CHAPTER 17. Preexisting Medical Conditions
Lois Schick
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Identify patients with an increased perioperative risk.
2. State the specific perioperative nursing care priorities for the high-risk patient.
3. Describe techniques to reduce perioperative morbidity and mortality.
I. PREEXISTING MEDICAL CONDITIONS
A. Increases American Society of Anesthesiologists classification
B. Increases perioperative risk, morbidity, and mortality
C. May require multiple medications
1. Increased potential for drug interactions
2. Increased potential for laboratory test alterations
3. Increased potential for noncompliance
D. May jeopardize ambulatory status
II. CARDIOVASCULAR DISEASES (see Chapter 32)
A. Hypertension
1. Definition: systolic blood pressure (BP) >140 mm Hg and/or diastolic BP >90 mm Hg on three separate readings
a. Ideal BP of 120/80 mm Hg or less
b. Hypertensive crisis: BP >180/110 mm Hg or mean arterial pressure >150 mm Hg
2. Incidence: 24% of U.S. population; greater in males than females
3. Significance
a. Risk factor for coronary artery disease, cerebrovascular accidents, congestive heart failure, arterial aneurysm, and end-stage renal failure
b. Common in diabetics associated with diabetic neuropathy
4. Etiology and findings
a. Severe hypertension (diastolic BP >110 mm Hg): immediate evaluation with surgery cancelled because of increased cardiac morbidity
b. Primary (essential hypertension): untreated or inadequate treatment
(1) Accounts for >95% of patients
(2) Risk factors (Box 17-1)
BOX 17-1
PRIMARY RISK FACTORS FOR HYPERTENSION
Family history
Black race
Obesity
Hyperlipidemia
Diabetes
Tobacco use
Excessive alcohol use
Stress
Sedentary lifestyle
Aging
Oral contraceptives
High-fat diet, high-sodium diet, or both
(3) Poor compliance
(a) Lack of symptoms (silent myocardial infarction [MI])
(b) Side effects of pharmacological agents
(c) Cost of pharmacological agents
(4) Mechanisms
(a) Hyperactivity of sympathetic nervous system: epinephrine and norepinephrine increase cardiac contractility and vasoconstriction.
(b) Hyperactivity of renin-angiotensin-aldosterone system
(c) Endothelial dysfunction: vasoconstriction leads to hypertrophy of vascular smooth muscles.
c. Secondary (Box 17-2)
(1) Accounts for <5% causes
BOX 17-2
SECONDARY RISK FACTORS FOR HYPERTENSION
Increased renin-angiotensin levels
Acute and chronic glomerulonephritis
Eclampsia or preeclampsia of pregnancy
Central nervous system injuries (head, spinal cord)
Burns
Drug side effects: oral contraceptives, steroids, cocaine, amphetamines, methamphetamine, decongestants
Drug interactions: monoamine oxidase inhibitors, ethyl alcohol
Drug withdrawal: clonidine, beta-blockers, alcohol
Pheochromocytoma
Polycythemia
Coarctation of the aorta
Pituitary or adrenocortical hyperfunction: Cushing’s syndrome and primary hyperaldosteronism
Vasculitis
Scleroderma
5. Perianesthesia considerations
a. Advise patient to take routine prescription antihypertensive medication on day of surgery with sip of water.
b. Ask about presence of heart disease during preoperative interview.
c. Postoperative systemic hypertension warrants prompt assessment and treatment to minimize risks of myocardial ischemia, heart failure, stroke, and bleeding.
(1) Assess for pain.
(2) Assess for fluid overload.
B. Coronary artery disease (CAD)
1. Definition: accumulation of plaque within coronary arteries resulting in narrowing or obstruction
2. Incidence: common in men; predominantly younger than 55 years; equal in men and women older than 55
3. Significance: increased risk for MI, diabetes, hypertension, renal disease, dysrhythmias, high cholesterol, hyperlipidemia, congestive heart failure (CHF), familial incidence, and sudden death
4. Etiology
a. Atherosclerosis with obstructive deposits in coronary arteries
b. Common factors:
(1) Genetics
(2) Diet
(3) Environment
(4) Hypertension
(5) Diabetes
c. Myocardial ischemia may occur when there is an increase in oxygen demand in the following conditions:
(1) Increased sympathetic activity
(2) Surgical stress and pain
(3) Interruption of beta-blocker medications
(4) Use of sympathomimetic drugs
d. MI may occur because of reduced oxygen supply in the following conditions:
(1) Hypotension
(2) Vasospasm
(3) Anemia
(4) Hypoxia
5. Perianesthesia considerations
a. Requires evaluation and clearance from a cardiologist
b. May increase intraoperative monitoring requirements
c. Assess for any of following signs of CHF and if present, surgery may be cancelled.
