Arterial-Venous Oxygen Content Difference and Oxygen Transport (Delivery) and Consumption Calculations
PREREQUISITE NURSING KNOWLEDGE
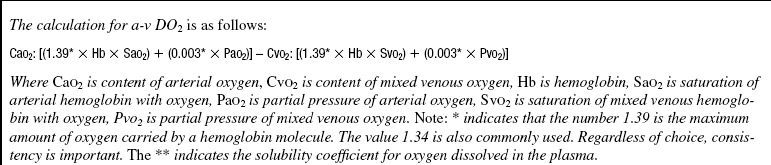
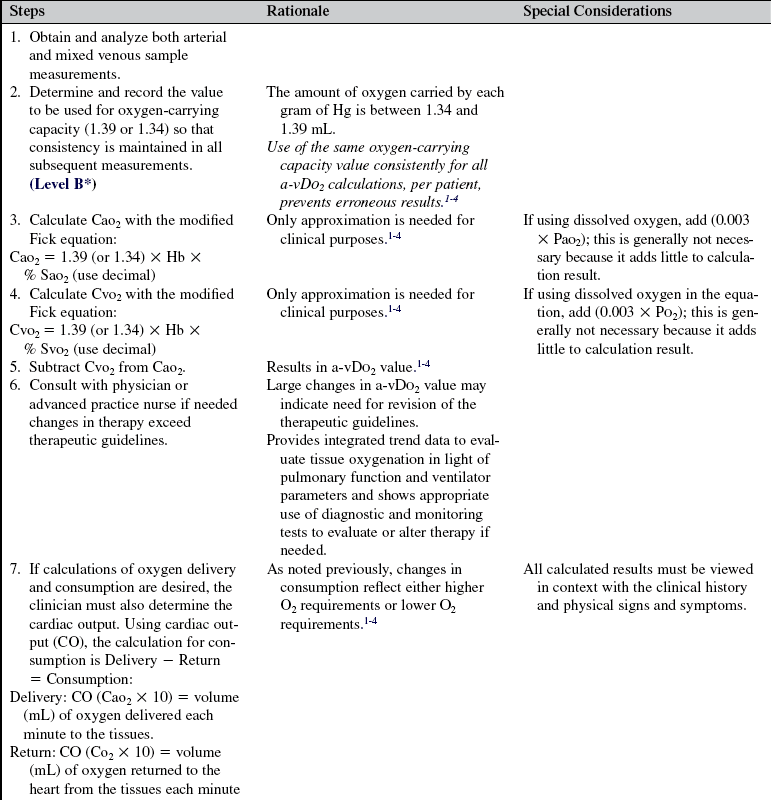
• Most oxygen carried in the blood is bound to hemoglobin and is referred to as oxygen saturation. A small percentage also is dissolved in the plasma. The total blood oxygen content is determined by adding the amount of oxygen bound to hemoglobin to that dissolved in the plasma. Oxygen content can be calculated for the arterial blood (CaO2) and the venous blood (CO2). By calculating the oxygen contents for arterial and venous blood and subtracting them, a rough estimate of oxygen use can be made. This value is either expressed as mL/dL or as vol %. A normal arterial-venous oxygen content difference (a-vDO2) is 5 vol % (range, 4 to 6 vol %). In general, because the contribution of dissolved oxygen is slight, it is not used clinically to calculate CaO2.3,4 It is essential to remember that hemoglobin is one of the most important variables in oxygenation status.
