CHAPTER 25. Postoperative Nausea and Vomiting
Susan Jane Fetzer
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Differentiate nausea, vomiting, and retching.
2. Describe the phases of perianesthesia-related nausea and vomiting.
3. Determine a patient’s risk of experiencing postoperative nausea and vomiting (PONV).
4. Describe the difference between prophylactic and rescue therapy for PONV.
5. List five categories of PONV drugs that work on the chemoreceptor zone.
6. List five nursing interventions in the care of the patient at high risk for PONV or postdischarge nausea and vomiting (PDNV).
7. Describe the importance of risk-adjusted multimodal therapy for PONV.
I DEFINITIONS
A Nausea
1. Subjective sensation in back of throat or epigastrium
2. Conscious cortical activity
3. Conscious awareness of the need to vomit
4. No expulsive muscular movements
5. May not culminate in vomiting
6. Synonyms: sick to my stomach, upset stomach, butterflies, queasy
B Vomiting
1. Objective forceful evacuation of gastric contents through oral or nasal cavity
2. Autonomic reflex directed by brainstem
3. May or may not be preceded by nausea
4. Coordinated muscular movements
5. Associated with physiological changes
a Increased heart rate
b Increased respiratory rate
c Sweating
6. Synonyms
a Pitching
b Barfing
c Ralphing
d Upchucking
e Puking
C Retching
1. An attempt to vomit
2. Nonproductive
3. Synonyms
a Dry heaves
b Gagging
D Vomiting and retching also termed emetic episodes
E PONV
1. Defined as nausea, vomiting, and retching separately or combined
2. Occurs within first 24 hours after inpatient surgery
3. Early PONV: First 2 to 6 hours after surgery
4. Late PONV: After transfer to the postoperative unit, 6 to 24 hours after surgery
F PDNV
1. Occurs after discharge from health care facility
G Delayed PDNV
1. Occurs 24 hours after surgery
II CONSEQUENCES OF PONV
A Physiological
1. Surgical site disruption
2. Esophageal tears
3. Gastric herniation
4. Fatigue
5. Dehydration
6. Electrolyte imbalance
7. Airway compromise with aspiration
8. Increased intracranial pressure
9. Increased ocular pressure
B Delay of oral nutrition and drug therapy
1. Poor pain management
2. Interference with diabetic and antihypertensive drug regimens
3. Potential for dehydration
C Increased costs
1. Each vomiting episode delays discharge from post anesthesia care unit by an average of 20 minutes.
2. Cost of treating vomiting is three times greater than cost of treating nausea.
3. Readmission
4. Increased length of stay
5. Increased cost of complications
6. Delay in resuming activities of daily living
7. Increased nursing time
D Patient satisfaction
1. PONV is among top 10 most undesirable outcomes after surgery.
III ETIOLOGY OF PONV
A Nature of PONV is multifactorial.
B Vomiting center (VC)
1. Located in the lateral reticular formation, medulla (mid brainstem) of the brain
2. Composed of three major nuclei
a Nucleus tractus solitarius
b Dorsal motor nucleus of the vagus nerve
c Nucleus ambiguous involved with coordination of motor activity during vomiting
3. Stimulated by multiple afferent sensory inputs
a Chemoreceptor triggering zone (CTZ)
b Pharyngeal nerve input
(1) Stimulated by mechanical irritation
(2) Gagging can result in retching and vomiting.
c Vagus mucosal pathways from gastrointestinal system
(1) Mechanical receptors in stomach sensitive to distention and contraction
(2) Chemoreceptors in duodenum and stomach sensitive to noxious substances
(3) Vagal afferents also located in eye and oropharynx
(a) Manipulation of the eye can result in VC stimulation.