(1) Shortness of breath
(2) Dyspnea on exertion or nocturnal
(3) Jugular venous distention
(4) Crackles
(5) Edema
d. Assess incidence and triggers of chest pain.
(1) If new onset (<2 months) or unstable, postpone surgery pending cardiologist evaluation.
(2) All prescription medications to be taken on morning of surgery with sip of water
e. Treatment:
(1) Coronary vasodilators (nitrates)
(2) Exercise
(3) Diet
(4) Weight loss
(5) Antihyperlipidemia drugs
(6) Aspirin
(7) Patient education
f. Second and third postoperative days are most common time for MI in noncardiac surgical patients.
g. Intraoperative ischemia designates patient as “high risk” in postoperative period.
C. Heart failure
1. Definition
a. Heart cannot pump enough blood to meet the body’s metabolic needs.
b. CHF is an interruption in circulation.
(1) Failure of heart to function normally
(2) Impairment of heart to fill or empty the left ventricle
(3) Congestion in lung and peripheral beds
(a) Respiratory symptoms
(b) Peripheral edema
2. Incidence
a. Most common inpatient diagnosis for patients older than 65 years
b. Complication of most cardiac disease: 4 to 5 million cases in United States
c. Primary diagnosis for 1 million hospitalizations
d. Medium survival after onset for men is 1.7 years and 3.2 years for women.
3. Significance: increased risk for pulmonary edema, dyspnea, peripheral edema
4. Etiology: CAD, myocardial infarction, rheumatic heart disease, volume overload, congenital heart disease, noncompliance with medications
a. Acquired acute or chronic cardiac disease
b. Congenital heart disease
c. Multiple precipitating causes
(1) Noncompliance with medications
(2) Excessive sodium
(3) Excessive intravenous (IV) fluids
(4) Drugs
(a) Beta-blockers
(b) Corticosteroids
(c) Nortriptyline
(d) Disopyramide
(e) Nonsteroidal anti-inflammatory drugs (NSAIDs)
(f) Androgens
(g) Estrogens
(h) Doxorubicin
(5) High-output states
(a) Pregnancy
(b) Fever
(c) Hyperthyroid
(d) Sepsis
(e) Arteriovenous fistula
(f) Anemia
5. Perianesthesia considerations
a. If symptomatic (see section II.B), surgery cancelled
b. Auscultate breath sounds on arrival, on admission to post anesthesia care unit phase I, and before discharge.
c. Obtain chest x-ray.
d. Obtain cardiologist clearance before surgery.
e. Increased mortality rate by 40% during first 4 years after diagnosis
f. Strict intake and output records
g. Aggressive pain management to avoid sympathetic activation of pulmonary edema intraoperatively and postoperatively
h. Regional anesthesia acceptable for peripheral operations
i. May need postoperative mechanical ventilatory support
j. Treatment:
(1) Diuretics
(2) Inotropic therapy
(3) Oxygen
(4) Low-sodium diet
(5) Ventricular assist devices
D. Mitral valve disease
1. Definition: prolapse or stenosis of mitral heart valve that results in resistance to left ventricular emptying (increased afterload)
a. Prolapse: billowing of posterior mitral leaf into the left atrium during systole
b. Regurgitation: the mitral valve does not close tightly which allows the blood to flow backward to the heart.
c. Stenosis: mechanical obstruction to left ventricular filling secondary to progressive decreases in the mitral valve orifice
2. Incidence: age <30 congenital; age >70 degenerative
3. Significance:
a. Increased risk of angina
b. Syncope
c. Fatigue
d. Dyspnea
e. Heart murmur on auscultation
f. Pulmonary embolism
g. Dysrhythmias
4. Etiology:
a. Congenital
b. Rheumatic heart disease
c. Aging
5. Perianesthesia considerations
a. It is suggested patients at greatest risk for a bad outcome from infective endocarditis take short-term preventive antibiotics before dental work.
b. Patients at greatest risk for bad outcomes include
(1) Artificial heart valves
(2) History of previous infective endocarditis
(3) Certain specific, serious congenital heart conditions
(4) Cardiac transplant that develops a problem in a heart valve
c. May be anticoagulated on warfarin; check prothrombin time/international normalized ratio (PT/INR)
(1) Patient may be asked to stop warfarin 3 days before surgery.
d. Risk of pulmonary edema
e. Avoid hypertension and acute increases in sympathetic tone.
f. Treatment
(1) Prolapse often requires no treatment.
(2) Regurgitation often requires valve replacement if ejection fraction <0.6.
