralateral hand.
(ii) With weight on “good leg,” patient steps down with affected leg and crutches.
(iii) Patient brings unaffected leg down to same stair.
b. Walkers
(1) Selection criteria: prescribed for persons who require more stability than crutches can provide, such as those with impaired balance or coordination
(2) Types of walkers
(a) Simple walker: most common type of walker; consists of sturdy frame with handgrips
(b) Platform walker: walker used to distribute weight to forearm; consists of a sturdy frame with forearm platform; reduces stress on arthritic wrist and fingers
(3) Proper fit of simple walker
(a) Instruct patient to stand erect while wearing comfortable walking shoes, heels even with back of walker.
(b) Raise or lower all four legs of walker equally so that elbows are bent 20° to 30°.
(4) Walker gait
(a) Patient advances walker a short arm length forward, planting walker firmly on all four legs.
(b) Patient advances affected foot, then advances body forward while supporting weight on arms.
(5) Stairs: performed with folded walker in manner similar to stair climbing with crutches
c. Canes
(1) Selection criteria: prescribed for patients with minor disability and good balance, often after use of crutches or walker
(2) Types of canes
(a) Simple cane: central post with curved handle
(b) Quad cane: central post with four distal legs and curved handle
(3) Proper fit of cane
(a) Instruct patient to stand erect while wearing comfortable walking shoes, cane 2 inches (5 cm) in front and 6 inches (15 cm) to the side of unaffected leg.
(b) Raise or lower central post so that elbow is bent 20 ° to 30 °.
(4) Cane gait
(a) Instruct patient to hold cane in hand opposite affected side.
(b) Patient puts weight on “good leg,” advancing affected leg and cane a comfortable distance.
(c) Patient supports weight on both cane and affected leg, stepping through with “good leg.”
(5) Stairs: performed with cane hand opposite affected leg in manner similar to stair climbing with crutches
IV. ASSESSMENT PARAMETERS
A. Vascular assessment (Box 42-2)
1. Pulses
a. Assess operative extremity first; compare finding with the opposite extremity.
(1) Note rate, rhythm, quality.
(2) Compare distal with proximal pulses and side to side.
b. Diminished neurovascular function requires prompt intervention to prevent complications and/or permanent damage.
2. Skin color
a. Note pallor or blanching, suggestive of insufficient arterial blood flow.
b. Note duskiness or cyanosis, suggestive of insufficient venous return.
c. Compare side to side.
3. Skin temperature
a. Note increase or decrease in temperature.
(1) Cold hand or foot may indicate diminished arterial blood supply to the area.
(2) Extremity that is hot may indicate decreased venous return.
4. Capillary refill
a. Compress nail bed and quickly release; expect return of color in 3 seconds.
(1) Rapid refill suggests venous congestion.
(2) Slow refill suggests arterial insufficiency.
b. Compare side to side.
5. Edema
a. Note location and severity.
b. Note effect of elevating extremity above heart level on extent of edema.
c. Compare side to side.
6. Pain
a. Assess level of pain.
(1) Severe pain, particularly on passive motion, reliable sign of probable neurovascular compromise
(2) If vascular status compromised, pain intensifies even with use of opioids and therapeutic measures.
B. Peripheral nervous system assessment
1. Sensory component
a. Note patient’s ability to detect sensory stimulation.
(1) Pain
(2) Light touch
(3) Deep touch
(4) Heat or cold
(5) Vibratory sense
(6) Proprioception
(7) Two-point discrimination
b. Note location and severity of any change.
c. Compare side to side.
2. Motor component
a. Note patient’s ability to move extremity actively through range of motion (ROM).
b. Grade strength of major muscle groups.
(1) Grade 5: active ROM against strong resistance (considered “normal” in well-functioning adult)
(2) Grade 4: active ROM against moderate resistance
(3) Grade 3: active ROM against gravity only
(4) Grade 2: weak, incomplete ROM against gravity
(5) Grade 1: no notable motion, but visible contractility of muscle group
(6) Grade 0: no motion or visible contractility
c. Compare side to side.
C. Integrated peripheral nervous system assessment of extremities
1. Upper extremity
a. Radial nerve
(1) Sensory: touch web space between thumb and index finger.
(2) Motor: extend wrist, hyperextend thumb.
b. Median nerve
(1) Sensory: touch tip of index finger.
(2) Motor: oppose thumb to small finger.
c. Ulnar nerve
(1) Sensory: touch tip of small finger.
(2) Motor: abduct fingers.
2. Lower extremity
a. Peroneal nerve
(1) Sensory: touch lateral side of great toe, medial side of second digit.
(2) Motor: dorsiflex ankle, hyperextend great toe.
b. Tibial nerve
(1) Sensory: touch each lateral and medial aspect on sole of foot.
(2) Motor: plantar flex ankle, flex great toe.
V. COMPLICATIONS COMMON TO ORTHOPEDICS
A. Deep vein thrombosis (DVT)
1. Definition: obstruction of deep venous circulation by a blood clot, usually distal to the cusp of a venous valve
2. Etiology: Virchow’s triad
a. Venous stasis: immobilization, peripheral edema
b. Vascular wall damage: trauma, traction of vessel during limb manipulation (dislocation), surgery
c. Hypercoagulable state: clotting disorder, dehydration
3. Incidence and risk factors
a. Seen in 40% to 60% of patients with lower extremity surgery or injury
b. Factors increasing risk for DVT
(1) Increased age
(2) Surgery
(a) Orthopedic
(b) Abdominal
(c) Gynecological
(3) Immobility
(4) Lower extremity trauma
(5) Previous DVT
(6) Obesity
(7) Use of oral contraceptives
(8) Coexistence of:
(a) Peripheral vascular disease
(b) Malignancy
(c) Stroke
(d) Pregnancy
(e) Cardiac disease
(f) Smoking
(g) IV drug abuse
(h) Inflammatory bowel disease
(i) Dehydration
(j) Sickle cell disease
c. Factors decreasing risk for DVT
(1) High mobility
(2) Good hydration
(3) Use of epidural anesthesia
(4) Use of anticoagulants
4. Postanesthesia care
a. Assess for signs and symptoms of DVT: most common at least 48 to 72 hours after immobilization or surgery.
(1) Unilateral edema of the lower extremity, unrelieved with elevation
(2) Warmth, redness, tenderness, “fullness” of lower extremity
b. Monitor results of diagnostic tests.
(1) Noninvasive: Doppler ultrasonography
(2) Invasive: ascending contrast venography (most diagnostic)
c. Initiate interventions to prevent DVT.
(1) Provide adequate hydration.
(2) Encourage maximal mobility and early ambulation.
(3) Apply mechanical devices per order in operating room or PACU to combat early DVT formation.
(a) Antiembolic hose
(b) Sequential compression devices to lower leg or calf
(c) Plantar “foot pumps”
(d) Inconclusive data exist comparing device effectiveness with or without anticoagulation.
(4) Administer anticoagulants per order.
(a) Oral warfarin: may be ordered day before, day of surgery, or in first 24 hours postoperatively
(b) Low–molecular weight heparin: generally begun at least 12 hours postoperatively
(c) Aspirin
(d) Additional pharmacological agents for high-risk patients
(i) Danaparoid
(ii) Dextran
(iii) Thrombin inhibitors
(iv) Dermatan sulfate
d. Initiate early interventions to treat patient with known DVT.
(1) Administer anticoagulation per order: bolus heparin, then adjust to achieve recommended international normalized ratio (INR).
(2) Decrease risk for clot embolization.