(b) Oropharyngeal suctioning can result in VC stimulation.
d Midbrain afferent pathways
(1) Stimulated by increased intracranial pressure
e Neuronal pathways from vestibular apparatus
(1) Direct stimulation from cranial nerve VIII
f Reflex afferent pathways from the cerebral cortex
(1) Learned response of anticipatory nausea and vomiting
(2) Cortical afferent stimulation
(a) Emotional: stress, anxiety, fear
(b) Sights and sounds of surgical suite
4. Chemoreceptors located in VC
a Cholinergic
b Histaminic
c Opioid (mu)
d Neurokinin 1 (NK1)
5. Response of VC to multiple inputs is activation of efferent motor pathways of vomiting reflex.
a Gastric efferent response
b Respiratory efferent response
C CTZ
1. Located in area postrema on floor of fourth ventricle of brain
2. Adjacent to VC
3. Very vascular, making it sensitive to decreased blood flow (e.g., hypotension)
4. Outside the blood-brain barrier, making it responsive to emetogenic substances in blood or spinal fluid such as:
a Uremia, hypercalcemia
b Antineoplastic drugs
c Blood sugar fluctuations
d Hormonal influences
e Serum narcotic level
f Inhalation anesthetics
g Levels of dopamine and serotonin
5. Sensitive to intracerebral pressure
6. Contains chemoreceptors
a Serotonin type 3 (5-hydroxytryptamine, 5-HT 3)
b Dopamine type 2 (D 2)
c Histamine type 1 (H 1)
d Muscarinic cholinergic type 1 (M 1)
e Mu opioid
f Stimulation of CTZ chemoreceptors results in stimulation of VC
7. Point of entry of vagal afferent nerve pathways
a Receives vagal stimulation resulting from noxious substances in gut and stomach
b Vagal stimulation triggers serotonin receptors.
c Stimulation of vagal afferents during perianesthesia period creates PONV through CTZ.
(1) Opioids delay gastric emptying, promoting distention and vagal stimulation.
(2) Handling abdominal contents during surgery promotes vagal stimulation.
(3) Pneumoperitoneum secondary to laparoscopic procedures results in vagal stimulation.
(4) Intestinal ischemia creates vagal stimulation.
(5) Vagal stimulation results in serotonin release in GI tract.
8. Point of entry for vestibular afferent pathways
a Changes in motion and pressure increase vestibular activity.
b Vestibular apparatus of inner ear triggers histamine receptors.
(1) Mechanism that creates motion sickness
(2) Mechanism that results in PONV during rapid position changes
c Believed mechanism initiated by nitrous oxide
9. Point of entry for cortical afferent pathways
a Cortical emotional input & stress, anxiety, depression, fear, cognitive overload
b Physiological & hypoxia, pain, hypotension, intracranial pressure
c Sensory input & sight, sound, smell
d Nucleus tractus solitarius (NTS)
10. Physical proximity to CTZ
11. Major site of vagal afferents from vestibular apparatus
12. Contains chemoreceptors
a D 2
b 5-HT 3
c H 1
d M 1
e Vomiting reflex
1. Efferent output of VC
14. Vomiting occurs in three phases.
a Preejection phase
(1) Increase in salivation and swallowing
(2) Decrease in gastric tone
(3) Pallor, diaphoresis
(4) Tachycardia
(5) Regurgitation of small intestine content into stomach
(6) Mediated by vagus nerve and acetylcholine
b Ejection phase
(1) Respiratory inhibition
(2) Closure of glottis to prevent aspiration
(3) Elevation of soft palate
c Postejection phase
(1) Associated with relief of nausea
IV INCIDENCE OF PONV
A PONV occurs in one third of all patients undergoing surgery with anesthesia.
B Up to 80% incidence among patients with predetermined risk factors
C Incidence of PDNV up to 50%
D Patients with PONV are four times more likely to have PDNV.
E More than one third of patients with PDNV will not have PONV.
V RISK FACTORS FOR PONV
A Independent risk factors
1. Independent predictors of PONV
2. Gender
a Females at two to four times higher risk starting at puberty
b No gender difference before puberty
c Unknown relationship of PONV to progesterone, estrogen, and gonadotropin hormonal levels
d Hormonal fluctuation in menstrual cycle may be responsible for PONV differences among women.
e Research has disapproved increased susceptibility during first week of menstrual cycle.