(3) When symptoms increase or pulmonary hypertension develops, stenosis requires:
(a) Valve reconstruction
(b) Commissurotomy
(c) Valve replacement
(d) Prophylaxis against endocarditis
(e) Diuretics
(f) Anticoagulant therapy
(g) Low-sodium diet
(h) Controlling heart rate, because tachycardia impairs left ventricular filling and increases left atrial pressure
(i) Digoxin
(ii) Beta-blockers
(iii) Calcium channel blockers
E. Aortic valve disease (Table 17-1)
1. Insufficiency: also described as aortic regurgitation, aortic incompetence
2. Aortic stenosis
| ECG, Electrocardiogram; INR, international normalized ratio. | ||
| Insufficiency | Stenosis | |
|---|---|---|
| Definitions |
Aortic valve leaflets do not close properly
Blood flows back into left ventricle during systole
|
Stiff and fibrotic valve
Narrowing of aortic valve
|
| Incidence | Manifests in third to sixth decade | Manifests in third to sixth decade |
| Significance |
Dyspnea
Syncope
Congestive heart failure
ECG changes
Pulmonary edema
Exercise intolerance
|
Dyspnea on exertion
Chest pain (angina)
Syncope
Congestive heart failure
Exercise intolerance
Risk for bacterial endocarditis
|
| Etiology |
Rheumatic heart disease
Congenital
Marfan syndrome
Acquired disease (syphilis, aortic dissection)
Infection (endocarditis)
Trauma
|
Congenital defect
Rheumatic heart disease
Calcification
|
| Perianesthesia considerations | PREPROCEDURE
Continue preoperative medications
Monitor atrial fibrillation
Check INR
Antibiotic therapy
POST PROCEDURE Suppress catecholamines on emergence
May have delayed emergence
Monitor cardiac output
Treat atrial dysrhythmias
Restart preoperative medications (digoxin, diuretics)
Maintain or increase contractility (use dopamine)
Decrease afterload (nicardipine, nitroprusside)
Anticoagulate
|
PREPROCEDURE
Continue preoperative medications (anticoagulant therapy)
Suppress catecholamines (control pain)
POST PROCEDURE Avoid tachycardia
Avoid histamine and catecholamine release
Consider dexmedetomidine infusion (provides analgesia without respiratory depression; can delay awakening; can potentiate beta-blockers)
Restart preoperative medications
Digoxin, diuretics, anticoagulants if chronic atrial fibrillation)
|
F. Dysrhythmias
1. Definition: alteration in conduction system requiring pharmacological or surgical (automatic implantable cardiac defibrillator [AICD], pacemaker) intervention
2. Incidence: very common (dysrhythmias)
a. Use of pacemakers and AICDs increases with age.
b. Common outcome of coronary artery disease
3. Significance: increased risk of MI and progression to lethal dysrhythmias
4. Etiology:
a. CAD
b. CHF
c. Valve disease
d. Myocardial infarction
e. Hypoxia
f. Hypercarbia
g. Electrolyte imbalance
h. Acid-base alterations
i. Altered activity of the autonomic nervous system
j. Drugs (i.e., volatile anesthetics, catecholamines)
5. Perianesthesia considerations
a. Treatment: pharmacological, patient education, pacemaker (heart block, asystole), cardioversion, AICD (ventricular fibrillation)
b. Perioperative significance
(1) Patient to take anti-dysrhythmic medications on day of surgery
(2) Inquire about type of pacemaker and setting (patient may have pacer identification card); document in chart (may need to call cardiologist).
(3) Have external pacemaker readily available.
(4) Have cardiologist available, although not necessarily in the operating room (OR).
(5) If patient has AICD, bovie or cautery should not be used during surgery.
(a) If bovie or cautery must be used, AICD is turned off.
(b) External defibrillator must be available in OR suite for immediate use if needed.
III. PULMONARY DISEASES (see Chapter 31)
A. Chronic obstructive pulmonary disease (COPD)
1. Definition: term includes chronic bronchitis and emphysema.
a. Bronchitis
(1) Chronic productive cough caused by excess bronchial mucus secretions
(2) Reduction in expiratory flow rate
(3) Signs include cough, increased sputum production, dyspnea, wheezing.
b. Emphysema
(1) Characterized by abnormal permanent enlargement air spaces distal to terminal bronchioles
(2) Destruction of parenchyma
(3) Increased minute ventilation to compensate for hypercapnia
(4) Signs include barrel chest, pursed lip breathing, decreased breath sounds, dyspnea.
2. Incidence: 20% to 30% of adults younger than 40 years; greater in males than in females
3. Significance: hypoxia, hypercapnia, pneumonia, respiratory failure, bronchospasm, atelectasis
4. Etiology: cigarette smoking, air pollution, occupational exposure to smoke
5. Perianesthesia considerations
a. Treatment: bronchodilators, possibly anticholinergics and corticosteroids, patient education to stop smoking at least 8 to 10 weeks before surgery
b. General anesthesia may exacerbate symptoms and disease; regional anesthesia avoids intubation and use of controlled ventilation.
c. Patient’s respirations controlled by hypoxic drive.
(1) High flow, high concentration of oxygen may produce apnea.