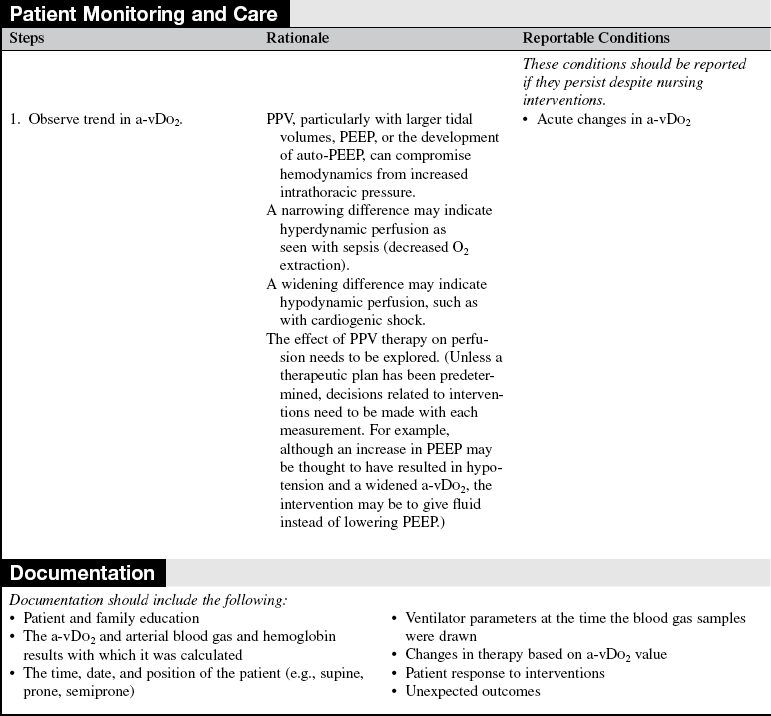
• The partial pressure of mixed venous oxygen pressure (PO2) and mixed venous oxygen saturation (SO2) reflects tissue oxygenation under most conditions. When blood flow does not increase to meet higher tissue oxygen demands (as in hypodynamic conditions [e.g., shock]), more oxygen is extracted from the arterial blood, and the PO2 and SO2 decrease. The gradient between CaO2 and CO2 widens. Conversely, when blood flow is increased (e.g., hyperdynamic flow, as in sepsis), less oxygen is extracted from the arterial blood; PO2 and SO2 increase, and a-vDO2 decreases.3,4
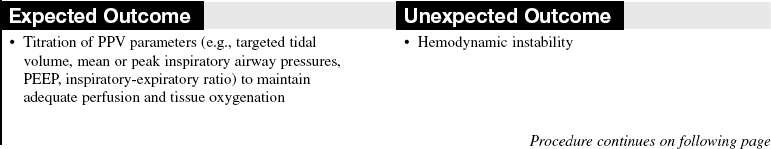
• A major clinical goal of positive-pressure ventilation (PPV) and positive end-expiratory pressure (PEEP) is improved oxygenation. One potential complication of these therapies is hypotension from the effect of increased intrathoracic pressures on venous return.1,2
• Calculation of a-vDO2 may reflect tissue oxygenation in some cases; however, it is not a direct measurement and can be used only for approximation. The measurement of lactic acid is thought to be a more accurate assessment of tissue hypoxia, but the formation of lactic acid occurs late in the clinical course and is often irreversible.2 It slowly clears on improvement of the patient’s condition.
• In addition to hemoglobin, one of the most important variables affecting oxygen use is cardiac output. When cardiac output is inadequate, more oxygen is extracted from the arterial blood, which lowers the CO2.
• The product of cardiac output and CaO2 is oxygen delivery. Oxygen consumption may be calculated by determining the product of cardiac output and a-vDO2.1–4
• Measurement of cardiac output is necessary for oxygen delivery and oxygen consumption calculations (see Procedure 67).
• Normal values for oxygen delivery and consumption are approximately 1000 mL O2/min and 250 mL O2/min, respectively.1–4
• Confirmation of pulmonary artery catheter placement is necessary to ensure accuracy of measurements (see Procedure 73).1,2
• Calculation of the a-v difference requires the sampling of arterial blood from an indwelling arterial line or arterial puncture (see Procedures 64 and 80) and mixed venous blood from a pulmonary artery catheter (see Procedure 66).1,2
EQUIPMENT
PATIENT AND FAMILY EDUCATION
• Inform the patient and the family of the patient’s perfusion status and changes in therapy and interpret the changes. If the patient or another family member requests specific information about arterial venous oxygen content differences, explain the general relationship between a-vDO2 and perfusion.  Rationale: Most patients and families are less concerned with the diagnostic and therapeutic details and more concerned with how the patient’s condition is progressing overall or in relation to a specific physiologic function.
Rationale: Most patients and families are less concerned with the diagnostic and therapeutic details and more concerned with how the patient’s condition is progressing overall or in relation to a specific physiologic function.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess signs and symptoms of inadequate tissue oxygenation:
 Rationale: Calculations of a-vDO2 and O2 delivery and consumption are indicated to provide a rough quantitative estimate of tissue perfusion and oxygenation.
Rationale: Calculations of a-vDO2 and O2 delivery and consumption are indicated to provide a rough quantitative estimate of tissue perfusion and oxygenation.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient understands preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
References
![]() 1. Chulay, M, Gawlinski, A, AACN protocols for practice. -hemodynamic monitoring series. American Association of Critical-Care Nurses, Aliso Viejo, CA, 1998.
1. Chulay, M, Gawlinski, A, AACN protocols for practice. -hemodynamic monitoring series. American Association of Critical-Care Nurses, Aliso Viejo, CA, 1998.
2. Miller, LR. Hemodynamic monitoring. In: Chulay M, Burns SM, eds. AACN essentials of critical care -nursing. New York: McGraw-Hill, 2006.
3. West, JB, Pulmonary pathophysiology. the essentials. Lippincott Williams & Wilkins, Baltimore, 2008.
4. West, JB, Respiratory physiology. the essentials. ed 8. Lippincott Williams & Wilkins, Baltimore, 2008.