3. Positive history of motion sickness or previous PONV
a Riding in car, plane flight, boat travel
b History of PONV in parent or sibling may be a risk factor.
c Patients with motion sickness appear to have a well-developed vestibular reflex arc.
d Increases risk of PONV two to three times
4. Smoking status
a Nonsmokers at 1.5 to 2.5 times higher risk
b Chemical composition of cigarettes believed to increase hepatic enzyme activity to increase metabolism of anesthesia.
5. Use of postoperative opioids
a Long-acting opioids appear to increase risk.
b Morphine associated with more PONV than fentanyl
B Associated patient risk factors
1. Factors that are not strong enough to predict PONV but are associated with an increased risk
2. Age
a Risk of vomiting in children up to 42%
b Risk increases in children older than 2 years.
c Higher risk in school-age children aged 6 to 16 years, up to 51%
d Female gender adds greater risk after puberty.
e Risk stabilizes in adulthood and is decreased after age 70.
3. Presence of delayed gastric emptying/increased gastric volume
a Pregnancy
b Neurological disease
c Diabetes
d Measurement of delayed emptying is unavailable.
e Degree of PONV risk is not known.
f Obesity (body mass index) has been disproved as a PONV risk factor.
4. American Society of Anesthesiologists (ASA) status
a Healthier patients appear to be at higher risk.
b ASA 1 greater risk than ASA 3
5. Anxiety
a Preoperative anxiety is a weak predictor of PONV.
b Increased circulating levels of catecholamines may stimulate receptors.
c Air swallowing increases gastric volume and decreases gastric motility.
d Anxiety has not been shown to be a risk factor for children.
6. Pain
a Excessive pain increases the risk of PONV.
b Use of nonsteroidal anti-inflammatory agents to reduce need for opioids can lower risk of PONV.
c History of migraine is a possible risk for postoperative nausea.
7. Preoperative fasting
a More liberal criteria for clear liquids appear to reduce incidence of PONV.
b Positive relationship exists between length of liquid fast and incidence of PONV.
c ASA recommendations allowing healthy adults to drink clear liquids as little as 2 hours before surgery are beneficial in PONV.
d A 35% reduction in systolic blood pressure during anesthesia induction is associated with an increased incidence of PONV.
C Associated surgical risk factors
1. Factors not strong enough to predict PONV but associated with an increased risk
2. Surgery duration
a Longer duration of surgery increases the risk.
b Each 30-minute increase in outpatient surgical time increases baseline risk by 60%.
3. Type of surgery
a Controversial risk factor
b Type of surgery may be related to pain experience, opioid use, length of surgery, and surgical manipulation of emetogenic stimuli.
c Ear, nose, and throat: middle ear surgery stimulates vestibular afferents.
d Adenotonsillectomy: introduces blood into stomach as emetogenic irritant, pharyngeal afferent stimulation
e Ophthalmic strabismus: stimulates vestibular afferents
f Gynecological and breast: gender-related risk
g Laparoscopy: increases gastric volume as vagal afferent stimulant
h Abdominal: decreases gastric emptying as vagal afferent stimulant
i Plastic and reconstructive: surgery duration, risk of hypovolemia
j Shoulder: pain afferent stimulation
k Craniotomy: intracranial pressure stimulation
4. Hypovolemia
a Results in prolonged hypotension that can stimulate CTZ
b Results in postural hypotension
D Associated anesthetic risk factors
1. Factors not strong enough to predict PONV but associated with an increased risk
2. Use of volatile anesthetics or nitrous oxide
a Increases risk by 20%
b Risk of early PONV within 2 hours of surgery
c Effect depends on duration of exposure.
d Omitting nitrous oxide is known antiemetic prophylactic measure.
e No relationship to delayed PONV
3. Propofol
a Appears to have a protective effect in reducing PONV when used for maintenance
b No antiemetic effect when used for induction only
c Antiemetic effect lasts only 6 hours after surgery.
4. Gastric distention
a Laryngeal mask airway may create air in stomach.
b Rapid sequence induction with cricoid pressure may reduce air in stomach.