(a) Maintain patient on bed rest per order: common with large proximal DVT
(b) Avoid aggressive massage of involved extremity.
(c) Administer thrombolytic agent: uncommon therapy
(d) Prepare patient for surgical intervention: inferior vena cava filter inserted if multiple DVT
(e) Use noncemented prostheses if possible.
B. Pulmonary embolism (PE)
1. Definition: complete or partial obstruction of the pulmonary artery or one of its branches by a systemically mobile thrombus or foreign body
2. Causes: as listed for DVT
3. Incidence and risk factors
a. Seen clinically in 10% to 20% of patients undergoing major lower extremity surgery; fatal up to 10% of the time
b. Factors increasing risk for PE: unrecognized DVT and all other risk factors for DVT
4. Postanesthesia care
a. Assess for signs and symptoms of PE: most common 48 to 72 hours after injury or surgery; vary with degree of vessel occlusion.
(1) Dyspnea
(2) Tachypnea
(3) Restlessness
(4) Pleuritic chest pain
(5) Cough or hemoptysis
(6) Rales
(7) Pulmonary friction rub
(8) Hypoxemia
(9) Tachycardia
b. Monitor results of diagnostic tests.
(1) Noninvasive
(a) Electrocardiogram (ECG) may show:
(i) T-wave inversion
(ii) ST depression
(b) Chest x-ray film may show:
(i) Wedge-shaped defect
(ii) Accompanying diaphragmatic elevation
(2) Invasive
(a) Arterial blood gases: may be normal or show hypoxemia
(b) Lung scan (ventilation/perfusion studies): not reliable in absence of signs and symptoms
(c) Pulmonary angiography: highly diagnostic; usually performed only if lung scan nondiagnostic because of risk of examination
c. Initiate interventions to prevent PE (see DVT)
d. Initiate interventions to treat patient with known PE.
(1) Promote adequate gas exchange.
(a) Position patient in high Fowler’s.
(b) Instruct on slow deep breathing.
(c) Provide oxygen: nonrebreathing mask common
(d) Prepare for intubation if necessary.
(2) Administer anticoagulation per order: bolus heparin, then adjust to achieve recommended INR.
(3) Decrease risk for clot embolization (see DVT).
C. Fat embolism syndrome (FES)
1. Definition: mobilization of fat and free fatty acids that leads to acute pulmonary insufficiency
2. Causes
a. Mechanical theory: fat from marrow of broken bones embolized to lung and occludes small pulmonary vessels
b. Biochemical theory
(1) Stress response leads to release of catecholamines.
(2) Free fatty acids mobilize.
(3) Chylomicrons coalesce in lung.
(4) Chylomicrons increase capillary permeability within alveoli.
3. Incidence and risk factors
a. Seen clinically:
(1) In 1% to 10% of patients with fractures
(2) In 5% to 10% of patients with multiple fractures or pelvic fractures
(3) Up to 50% of patients with fractures may have subclinical FES.
(4) Rarely with insertion of intramedullary rods or stemmed prostheses
b. Possible at any age but most prevalent in:
(1) Men aged 20 to 40
(2) Elderly between ages 70 and 80
c. Factors that increase the risk for FES
(1) Invasion of intramedullary canal
(2) Sepsis
(3) Shock
4. Postanesthesia care
a. Assess for signs and symptoms of FES: often present 12 to 48 hours after causative event, often rapidly progressing.
(1) Confusion, agitation, anxiety
(2) Tachypnea, dyspnea, pulmonary edema
(3) Hypoxemia, hypocarbia
(4) Tachycardia, dysrhythmias, substernal chest pain
(5) Hypotension
(6) Petechiae of trunk or conjunctiva: occur 50% of time
(7) Pyrexia
b. Monitor results of diagnostic tests.
(1) Noninvasive
(a) ECG: may show atrial fibrillation
(b) Chest x-ray film: may show diffuse pulmonary infiltrate
(2) Invasive
(a) Arterial blood gases: may be normal or show hypoxemia
(b) Central venous pressure: elevated
(c) Pulmonary wedge pressure: initially reduced because of decreased perfusion of left atrium; later may rise
(d) Lung scan: may be performed in stable patient to rule out PE
(e) Pulmonary angiography: may be performed in stable patient to rule out PE
(f) Laboratory findings
(i) Elevated serum lipase
(ii) Elevated sedimentation rate
(iii) Elevated triglycerides
(iv) Elevated glomerular filtration rate
(v) Decreased hematocrit
(vi) Increased fat in urine
c. Initiate interventions to prevent FES.
(1) Maintain stability of fractured limbs.
(2) Treat sepsis and shock aggressively.
(3) Provide adequate hydration.
(4) Controversial whether to administer methylprednisolone to maintain integrity of pulmonary vascular system
d. Initiate interventions to treat patient with known FES: early diagnosis and aggressive treatment critical.
(1) Promote adequate gas exchange.
(a) Position patient in high Fowler’s.
(b) Instruct on slow deep breathing.
(c) Provide oxygen: nonrebreathing mask common.
(d) Prepare for intubation: common.
(2) Administer corticosteroids: creates antiadhesive effect on platelets, decreases inflammation of vascular membranes.
(3) Administer diuretics: reverses pulmonary edema.
(4) Support cardiovascular system.
(a) Provide adequate fluid replacement.
(b) Administer blood products.
(c) Enhance blood pressure: dopamine.
(d) Enhance pulmonary arterial pressure and right ventricle afterload: nitroglycerin drip.
D. Compartment syndrome
1. Definition: condition in which increased pressure within a muscle compartment may lead to severe neurovascular compromise
a. In cases of massive muscle destruction, may also see myoglobinuric renal function
2. Cause: any event that leads to increased extracompartmental or intracompartmental pressure, leading to edema and ischemia
3. Pathophysiology: edema-ischemia cycle
a. Compromise of muscle compartment from:
(1) Overuse
(2) Extended compression of limb
(3) Fracture
(4) Bleeding produces profound, quick response by surrounding tissue.
b. As edema of muscles increases, capillary bed perfusion compromised and venous congestion ensues.
(1) Edema compresses nerves and vessels.
(2) Progressive edema causes muscle ischemia.
(3) Histamine release by ischemic muscles causes capillary dilation and enhanced capillary permeability.
(4) Edema increases, resulting in greater compromised tissue perfusion and tissue oxygenation.
(5) Lactic acid formation increases, causing anaerobic metabolism to accelerate.
(6) Blood flow increases, causing increase in tissue pressure, leading to greater compartmental pressures.
c. If edema-ischemia cycle not arrested:
(1) Irreversible muscle damage in 4 to 8 hours
(2) Permanent nerve damage in 8 hours
d. Three types
(1) Acute compartment syndrome
(a) Trauma related, limb threatening
(2) Chronic compartment syndrome
(a) Overuse of muscles (i.e., weekend exercise enthusiast)
(3) Crush syndrome
(a) Prolonged compression of limb
4. Incidence and risk factors
a. Uncommon in general population; most commonly associated with fractures or injuries of the lower extremities
b. Development within:
(1) Thirty minutes to 3 hours post injury
(2) Postoperatively during first 7 days
c. Factors that increase the risk for compartment syndrome
(1) Fracture
(2) Severe soft tissue injury (e.g., crush injury)
(3) Prolonged limb compression
(a) Restrictive wraps, cast, brace, or apparatus
(b) Prolonged compression of limb
(i) Unconscious victim lying on own limb
(ii) Prolonged pressure from positioning device during lengthy surgery
(c) Prolonged use of antishock trousers
(d) Tight fascial closure
(4) Internal bleeding
(5) Increased capillary permeability: related to histamine release
(a) Infiltrated IV fluids or medications
(b) Some poisonous snake bites
(c) Severe frostbite
d. Postanesthesia care
(1) Assess for signs and symptoms of compartment syndrome: perform comprehensive neurovascular assessment, noting deterioration as follows.
