History
Comments
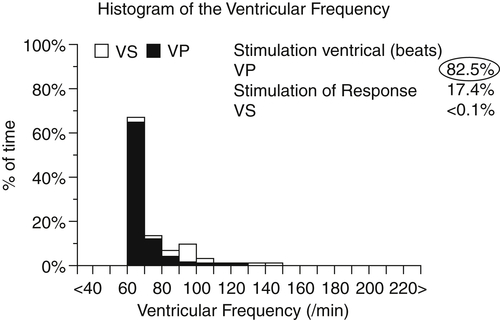
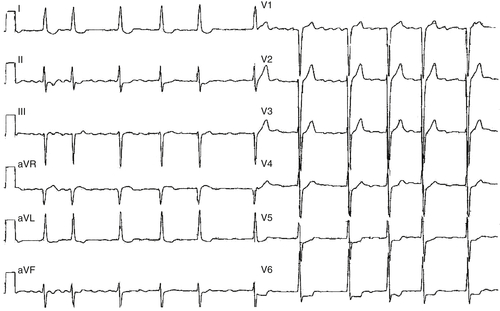
FIGURE 31-1
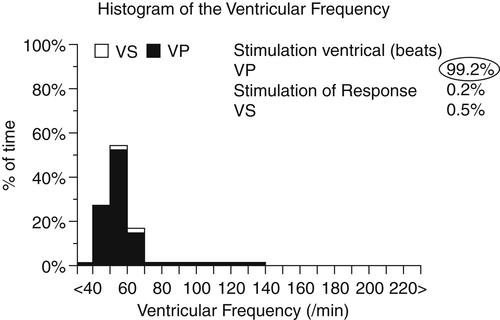
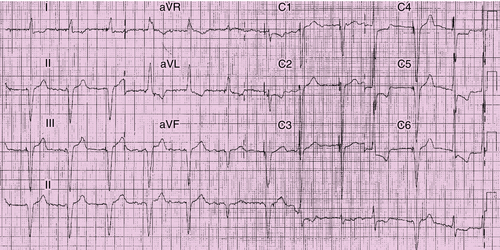
FIGURE 31-2
Current Medications
Comments
Current Symptoms
Comments
Physical Examination
Comments
Laboratory Data
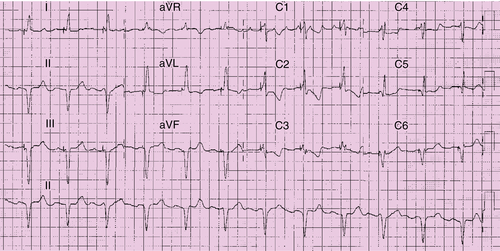
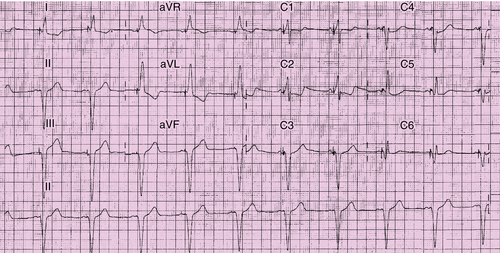
Electrocardiogram
Findings
Comments
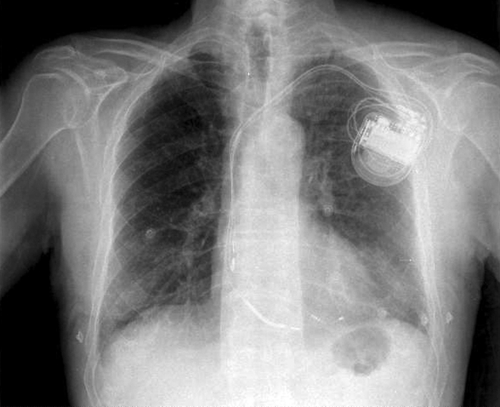
Chest Radiograph
Findings
Exercise Testing
Comments
Echocardiogram
Findings
Comments
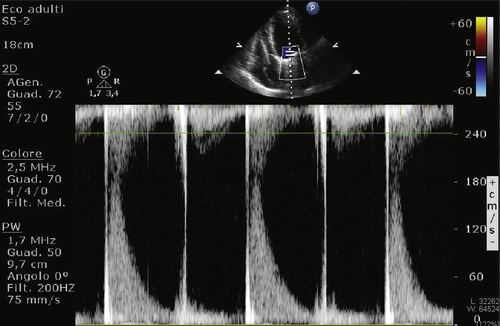
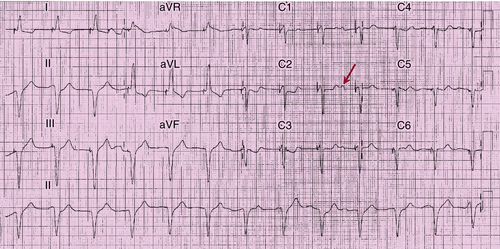
FIGURE 31-9
Findings
Comments
Findings
Comments
Findings
Comments
Focused Clinical Questions and Discussion Points
Question
Discussion
Question
Discussion
Question
Discussion
Final Diagnosis
Plan of Action
Intervention
Outcome
Comments
Selected References
1. Gasparini M., Steinberg J.S., Arshad A. et al. Resumption of sinus rhythm in patients with heart failure and permanent atrial fibrillation undergoing cardiac resynchronization therapy: a longitudinal observational study. Eur Heart J. 2010;31:976–983.
2. Kies P., Leclercq C., Bleeker G.B. et al. Cardiac resynchronisation therapy in chronic atrial fibrillation: impact on left atrial size and reversal to sinus rhythm. Heart. 2006;92:490–494.
3. Vardas P.E., Auricchio A., Blanc J.J. et al. European Society of Cardiology. Guidelines for cardiac pacing and cardiac resynchronization therapy: The Task Force for Cardiac Pacing and Cardiac Resynchronization Therapy of the European Society of Cardiology. Developed in Collaboration with the European Heart Rhythm Association. Eur Heart J. 2007;28:2256–2295.