(2) Nasal cannula <3 L oxygen preferred delivery system unless unable to maintain saturation
d. Encourage deep breathing and coughing after general anesthesia; postoperative pulmonary infections common
e. Ask patient to bring inhalers used to the facility on day of surgery.
f. Pulmonary function tests may be ordered preoperatively.
g. Consider impact of neuraxial blockade and/or sedation if COPD.
(1) COPD patients rely on intercostals and abdominal muscles.
(a) Clearing of secretions affected
(b) Coughing ability impacted
(c) Avoid techniques that provide sensory anesthesia above T6.
B. Asthma
1. Definition: tracheobronchial disorder characterized by obstruction to airflow secondary to narrowing of airways, edema, and inflammation
2. Incidence: 22 million cases in United States; affects 6 million children
3. Significance: increased risk of laryngospasm and bronchospasm on induction, hypoxemia, decreased peak flow rates
4. Etiology: allergic factors, genetic predisposition, smoke, infection, cold air, exercise, and occupational exposures such as grain dust, plastics, and fumes
5. Perianesthesia considerations
a. Treatment: oxygen, bronchodilators (beta-2 agonists), corticosteroids (acute asthma), mast cell stabilizers, education, mechanical ventilation
b. Encourage patient to avoid known irritants to minimize wheezing.
c. Question patient on the frequency, severity, and management of attacks.
d. Auscultate breath sounds preoperatively and postoperatively.
e. Increased risk of bronchospasm on intubation and emergence
f. Halothane, sevoflurane, and ketamine may be used because they cause bronchodilation during administration.
g. Ask patient to use and to bring any inhalers used to the facility on day of surgery.
h. If receiving steroids, determine last use and dose; may need steroid preoperatively.
(1) Steroids by inhalation diminish systemic affects.
(2) If steroid-resistant asthma, IV immunoglobin may be administered.
(3) If patient with severe asthma receiving long-term oral corticosteroid therapy, a burst of corticosteroids may need to be administered to prevent adrenal insufficiency.
i. Cancel surgery if patient has an upper respiratory infection.
C. Smoking
1. Definition: use of inhaled tobacco
2. Incidence: extremely common; teenagers, adults, and elderly. Young females fastest growing group
3. Significance: increased risk of COPD, heart disease, hypertension, peripheral vascular disease, hypoxia, poor tissue healing, postoperative pulmonary complications six times greater than that of nonsmoker, hyper-reactive airway, higher rate of prolonged mechanical ventilation
4. Etiology: access to and use of product, habituation
5. Perianesthesia considerations
a. Treatment: cessation, nicotine patch, Smokers Anonymous, self-withdrawal
b. Patient has elevated carboxyhemoglobin levels.
c. Carbon monoxide has greater affinity for hemoglobin than does oxygen.
d. Increased risk of bronchospasm and laryngospasm on induction, intubation, emergence
e. Encourage patient to stop smoking 8 weeks before surgery; be aware that most will not comply. No smoking on day of surgery.
f. If chronic productive cough, preoperative antibiotics may be used.
g. Consider deep extubation if severe reactive airway disease.
h. Epidural analgesia may be beneficial
(1) To decrease hypercoagulability
(2) In patients with CAD
(3) In patients with COPD
i. Risks associated with cigarette smoking (Table 17-2)
| Cardiovascular |
Coronary artery disease
Peripheral vascular occlusive disease
Cerebrovascular disease
Stroke
|
| Respiratory |
Chronic obstructive pulmonary disease
Reduced lung function
|
| Gastrointestinal |
Peptic ulcer disease
Esophageal reflux
Gum disease
Tooth loss
|
| Cancer |
Lung
Oral cavity
Larynx
Esophagus
Stomach
Pancreas
Kidney
Urinary bladder
Colon
|
| Gestational | PERINATAL
Increases in miscarriage; stillbirth; low birth weight
Sudden infant death syndrome
Impaired intellectual development
MATERNAL Increases in abruptio placenta and placenta previa
|
| Ophthalmic | Macular degenerationCataracts |
| Musculoskeletal |
Osteoporosis
Spinal disc disease
|
| Reproductive | Infertility |
| Immune | Inhibited immune function |
| Dermatologic | Premature facial wrinkling |
D. Obstructive sleep apnea
1. Definition: repetitive episodes of upper airway occlusion during sleep often with oxygen desaturation; apnea defined as cessation of airflow at mouth for >10 seconds
2. Incidence
a. Middle-aged women, 2%; middle-aged men, 4%
b. Suspected that 80% of cases undiagnosed
3. Significance:
a. Obesity with body mass index >30 and large neck circumference
b. High risk of postoperative complications when undergoing general anesthesia
c. Systemic and pulmonary hypertension
4. Etiology: chronic decrease in partial pressure of oxygen in arterial blood (Pa o2) during apneic episodes, pharyngeal fat deposits, obesity exacerbate upper airway obstruction
5. Perianesthesia considerations
a. Preoxygenation because of reduced functional residual capacity
b. Extubation when breathing spontaneously
c. Repetitive apnea can occur with opioid and benzodiazepine administration.
d. Bring in continuous positive airway pressure for postoperative usage.
e. Assess cardiovascular status.
f. Preoperative histamine (H 2) blockers and antacids for morbidly obese
g. Potential for airway obstruction at induction and on extubation
h. Aspiration risk
i. Postoperative thromboembolism
j. Worsening pulmonary hypertension and right-sided heart failure
k. Consider candidate for apnea even several hours postoperatively, especially after epidural anesthesia.