(a) Pain: most universal symptom related to muscle ischemia
(i) Pain extreme
(ii) Unrelieved
(iii) Aggravated by passive flexion or extension of digit or limb
(iv) Not well localized—involves entire compartment
(b) Pallor
(i) Seen in early stage; related to compression of artery
(ii) Later may be seen as cyanosis
(c) Paresthesias: commonly seen change related to compression of sensory nerve
(i) Burning
(ii) Searing
(iii) Electric sensations
(d) Pulselessness
(i) In early stage, pulse with decreased strength
(ii) Later, pulse nonpalpable but audible on Doppler ultrasonography
(iii) In later stages, no pulse found on Doppler ultrasonography
[a] Muscle and nerve ischemia can be occurring without occluding an artery.
[b] Pulses may be palpable in the patient with acute compartment syndrome.
(e) Paralysis
(i) In early stage, may be motor weakness related to compression of motor nerve
(ii) In later stage, may be complete paralysis
(f) Rigid or “tight” limb representing compartment engorgement
(g) Decreased urine output, with dark urine
(2) Monitor results of diagnostic tests.
(a) Direct measurement of compartment pressures
(i) Variety of methods in which catheter inserted into the compartment
[a] Catheter purged with normal saline
[b] Monitor intracompartmental pressure.
[c] Pressures greater than 30 to 35 mm Hg considered diagnostic and warrant surgical intervention.
(b) Laboratory findings of muscle destruction and renal insufficiency:
(i) Elevated
[a] Serum Creatine Kinase MM isoenzyme (CPK-MM)
[b] White blood cell count
[c] Serum potassium
[d] Serum phosphate
[e] Blood urea nitrogen (BUN)
[f] Serum creatinine
(ii) Reduced
[a] Serum calcium
[b] pH
(iii) Elevated urine myoglobin
(3) Initiate interventions to prevent compartment syndrome.
(a) Perform comprehensive neurovascular assessment on all patients at risk.
(b) Provide early measures to decrease lower extremity edema.
(i) Elevate limb above heart level.
(ii) Ice limb at site of injury or surgery.
(c) Decrease potential for further injury.
(i) Carefully handle injured part.
(ii) Maintain traction.
(iii) Brace
(iv) Cast
(4) Initiate interventions to treat patient with suspected or diagnosed compartment syndrome.
(a) Perform comprehensive neurovascular assessment every 15 minutes with special attention to compartment at risk.
(b) Maintain limb in neutral at level of heart.
(i) Enhances arterial blood flow
(ii) Reduces possible neurovascular impingement
(c) Remove ice: reduce vasoconstriction.
(d) Release or remove restrictive wraps, splints, or casts.
(e) Assess pain and administer analgesics.
(f) Maintain accurate input and output records.
(g) Provide emotional support.
(h) Assist with compartment pressure checks.
(i) Prepare patient for fasciotomy per order.
(i) Extensive surgical decompression of compartment
(ii) High risk for infection as a result of ischemic conditions
VI. THE PERIANESTHESIA EXPERIENCE
A. Preoperative phase—begins with patient’s decision to have surgery and ends when he or she enters the operating room
1. Goals
a. Thorough assessment of patient’s physical and psychosocial condition
b. Educating and preparing patient for surgery
2. Include the following:
a. Complete history including preexisting conditions
b. Medications
c. Allergies to foods, medications, or latex
d. Family history of anesthetic complications such as pseudocholinesterase deficiency and malignant hyperthermia
e. Social history—does the patient have assistance after surgery?
f. Lab work dependent on procedure and age of patient
g. Blood donation if replacement a possibility and time permits
h. Informed consent
i. NPO status
j. Preoperative education
(1) Begin discharge teaching.
(a) Use of assistive devices
(b) Pain management
(c) Signs of infection
(d) Dressing and incisional management
B. Intraoperative phase—the time patient is in the operating room to the time patient admitted to phase I PACU
1. Goals
a. Appropriate surgical positioning
b. Prevent infection.
c. Prevent injury.
d. Maintain sterile field.
e. Perform accurate surgical counts.
f. Procure needed equipment (i.e., type of implant, traction, fixator, cast material).
g. Assess fluids and vital signs.
C. Postoperative care, phase I—acute phase of recovery from anesthesia and surgical procedure
1. Routine phase I admission assessment and monitoring
2. Monitor surgical site.
a. Location of operative site
b. Neurovascular status
(1) Temperature
(2) Color
(3) Capillary refill
(4) Pulses
(5) Movement
(6) Sensation
3. Monitor patient’s level of pain (Box 42-3).
BOX 42-3
THE HIERARCHY OF IMPORTANCE OF THE BASIC MEASURES OF PAIN INTENSITY
1. The patient’s pain rating using a self-reported pain rating scale (e.g., 0-10 numerical rating scale)
2. The patient has experienced a procedure or condition that is thought to be painful (e.g., surgery).
3. Behavioral signs (e.g., facial expression, crying, restlessness, fidgeting)
4. Proxy pain rating provided by a family member or other person who knows the patient well
5. Physiological indicators (e.g., elevated vital signs)
From McCaffery M, Pasero C: Pain clinical manual, ed 2, St Louis, 1999, Mosby.
4. Prevent/treat nausea and vomiting as indicated.
5. Initiate physician orders.
6. Discharge to phase II per criteria (see Chapters 30 and 51) when:
a. Recovered from anesthesia
b. Hemodynamically stable
c. Pain managed
d. Nausea and vomiting controlled
e. Scoring criteria met
D. Postoperative care, phase II—observation period that includes preparing patient and support persons for home care (see Chapters 50 and 51)
1. Routine phase II assessment
2. Teaching postoperative care critical to successful recovery
a. Medications (pain control, antibiotics, resuming routine home medications)
b. Bowel management (stool softener)
c. Assessing neurovascular status
d. Care of dressings
(1) Incision site
(2) Wounds
(3) Drains
(4) Casts
(5) Cryotherapy
(6) Continuous passive motion (CPM)
(7) Pin sites
e. Signs of infection
f. When to call physician
(1) Increasing pain
(2) Fever
(3) Edema
(4) Infection
(5) Bleeding
(6) Change in neurovascular status
g. Diet
h. Mobility guidelines
i. Reinforce instructions on assistive devices.
j. Postoperative appointment with surgeon
k. Driving considerations
l. Self-care (showering, bathing)
E. Postoperative care, extended observation (see Chapter 50, Chapter 51 and Chapter 52)
1. Extended stays
2. Patient discharge goals (Box 42-4)
BOX 42-4
PATIENT DISCHARGE GOALS FOLLOWING AMBULATORY SURGERY AND ANESTHESIA
1. To promote patient satisfaction by minimizing disruptive influences associated with the patient’s perioperative care
2. To optimize quality patient care such that patients can be safely discharged from the facility
3. To educate patients regarding the anticipated recovery process, thus facilitating patient participation and compliance with postoperative care plus early recognition of problems
4. To proficiently manage patients to minimize cost to the patient, medical facility, and third-party payers
From Burden N, DeFazio Quinn DM, O’Brien D, et al (eds): Ambulatory surgical nursing, ed 2, Philadelphia, 2000, WB Saunders.
