CHAPTER 18. Complementary Therapies
Susan A. Goodwin and Jane C. Dierenfield
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Define the terms complementary therapies (CTs) and integrative medicine.
2. Discuss the influence of Eastern medicine, including Traditional Chinese Medicine and East Indian contributions.
3. Compare and contrast 27 commonly used herbs, vitamins, and dietary supplements.
4. Summarize six CTs that could be used in the perianesthetic period.
5. Briefly define additional CTs.
I. OVERVIEW OF COMPLEMENTARY THERAPIES (CTs)
A. Definitions
1. Conventional medicine—practiced by medical doctors or doctors of osteopathy, and other allied health professionals (e.g., registered nurses, psychologists, or physical therapists)
a. Taught at United States (U.S.) medical schools, and generally provided at U.S. hospitals
b. Commonly known as Western medicine and is based on biology and pathology
2. CTs: group of diverse medical and health care systems, practices, and products that are not presently considered to be a part of conventional medicine
a. Used in conjunction with conventional medicine, or used by themselves without conventional medicine
b. Based on Eastern philosophy, which is based on balance and harmony
c. Oriental medicine began approximately 5000 years ago. The Yellow Emperor’s Classic of Internal Medicine was written 2000 years ago.
3. Integrative medicine—the eventual combination of CT and medicine
4. Reliable evidence of complementary medicine efficacy is needed before its integration into clinical practice.
B. Clinical trial articles of complementary medicine increased from 1987 through the present.
II. CURRENT UTILIZATION OF CTS
A. Terms
1. “Complementary and alternative medicines” (CAMs) commonly used.
a. In the medical literature
b. By the National Center for Complementary and Alternative Medicine (NCCAM)
2. The term CAMs will be used when referring to medical practice.
3. In this chapter, CTs will be used to describe these interventions, as this term more appropriately describes nursing practice.
B. Current use
1. Searches conducted in 2008 on Ovid, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PubMed, and Google Scholar revealed a plethora of articles on CAM. Diverse patient and ethnic populations represented, and treatment of a variety of diseases and conditions was detailed.
2. When health insurance plans offered CT coverage, it varied by state and was often limited. Most CTs were paid out-of-pocket.
3. Health insurance covers the following:
a. Chiropractic
b. Acupuncture
c. Massage
d. Biofeedback
e. Naturopathy
C. NCCAM
1. In 1992, the National Institutes of Health established the Office of Alternative Medicine (OAM).
a. Mission: to provide the Americans with reliable information about the CAM safety and effectiveness
b. Budget for 1992 was $2 million.
2. Congress expanded the OAM into the NCCAM in 1998.
3. The annual budget was increased to $121.6 million in 2008.
4. CAM is defined by the NCCAM as a group of diverse medical and health care systems, practices, and products that are not presently considered to be part of conventional medicine.
5. A review of clinical trials listed on the NCCAM website lists 235 completed clinical trials, (90 that are beginning the recruiting process, and over 100 that are in progress as of March 2009).
D. Partial listing of CTs
1. Acupuncture/acupressure
2. Aromatherapy
3. Ayurveda
4. Chiropractic
5. Dietary supplements
6. Energy healing
7. Guided imagery
8. Herbal therapies
9. High-dose vitamin or megavitamin therapies
10. Homeopathy
11. Magnetic therapy
12. Massage
13. Meditation
14. Music
15. Naturopathy
16. Osteopathic
17. Prayer
18. Qigong
19. Reiki
20. Relaxation techniques
21. Therapeutic touch
22. Yoga
E. Recent trends in CTs in the U.S.
1. National surveys indicate that CTs are widely used and increasing in popularity.
2. Use of CTs tends to be higher among patients who are:
a. Female
b. Middle aged or younger, 35 to 49 years of age
c. White
d. Married
e. Employed
f. More affluent
g. Better educated, with some college education
h. Have more insurance
i. Live in the western part of the U.S.
3. People who use CTs also use medical doctors.
a. The more visits made to a medical doctor, the more likely he or she was to use CAM.
4. CTs are used less frequently by:
a. African Americans
b. Persons 65 years or older
5. CTs are used most frequently for:
a. Chronic pain
b. Anxiety and/or depression
c. Urinary tract problems
d. Back problems
e. Headaches
f. Allergies
g. Arthritis
h. Digestive problems
i. Cancer
j. Diabetes
k. Acquired immunodeficiency syndrome
l. Preventing future illness from occurring
m. Maintaining health and vitality
6. Unsupervised use, which is a form of expanded self-care, is the usual method of use for most CTs. There is usually no involvement of either a medical doctor or a complementary medicine practitioner.
