Defibrillation (External)
PREREQUISITE NURSING KNOWLEDGE
• Understanding of the anatomy and physiology of the cardiovascular system, principles of cardiac conduction, basic dysrhythmia interpretation, and electrical safety is needed.
• Basic and advanced cardiac life support (ACLS) knowledge and skills are necessary.
• Clinical and technical competence in the use of the defibrillator is needed.
• Ventricular fibrillation and pulseless ventricular tachycardia are lethal dysrhythmias. Early emergent defibrillation is the treatment of choice to restore normal electrical activity and coordinated contractile activity within the heart.2,8
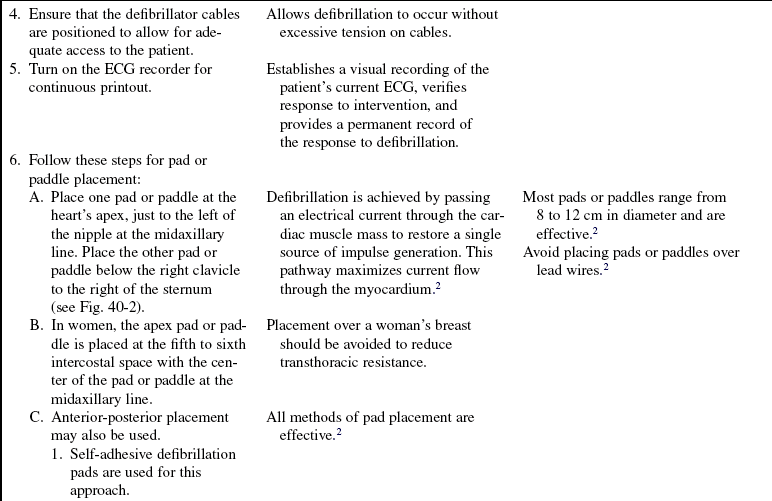
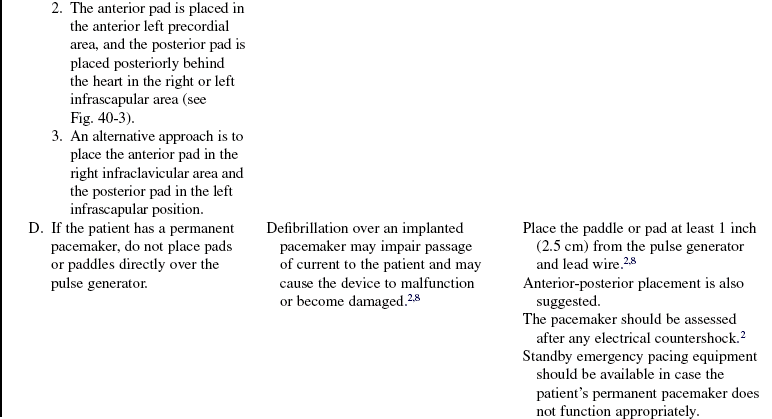
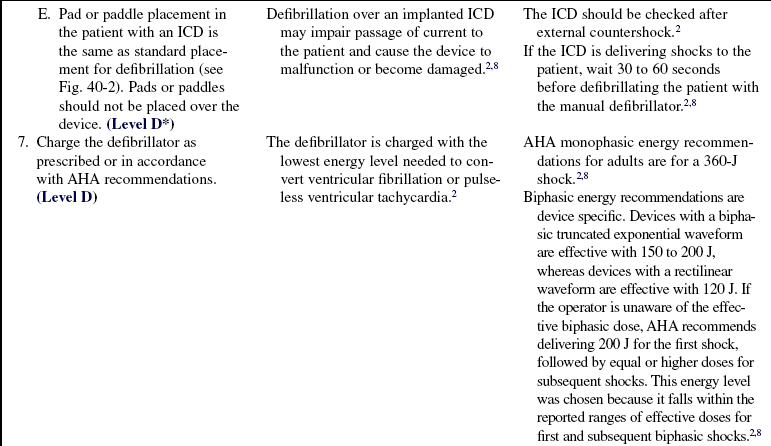
• The electrical current delivered with defibrillation depolarizes the myocardium, terminating all electrical activity and allowing the heart’s normal pacemaker to resume electrical activity within the heart.2,8 Defibrillator paddles or pads placed over the patient’s chest wall surface in the anterior-apex or anterior-posterior position maximize the current flow through the myocardium.2
• Defibrillators deliver energy or current in waveform patterns. Delivered energy levels may differ between different defibrillators and waveforms. Various types of monophasic waveforms are used in older defibrillators. Biphasic waveforms have been designed more recently and are used currently in implantable cardioverter defibrillators (ICDs), automatic external defibrillators, and most manual defibrillators.