IV. RENAL DISEASES (see Chapter 37)
A. Acute renal failure (ARF)
1. Definition: impairment or cessation of kidney function characterized by accumulation of nitrogenous waste and fluid and electrolyte imbalance
2. Significance: patient will experience derangement in fluid-electrolyte balance, acid-base homeostasis, calcium/phosphate metabolism, BP regulation, and erythropoiesis.
3. Incidence: 5% of hospitalized patients have coexisting renal disease that could contribute to perioperative morbidity.
4. Etiology
a. Prerenal: decreased renal blood flow leads to hypoperfusion.
(1) Hypovolemia
(2) Hypotension
(3) Vasoconstriction
(4) Inadequate cardiac output
b. Renal (intrinsic): damage to filtering structure of kidneys
(1) Ischemia
(2) Nephrotoxins
(3) Inflammation
c. Postrenal: urinary tract obstruction
(1) Prostatic hypertrophy
(2) Cancer of prostate or cervix
(3) Congenital anomalies
d. ARF pass through three distinct phases.
(1) Oliguric phase
(a) Necrosis of tubules
(b) Retrograde increase in pressure
(c) Decrease in glomerular filtration rate (GFR)
(d) Inability to conserve sodium
(e) Fluid volume excess
(f) Azotemia
(g) Electrolyte imbalance
(h) Renal failure can occur within 24 hours
(2) Diuretic phase
(a) Increased urine secretion of >400 mL/24 hours
(b) GFR increased or normal
(c) Increased blood urea nitrogen (BUN) produces osmotic diuresis, deficits of sodium and potassium.
(d) May last days or weeks
(3) Recovery phase
(a) Gradual return to normal or near normal
(b) Occurs in 3 to 12 months
5. Perianesthesia considerations
a. Patient inappropriate for ambulatory surgery
b. Assess hemoglobin and hematocrit levels.
c. Measure intake and output accurately.
d. Maintain proper electrolyte balance.
e. Use sterile technique because highly susceptible to infections.
B. Chronic renal failure (CRF)
1. Definition: progressive, irreversible disruption of the excretory and regulatory function of the nephron; inability to eliminate waste products and maintain fluid and electrolyte balance. When renal replacement therapy is required, the patient has end-stage renal disease (ESRD).
2. Incidence: 500,000 patients affected by ESRD in United States; 1.4 times higher for males than females, and 4 times higher for African Americans. CRF will develop in 25% to 30% of patients with ARF.
3. Significance: patients commonly diabetic with multiple laboratory alterations, hypertension and anemia
4. Etiology: pyelonephritis, polycystic kidneys, autoimmune, diabetes mellitus, drug-induced nephropathy (antibiotics, NSAIDs), hypertension, congenital
5. Perianesthesia considerations
a. All anesthetic techniques have potential to reduce renal perfusion.
b. Obtain preoperative weight.
c. Obtain preoperative glucose level in diabetic patients.
d. Determine date of last dialysis; if off schedule, anticipate fluid and electrolyte imbalance.
e. Instruct patient to take antihypertensive medications on day of surgery.
f. Anemia may compromise oxygenation, especially with hematocrit <18%.
g. Monitor electrolytes (potassium, BUN, serum creatinine) and renal function (urinalysis) preoperatively, as well as complete blood count and bleeding time.
h. Careful intake and output; may be on fluid restriction
i. Use of lactated Ringer’s or dextrose in lactated Ringer’s may lead to acidosis; use 0.9% normal saline or 5% dextrose in one-half normal saline.
j. Avoid same-arm venipunctures and BPs if patient has arteriovenous fistula for hemodialysis.
k. Avoid nephrotoxic drugs.
l. Consider decreased doses of medications eliminated through kidneys; avoid meperidine and potassium-containing solutions.
m. Increased risk for infection
n. Poor tolerance for physiological stress
o. Treatment: renal replacement therapy, hemodialysis, peritoneal dialysis, ultrafiltration, renal transplantation, diet, patient education
V. LIVER DISEASES
A. Key functions of liver
1. Detoxifies chemicals
2. Makes bile
3. Stores energy
4. Manufactures new proteins
5. Produces plasma
B. Hepatitis
1. Definition
a. Diffuse inflammation of liver
b. Infectious or noninfectious
c. Acute hepatitis is an inflammatory disease of hepatocytes.