7. The increasing use of CTs has occurred despite the fact that the majority of costs have been paid out-of-pocket.
F. Use of CTs throughout the world
1. In Denmark in 1987, 10% of the population used CTs.
2. In Australia in 1993, 49% of the population used CTs.
3. The United Kingdom spent $94 million on herbal remedies and $30 million on homeopathic remedies.
4. Germany spent $541 million on herbal remedies and $528 million on homeopathic remedies.
5. In Germany, herbal medicine is well integrated into the medical culture.
a. Tens of millions of prescriptions written by physicians for herbal medicines each year
G. Reasons for use of CTs
1. Dissatisfaction with conventional treatment
2. Desire to try all options, especially among cancer patients
3. Anecdotal information from friends or acquaintances
4. Belief that CTs are less harmful than conventional therapies
5. Many CTs are holistic and encompass a spiritual component, which is lacking in conventional medicine.
H. Implications for further study
1. The use of traditional randomized, double-blind, placebo-controlled clinical trials with CTs presents certain challenges.
2. It would be extremely difficult to design and implement randomized, double-blind, placebo-controlled clinical trials of all the CTs that are in use today.
3. Many of the CTs have been in use for thousands of years, with vast anecdotal success.
4. Treatment plans with CTs are often individualized and are thus hard to replicate.
5. CTs are increasingly being integrated with conventional medicine, rather than being used alone or in the place of conventional medicine.
6. Pharmaceutical companies invest between $350 and $500 million in a 10-year period to bring a new drug to market; when the drug is marketed, the money is recouped.
7. Obtaining financial support for research on herbs is difficult because there is no financial incentive for investment by pharmaceutical companies.
a. The herb is readily available, cannot be patented, and is thus not financially lucrative.
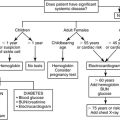
III. PREOPERATIVE ASSESSMENT OF PERIANESTHETIC PATIENTS
A. Lack of report of CTs
1. A study of older adults residing in Minnesota revealed that 62.9% used CAMs, while only 53% disclosed their CAM use to their primary care providers.
2. The flourishing use of herbal preparations increases the need to question preoperative patients about their use of herbals.
3. Many people do not view herbals as “medicine” or may be reluctant to disclose their uses of CT to conventional practitioners, such as nurses or doctors.
4. The preoperative nurse must make specific and repeated inquires to the patient about the potential use of herbals.
B. Herbals
1. Are plant-derived products used for medicinal and health purposes (Table 18-1).
| BPH, Benign prostatic hypertrophy; FDA, Food and Drug Administration; GABA, gamma-aminobutyric acid; GERD, gastroesophageal reflux disease; GI, gastrointestinal; INR, international normalized ratio; MAOIs, monoamine oxidase inhibitors; MI, myocardial infarction; NSAIDs, nonsteroidal anti-inflammatory drugs; PMS, premenstrual syndrome; PONV, postoperative nausea and vomiting; SSRIs, selective serotonin reuptake inhibitors (such as nefazodone, sertraline, or paroxetine); TMJ, temporomandibular joint. | |||||
| Herb | Actions | Uses | Side Effects | Perianesthetic Implications | Preoperative Precautions |
|---|---|---|---|---|---|
| Aloe vera | Anti-inflammatory. Relieves pain, decreases inflammation and swelling, and may encourage wound contraction. May increase blood flow. Useful for first- and second-degree burns. May be useful in the treatment of psoriasis. | Topical: Emollient. Encourages healing of a wound, burn, hemorrhoids, insect bites, poison ivy or oak, rashes, sunburn, and yeast infections. Oral: Treats or prevents constipation. | Rare topical allergic reactions. Oral gel can reduce absorption of many drugs. | Oral use may cause hypokalemia due to cathartic effects. | Not necessary |
| Arnica | An immunostimulant. May increase macrophage activity and blood circulation to injured area. Has anti-inflammatory and mild analgesia properties. Is frequently combined with goldenseal. | Topical and Oral: Relieves muscle, joint, and cartilage pain from bruises, contusions, hyperextensions, bursitis, and arthritis. | Long-term topical use can lead to toxic skin reactions. Internal use has a very narrow dosing range. The FDA classifies arnica as unsafe for internal use. The German Commission E does not recommend internal use because of potentially toxic effects. | May be the source of preoperative skin irritations. May have minimal anticoagulant effects. | 2 weeks |
| Black cohosh | Estrogenic activity. Causes hypotensive effects via decreased vascular spasm. Has sedative, anti-inflammatory, and antispasmodic effects. | Approved by the German Commission E for the treatment of PMS, dysmenorrhea, and menopausal symptoms, including mood changes. May inhibit bone loss caused by menopause. Appears to increase the normal growth of vaginal cells, thereby reducing vaginal dryness and dyspareunia. Alleviates insomnia. Used as an anti-inflammatory for arthritis. (Remifemin, a European form of black cohosh, is available in the United States.) | GI discomfort, frontal headache, nausea, heaviness in the legs, weight problems, dilated pupils, and flushed face. Avoid use during pregnancy or lactation. | May cause hypotension and bradycardia. May potentiate antihypertensive medications. | 2 weeks |