• Monophasic waveforms deliver energy in one direction. The energy travels through the heart from one paddle or pad to the other.2
• Biphasic waveforms deliver energy in two directions. The energy travels through the heart in a positive direction and then reverses itself and flows back through the heart in a negative direction.10 Researchers have found that biphasic waveform technology is able to decrease the amount of current needed to terminate the dysrhythmia (less than or equal to 200 J), decreasing the amount of potential damage to the myocardium.7,13 Researchers also found that 115- to 130-J biphasic waveform shocks achieved the same first shock success rate as 200-J monophasic waveform shocks and these shocks also produced less ST-segment change than the monophasic shocks.1,7 Investigators from in-hospital and out-of-hospital studies concluded that repetitive lower energy biphasic waveform shocks had equal or higher success rates for eradicating ventricular fibrillation than defibrillators that increase the current with each shock (200 J, 300 J, 360 J).1,2 More research is needed to determine a specific recommendation for the optimal energy level for biphasic waveform defibrillation.1,2,7 Biphasic energy recommendations are device specific. Biphasic defibrillators use one of two waveforms. Devices with a biphasic truncated exponential waveform are effective with 150 to 200 J of energy, whereas devices with a rectilinear waveform are effective with 120 J of energy. If the operator is unaware of the effective biphasic dose, the American Heart Association (AHA) recommends delivery of 200 J for the first shock, followed by equal or higher doses for subsequent shocks.2,8 This energy level was chosen because it falls within the reported ranges of effective doses for first and subsequent biphasic shocks.2,8
• Biphasic defibrillators measure and compensate for transthoracic impedance before the delivery of the shock, which allows the defibrillator to deliver the actual amount of energy selected by the rescuer.1,2
• A wearable cardioverter defibrillator (WCD) has recently been developed for patients at high risk for sudden cardiac death. Patient populations may include those who do not meet the current guidelines for an ICD implantation but who are at risk; those who are unable to receive an ICD because of infection; and those patients at high risk who are awaiting cardiac transplant. This wearable defibrillator has the ability to detect and treat life-threatening tachydysrhythmias without bystander support and allows the patient to ambulate freely. The initial defibrillators were programmed to provide a monophasic waveform for shocks. Preliminary results have shown that WCD is a safe and effective method to terminate life-threatening dysrhythmias in this high-risk patient population. The next generation devices use biphasic shocks, which are also proving to be successful in terminating ventricular fibrillation.11
EQUIPMENT
• Defibrillator with electrocardiogram (ECG) oscilloscope/recorder
• Conductive gel, paste, or prepackaged gelled conduction pads or self-adhesive defibrillation pads connected directly to the defibrillator
• Bag-valve device with mask and oxygen delivery
• Flow meter for oxygen administration, oxygen source
• Emergency suction and intubation equipment
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Teaching may need to be performed after the procedure.  Rationale: If emergent defibrillation is performed in the face of hemodynamic collapse, education may be impossible until after the procedure has been performed.
Rationale: If emergent defibrillation is performed in the face of hemodynamic collapse, education may be impossible until after the procedure has been performed.
• Assess patient and family understanding of the etiology of the dysrhythmia.  Rationale: This assessment determines the patient and family understanding of the condition and guides additional educational needs.
Rationale: This assessment determines the patient and family understanding of the condition and guides additional educational needs.
• Explain the procedure to the patient and the family.  Rationale: This explanation decreases anxiety and promotes understanding.
Rationale: This explanation decreases anxiety and promotes understanding.
• Explain to the patient and the family the signs and symptoms of hemodynamic compromise associated with preexisting cardiac dysrhythmias.  Rationale: This explanation enables the patient and the family to recognize when to contact the nurse or physician.
Rationale: This explanation enables the patient and the family to recognize when to contact the nurse or physician.
• Evaluate and discuss with the patient the need for long-term pharmacologic support.  Rationale: This evaluation and discussion allows the nurse to anticipate educational needs of the patient and family regarding specific discharge medications.
Rationale: This evaluation and discussion allows the nurse to anticipate educational needs of the patient and family regarding specific discharge medications.
• Assess and discuss with the patient the need for lifestyle changes.  Rationale: Underlying pathophysiology may necessitate alterations in the patient’s current lifestyle and require a plan for behavioral changes.
Rationale: Underlying pathophysiology may necessitate alterations in the patient’s current lifestyle and require a plan for behavioral changes.