F. Nursing diagnosis for orthopedic patient
1. Anxiety and fear related to surgical procedure, loss of control
2. Knowledge deficit relating to surgical procedure and perianesthesia experience
3. High risk for ineffective coping
4. Risk for neurovascular compromise from perioperative positioning
5. Pain management deficit
6. Impaired physical mobility secondary to surgical procedure and postoperative pain management
7. Knowledge deficits regarding mobility skills
8. Self-care deficits
9. Activity intolerance
10. Potential for constipation from immobility and use of opioids
11. High risk for skin breakdown
12. Potential for infection
13. Potential for neurovascular compromise related to cast or traction devices
14. Knowledge deficit relating to use of CPM, cryotherapy, and/or assistive devices
15. Potential for DVT
VII. COMMON OPERATIVE PROCEDURES
A. Definitions
1. Upper extremity
a. Carpal tunnel release—decompression of the median nerve by dividing the transverse carpal ligament
b. Finger amputation and revision—generally for:
(1) Traumatic injuries
(2) Infection
(3) Vascular compromise
c. Joint replacement—performed to improve function in patients with rheumatoid arthritis or other degenerative diseases
(1) Shoulder
(2) Small joints of the finger
(3) Hand
(4) Wrist
d. Olecranon bursectomy—excision of bursal wall and calcifications
e. Open reduction, internal fixation—surgical placement of hardware such as pins, screws, or plates to maintain position of bones for healing
f. Release of de Quervain’s hand—decompression of dorsal compartment of the hand to treat stenosing tenosynovitis of the wrist at the base of the thumb
g. Release of Dupuytren’s contracture—fasciotomy or fasciectomy to treat contracture in the palmar surface of the hand
h. Rotator cuff repair—repair of muscles and tendons of the rotator cuff
i. Synovectomy—removal of part or all of the synovial lining of a joint to retard progression of rheumatic destruction of the joint
2. Lower extremity
a. Anterior cruciate ligament (ACL) reconstruction—replacement of damaged ligament with autograft, allograft, or synthetic ligament to return stability to the knee after ligament tear
b. Arthroscopic meniscectomy—removal of part of the meniscus (cartilage) of the knee using arthroscopic technique
c. Osteotomy—cutting a bone to change its position for weight bearing or to correct an abnormal curvature
d. Prepatellar bursectomy—excision of bursal wall and calcifications
3. Miscellaneous
a. Arthroscopy: shoulder, wrist, knee, ankle
(1) Diagnostic arthroscopy can be performed in a variety of joints.
(2) Involves insertion of fiberoptic instrument into a joint to visualize interior
(3) Multiple procedures can be performed through a scope, including but not limited to:
(a) Debridement
(b) Biopsy
(c) Meniscectomy
(d) Ligament repair
(e) Removal of loose bodies
b. Bone biopsy—arthroscopic or open
c. Cast change
d. Closed reduction of fractures
e. Cyst removal
f. Debridement—arthroscopic or open
g. Excision of bone spurs—commonly formed as a result of osteoarthritic changes
h. Excision of ganglion—removal of cystic mass found over a joint or tendon sheath
i. Excision of lesion
j. Hardware removal
k. Joint manipulation (e.g., after knee arthroplasty)
l. Muscle biopsy
m. Removal of foreign body
n. Simple tendon repair
o. Fasciotomy—surgical incision of fascia to relieve constriction and swelling in a muscle compartment
p. Bone graft—transfer of autologous or homologous bone from one site to another to replace bone, stabilize an internal fixation, or promote a bony fusion
q. Arthroplasty—surgical resection of a joint with placement of prosthesis; may be done as open repair or arthroscopically assisted repair
r. Tendon transfer—transference of tendon insertion point to different position to improve muscle function
s. Amputation—surgical removal of a body part
t. Replantation—surgical reattachment of a body part (i.e., finger, hand, arm, toe) that has been completely cut from a person’s body
(1) Goal is to give the patient back as much use of the original area as possible.
VIII. TYPES OF ORTHOPEDIC SURGERY
A. Rotator cuff repair
1. Composed of four muscles and tendons
a. Supraspinatus
b. Subscapularis
c. Infraspinatus
d. Teres minor
2. Areas of shoulder most easily seen arthroscopically
a. Glenohumeral joint
(1) Ball-and-socket joint at end of humerus
(2) Most mobile joint in body
(3) Muscles and ligaments of rotator cuff strengthen this joint
b. Subacromial space
c. Acromioclavicular joint
3. Procedure: arthroscopically assisted repair; also done as open repair if large enough tear involving more than one tendon
4. Purpose
a. Pain relief
b. Improvement of functional abilities of joint
5. Types of tears
a. Four muscles identified above and their tendons comprise rotator cuff.
(1) Subscapularis most frequently torn muscle, responsible for internal rotation of humerus
b. Tears occur more in women and are seen most frequently after age 40.
c. Etiology
(1) Degenerative weakened areas in cuff as a result of aging process
(2) Severe tears may result from:
(a) Heavy lifting
(b) Throwing object
(c) Fall on shoulder
(d) Sudden adduction force applied to rotator cuff while arm is held in abduction
6. Postanesthesia care
a. Neurovascular assessment of affected arm
b. Support surgical arm in sling or sling and swathe with abductor pillow to maintain joint alignment and diminish tension from operative shoulder.
c. Ice packs or cryotherapy to decrease edema and pain
d. Monitor dressing; reinforcing or changing may be required because of multiple puncture sites and leaking of irrigation fluids used intraoperatively to visualize joint.
e. Pain management
(1) Intraoperative intra-articular injection of local anesthetic
(2) Interscalene block
(3) Opioids
(4) NSAIDs
f. Physical therapy and home mobility instructions reinforced
(1) Emphasize importance of following instructions to avoid exacerbation of condition.
(2) Rehabilitation usually takes 6 months to 1 year.
g. Complications
(1) Contractures of elbow and shoulder if patient noncompliant with rehabilitation program
(2) Potential damage to deltoid muscle
(3) Repair work to cuff not holding because of misuse or overuse by patient
B. Spinal fusion and stabilization (thoracolumbar spine)
1. Procedure: surgical stabilization of spine using mechanical instrumentation with or without bone graft augmentation
2. Purpose
a. Prevent progression of spinal deformity.
b. Correct spinal deformity: lateral curves greater than 40 °.
c. Reduce actual or potential neurological or cardiopulmonary deficits.
3. Methods of spinal fusion
a. Posterior spinal fusion with instrumentation
(1) Cotrel-Dubousset instrumentation: most common
(2) Harrington distraction rods or spinous process wiring
(3) Luque rods: most common for paralytic scoliosis
b. Anterior spinal fusion
(1) Zielke instrumentation
(2) Harms instrumentation
c. Combined anterior and posterior surgery
(1) Recommended for adults or children with severe deformities
(2) Anterior approach performed first, posterior approach commonly staged 5 days or more later (but may be performed during the same surgery)
d. Bone graft
(1) Autograft: bone transplanted from one part of person’s body to another part (i.e., from iliac crest)
(2) Allograft: donor bone or tissue
(3) Graft placed on decorticated spine to encourage osteoinduction
e. Minimally invasive spinal surgery
(1) Smaller incisions
(2) Microscopically assisted tissue dissection
(3) Conservative removal of only extruded or sequestered nucleus pulposus
(4) Percutaneous techniques; microscopic diskectomy; endoscopically visualized methods
(5) Less surgical morbidity
4. Postanesthesia care
a. Assess neurovascular status: perform comprehensive neurovascular assessment every 15 minutes for first 2 hours, then hourly.