| Chamomile | Mild sedative. Has antispasmodic, antibacterial, antipyretic, and anti-inflammatory activity. | Used as an antiemetic, for indigestion, to decrease cramping secondary to diarrhea, and as an aid for sleep. Used for dysmenorrhea and to treat arthritis. | Allergic reactions are common, especially in patients who are allergic to ragweed, and include contact dermatitis and pharyngeal edema. | May potentiate sedation. Anticoagulant effects due to platelet inhibition. | 2 weeks |
| Cranberry | Prevents Escherichia coli from adhering to bladder wall and the urinary tract. Acidifies the urine. | To acidify the urine and treat urinary tract infections. Decreases the incidence of urinary stones. | None with normal doses. Very large doses may result in diarrhea. | None known | Not necessary |
| Echinacea | Anti-inflammatory, immunostimulating, bacteriostatic, bactericidal, and free-radical scavenging effects. Causes activation of cell-mediated immunity. Enhances phagocytosis. Decreases the activity of viruses. | Used for the prophylaxis and treatment of bacterial and fungal infections. Begin use at the first sign of a cold to decrease cold symptoms and duration. If used for longer than 8 weeks, the effectiveness declines. Also used to treat chronic wounds, ulcers, and arthritis. Used in Germany along with chemotherapy to treat cancer. | Use longer than 8 weeks could cause immunosuppression and hepatotoxicity (some controversy exists about this). Should not be used with other hepatotoxic drugs, such as anabolic steroids, amiodarone, methotrexate, or ketoconazole. Do not give concomitantly with immunosuppressants. Can cause transplant rejection. Use with caution in patients with asthma or allergic rhinitis. May cause allergic responses in individuals allergic to ragweed. | Causes inhibition of hepatic enzymes. May affect many anesthetic agents. | 2 weeks |
| Evening primrose oil | Chemical constituents are prostaglandin precursors, which have anti-inflammatory properties. | Used for PMS symptom relief, diabetic neuropathy, numerous skin conditions, and chronic autoimmune diseases such as rheumatoid arthritis, Raynaud’s syndrome, and multiple sclerosis. | Lowers seizure threshold and increases anticonvulsant requirements. Nausea, softening of stools, and headache. | May interact with drugs that are anticonvulsants. Inhibits platelet aggregation. | 2 weeks |
| Feverfew | A prostaglandin inhibitor. Has been shown to suppress 86%-88% of prostaglandin production. | Used to treat migraines, other types of headaches. Can reduce the number as well as severity of migraines. Also used to treat fever, dizziness, stomachache, and rheumatoid arthritis. | NSAIDs may negate the effects of feverfew in the treatment of migraines. May cause mouth ulcers. | Anticoagulant effects due to platelet inhibition. | 2 weeks. Discontinuation after prolonged use can cause a rebound effect, resulting in symptoms of migraine, insomnia, and anxiety. A slow withdrawal may reduce these effects. |
| Garlic | Can lower the risk of developing atherosclerosis through its antihypertensive and anticholesterolemic effects, as well as platelet inhibition. Has antibacterial and antiviral properties. Appears to prevent some cancers. | Used to treat hypertension, hypercholesterolemia, atherosclerosis, and infection. | Inhibits platelet function and fibrinogen. Concomitant use with aspirin, NSAIDs, or anticoagulants is not recommended. May cause nausea, hypotension, and allergy. Bad breath is a common side effect. | Anticoagulant effects due to platelet inhibition. Can cause hypotension. | 2 weeks |
| Ginger | Has antiemetic, antispasmodic, and anti-inflammatory properties. A potent inhibitor of thromboxane synthetase. | Used to treat PONV, motion sickness, hyperemesis gravidarum, intestinal gas, indigestion, and arthralgias. | Inhibits platelet function. May cause GI upset when taken on an empty stomach. | Anticoagulant effects due to platelet inhibition. May cause hypotension or bradycardia. | 2 weeks. However, there have been studies in which ginger was given just before surgery to reduce PONV, and no increased bleeding was seen. |
| Ginkgo biloba (also sold under Bai Guo Ye, Baiguo, & Fossil Tree) | Its components act as antioxidants, alter vasoregulation, alter neurotransmitter and receptor activity, and inhibit platelet-activating factor. | Stabilizes and perhaps improves cognitive function in patients with dementia. Used for peripheral vascular disease, vertigo, tinnitus, and erectile dysfunction. Promotes vasodilation, improves mental function and sexual functioning. Slows macular degeneration and protects the retina, especially in diabetic retinopathy. | Mild GI upset and headache. Inhibits platelet function and fibrinogen. Concomitant use with aspirin, NSAIDs, or anticoagulants is not recommended. May diminish effectiveness of anticonvulsants. | Anticoagulant effects due to platelet inhibition. | 2 weeks |