• Assess and discuss with the patient the need as applicable for an ICD.  Rationale: Life-threatening dysrhythmias may persist after initial defibrillation and pharmacologic interventions.4
Rationale: Life-threatening dysrhythmias may persist after initial defibrillation and pharmacologic interventions.4
• Assess and discuss with the patient the need as applicable for an emergency communication system.  Rationale: People with recurrent life-threatening dysrhythmias are at risk for cardiac arrest.4
Rationale: People with recurrent life-threatening dysrhythmias are at risk for cardiac arrest.4
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the ECG results for tachydysrhythmias, including paroxysmal supraventricular tachycardia, atrial fibrillation, atrial flutter, atrial tachycardia, and ventricular tachycardia.  Rationale: Tachydysrhythmias often precede ventricular fibrillation, can be life-threatening, and can precipitate deterioration of hemodynamic stability.2
Rationale: Tachydysrhythmias often precede ventricular fibrillation, can be life-threatening, and can precipitate deterioration of hemodynamic stability.2
• Assess the ECG results for ventricular fibrillation.  Rationale: Ventricular fibrillation is life-threatening; if not terminated immediately, death ensues.2
Rationale: Ventricular fibrillation is life-threatening; if not terminated immediately, death ensues.2
• Assess vital signs.  Rationale: Blood pressure and pulse are absent in the presence of ventricular fibrillation because of the loss of cardiac output.2
Rationale: Blood pressure and pulse are absent in the presence of ventricular fibrillation because of the loss of cardiac output.2
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teachings (if time is available). Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• If possible, ask a member of pastoral care or another designated healthcare provider to provide support for family members during the procedure.  Rationale: Pastoral care team members or the clergy may provide support to ease family members’ anxiety during the procedure.
Rationale: Pastoral care team members or the clergy may provide support to ease family members’ anxiety during the procedure.
• Remove all metallic objects from the patient.  Rationale: Metallic objects are excellent conductors of electrical current and could result in burns.
Rationale: Metallic objects are excellent conductors of electrical current and could result in burns.
• Remove transdermal medication patches from the patient’s chest or ensure the defibrillator pad or paddle does not touch the patch.  Rationale: Transdermal medication patches may block the transfer of energy from the pad or paddle to the patient and produce a chest burn when the pad or paddle is placed over it.2,8
Rationale: Transdermal medication patches may block the transfer of energy from the pad or paddle to the patient and produce a chest burn when the pad or paddle is placed over it.2,8
• Ensure that the patient is in a dry environment, and dry the patient’s chest, if it is wet.  Rationale: Water is a conductor of electricity. If the patient and rescuer are in contact with water, the rescuer may receive a shock or the patient may receive a skin burn. Also, if the patient’s chest is wet, the current may travel from one paddle across the water to the other, resulting in a decreased amount of energy to the myocardium.2,8
Rationale: Water is a conductor of electricity. If the patient and rescuer are in contact with water, the rescuer may receive a shock or the patient may receive a skin burn. Also, if the patient’s chest is wet, the current may travel from one paddle across the water to the other, resulting in a decreased amount of energy to the myocardium.2,8
• If the patient has a hairy chest, clipping or removing the hair from the chest (if time is available) may be necessary.  Rationale: This action allows the electrodes to adhere to the chest.2,8 Chest hair has been known to increase transthoracic impedance in patients.12,14
Rationale: This action allows the electrodes to adhere to the chest.2,8 Chest hair has been known to increase transthoracic impedance in patients.12,14
• Initiate basic life support (BLS) if immediate defibrillation is not available.  Rationale: Basic life support maintains cardiac output to diminish irreversible organ and tissue damage.2
Rationale: Basic life support maintains cardiac output to diminish irreversible organ and tissue damage.2
• Oxygenate the patient with a bag-valve device with mask and 100% oxygen.  Rationale: Adequate oxygenation diminishes the risk of cerebral and cardiac complications.3,8
Rationale: Adequate oxygenation diminishes the risk of cerebral and cardiac complications.3,8
• Place the defibrillator in the defibrillation mode.  Rationale: The defibrillation mode must be set to disperse the electrical charge randomly because the synchronization mode does not fire in the absence of a QRS complex.
Rationale: The defibrillation mode must be set to disperse the electrical charge randomly because the synchronization mode does not fire in the absence of a QRS complex.