5. Perioperative opioid administration
a Direct action on the CTZ receptors
b Decreases gastric emptying times
c Slows gastric motility
6. Type of approach
a General anesthesia has higher rate of PONV than regional approaches.
b Induction agents associated with higher incidence of PONV
(1) Ketamine
(2) Etomidate
c Inhalation agents have higher rate of PONV than intravenous agents.
d Selection of reversal agents: neostigmine and physostigmine may increase PONV.
E Associated postoperative risk factors
1. Pain
2. Movement
3. Hypotension
4. Blood in stomach
a Oropharyngeal bleeding
(1) Nasal surgery
(2) Adenotonsillectomy
(3) Dental extraction
(4) Pharyngeal procedures
b Gastrointestinal procedures
F Differences in PONV
1. Research suggests that risk factors for nausea are different than risk factors for vomiting.
VI ASSESSMENT OF PONV
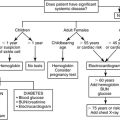
A Preoperative assessment
1. Risk scoring tools group independent risk factors to predict PONV.
2. Simplified tools treat each risk factor equally.
a Apfel et al. risk assessment (1 point for each of four findings)
(1) Risk assessment
(a) Female
(b) History of motion sickness or PONV
(c) Nonsmoker
(d) Anticipated use of postoperative opioids
(2) Scores range from 0 to 4 points.
(3) Risk of PONV by score
(a) 0 & 10%
(b) 1 & 21%
(c) 2 & 39%
(d) 3 & 61%
(e) 4 & 79%
b Koivuranta et al. risk assessment (1 point for each of five findings)
(1) Risk assessment
(a) Female
(b) History of PONV
(c) History of motion sickness
(d) Nonsmoker
(e) Surgery over 60 minutes
(2) Scores range from 0 to 5 points.
(3) Risk of postoperative nausea and postoperative vomiting by score
(a) 0 & 17% and 7%, respectively
(b) 1 & 18% and 7%, respectively
(c) 2 & 42% and 17%, respectively
(d) 3 & 54% and 25%, respectively
(e) 4 & 47% and 38%, respectively
(f) 5 & 87% and 61%, respectively
c Eberhart et al. risk assessment (1 point for each of four findings)
(1) Risk assessment
(a) History of postoperative vomiting in child, parent, or sibling
(b) Duration of surgery over 30 minutes
(c) Age older than 3 years
(d) Strabismus surgery
(2) System developed for risk assessment of vomiting in children
(3) Scores range from 0 to 4 points.
(4) Risk of postoperative vomiting by score
(a) 0 & 9%
(b) 1 & 10%
(c) 2 & 30%
(d) 3 & 55%
(e) 4 & 70%
d Scoring systems have 55% to 80% accuracy in predicting PONV.
e Score offers method to plan prophylactic antiemetic interventions.
3. Carefully assess for motion sickness history.
a Nausea or vomiting when riding in a car, boat, plane, bus
b Avoidance of amusement park rides
4. Carefully assess preoperative hydration status.
a Length and extent of “nothing by mouth” period
b Use of diuretics
c Administration of bowel preparation regimens
B Postoperative assessment
1. Knowledge of patient PONV risk factors and risk score
2. Knowledge of prophylactic antiemetics administered
a Receptor targeted
b Timing of administration
3. Knowledge of patient fluid volume status
4. Assess patient routinely for PONV.
a Only one third of patients communicate nausea to health care providers.
b Direct specific questioning captures a higher percentage of actual PONV incidence.
C PONV assessment
1. Timing (early vs late)
2. Duration
3. Nausea
a Rated on scale of 0 to 10; 10 is worst it can get
b Continuous versus intermittent
c Precipitating events
(1) Occurring with motion
(2) Concurrent pain
(3) Smells, sounds, visual stimuli
(4) After eating/drinking
(5) Hypotension
(6) Medications
4. Vomiting
a Amount of vomitus
b Frequency of episodes
c Color, consistency, presence of blood
d Precipitating events
VII PONV PLAN
A Nursing diagnosis
1. Calculate risk of PONV for each patient.
2. Communicate risk to anesthesia provider.
B Multimodal therapy based on risk assessment.