| Ginseng | A number of ginseng products exist, whose effects vary widely. It is important to be familiar with which ginseng is used. In general, acts as an adaptogen, protecting the body against stress and restoring homeostasis. The underlying mechanism appears to be similar to steroids. Acts as an immunostimulant. Has a hypoglycemic effect. | Used to reduce stress and improve vitality. Can also be used for mild depression, chronic fatigue syndrome, fibromyalgia, and stress-induced asthma. Improves cognitive function, attention span, psychomotor performance, and concentration. | May cause headache, tremulousness, and insomnia. Avoid in patients with bipolar syndrome and psychosis. Avoid concurrent use with estrogens and corticosteroids due to additive effects. May lower blood glucose levels; should not be used in patients with diabetes. Concomitant use with aspirin, NSAIDs, or anticoagulants is not recommended due to inhibition of platelet function. | Anticoagulant effects due to platelet inhibition. Can cause hypertension or tachycardia. May potentiate sedation and hypoglycemia. | 2 weeks |
| Goldenseal | Has antibacterial properties. May reduce gastric inflammation. Frequently combined with arnica. | Used for its antibacterial and antifungal properties to treat conjunctivitis, gastric and duodenal ulcers, thrush, and strep throat. | Excessive doses can cause jaundice and elevated liver enzymes. Contraindicated with diarrhea, GI cramping, and nausea and vomiting. | Use cautiously with heparin. May augment or diminish effects of antihypertensives. | 2 weeks |
| Kava-kava | Acts as a sedative-hypnotic possibly by potentiating GABA inhibitory neurotransmission. Has mild analgesic and muscle-relaxing effects. Has abuse potential. | Alleviates stress, anxiety, tension, and nervousness. Used as an anxiolytic and sedative. Relieves tension headaches and muscle spasms (restless leg syndrome, TMJ pain). | Avoid concomitant use with barbiturates, alcohol, and benzodiazepines as excessive sedation can occur. Do not use with antiparkinsonian drugs. Decreases platelet function. Heavy use produces kava dermopathy, characterized by reversible, scaly, cutaneous eruptions accompanied by jaundice. The sale of kava has recently been banned in Canada and the United Kingdom because of reported liver damage. | Excessive sedation can occur with anesthetic drugs. Anticoagulant effects due to platelet inhibition. | 24 hours |
| Ma huang (ephedra) | Known as ephedra. Ephedrine, a sympathomimetic amine, is the predominant active compound. It increases heart rate and blood pressure, bronchodilates, has anti-inflammatory properties, and inhibits prostaglandins. | Commonly used as a decongestant for allergies and hay fever. Used to promote weight loss, increase energy, and treat bronchospastic disorders such as asthma or bronchitis. Also used as an aphrodisiac. | Cause dose-dependent increases in blood pressure and heart rate. Can cause palpitations, coronary spasm, MI, and stroke. Concomitant use of ephedra and MAOIs can result in hyperpyrexia and hypertension. The American Medical Association has called for a ban of ephedra in supplements. | May cause hypertension or arrhythmias. When given halothane, may cause ventricular dysrhythmias. | 7 days |
| Peppermint | Relaxes the lower esophageal sphincter. Antispasmodic, smooth muscle relaxant. | Used for nausea, rhinitis, heartburn, and flatulence. | Avoid in patients with hiatal hernia and GERD, as the relaxation of the lower esophageal sphincter may worsen symptoms. | None known | Not necessary |
| Saw palmetto (also called American dwarf palm tree, cabbage palm or ju-zhong) | Increases urinary flow, decreases nocturia, and decreases postvoid residual volumes. Acts as a urinary antiseptic. | Relief of BPH symptoms, such as frequent urination, difficulty in initiating urination, and high residual volume. Useful in chronic pelvic pain, bladder disorders, decreased sex drive, hair loss, and hormone imbalance. | Side effects uncommon, but may include mild GI distress, bleeding, and headache. Because of its antiplatelet effect, the use of aspirin on NSAIDs may increase bleeding risk. | May increase INR in patients receiving warfarin. | 2 weeks |
| St. John’s Wort | Acts similarly to MAOIs or SSRIs by inhibiting serotonin, norepinephrine, and dopamine reuptake by neurons. | Licensed in Germany for the treatment of anxiety, depression, nerve pain, and sleep disorders. Use for moderate depression may be more effective than a placebo. A 2005 study found that St. John’s Wort was more effective than fluoxetine (Prozac). | Avoid concomitant use with MAOIs and SSRIs, which could result in a serotonin syndrome. May inhibit the absorption of iron. Causes photosensitivity. Through enzyme induction, increases the metabolism of many drugs, including cyclosporine, alfentanil, midazolam, lidocaine, calcium channel blockers, warfarin, and SSRIs. Avoid in pregnancy. | May potentiate anesthetic effects. May affect blood pressure. | 7 days. Discontinuation is especially important in patients awaiting organ transplantation or who may require anticoagulation therapy postoperatively. |
| Valerian | Causes a significant decrease in sleep latency. Causes dose-dependent sedation and hypnosis. | Used for insomnia, anxiety, headache, irregular heartbeat, depression, or trembling. | Avoid concomitant use with barbiturates, alcohol, and benzodiazepines as excessive sedation can occur. Can cause “morning hangovers.” May cause paradoxical stimulation, GI upset, nervousness, disturbed sleep, and rare liver toxicity. | May potentiate sedation caused by anesthesia. | 7 days. Abrupt discontinuation in patients who are physically dependent may cause benzodiazepine-like withdrawal. Taper over several weeks. |