(1) Note bowel and bladder dysfunction.
(2) Assist with somatosensory evoked potential monitoring as ordered.
(3) Assess strength and sensation in extremities; notify surgeon of weakness and/or new paresthesias.
b. Assess for headache, possibly related to spinal fluid leak.
c. Assess for wound drainage.
(1) Note dependent drainage on dressing and bed.
(2) Note formation and extent of hematoma.
(3) Maintain occlusive compression dressing to operative site.
(4) Maintain drainage device if present.
d. Position patient for safety.
(1) Patient commonly positioned supine in regular hard bed
(2) Maintain patient in neutral body alignment.
(3) Log roll patient side to side with physician order.
(4) Assist patient’s movement with draw sheet.
(5) Discourage patient use of trapeze or pulling under patient’s axilla (to avoid rod displacement).
e. Monitor for complications after spinal fusion (see Complications Common to Orthopedics, section V).
(1) Reduced gas exchange and ineffective breathing patterns
(a) Encourage coughing and deep breathing hourly.
(b) Assess equality and clarity of breath sounds.
(c) Obtain chest x-ray film after anterior fusion to determine lung expansion.
(d) Monitor arterial blood gases.
(e) Turn patient side to side every hour.
(2) Gastric distention and decreased peristalsis
(a) Auscultate for bowel sounds hourly.
(b) Insert nasogastric tube if necessary.
(c) Administer stool softener as needed.
C. Arthroplasty (joint reconstruction)
1. Procedure: reconstruction of articulating surfaces of joint
2. Purpose
a. Relief of chronic disabling pain
b. Improvement in joint function and activities of daily living
c. Correction of deformity
d. Prevention of further bone destruction
e. Stabilization of joint
3. Joints replaced
a. Most common arthroplasties
(1) Hip
(2) Knee
(3) Shoulder
b. Other joints replaced
(1) Elbows
(2) Fingers (proximal interphalangeal joint, metacarpophalangeal joint)
(3) Wrist and thumb
(4) Ankle
(5) Temporomandibular joint
4. Common diagnosis prearthroplasty
a. Degenerative arthritis (OA or osteoarthrosis)
b. Rheumatoid arthritis
c. Avascular necrosis (osteonecrosis or ischemic necrosis)
d. Posttraumatic arthritis
5. Types of arthroplasties
a. Hemiarthroplasty (one joint surface reconstructed with artificial part)
(1) Cup arthroplasty: placement of metal cup over femoral head (uncommon in modern arthroplasties)
(2) Endoprosthesis: replacement of femoral head with stemmed prosthesis stabilized in proximal medullary canal
(a) Austin Moore prosthesis: prosthetic femoral head articulates with natural acetabulum.
(b) Bipolar prosthesis: prosthetic femoral head articulates with plastic liner of large metal “shell” placed against acetabulum (greatest motion is within prosthetic device).
(3) Hip resurfacing: type of hip replacement that replaces the two surfaces of hip joint, conserving bone (head of femur preserved)
b. Total joint arthroplasty: both joint surfaces reconstructed with artificial parts
6. Materials commonly used
a. Metals
(1) Cobalt chromium
(2) Titanium or titanium alloys
b. Ceramics
c. Plastics (high–molecular weight polymers)
d. Polymethylmethacrylate (“bone cement”)
7. Methods of component fixation in bone
a. Cement
(1) “Gold standard” of fixation
(2) Cement injected under pressure
(3) Cement hardens in minutes, emits heat in process.
(4) Allows for immediate full weight bearing on extremity
b. Biological ingrowth
(1) Microtextured surface of prosthesis allows bone to “grow into” and stabilize component.
(2) Bone ingrowth optimized with tight fit of prosthesis into healthy dense bone
(3) Attempts at “tight fit” can cause intraoperative fracture.
(4) Postoperative weight-bearing restrictions generally continue for average of 2 months.
c. Press fit
(1) Used for stemmed components only
(2) Stem impacted snugly into canal of bone with cement; stem mechanically supported by cortical bone
8. Potential complications common to arthroplasties
a. DVT
(1) Single most common complication with lower extremity joint arthroplasty
(2) Prophylaxis generally given to all patients
b. PE
c. Fat embolism: rare, possible during insertion of stemmed devices or in situations of acute traumatic injury
d. Compartment syndrome: rare, may occur as a result of compression of contralateral limb during surgery or with large wound hematoma
e. Peripheral neurovascular impairment
f. Infection—number one causative organism, Staphylococcus aureus
(1) Superficial wound infection
(a) Generally limited
(b) May be related to stitch abscess
(c) Treated with topical or oral antibiotics or both
(2) Deep wound infection
(a) Acute: attributed to perioperative event
(b) Late: attributed to hematological spread of infection in body from remote site
(i) Urinary tract infection
(ii) Abscessed tooth
(c) Acute deep infection requires open irrigation of joint and possible exchange of liner and long-term antibiotics.
(d) Late deep infection often requires:
(i) Removal of prosthesis
(ii) Debridement of bone or tissue
(iii) Long-term antibiotics
9. Postanesthesia care of patient with hip arthroplasty
a. Assess neurovascular status.
(1) Perform comprehensive neurovascular assessment at least every hour for first 4 hours.
(2) Note signs of peroneal nerve palsy, possibly resulting from stretch injury caused by intraoperative hip dislocation, limb lengthening, or hematoma.
(a) Weak or absent dorsiflexion of foot and ankle against examiner resistance
(b) Decreased sensation or numbness
(i) Lateral aspect of great toe
(ii) Medial aspect of second toe
b. Assess for signs of wound drainage: blood loss should not exceed 500 mL in first 8 hours.
(1) Note dependent drainage on dressing and bed.
(2) Note formation and extent of hematoma.
(a) May suggest active hemorrhage
(b) May require surgical evacuation
(3) Maintain occlusive compression dressing on operative site, reinforcing if necessary.
(4) Maintain drainage device if present.
(a) Closed suction device such as a hemovac commonly used
(b) Gravity device: uncommon
(c) Autotransfusion device: used to collect and reinfuse blood according to established guidelines
c. Position lower extremity to reduce risk of dislocation.
(1) Maintain operative extremity in neutral alignment.
(2) Avoid hip adduction.
(a) Place pillow or abduction device between legs at all times.
(b) Turn patient carefully to unaffected side, maintaining abduction, if allowed.
(3) Avoid hip flexion greater than 90 °.
(a) Avoid raising head of bed and foot of bed at same time.
(b) Encourage use of overhead trapeze for support during position changes.
(4) Avoid extremes in hip rotation using trochanteric roll to side(s) of affected leg, considering surgical approach.
(a) Avoid internal rotation if posterior approach.
(b) Avoid external rotation if anterolateral approach.
d. Provide aids to enhance patient compliance to position restrictions.
(1) Long-handled reacher
(2) Long shoe horn
(3) Sock aid
(4) Elevated toilet seat
(5) Chair cushions
e. Provide for pain control.
(1) Instruct patient regarding use of parenteral patient-controlled analgesia.
(2) Expect IV, epidural, or intrathecal opioids postoperatively.
f. Prevent infection.
(1) Use strict aseptic technique for all invasive procedures.
(2) Insert Foley catheter if signs of bladder distention.
(3) Instruct patient in aggressive pulmonary hygiene.