1. Prophylactic interventions (Table 25-1)
a Hydration
b Risk reduction interventions
c Pharmacological combination therapy
d Complementary therapy
| D2, Dopamine receptor blocker; 5- HT3, serotonin receptor blocker; H1, histamine receptor blocker; M1, muscarinic receptor blocker; NK1, NK receptor blocker; P, prophlaxis; R, rescue. | ||||||
| Agent | Trade Name | Receptors Affected | Use | Route | Dosage | Notes |
|---|---|---|---|---|---|---|
| Aprepitant | Emend | NK1 | P | PO | 40 mg | Best effect when given 1-3 hours prior to induction |
| Dexamethasone | Decadron | Unknown | P, R | IV | 4 mg | Administer before anesthesia induction. Used in combination with other antiemetics; vaginal/anal itching side effects |
| Dimenhydrinate | Dramamine | H1, M1 | P, R | IV, IM | 50-100 mg | Anticholinergic effects include dry mouth, urinary retention |
| Dolastron | Anzemet | 5-HT3 | P, R | IV | 12.5 mg | |
| Droperidol | Inapsine | D2 | P, R | IV | .625-1.25 mg | Best effect when given at end of surgery; little anti-vomiting effect; dose dependent side effects; requires 3 hours of EKG monitoring after dosing |
| Granisetron | Kytril | 5-HT3 | P, R | IV | 5 mcg/kg-1mg | |
| Metoclopramide | Reglan | D2 | R | IV | 10 mg | Increases GI motility; not used for gastric surgery; recommended dosage does not offer effective prophylaxis |
| Ondansetron | Zofran | 5-HT3 | P, R |
IV
Sublingual
|
4 mg | Best effect when given 15-30 minutes prior to end of surgery; headache is common side effect |
| Prochloperazine | Compazine | D2 | R |
IV, IM
PR
|
5-10 mg
25 mg
|
Extrapyramidal symptoms possible; sedative; anticholinergic effects include dry mouth, urinary retention |
| Promethazine | Phenergan | D2, H1, M1 | R |
IV
IM, PR
|
6.25-12.5 mg
12.5-25 mg
|
|
| Scopolamine | Transderm Scop | H1, M1 | P, R | Transdermal | 1.5 mg patch | Apply 4 hours prior to end of surgery; interferes with vestibular impulse transmission; anticholinergic effects; not used for patients with narrow angle glaucoma include dry mouth, urinary retention |
2. Rescue interventions
VIII PROPHYLACTIC INTERVENTIONS
A Hydration
1. Preoperative 20 mL/kg (1-1.5 L) isotonic fluid bolus has been shown to decrease incidence of PONV.
2. Forced postoperative (predischarge) fluid consumption increases PONV by 60%.
B Intraoperative anesthetics
1. Total intravenous anesthesia (TIVA) with propofol and oxygen decreases risk equivalent to one pharmacological receptor blocking agent.
C Risk factor score determines pharmacological prophylaxis.
1. Low risk
a Chance of PONV 10% to 20%
b Interventions needed—none
2. Moderate risk
a Chance of PONV 40%
b Interventions needed—one
3. Severe risk
a Chance of PONV 60%
b Interventions needed—two
4. Very severe risk
a Chance of PONV 80%
b Interventions needed—three or more
5. Medical consequences
a Regardless of risk score, prophylaxis is indicated if medical consequences of vomiting are high (e.g., wired jaw).
D Pharmacological interventions
1. Efficacy based on number needed to treat (NNT)
a Number of patients needed to receive the intervention to prevent one emetic event that would have occurred if the intervention was not used
b Quantitative method to compare efficacy of interventions
c NNT translates into risk reduction for event (e.g., NNT of 5 equals a 20% risk reduction).
2. Depending on risk score, consideration is given to the number of VC receptors to be blocked (i.e., D 2, M 1, H 1, 5-HT 3, NK1).