2. Thirty percent of all modern drugs derived from plants
3. The use of herbals has increased significantly in the past 10 years.
4. Herbals may have many allergic reactions as well as interactions with prescription drugs.
5. Perioperative patients are exposed to a great number of pharmacological agents during their surgical experience.
a. Potential for adverse drug interactions is much higher than during their everyday life.
b. Potential interactions with anesthetic drugs
(1) Coagulation disturbances
(2) Prolongation of anesthetic sedation
(3) Adverse cardiovascular effects
(4) The American Society of Anesthesiologists recommends that patients discontinue herbal medicines at least 2 weeks before surgery.
C. Regulation of herbals in the U.S.
1. In 1994, herbal medications were classified as dietary supplements in the Dietary Supplement Health and Education Act.
2. This law exempts herbals from the safety and efficacy requirements that must be met by prescription and over-the-counter drugs. It requires:
a. No proof of efficacy
b. No proof of safety
c. Sets no standards for quality control
d. That supplements not promise a specific cure on the label
3. There is no guarantee that the herb(s) listed on the packaging are actually present, that the ingredient is bioavailable, the dosing is appropriate, or whether the next bottle will have the same composition.
a. The same herb marketed by different manufacturers can vary greatly.
b. Herbs manufactured from outside the U.S. may contain heavy metals, pesticides, and even pharmaceuticals.
4. The Food and Drug Administration must show that an herbal product is unsafe before it can be removed from the market.
5. There is no mechanism for reporting of herbal adverse effects, or herbal and drug interactions; thus, they are grossly underreported.
D. Regulation of herbals in Europe
1. In Germany, France, the United Kingdom, and Canada, regulating agencies enforce standards of herb quality and safety assessment of manufacturers.
2. The German Commission E Monographs are a comprehensive study of herbals.
3. Significant numbers of studies are being conducted in Germany, France, Japan, China, and India.
E. Vitamins and dietary supplements
1. Vitamins are complex organic substances found in most foods that are essential for the normal function of the body.
2. Dietary supplements correct a dietary deficiency.
3. A number of commonly used vitamins and dietary supplements interact with perianesthetic drugs in similar ways to herbals (Table 18-2).
| ADP, Adenosine diphosphate; GI, gastrointestinal; NSAIDs, nonsteroidal anti-inflammatory drugs. | |||||
| Dietary Supplements | Actions | Uses | Side Effects | Perianesthetic Implications | Preoperative Discontinuation |
|---|---|---|---|---|---|
| Chondroitin | Usually given in conjunction with glucosamine. Contains glycosaminoglycans, which increase proteoglycan concentration, a substance that forms cartilage in joints. Reduces collagen breakdown. Has anti-inflammatory effects. | May improve joint pain and function in osteoarthritis. | Mild GI symptoms. Concomitant use with warfarin should be avoided. | None | Not necessary |
| Coenzyme Q 10 | A fat-soluble chemical present in all tissue used to make ADP. Acts as an antioxidant, removing free radicals. Improves immune function. | Used to treat cancer, heart failure, cardiomyopathy, hypertension, angina, and dysrhythmias. | Mild GI distress. Works synergistically with antihypertensives. Concomitant use with warfarin should be avoided. May diminish the effects of aspirin, NSAIDs, and other anticoagulants. | May augment hypotensive effects of anesthesia. May have anticoagulant effects. | 2 weeks |
| Fish oil | Has anti-inflammatory and antiembolus effects. Promotes vasodilation. Reduces cholesterol production. | Used to treat coronary artery disease, hyperlipidemia, hypertension, and diabetes. | Belching, bad breath, heartburn, and nosebleeds. May increase bleeding time. Works synergistically with antihypertensives. | Anticoagulant effects due to inhibition of platelet aggregation. May augment the hypotensive effects of anesthesia. | 2 weeks |
| Glucosamine | Usually given with chondroitin. An aminomonosaccharide, which stimulates the production of glycosaminoglycans, a component of cartilage. Has anti-inflammatory effects. | May improve joint pain and function in osteoarthritis. Slow acting; may have to take it for up to 2 months before benefits are seen. | Mild GI distress. Avoid if allergic to shellfish or iodine. May raise blood sugar levels. | None | Not necessary |
| Melatonin | A hormone produced by the pineal gland during sleep. Produced from tryptophan. | Used to treat insomnia and sleeplessness caused by jet lag or working the night shift. | Headaches, vivid dreams or nightmares, and morning hangovers. Contraindicated in severe mental illness or autoimmune disease. | May potentiate sedation. | 24 hours |