References
![]() 1. AHA, Low-energy biphasic waveform defibrillation. -evidence-based review applied to emergency cardiovascular care guidelines; a statement for healthcare professionals from the American Heart Association Committee on Emergency Cardiovascular Care and the Subcommittees on Basic Life Support, Advanced Cardiac Life Support and Pediatric Resuscitation. Circulation 1998; 97:1654–1667.
1. AHA, Low-energy biphasic waveform defibrillation. -evidence-based review applied to emergency cardiovascular care guidelines; a statement for healthcare professionals from the American Heart Association Committee on Emergency Cardiovascular Care and the Subcommittees on Basic Life Support, Advanced Cardiac Life Support and Pediatric Resuscitation. Circulation 1998; 97:1654–1667.
![]() 2. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 5. electrical therapiesautomated external -defibrillators, defibrillation, cardioversion, and pacing. Circulation. 2005; 112(Suppl IV):IV-35–46.
2. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 5. electrical therapiesautomated external -defibrillators, defibrillation, cardioversion, and pacing. Circulation. 2005; 112(Suppl IV):IV-35–46.
![]() 3. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 7. 1. adjuncts for airway control and ventilation. Circulation. 2005; 112(Suppl IV):IV-51–57.
3. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 7. 1. adjuncts for airway control and ventilation. Circulation. 2005; 112(Suppl IV):IV-51–57.
![]() 4. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 7. 2. management of cardiac arrest. Circulation. 2005; 112(Suppl IV):IV-58–66.
4. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 7. 2. management of cardiac arrest. Circulation. 2005; 112(Suppl IV):IV-58–66.
![]() 5. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 7. 4. monitoring and medications. Circulation. 2005; 112(Suppl IV):IV-78–83.
5. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 7. 4. monitoring and medications. Circulation. 2005; 112(Suppl IV):IV-78–83.
![]() 6. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 7. 5. postresuscitation support. Circulation. 2005; 112(Suppl IV):IV-84–88.
6. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 7. 5. postresuscitation support. Circulation. 2005; 112(Suppl IV):IV-84–88.
![]() 7. Faddy, SC, et al, Biphasic and monophasic shocks for transthoracic defibrillation. a meta analysis of randomized controlled trials. Resuscitation 2003; 58:9–16.
7. Faddy, SC, et al, Biphasic and monophasic shocks for transthoracic defibrillation. a meta analysis of randomized controlled trials. Resuscitation 2003; 58:9–16.
8. Field, JM. Advanced cardiac life support provider manual. Dallas: American Heart Association; 2006.
![]() 9. Graham-Garcia, J, et al, Defibrillation and biphasic shocks. implications for perianesthesia nursing. J Perianesth Nurs. 2005; 20(1):23–34.
9. Graham-Garcia, J, et al, Defibrillation and biphasic shocks. implications for perianesthesia nursing. J Perianesth Nurs. 2005; 20(1):23–34.
![]() 10. Mair, M, Monophasic and biphasic defibrillators. the evolving technology of cardiac defibrillation. Am J Nurs. 2003; 103(8):58–60.
10. Mair, M, Monophasic and biphasic defibrillators. the evolving technology of cardiac defibrillation. Am J Nurs. 2003; 103(8):58–60.
![]() 11. Reek, S, et al. Clinical efficacy of a wearable defibrillator in acutely terminating episodes of ventricular fibrillation using biphasic shocks. PACE. 2003; 26:2016–2022.
11. Reek, S, et al. Clinical efficacy of a wearable defibrillator in acutely terminating episodes of ventricular fibrillation using biphasic shocks. PACE. 2003; 26:2016–2022.
![]() 12. Sado, DM, et al. Comparison of the effects of removal of chest hair with not doing so before external defibrillation on transthoracic impedance. Am J Cardiol. 2004; 93:98–100.
12. Sado, DM, et al. Comparison of the effects of removal of chest hair with not doing so before external defibrillation on transthoracic impedance. Am J Cardiol. 2004; 93:98–100.
![]() 13. White, RD. New concepts in transthoracic defibrillation. Emerg Med Clin North Am. 2002; 20:785–807.
13. White, RD. New concepts in transthoracic defibrillation. Emerg Med Clin North Am. 2002; 20:785–807.
![]() 14. White, RD, et al. Transthoracic impedance does not affect defibrillation, resuscitation or survival in patients with out-of-hospital cardiac arrest treated with non-escalating biphasic waveform defibrillator. Resuscitation. 2005; 64:63–69.
14. White, RD, et al. Transthoracic impedance does not affect defibrillation, resuscitation or survival in patients with out-of-hospital cardiac arrest treated with non-escalating biphasic waveform defibrillator. Resuscitation. 2005; 64:63–69.