(1) Most often caused by a virus
(2) May be from drugs and toxins
(3) Lasts less than 6 months
d. Chronic hepatitis (active): widespread destruction of hepatocytes causing cirrhosis and hepatic failure
(1) Nonprogressive inflammatory disease confined to portal areas
(2) Lasts more than 6 months
2. Incidence (varies with cause)
a. Hepatitis A: 25% of cases
(1) Active viral hepatitis associated with high morbidity and mortality
(2) Elective surgery should not be performed on patients until 4 weeks after blood tests normalized.
b. Hepatitis B: 3% to 5% of population has disease, whereas 0.3% to 1% are carriers.
c. Hepatitis C: most common cause of acute viral hepatitis; greater in males than in females
3. Significance: hepatitis in presence of alcoholism increases risk of cirrhosis and depending on extent of disease, may have alterations in:
a. Coagulation
b. Fluid and electrolytes
c. Wound healing
4. Etiology: viral
a. Hepatitis A: transmitted enterically (fecal-oral route)
(1) Contaminated water
(2) Raw or partially cooked shellfish
(3) Infectious
(a) Two weeks before jaundice
(b) One week after jaundice
b. Hepatitis B: carried in and spread by blood and body fluid including sexual contacts
c. Hepatitis C: transmitted via blood transfusions and body fluids, although in 50% of cases route of transmission unknown
(1) Fifty percent of infected cases become chronic.
(2) No immunity is developed.
(3) Leading cause of liver transplantation in United States
d. Chronic infection from hepatitis leads to cirrhosis and liver cancer.
5. Perianesthesia considerations
a. Treatment: supportive because disease is viral
(1) Hepatitis A: immune globulin, hepatitis A vaccine, treat at home unless dehydrated
(2) Hepatitis B: hepatitis B vaccine for prevention, hepatitis B immune globulin for passive immunization, bed rest, and orthotopic liver transplantation for liver failure
(3) Hepatitis C: type 1 interferon with or without ribavirin; orthotopic liver transplantation for liver failure
b. Patients with acute hepatitis are inappropriate for ambulatory surgery.
c. Patients with chronic persistent hepatitis should be evaluated by a gastroenterologist before surgery.
d. Consider obtaining preoperative liver enzymes to compare with previous levels.
(1) Increases reflect worsening of disease.
(2) Requires medical evaluation before surgery
e. Anticipate hypoglycemia and potential fluid overload postoperatively.
f. Be cognizant of potential for delayed awakening from prolonged drug metabolism or encephalopathy.
g. Vigilance to universal precautions
C. Cirrhosis—liver failure
1. Definition: hepatic fibrosis producing portal hypertension including ascites, variceal bleeding, hepatic encephalopathy
2. Incidence: 30,000 deaths per year; greater in males than in females
3. Significance: inappropriate for ambulatory surgery
4. Etiology: excessive alcohol ingestion, chronic viral hepatitis
5. Perianesthesia considerations
a. Volatile anesthetics decrease hepatic blood flow.
b. At risk for aspiration
c. Treatment
(1) Parenteral vitamin K if PTs prolonged
(2) Monitor arterial blood gases, pH.
(3) Monitor intake and urine output.
(4) Monitor for hypoglycemia.
d. Ensure adequate hydration.
D. Alcohol abuse (Table 17-3)
1. Definition: illness characterized by significant impairment associated with persistent and excessive use of alcohol
a. Physiological impairment
b. Psychological impairment
c. Social impairment
2. Incidence: 10% of men; 3.5% of women; 11% to 15% of all adults; highest incidence between 18 and 39 years of age
3. Significance: associated with malnutrition, poor compliance, hypertension, pulmonary disease with concomitant cigarette use, stroke, diabetes, gastrointestinal (GI) disease
4. Etiology: biological, psychological, and sociocultural factors
5. Perianesthesia considerations
a. Compliance with preoperative and postoperative instructions may be poor.
b. Determine usual consumption, time, and amount of last drink.
c. Patients arriving intoxicated for ambulatory procedures should have surgery cancelled.
d. Malnutrition may compromise wound healing.
e. Correct hyponatremia and hypokalemia slowly (over 24-48 hours).
f. Aberrant responses to narcotics and benzodiazepines
g. At risk for cirrhosis, alterations in coagulation, and bleeding
h. Delirium tremens may require heavy sedation or restraints to prevent patient self-injury.
(1) First sign of delirium tremens in patient still sedated after general anesthesia may be tachycardia.