| Vitamin C | An essential nutrient needed for collagen and tissue formation, hormone production, carbohydrate metabolism, and immune system function. | A wide variety of uses, including treatment and prophylaxis of colds, fractures, immune system stimulation, wound healing, and periodontal disease. | Rare side effects. May cause GI distress. | May decrease the effects of heparin or warfarin. | Not necessary |
| Vitamin E | An essential fat-soluble vitamin. Acts as an antioxidant, binding to free radicals. A component of the immune system, maintains healthy eyes and skin, and promotes normal clotting. | A wide variety of uses, including diabetes, Alzheimer’s disease, fibrocystic breast disease, immune system integrity, skin disorders, and menopause. | Rare side effects. As a fat-soluble vitamin, is stored in the liver. | Anticoagulant effects due to inhibition of platelet aggregation. May augment the hypotensive effects of anesthesia. | 2 weeks |
| Zinc | Acts as an immunostimulant. | Used to decrease the symptoms and longevity of the common cold. | Do not give with immuosuppressants. May cause nausea and a bad taste. | None known | Not necessary |
IV. CTs USEFUL IN PERIANESTHESIA
A. Nursing and CT
1. Nurses are in a unique position to combine conventional Western medicine and CTs.
2. Integrative and holistic nature of nursing lends to the esoteric nature of many complementary interventions.
3. Forty-seven percent of state boards of nursing permit the practice of some CAMs (Arizona, Arkansas, California, Connecticut, Illinois, Iowa, Kansas, Louisiana, Maine, Maryland, Massachusetts, Mississippi, Missouri, New Hampshire, New York, Nevada, North Carolina, North Dakota, Ohio, Oregon, Pennsylvania, Texas, Vermont, and West Virginia).
4. The practice of CAMs is under discussion in seven states: Delaware, District of Columbia, Georgia, Minnesota, New Jersey, New Mexico, and Washington.
5. The remaining 40% of states have no formal position on CAMs (Alabama, Alaska, Colorado, Florida, Georgia, Hawaii, Idaho, Indiana, Kentucky, Michigan, Montana, Oklahoma, Puerto Rico, Rhode Island, South Carolina, Tennessee, Utah, Virgin Islands, Virginia, Wisconsin, and Wyoming).
B. Six CTs practiced by nurses in the perianesthetic setting
1. Aromatherapy
a. Use of essential oils (EOs) for therapeutic or medical purposes
b. Used throughout history in many cultures, including ancient Egypt in 3000 b.c.
c. EOs are steam distillates from aromatic plants and can be used with massage, friction, inhalation, compresses, and baths.
d. EOs can have sedative, stimulatory, analgesic, antispasmodic, and antibacterial properties.
e. The effects of the EO depend on the therapeutic actions of the oil as well as the learned smell memory of the patient.
f. Inhaled peppermint and ginger can be used to treat postoperative nausea and vomiting.
g. Inhaled lavender, Roman chamomile, lemongrass, and rose can be used to treat pain.
h. Topical lemon, clove, cinnamon bark, eucalyptus, rosemary, and melaleuca (also known as tea tree oil) have antiviral, antiseptic, antibacterial, and anti-infectious properties.
2. Massage
a. An ancient technique; a Chinese medical work written in 2760 b.c. contains descriptions of massage techniques.
b. Modern massage developed by Henrik Ling from Sweden (1776-1839)
c. A series of soothing and energizing stroking techniques that stimulate the muscles, increasing their ability to absorb nutrients and eliminate waste products
d. Nonpharmacological and holistic intervention
e. Relieves muscle tension, stimulates the nervous system, enhances skin condition, improves circulation, aids digestion and intestinal function, increases mobility in joints, relieves chronic pain and especially low back pain, and reduces swelling and inflammation
f. Used to ease childbirth; with asthmatic children to improve breathing; with terminally ill, homebound, and nursing home residents; and with preoperative and postoperative patients
g. Do not use massage with fever, infections, open wounds, contagious skin conditions or diseases, phlebitis, or acute strains or sprains; wait 48 hours after a strain or sprain to massage.
3. Music
a. Uses melody to effect changes in behavior, emotions, and physiology
b. Lowers anxiety, provides distraction, promotes relaxation, and increases pain tolerance; helps the body release energy used for healing
c. Used in the perioperative period, and many patients feel less anxious when listening to music before and after surgery.
d. A trained sound therapist uses a wide range of tools (i.e., musical instruments, tapes, tuning forks, and machines that release sound waves at specific frequencies to help heal the body).