3. Serotonin receptor antagonists
a Ondansetron (Zofran)
(1) First marketed and most widely studied 5-HT 3 antagonist
(2) Appears to have better antivomiting effect than antinausea effect
(3) Highly selective with a greater affinity for 5-HT 3 receptor than any other receptor
(4) Works by binding to the CTZ and vagal afferent 5-HT 3 receptors
(5) Administer 15 to 30 minutes before end of surgery.
(6) Appears effective in PDNV
(7) No value of additional dose if maximal dose of 4 mg has been administered in 24 hours
(8) Oral form (oral disintegrating tablet [ODT]) can be used in PDNV.
(9) NNT & 5 to 6
b Granisetron (Kytril)
c Dolasetron (Anzemet)
(1) Administer 30 minutes before end of surgery to permit required conversion to hydrodolasetron.
(2) Timing of administration for prophylaxis has little effect on efficacy.
(3) Known to increase QT interval
d Palonosetron
(1) Currently approved for chemotherapy-induced nausea and vomiting only
(2) No apparent antinausea effect
(3) High incidence of headache
e Overall, 5-HT 3 agents most effective when given at the end of surgery
f Little evidence supporting superiority in PONV of any one 5-HT 3 compound
g Fewer side effects than other antiemetics: headache, constipation
h Can be used in pediatrics
i Fewer side effects improve suitability for ambulatory surgery.
j NNT & 5 to 8
4. Antidopaminergics & D 2 antagonists
a Butryophenone
(1) Droperidol (Inapsine)
(a) Appears to have a better antinausea effect than antivomiting effect
(b) Better when administered at the end of surgery
(c) NNT & 3 to 5 if given with patient controlled analgesia PCA opiates over 24 hours
(d) Larger doses needed for vomiting
(e) Side effects of sedation and dizziness, which are dose dependent
(f) Decreases risk of hypotension, which can generate PONV
(g) Extrapyramidal reactions including anxiety, agitation, restlessness
(h) Food and Drug Administration Black Box warning (2001)
(i) ECG monitoring required for 2 to 3 hours after dose
(ii) Possible QT prolongation resulting in arrhythmias
(iii) Restricted to use as second-line therapy
(2) Haloperidol (Haldol)
b Benzamide
(1) Metoclopramide (Reglan)
(a) Blocks D 2 receptors in CTZ and VC
(b) At higher doses blocks 5-HT 3 receptors in CTZ
(c) Weak effect
(d) Only better than placebo in 50% of cases for nausea
(e) Short half-life
(f) Most common administered dose (10 mg IV) when given alone not effective for prophylaxis
(g) Because of increased gastric emptying not recommended for gastric surgery
(h) Unpleasant side effects even at normal dosages: restlessness, agitation, weakness, drowsiness
5. Phenothiazines
a Promethazine (Phenergan)
b Prochlorperazine (Compazine)
c Blocks D 2 receptors in CTZ
d Blocks H 1 receptors in CTZ
e Blocks M 1 receptors in vestibular apparatus
f Need to monitor patients for sedation, hypotension, and extrapyramidal symptoms
6. NK1 receptor agonists
a Aprepitant (Emend)
b Neuropeptide substance P receptors found in NTS and CTZ
c NK1 receptors also located in peripheral nervous system
7. Antihistamines
a Diphenhydramine, dimenhydrinate
b Block H 1 receptors in CTZ
c Act directly on VC
d Block M 1 receptors in vestibular apparatus
e Good for treatment of vertigo and motion sickness
f Side effects: drowsiness, blurred vision, and urinary retention
g NNT = 5 to 8
8. Anticholinergics
a Blocks M 1 receptors
b Scopolamine
(1) Belladonna alkaloid
(2) Also blocks H 1 receptors in VC
(3) Suppresses the noradrenergic system leading to reduced vestibular sensitivity
(4) Transdermal patch application behind ear
(5) Applied 4 hours before anticipated end of surgery
(6) May be applied preoperatively for short surgeries
(7) Contraindicated for patients with narrow-angle glaucoma because of increase in intraocular pressure
(8) Side effects: inhibits salivation (dry mouth), dizziness, increases heart rate, dilates pupils, drowsiness, urinary retention
(9) Slow release system delivers dose over 3 days if left on.