10. Postanesthesia care of patient with knee arthroplasty
a. Assess neurovascular status.
(1) Perform comprehensive neurovascular assessment at least every hour for first 4 hours.
(2) Note signs of tibial nerve palsy, possibly caused by stretch injury from:
(a) Intraoperative knee dislocation
(b) Extensive swelling
(c) Hematoma
b. Assess for signs of wound drainage: blood loss should not exceed 500 mL in first 8 hours.
c. Position extremity to reduce edema and prevent constricture.
(1) Maintain operated extremity in neutral alignment.
(2) Elevate extremity on pillow or towel roll.
(3) Avoid placement of pillow beneath popliteal fossa.
(4) Avoid prolonged side lying with knee flexed.
d. Provide assistive devices to enhance patient’s independence.
(1) Long-handled reacher
(2) Long shoe horn
(3) Sock aid
(4) Elevated toilet seat
(5) Chair cushions
e. Encourage aggressive range of motion of knee.
(1) Activate CPM machine as ordered.
(a) Supplied and adjusted by trained personnel
(b) Degrees of flexion and extension ordered by physician
(c) Gradually increase knee flexion and extension per order according to patient tolerance.
f. Provide for pain control.
g. Prevent infection.
11. Postanesthesia care of patient with shoulder arthroplasty
a. Assess neurovascular status.
(1) Perform comprehensive assessment at least every hour for first 4 hours.
(2) Note deficit in medial, radial, or ulnar nerve.
b. Assess for wound drainage: blood loss should not exceed 150 mL in first 24 hours.
(1) Note dependent drainage on dressing and bed.
(2) Note formation and extent of hematoma.
(3) Maintain occlusive compression dressing to operative site.
(4) Maintain drainage device if present.
(a) Suction device: most common
(b) Gravity device: uncommon
c. Positioning to reduce risk of dislocation
(1) Maintain postoperative extremity positioning.
(a) Shoulder adduction and internal rotation using sling and swathe dressing with affected arm at side: most common
(b) Shoulder abduction with abduction frame or airplane splint: less common
d. Assist with measures to reduce edema.
(1) Encourage range of motion of upper extremity joints distal to shoulder.
(a) Range of motion of fingers and wrist commonly encouraged at least every hour
(b) Range of motion of elbow often allowed: patient lightly stabilizes upper arm with unaffected hand during elbow range of motion.
e. Provide overhead trapeze and assistive devices to enhance patient ability to perform activities of daily living.
f. Encourage range of motion of shoulder as soon as possible.
(1) Activate CPM machine as ordered.
(a) Supplied and adjusted by trained personnel
(b) Used in supine position or in chair-sitting position
(c) Degrees and direction of movement ordered by physician
(d) Increase shoulder motion per order and according to patient tolerance.
g. Provide for pain control.
h. Prevent infection.
D. Open reduction internal fixation (ORIF) of femoral fracture
1. Procedure: operative reduction of fracture of femur and stabilization with hardware
2. Purpose
a. Attains and maintains reduction of fracture
b. Enhances fracture healing through stability
c. Allows for early mobilization of patient
3. Types of femoral fractures
a. Femoral neck fracture
(1) Basilar: fracture at distal neck of femur
(2) Subcapital: fracture directly under femoral head
b. Intertrochanteric fracture: fracture on a line through greater and lesser trochanter
c. Subtrochanteric fracture: transverse fracture between lesser trochanter and a site 1 inch or more below greater trochanter
d. Femoral shaft fracture: fracture between greater trochanter and knee
4. Commonly used fixation devices
a. Wires and pins
b. Bone screws
c. Plates with screws
d. Compression (sliding) hip screw
e. Intramedullary rods and nails
5. Postanesthesia care
a. Assess neurovascular status: perform comprehensive neurovascular assessment.
b. Maintain proper positioning.
(1) Place extremities in neutral position.
(2) Use trochanter roll (rolled sheet or blanket) or sandbag to prevent rotation of lower extremities.
(3) Turn patient only if physician order.
(a) Usually approved to turn to unaffected side only
(b) Maintain anatomical positioning by using pillows between legs and back for support.
(4) Prevent dislocation after ORIF for femoral neck fracture (less stable because capsule of hip interrupted).
(a) Avoid hip flexion greater than 90 °.
(b) Avoid hip adduction by placing abduction devices between legs.
(c) Avoid extremes in rotation with trochanter roll.
(d) Provide overhead trapeze to aid patient movement.
c. Prevent extremity edema.
(1) Elevate extremity above level of heart using pillows.
(2) Avoid direct pressure in popliteal fossa.
d. Monitor wound drainage.
(1) Maintain patency of drainage device if present.
(2) Expect pattern of decreasing drainage after first 2 to 4 hours postoperatively.
(3) Assess for dependent drainage underneath operative site and for drainage on dressing or cast.
(4) Maintain occlusive compression dressing, reinforcing if needed.
e. Monitor for complications after femoral fracture.
(1) Infection
(a) Most common with open fracture
(b) Assess for systemic signs or symptoms of infection.
(c) Assess for local signs of infection (visibly reddened incision line).
(d) Identify high-risk patient.
(i) Malnourished
(ii) Infirm
(iii) Incontinent
(iv) Urinary tract infection present
(v) Tooth abscess present
(2) DVT—high risk in patients who are:
(a) Elderly
(b) Dehydrated
(c) Immobile
(d) History of DVT
(3) PE: high risk as for DVT
(4) Compartment syndrome—high risk in patients with:
(a) Prolonged limb compression
(b) Extensive soft tissue trauma
(c) Vascular trauma
(d) Sepsis
(5) FES—high risk in patients with:
(a) Fracture of midshaft femur
(b) Fractures associated with sepsis or shock
E. Arthroscopy
1. Procedure: examination of interior of joint with small fiberoptic tube in effort to visualize accurately or treat joint cavity
2. Purpose
a. Diagnosis of pathological condition
(1) Direct visualization
(a) Articular surfaces
(b) Synovium
(c) Supportive tissue
(d) Foreign tissue
(2) Biopsy of synovium
b. Treatment of pathological condition
(1) Repair or resection of torn menisci
(2) Debridement of cartilage
(3) Removal of foreign body
(4) Arthroscopic-assisted ligament repair
(5) Fixation of minor damage to cartilage
3. Joints amenable to arthroscopy
a. Knee: most common
b. Hip
c. Ankle
d. Shoulder
e. Elbow
f. Temporomandibular joint
4. Postanesthesia care
a. Assess neurovascular status: perform comprehensive neurovascular assessment.
b. Assess multiple portal sites.
(1) Monitor dressing for drainage.
(2) Maintain original dressing, reinforce with additional bulky dressing, and Ace wrap if needed.
c. Prevent extremity edema.
(1) Elevate extremity above level of heart with pillows.
(2) Avoid direct pressure in popliteal fossa.
d. Monitor for postarthroscopy complications.
(1) Infection
(a) Monitor portal sites for:
(i) Redness
(ii) Swelling
(iii) Pain
(iv) Erythema
(v) Most common complication: superficial infection
(b) Instruct patient in manifestation of signs and symptoms of systemic and deep infection: uncommon, occurring more than 24 hours postoperatively.
(2) Major complications: rare but may include DVT, PE, and compartment syndrome
e. Instruct patient regarding use of crutches.
f. Provide for pain control.
(1) Oral opioids commonly used postoperatively
(2) Parenteral patient-controlled analgesia may be used for 24 hours when more extensive joint repair performed (e.g., ACL repair).
g. Position joint and allow for movement per order.