4. Relaxation therapy
a. Encompasses a variety of stress-reduction techniques
b. Can be done with yoga, meditation, guided imagery, hypnosis, positive suggestions, and breathing techniques
c. Elicits a relaxation response, which results in reduced muscle tension, decreased blood pressure, heart rate, and respiration, and reduced oxygen consumption
d. Surgical patients who use relaxation exercises recover more quickly, use less pain medication, have lower blood pressure, and have fewer postoperative complications than those who do not use them.
5. Therapeutic touch
a. First developed in the early 1970s by Dolores Kreiger, PhD, RN, and psychic Dona Kunz
b. Similar to qigong
c. Based on an ancient technique called laying-on of hands
d. The healing force of the therapist positively affects the patient’s recovery.
e. Practitioner scans the patient’s energy field by moving his or her hands in a sweeping motion above the body, clears the energy field to blockages of energy, and facilitates the flow of energy from his or her hands to the patient’s energy field.
f. Used to promote relaxation and reduce stress, pain, anxiety, and restlessness—can also promote a sense of well-being
g. Used in acute situations to treat sprains or muscle spasms, to sooth and relax, and to decrease heart rate and blood pressure
h. Enhances the onset of pain medications as well as the effectiveness
6. Guided imagery
a. A form of self-hypnosis that uses directed thoughts and suggestions; based on the concept that your body and mind are connected
b. Used to relieve physical, mental, and emotional stress, as well as many of the medical conditions associated with stress
c. Used to stimulate the immune system and promote healing
V. BRIEF DEFINITIONS OF SELECTED CTS
A. Acupuncture/acupressure
1. Based on traditional Chinese medical theory, and has been in existence for at least 2500 years
2. Involves inserting thin-gauged needles into specific anatomical points in the body for therapeutic purposes
3. Disrupted patterns of energy flow (qi) that travel in meridians are rebalanced by acupuncture
4. Insertion points tend to correspond to areas where connective tissue is the thickest.
5. Acupressure uses the fingers, hands, elbows, or other devices to press on the surface of the skin on the same anatomical points used in acupuncture; no needles are involved.
6. Acupressure and acustimulation devices may be used to treat postoperative nausea and vomiting.
B. Ayurvedic
1. Ayurvedic medicine is traditional Hindu medicine, and was developed more than 5000 years ago.
2. Ayurveda means the “science of life.”
3. The physician prevents or treats diseases by restoring the balance of body, mind, and spirit with diet, exercise, meditation, herbs, massage, and controlled breathing.
C. Balneotherapy involves the use of baths in the treatment of health conditions.
D. Chiropractic
1. Focuses on the relationship between bodily structure and function
2. Focuses on how that relationship affects the preservation and restoration of health
3. Uses spinal manipulation and adjustments to bring about healing
E. Homeopathy
1. A Western system of care based on the belief that very dilute substances are able to stimulate a healing response in the body
2. Developed by Samuel Hahnemann, a German physician who practiced medicine in the late 1700s
3. Stimulates the body’s defense mechanisms to cure symptoms by administering minute doses of medicinal substances; these same substances at higher doses would actually cause symptoms or disease.
F. Magnetic therapy
1. Electromagnetic fields are invisible lines of force that are present in the earth and are believed to be produced by electric currents flowing at the earth’s core.
2. Often used to relieve pain
G. Meditation
1. A cultivation of the mind through quieting, and observing one’s inner state
2. Learning to slow down and examine passing sensations in minute detail
3. The practitioner allows pain, emotions, and bodily sensations to be experienced as a natural progression of life.
4. Results in:
a. Reduction of stress activity
b. Lowers heart rate
c. Lowers blood pressure
d. Lowers respirations
e. Evokes the “relaxation response”
H. Naturopathy
1. Arose in the late nineteenth century in America
2. Works with natural healing forces within the body to restore health through nutrition, exercise, homeopathy, acupuncture, herbal medicine, hydrotherapy, massage, counseling, and/or pharmacology
I. Osteopathic medicine
1. A form of conventional medicine that emphasizes that diseases arise in the musculoskeletal system
2. Its paradigm is that all the body’s systems work together, and a disturbance in one system may affect functioning in other body systems.
J. Prayer
1. Addresses a “Supreme Being” or a “Higher Power” and implies a relationship between the individual and the “Higher Power”
2. Control of healing is given to a higher being.
3. Resembles meditation, bringing similar benefits such as lowered blood pressure and a strengthened immune system
K. Qigong—“Qi”
1. Pronounced “chee kung”
2. An ancient term denoting the vital energy of the body, and gong is the skill to work with qi
3. Part of traditional Chinese medicine
4. Combines movement, meditation, and regulation of breathing to remove blockages that stop or slow the flow of qi and to ensure an equal balance of qi within the body
5. Qigong masters can treat organ systems or body areas with or without physical contact.
6. Used to enhance the immune system, treat heart disease, stroke, hypertension, osteoporosis, cancer, and senility
L. Reflexology
1. Practiced by Egyptians as early as 2330 b.c.
2. A touch modality based on the principle that reflexes exist on each foot and hand that correspond to the glands, organs, and parts of the body.