(2) Occurrence of delirium tremens in perioperative period associated with high incidence of morbidity and mortality
i. Increased incidence of aspiration pneumonitis
(1) Concomitant pulmonary disease will require aggressive postoperative pulmonary hygiene.
j. Long-term consumption impairs hepatic metabolism; short-term consumption inhibits drug metabolism.
k. Polyneuropathy is a relative contraindication to regional anesthesia.
| Early manifestations |
Generalized tremor
Autonomic nervous system hyperactivity
Insomnia
Agitation
|
| Delirium tremens (2-4 days after cessation of alcohol ingestion) |
Hallucinations
Combativeness
Hyperthermia
Tachycardia
Hypotension/hypertension
Seizures
|
| Treatment |
Diazepam (5-10 mg IV every 5 minutes until patient becomes calm)
Esmolol until heart rate <100 beats/min
Correction of electrolyte (magnesium) and metabolic (thiamine) derangements
Lidocaine
Physical restraining
|
VI. NEUROMUSCULAR, SKELETAL, CONNECTIVE TISSUE DISEASES (see Chapters 33 and 42)
A. Spine Curvature
1. Definition: C-shaped or S-shaped lateral curvature of vertebral spine
a. Kyphosis: anterior flexion of vertebral column
b. Scoliosis: lateral curvature of vertebral column
2. Incidence: greater in women than in men (80% women)
3. Significance: most commonly diagnosed and treated in childhood during maximal growth period
4. Etiology: idiopathic, congenital, neuropathic, myopathic, or traumatic
5. Perianesthesia considerations
a. Severe deviations (>50 °) can compromise cardiopulmonary function.
b. Any significant curvature involving the thoracic spine may alter lung function: obtain preoperative pulmonary function tests and institute aggressive pulmonary care postoperatively.
c. Curvature can cause lower back pain.
d. Deformity may compromise intraoperative positioning.
e. Patients with concomitant myopathies likely to require postoperative ventilation; inappropriate as outpatients
f. In childhood and adolescence: exercises, weight reduction, bracing, casting, surgery (spinal fusion with rod placement)
g. In adults: spinal fusion
h. Avoid depressant drugs.
B. Arthritis: rheumatoid and osteoarthritis
1. Definitions
a. Rheumatoid: chronic inflammatory disease of multiple joints producing disability and disfigurement
b. Osteoarthritis: degenerative disease of articular cartilage with minimal inflammation
2. Incidence
a. Rheumatoid: 1 in 1000 children; greater in females than in males; most common between ages of 30 and 50 years
b. Osteoarthritis: 63% to 85% of Americans older than 65 years; 20 million patients
3. Significance
a. Rheumatoid: increased incidence of cardiopulmonary involvement
b. Osteoarthritis: most common form of joint disease with stiffness, discomfort, pain
4. Etiology
a. Rheumatoid: unknown, includes genetics, altered immune response, trauma
b. Osteoarthritis: aging, genetics
5. Perianesthesia considerations
a. Rheumatoid arthritis
(1) Joint stiffness worse in morning; consider afternoon scheduling.
(2) Pericardial effusion, thickening present in one third of adults
(3) Pleural effusion is the most common pulmonary alteration.
b. Osteoarthritis
(1) Corticosteroids not recommended; increased risk of degenerative joint changes
c. Arthritis (both types)
(1) Cervical spine and temporomandibular joint involvement may restrict neck mobility for intubation; may require use of fiberoptic bronchoscopy.
(2) Limited joint mobility may compromise intraoperative positioning.
(3) NSAIDs can alter platelet function and coagulation and cause mild anemia.
(4) Obtain preoperative coagulation studies, hemoglobin, and hematocrit.
(5) Treatment: goal is to maintain joint function and to minimize disability.
(a) Rheumatoid: symptomatic, NSAIDs, gold, methotrexate, corticosteroids, and newer treatment with combination of tumor necrosis factor (TNF) blocking drugs with methotrexate for patients who failed traditional disease modifying anti-rheumatic drugs
(b) Osteoarthritis: NSAIDs and heat
C. Muscular dystrophy (MD)
1. Definition
a. Progressive disease of muscle resulting in painless degeneration and atrophy of skeletal muscles
(1) Caused by increased permeability of skeletal muscle membranes and presents with decreased cardiopulmonary reserve
(2) Ten different varieties, with Duchenne’s MD most common and severe
(3) Inappropriate for ambulatory surgery because of late respiratory depression
b. Incidence: 1:544,000 in United States, which is 500 newborn boys per year; Duchenne’s most prevalent in children, whereas myotonic MD more common in adults. Becker’s MD is a milder form of Duchenne’s MD.
c. Significance: gait problems, waddling gait, falls, difficulty standing up, difficulty climbing stairs, difficulty descending stairs, lordosis, firm-looking muscles, enlarged muscles, enlarged calf muscles
d. Etiology: various genetic mechanisms involving enzymatic or metabolic defect, X- linked recessive disorders
e. Perianesthesia considerations
(1) Provide limited sedation.