(1) Avoid direct pressure under joint and on bony prominences.
(2) Encourage active range of motion to all unaffected joints.
(3) Provide CPM machine per order.
(4) Provide for joint support with hinged brace or other device per order.
F. ACL repair
1. Most frequently injured or torn ligament in knee joint
a. Research supports increased ACL injury in female athletes.
(1) ACL contains hormone receptor sites for:
(a) Estrogen
(b) Progesterone
(c) Relaxin
(2) Injuries seen more during menses, when estrogen causes ligament to relax
2. Procedure: reconstruction may be arthroscopically assisted or as open arthrotomy. Graft choices for reconstruction include:
a. Autogenous
(1) Patellar tendon—graft of choice, most reliable
(2) Semitendinous tendon
(3) Iliotibial band
(4) Gracilis muscle
(5) Fascia lata
b. Allograft—tissue from cadaver
(1) Less painful for patient
(2) Possibility of graft rejection
c. Ligament substitutes
(1) Scaffolds—protect soft tissue; allow ingrowth
(2) Synthetic ligaments—prone to mechanical failure, usually used as last resource
(a) Gore-Tex (polytetrafluoroethylene/Teflon), braided
(b) Polyester—woven, mesh
3. Purpose
a. Improve joint stability by strengthening anterior-posterior control of knee.
4. Complications of ACL repair
a. Compartment syndrome
b. Neurovascular impairment from inadvertent suturing of peroneal nerve, resulting in possible footdrop, decreased sensation to foot
c. Prolonged tourniquet time could cause sciatic or femoral nerve palsy.
d. Rare—fracture to femur or sprain to ligaments from leg brace used intraoperatively
e. Pain from use of tourniquet and leg brace intraoperatively
f. Rare—hemarthrosis and thromboembolism
5. Postanesthesia care of patient with ACL repair
a. Assess neurovascular status.
b. Assess wound drainage; check dressing and drain.
c. Position leg to decrease edema, pain.
d. Begin cryotherapy, CPM as directed.
(1) Cold from cryotherapy decreases:
(a) Inflammation
(b) Pain
(c) Swelling
(d) Potential for postoperative bleeding with hematoma formation and muscle spasm
e. Keep knee immobilizer on to stabilize joint.
f. Aggressively manage pain.
(1) Multimodal, preemptive pharmacological approach most effective
(a) Intra-articular injection of local anesthetics, opioids, NSAIDs, clonidine, and/or corticosteroids before incision made
(b) Opioid receptors (mu, delta, kappa) found in peripheral nerves and play role in preventing and/or diminishing postoperative pain
(c) Joint medication injection
(i) Local anesthetics (bupivacaine) manage pain approximately 2 to 4 hours.
(ii) Opioids such as morphine, 2 to 5 mg, injected into the joint may last up to 8 to 12 hours without systemic side effects.
(iii) Using a combination approach provides early onset and longer duration of analgesia.
(iv) Intra-articular meperidine has been shown to cause systemic side effects, but does appear to have an earlier onset than morphine.
(d) Corticosteroids (methylprednisolone) and NSAIDs (ketorolac) provide analgesia by diminishing the inflammatory response after arthroscopic knee surgery.
(e) Clonidine increases duration time of intra-articular morphine and local anesthetics.
(f) Effective pain management promotes quicker healing and increased compliance with rehabilitation programs.
(g) Use of preemptive analgesia reduces opioid use postoperatively.
(2) Femoral block, no weight bearing until worn off
(a) Average length of analgesia: 29 hours
(3) Postoperative NSAIDs and opioids as directed
(a) Controlled-release oxycodone (OxyContin): twice-per-day dosing schedule
(i) Provides extended pain relief
(ii) Promotes increased patient compliance
(4) Epidural analgesia—allows for:
(a) Earlier ambulation
(b) More comfort during rehabilitation
(c) Improved pulmonary function
G. Amputation
1. Procedure: surgical (or traumatic) removal of a body part
2. Purpose
a. Reduce risk of systemic sepsis
b. Control pain of ischemia
c. Maximize mobility
3. Types of amputation
a. Traumatic: results in extreme destruction of soft tissue and bone in presence of infectious microorganisms
b. Elective
(1) Closed (flap): performed in absence of infection
(2) Open (guillotine): performed in presence of infection, allowing drainage of infectious material
4. Indications for elective amputation
a. Peripheral vascular disease: most frequent indication for lower extremity amputation, often associated with diabetes mellitus
b. Severe trauma: most frequent indication for upper extremity amputation
c. Other indications (in order of frequency)
(1) Acute or chronic infection: osteomyelitis or gangrene
(2) Trophic ulcers
(3) Severe crushing injuries
(4) Malignancies
(5) Frostbite
(6) Congenital deformities
5. Postanesthesia care of patient after amputation
a. Assess neurovascular status: perform comprehensive neurovascular assessment.
b. Assess for signs of wound drainage.
(1) Note dependent drainage on dressing and bed.
(2) Note unusual odors or color of drainage (important in presence of infection).
c. Maintain stump dressing.
(1) Plaster cast: rigid dressing
(a) Prevents swelling of stump
(b) Protects stump from trauma
(c) Used when patient will be fitted for immediate prosthesis (usually Pylon type)
(2) Soft dressing: gauze with elastic wrap
(a) Prevents swelling of stump
(b) Used when use of prosthesis unlikely
d. Position extremity to minimize complications.
(1) Elevate stump to facilitate venous return first 24 to 48 hours.
(2) After 48 hours, position to prevent hip flexion contractures.
(a) Avoid stump elevation.
(b) Instruct patient to lie intermittently prone (encourages hip extension).
e. Provide for pain control.
(1) Administer parenteral opioids as ordered for postoperative surgical pain.
(2) Assess for phantom limb pain.
(a) Pain sensation in area of absent, amputated limb
(b) Common in first 24 to 48 hours postoperatively in traumatic amputation
(c) Treated with opioids and phenytoin
(d) Adequate treatment important to reduce risk of chronic phantom pain syndrome
f. Instruct patient regarding phantom limb sensation: sensation that amputated limb present.
(1) Inform patient that phenomenon is common in early postoperative period.
(2) Instruct patient that sensation is normal phenomenon.
(3) Treat with nonpharmacological methods.
g. Provide emotional support.
H. Replantation of amputated digits or limbs
1. Procedure: reattachment of totally or partially amputated part involving restoration of structures
a. Vascular
b. Nervous
c. Bony
d. Soft tissue
2. Possible sites for replantation
a. Upper extremity
(1) Digits
(a) Most common traumatic amputation
(b) Replantation attempted in:
(i) Proximal digit amputations
(ii) Amputation of multiple digits
(iii) Amputation of index finger or thumb
(c) Viability after replantation: 80% to 90%
(d) Functional return after replantation: 65%
(2) Arms: less successful result
b. Lower extremity
(1) Digits: great toe
(2) Leg
(a) Amputation through tibia or fibula shows unfavorable results with high infection rate.
(b) Leg length discrepancies common
3. Factors influencing prognosis
a. Positive factors
(1) Clean-cut (guillotine) amputation
(2) Young patient
(3) Hemodynamically stable patient
(4) Absence of systemic disease
(5) No history of smoking, alcohol, or drug abuse
(6) Absence of gross contamination of wound
(7) Amputated part wrapped in gauze and placed in cool environment
(8) Replantation attempted within 24 hours
b. Negative factors
(1) Crushing injury
(2) Extremes of age
(3) History of peripheral vascular disease, hypertension, or other chronic illness
(4) History of smoking, alcohol, or drug abuse
(5) Grossly contaminated wound
(6) Delay in retrieval and care of amputated part
(7) Delay in replantation
4. Postanesthesia care of patient postreplantation
a. Assess neurovascular status at least every 15 minutes.