(10) Effective in PDNV
(a) Patients sent home require education for side effects.
(b) Patients sent home require education on proper use and removal of the patch.
(11) Not appropriate for children
(12) Use cautiously in elders, lactating mothers.
(13) NNT = 4
9. Glucocorticoids
a Dexamethasone (Decadron), methylprednisolone (Solu-Medrol)
b Precise method of action unknown
c More effective when administered before anesthesia induction
d Minimal adverse effects
e Low cost
f Additive effect when used with other agents, especially 5-HT 3 blockers
g Effective for early and late PONV
h Appears effective for PDNV
i NNT late postoperative nausea & 4
j NNT late postoperative vomiting & 7
10. Gastroprokinetics
a Increases gastric motility, which decreases stomach distention
b Small quantities of clear fluids can result in gastroprokinesis.
c Metoclopramide (Reglan)
(1) Enhances gastric emptying
(2) Increases upper motility
(3) Weak 5-HT 3 activity only in high doses
(4) Short half-life
(5) Not effective for prevention of PONV alone
(6) May be effective when used in combination with dexamethasone
(7) Side effects include hypotension, increased heart rate, sedation.
11. Mucosal blocking agents
a Vomiting is stimulated by gastric mucosa release of neuroactive agents:
(1) 5-HT 3
(2) Cholecystokinin
b Serotonin (5-HT 3) blockers inhibit 5-HT release.
c Different effect of agents related to individual genetic metabolism
d Greater effect on reducing vomiting than nausea
e Best effect for abdominal and pelvic surgeries
12. Cortical depressants
a Cannabinoids
b Benzodiazepines
c Scant research on effectiveness in PONV/PDNV
13. Multimodal therapy
a No antiemetic is entirely effective.
b Multimodal therapy refers to a combination of interventions that is more effective than a single strategy to increase antiemetic efficacy.
c Combining two or more antiemetics has demonstrated improved prophylaxis.
E Reduce risk by maintaining cardiorespiratory stability.
1. Treat hypotension aggressively.
2. A 35% drop in blood pressure will change intestinal perfusion and increase PONV.
3. Supplemental oxygen
F Universal prophylaxis
1. Likely PONV incidence of 10% to 20% despite any or all therapy
2. Prophylaxis for everyone without regard for risk not cost-effective
3. Universal prophylaxis increases risks of adverse drug effects.
IX RESCUE INTERVENTIONS
A Despite prophylaxis, PONV occurs.
B Before using additional modalities, other causes of PONV should be ruled out.
C Rescuing the patient with PONV requires a different treatment approach than prophylaxis.
D A drug used for prophylaxis should not be used for rescue in the immediate postoperative period.
E Select agent with a different receptor blocking ability.
F Late PONV patients can be treated with any of the prophylactic agents except dexamethasone or scopolamine.
G Nurse must be aware of antiemetic drugs and their mechanisms of action.
H Aggressive fluid therapy if tolerated may be helpful.
I Delayed PDNV
1. Ondansetron dissolving tablets (Zofran ODT)
2. Promethazine suppository or tablet
3. Prochlorperazine oral tablet or suppository
4. Scopolamine patch
X COMPLEMENTARY THERAPIES
A Ginger
1. Possible antiemetic effect, although exact mechanism unknown
a Antiserotonin effects
b 5-HT 3 receptor antagonist
c Antispasmodic to reduce gastric motility
2. Central nervous system and GI systems effects
3. Dose is not clear, but evidence points to 1 gram or more.
4. Active ingredients in ginger preparations have not been standardized.
5. Research meta-analysis indicates better effect than placebo.
6. Should not be recommended for patients taking warfarin
B Aromatherapy
1. Essential oils including ginger, cardamom, and tarragon
2. Peppermint oil
a Traditional cure for vomiting
b Some success with nausea in obstetrics and gynecology
3. Isopropyl alcohol inhalation
a Risk free
b Low cost
c Efficacy has not been established through research.