3. Three different methods exist.
a. Foot—the most commonly practiced
b. Hand
c. Zone therapy
4. Used to reduce anxiety, stress and tension, and facilitate sleep
M. Reiki
1. A Japanese word denoting “Universal Life Energy”
2. Based on a belief that when spiritual energy is channeled through a Reiki practitioner, the patient’s spirit is healed, which heals the body
N. Yoga
1. An East Indian practice that has existed for 5000 years
2. The word yoga comes from the Sanskrit word yui, which means to unite.
3. A central belief of yoga is that a healthy body, mind, and spirit are needed for a healthy person.
4. Involves stretching exercises, breathing control, and meditation
5. Yoga training results in decreased sympathetic tone, decreased peripheral vascular resistance, improved cardiac output, and lowered blood pressure and heart rate.
a. Can help many conditions, including diabetes, epilepsy, obesity, asthma, depression, osteoarthritis, and cardiovascular disease
BIBLIOGRAPHY
1. American Massage Therapy Association, ASPAN’s evidenced-based clinical practice guideline for the prevention and/or management of PONV/PDNV, Available at:www.amtamassage.org; Accessed November 25, 2008.
2. American Society of PeriAnesthesia Nurses PONV/PDNV Strategic Work Team, ASPAN’s evidence-based clinical practice guideline for the prevention and/or management of PONV/PDNV, J Perianesth Nurs 21 (4) ( 2006) 230–250.
3. Barnes, J.; Abbot, N.C.; Harkness, E.F.; et al., Articles on complementary medicine in the mainstream medical literature: An investigation of MEDLINE, 1966 through 1996, Arch Intern Med 159 (15) ( 1999) 1721–1725.
4. Buckle, J., Clinical aromatherapy in nursing. ( 1997)Arnold, London.
5. Cheung, C.K.; Wyman, J.F.; Halcon, L.L., Use of complementary and alternative therapies in community-dwelling older adults, J Altern Complement Med 13 (9) ( 2007) 997–1006.
6. Cumulative index for nursing and allied health literature (CINAHL), Available at:www.cinahl.com; Accessed November 25, 2008.
7. Gach, M.R., Acupressure, Available at:www.acupressure.com; Accessed January 13, 2008.
8. HerbMed, Available at:www.herbmed.org; Accessed November 25, 2008.
9. Hulisz, D.T.; Wiebe, C.; Hart, C.A., Top herbal products: Efficacy and safety concerns, Available at:www.medscape.com/viewprogram/8494_pnt; Accessed January 1, 2008.
10. Kuhn, M.A.; Winston, D., Herbal therapy and supplements. ( 2000)Lippincott, Philadelphia.
11. National Center for Complementary and Alternative Medicine, Available at:http://nccam.nih.gov; Accessed August 7, 2008.
12. National Center for Complementary and Alternative Medicine, Paying for CAM treatment, Available at:http://nccam.nih.gov/health/financial/; Accessed August 11, 2008.
13. National Center for Complementary and Alternative Medicine, Available at:http://nccam.nih.gov; Accessed November 25, 2008.
14. Ness, J.; Cirillo, D.J.; Weir, D.R.; Nisly, N.L.; Wallace, R.B., Use of complementary medicine in older Americans: Results from the health and retirement study, Gerontologist 45 (4) ( 2005) 516–524.
15. Office of Dietary Supplements, National Institutes of Health, Black cohosh, Available at:http://ods.od.nih.gov/factsheets/blackcohosh.html; Accessed October 3, 2008.
16. PDR for essential oils. ( 1999)Essential Science Publishing, USA.
17. Prioreschi, P., Alternative medicine in ancient and medieval history, Med Hypotheses 55 (4) ( 2000) 319–325.
18. PubMed, Available at:www.ncbi.nlm.nih.gov/pubmed; Accessed November 25, 2008.
19. RJ Buckle Associates, Available at:www.rjbuckle.com; Accessed November 25, 2008.
20. The Nurse Healers–Professional Associates International and Therapeutic Touch, Available at:www.therapeutic-touch.org; Accessed November 25, 2008.
21. Weil, A., Guided imagery therapy. ( 2008)Weil Lifestyle, LLC; Available at:www.drweil.com/drw/u/id/ART00468; Accessed January 13, 2008.
22. Working to get ephedra banned, Consum Rep 68 (2) ( 2003) 6.
23. Wren, K.R.; Kimbrall, S.; Norred, C.L., Use of complementary and alternative medications by surgical patients, J Perianesth Nurs 17 (3) ( 2002) 170–177.
24. Wren, K.R.; Norred, C.L., Complementary and alternative therapies. ( 2003)W.B. Saunders, Philadelphia.