(1) Perform comprehensive bedside assessment.
(2) Perform technical monitoring as ordered.
(a) Doppler ultrasonography
(b) Temperature probes
(c) Muscle contraction monitoring (evoked M wave)
(d) Fluorometry readings (determines venous return)
(3) Promptly notify physician if negative change occurs.
b. Promote circulation and prevent vasoconstriction.
(1) Elevate extremity above heart level.
(2) Administer thrombolytic agents to decrease clotting in peripheral vessels.
(3) Maintain room temperature at 78 ° F to 90 ° F (26 ° C to 30 ° C).
(4) Prevent patient exposure to nicotine and caffeine.
(5) Maintain patient hydration.
c. Prevent infection.
(1) Administer antibiotics as ordered.
(2) Assess for signs and symptoms of infection.
(3) Provide for nutritional needs necessary for wound healing (high-protein diet).
d. Provide for pain control.
(1) Provide oral opioids as needed.
(2) Assess pain, while noting that changes in pain pattern may be suggestive of ischemia.
e. Provide emotional support.
f. Complications
(1) Venous congestion
(a) Massage digit.
(b) Leech therapy
(c) Revision of replantation
(2) Thrombosis
(a) Anticoagulants
(b) Revise surgically.
(3) Sepsis
(4) Renal failure
(5) Contractures
(6) Diminished or lost proprioception
I. Nursing interventions
1. Upper extremity procedures
a. Position the hand above heart.
b. Provide a sling if ordered.
c. Assess and protect cast and splint.
(1) Cast should be kept dry.
(2) Observe for cast defects that could lead to tissue compression damage.
d. Apply ice packs as ordered.
e. Check neurovascular status.
(1) Nerve function
(a) Radial
(i) Check sensation at thumb–index finger web.
(ii) Have patient hyperextend thumb or wrist.
(b) Median
(i) Check sensation on distal surface of index finger.
(ii) Have patient oppose thumb and finger.
(c) Ulnar
(i) Check sensation at distal end of small finger.
(ii) Have patient abduct all fingers.
(2) Vascular status—assess capillary refill.
(a) Normal capillary refill: 3 seconds or less
(b) Perform blanch test.
(i) Compress and release nail bed quickly.
(c) Compare capillary refill with unaffected extremity.
(d) Rapid filling may indicate venous congestion.
(e) Sluggish filling is a sign of arterial insufficiency.
(f) Note color, comparing with unaffected extremity.
(i) Blanching or pallor indicates arterial insufficiency.
(g) Cyanosis indicates insufficient venous return.
(3) Mobility
(a) Within limitations of casts, splints, and so forth, have patient wiggle fingers.
(i) Should be easy
(ii) Should not be painful
2. Lower extremities
a. Position extremity above heart.
b. Assess and protect cast and splint.
(1) Cast should be kept dry.
(2) Observe for cast defects that could lead to tissue compression damage.
c. Apply ice packs or cooling device as ordered.
d. Check neurovascular status frequently.
(1) Nerve function—peroneal
(a) Check sensation at lateral surface of great toe and medial surface of second toe.
(b) Have patient dorsiflex ankle and extend toes.
(c) Peroneal nerve damage results in foot drop.
(2) Nerve function—tibial
(a) Check sensation at medial and lateral surfaces of sole of foot.
(b) Have patient plantar flex ankle and flex toes.
(c) Signs and symptoms of nerve damage
(i) Pain that is:
[a] Increasing
[b] Persistent
[c] Localized
(ii) Paresthesia
(iii) Hyperesthesia
(iv) Numbness
(v) Motor weakness
(vi) Paralysis
(3) Vascular status
(a) Perform blanch test.
(i) Compress and release nail bed quickly.
(ii) Compare capillary refill with unaffected extremity.
(iii) Rapid filling may indicate venous congestion.
(iv) Sluggish filling is a sign of arterial insufficiency.
(b) Note color, comparing with unaffected extremity.
(i) Blanching or pallor indicates arterial insufficiency.
(ii) Cyanosis indicates insufficient venous return.
(c) Signs and symptoms of nerve damage
(i) Loss of pulse
(ii) Sluggish or absent capillary refill
(iii) Pallor
(iv) Cyanosis
(v) Blanching
(vi) Temperature decrease
(vii) Paresthesia
(viii) Hyperesthesia
(4) Mobility
(a) Within limitations of casts, splints, and so forth, have patient wiggle toes.
(i) Should be easy
(ii) Should not be painful
(b) Severe pain on dorsiflexion of toes can indicate compartment syndrome.
BIBLIOGRAPHY
1. Baird, C., First line treatment for osteoarthritis, part 1: Pathophysiology, assessment, and pharmacologic interventions, Orthop Nurs 20 (5) ( 2001) 17–24.
2. Bert, J.M., Unicompartmental knee replacement, Orthop Clin North Am 36 (4) ( 2005) 513–522.
3. Crovetti, M.; Tarno, J., Birmingham Hip Resurfacing System, www.hipsurfacing.com; Available at: Accessed January 12, 2009..
4. Burden, N., Care of the orthopedic patient in the ambulatory surgery setting, J Perianesth Nurs 22 (3) ( 2007) 207–210.
5. Cascio, B.; Wilckens, J.; Ain, M.; et al., Documentation of acute compartment syndrome at an academic health care center, J Bone Joint Surg 87 (2) ( 2005) 346–350.
6. Center Orthopedic & Neurosurgical Care & Research, www.neuro-ortho.com; Available at: Accessed January 12, 2009..
7. Cluett, J., ACL reconstruction-graft choices for ACL surgery, About.com; Available at: Accessed 2006..
8. Drain, C.B.; Odom-Forren, J., Care of the orthopedic surgical patient, In: (Editors: Drain, C.B.; Odom-Forren, J.) Perianesthesia nursing: A critical care approached 5 ( 2009)Saunders, Philadelphia.
9. Hodgson, B.B.; Kizior, R.J., Saunders 2010 nursing drug handbook. ( 2010)Saunders, Philadelphia.
10. Iacono, M.V., Osteoporosis: A national public health priority, J Perianesth Nurs 22 (3) ( 2007) 175–183.
11. Mamaril, E.M.; Childs, S.G.; Sortman, S., Care of the orthopaedic trauma patient, J Perianesth Nurs 22 (3) ( 2007) 184–194.
12. Nagelhout, J.J.; Plaus, K.L., Handbook of nurse anesthesia. ed 4 ( 2010)Saunders, Philadelphia.
13. Pasero, C.; McCaffery, M., Orthopaedic postoperative pain management, J Perianesth Nurs 22 (3) ( 2007) 160–174.
14. Rothrock, J.C., Alexander’s care of the patient in surgery. ed 13 ( 2007)Mosby, St Louis.
15. Worth, M.A.; Tapscott, R.S.; Southworth, C.; et al., Treatment of glenohumeral arthritis with hemiarthroplasty surgical technique, J Bone Joint Surg 89 (2 Suppl 1) ( 2007) 10–25.
16. Yeung, A.T.; Yeung, C.A., Minimally invasive techniques for the management of lumbar disc herniation, Orthop Clin North Am 38 (3) ( 2007) 363–372.