C P6 stimulation
1. Includes acupressure, acupuncture, transcutaneous electrical stimulation
2. Better than placebo with NNT & 4 to 5
3. May reduce nausea
4. No effect shown in children
5. Little impact on vomiting
D Supplemental oxygen
1. Appears to affect GI tract, which has high metabolic demands and intolerance to ischemia
2. Evidence is conflicting.
3. Majority of research indicates that oxygen is of limited or no benefit.
4. Reduces PONV by 50% in colorectal surgery
5. Inexpensive and risk free
6. Administered dose for 2 hours postoperatively
E Untested modalities
1. Cool washcloths to forehead
2. Deep breathing
3. Repositioning
XI PEDIATRIC PONV THERAPY CONSIDERATIONS
A Use of propofol increases risk of bradycardia during strabismus surgery.
B Droperidol causes more extrapyramidal reactions in children.
C Should not force oral fluids before discharge
D Nonpharmacological techniques have not shown effectiveness in children.
XII NURSING INTERVENTIONS
A Knowledge of patient risk score
B Awareness of antiemetic prophylaxis plan of care
C Prepare environment to reduce emetic stimulation.
1. Sights, smells, conversation
D Ensure adequate preoperative and postoperative hydration.
E Provide adequate analgesia.
1. Appropriate opioids
2. Appropriate nonsteroidal anti-inflammatory drugs
F Move and ambulate patients slowly postoperatively.
G Patient education
1. Knowledge of risk factors
2. Awareness of future risk
3. Management of PDNV
a How to manage fluids and food
b How to manage medications with known gastric irritation
c When to contact health care provider
XIII DOCUMENTATION
A Document each symptom: nausea, vomiting, retching.
B Nausea
1. Timing
a Intermittent
b Continuous
c Preceding vomiting
2. Preceding events
a Transport (motion induced)
b Medication (opioid induced)
c Food/fluids (gastric motility)
3. Rank on severity scale
a Verbal descriptive scale
b Visual analog scale
C Vomiting
1. Frequency
2. Volume
3. Characteristics of emesis
a Content
(1) Undigested food
(2) Hematemesis
(3) Coffee ground
(4) Bilious
(5) Feculent
b Color
D Retching
1. Frequency
2. Precipitating events
E Efficacy of interventions for PONV
1. Response to rescue pharmacology
2. Response to complementary interventions
BIBLIOGRAPHY
1. American Society of PeriAnesthesia Nurses, ASPAN’s evidence-based clinical practice guideline for the prevention and/or management of PONV/PDNV, J Perianesth Nurs 21 (4) ( 2006) 230–250.
2. Couture, D.J.; Maye, J.P.; O’Brien, D.; et al., Therapeutic modalities for the prophylactic management of postoperative nausea and vomiting, J Perianesth Nurs 21 (6) ( 2006) 398–403.
3. Gan, T.J., Risk factors of postoperative nausea and vomiting, Anesth Analg 102 (6) ( 2006) 1884–1898.
4. Golembiewski, J.A.; O’Brien, D., A systematic approach to the management of postoperative nausea and vomiting, J Perianesth Nurs 17 (6) ( 2002) 364–376.
5. Golembiewski, J.A.; Tokumaru, S., Pharmacological prophylaxis and management of adult postoperative/discharge nausea and vomiting, J Perianesth Nurs 21 (6) ( 2006) 385–397.
6. Habib, A.S.; Gan, T.J., Evidence-based management of postoperative nausea and vomiting: A review, Can J Anaesth 51 (4) ( 2004) 326–341.
7. Murphy, M.J.; Hooper, V.D.; Sulivan, E.; et al., Identification of risk factors for postoperative nausea and vomiting in the perianesthesia adult patient, J Perianesth Nurs 21 (6) ( 2006) 377–384.
8. Odom-Forren, J.; Fetzer, S.J.; Moser, D.K., Evidence-based interventions for post discharge nausea and vomiting: A review of the literature, J Perianesth Nurs 21 (6) ( 2006) 411–430.