(2) Succinylcholine is contraindicated because of hyperkalemia.
(3) Encourage coughing, deep breathing exercises including diaphragmatic breathing.
D. Myasthenia gravis (see Chapter 19)
1. Definition: chronic autoimmune disease of neuromuscular junction
a. Causes disturbance in transmission of impulses between motor neurons and innervated muscle cells
b. Results in fatigue and diminished muscle strength
2. Incidence: 5-14 people per 100,000 with incidence of women aged 20 to 30 years, older than 60 years
3. Significance: disease classified as type I to IV based on skeletal muscle involvement and severity of symptoms
a. Type I: involvement of only extraocular eye muscles
b. Type IIA: slow, progressive mild skeletal muscle weakness without respiratory muscle involvement
c. Type IIB: severe, rapidly progressive form of skeletal muscle weakness with respiratory muscle weakness
d. Type III: acute onset, rapid deterioration of skeletal muscle strength with high mortality
e. Type IV: severe skeletal muscle weakness that results from progression of type I or type II
4. Etiology: unknown; thymus gland abnormality; autoimmune disease of neuromuscular junction mediated by reduction in number of acetylcholine receptors at neuromuscular junction
5. Perianesthesia considerations
a. Not appropriate for ambulatory surgery if type IIB, III, or IV
b. Will likely require prolonged postoperative ventilatory support
c. Anticholinesterase drugs alter effects of nondepolarizing muscle relaxants with variable responses.
d. Susceptible to respiratory depression
e. Consider epidural analgesics.
f. Treatment: anticholinesterase drugs pyridostigmine (Mestinon), corticosteroids, immunosuppressants, plasmapheresis, thymectomy
E. Parkinson’s disease (paralysis agitans) (see Chapter 19)
1. Definition: slow adult-onset, progressive disease of central nervous system (CNS) degeneration characterized by classic triad of resting tremor, muscle rigidity, and bradykinesia (slow movement)
2. Incidence: 50,000 new cases per year; greater in men than in women; onset >40 years of age
3. Significance: do not assume presence of mental status changes.
4. Etiology: possible genetic predisposition
5. Perianesthesia considerations
a. Physical limitations may increase need for assistive devices.
b. Continue levodopa on day of surgery—interruption of drug for 6 to 12 hours can result in loss of drug’s therapeutic effect, including difficulty in maintaining ventilation.
c. Levodopa may produce orthostatic hypotension, dysrhythmias, hypertension.
d. Use of phenothiazines (Compazine) and butyrophenones (Droperidol) contraindicated—may produce extrapyramidal effects
e. Depression common in advanced stages of disease (if monoamine oxidase [MAO] inhibitors being used, notify anesthesiologist)
f. Intravascular volume depletion and inadequate response to hypotension make BP and heart rate fluctuate.
g. Ketamine may cause exaggerated sympathetic response.
h. Potential hyperkalemic response to succinylcholine
i. Postoperative period
(1) Close attention to respiratory status
(2) Close attention to CNS state
(3) Begin anti-Parkinson’s therapy immediately after surgery.
j. Treatment: no cure
(1) Goal is to control symptoms and to slow disease course.
(2) Dopaminergics
(a) Levodopa
(b) Levodopa in combination with Carbidopa (Sinemet, Parcopa)
(c) Bromocriptine mesylate (Parlodel)
(d) Pramipexole (Mirapex)
(e) Amantadine hydrochloride (Symmetrel)
(f) Ropinirole (Requip)
(g) Dopaminergics are contraindicated with:
(i) Glaucoma
(ii) Within 2 weeks of administration of MAO inhibitors
(3) Stereotaxic surgery
(4) Experimental treatment with fetal adrenal implantation
F. Multiple sclerosis (MS) (see Chapter 19)
1. Definition: autoimmune demyelinating disease that affects both the spinal cord and brain
2. Incidence: MS usually begins between ages of 20 and 40 years; 8:1 women to men; occurs in temperate climates.
3. Significance: injuries from falls, urinary tract infection, joint contractures, pressure ulcers
4. Etiology: unknown
a. Slow-acting or latent viral infection, an autoimmune response, environmental and genetic factors
b. Emotional stress, overwork, fatigue, pregnancy, and acute respiratory tract infections exacerbate or precede onset
5. Perianesthesia considerations
a. Document preoperative neurologic status.
b. May need premedication with benzodiazepines
c. Provide adequate volume status.
d. Consider steroid supplementation.
e. Exacerbation of MS with hyperthermia
f. Hyperkalemia with succinylcholine
G. Lupus erythematosus
1. Definition
a. Chronic inflammatory disorder of connective tissues
(1) Discoid lupus erythematosus (skin)
(2) Systemic lupus erythematosus
b. Characterized by recurring remissions and exacerbations
2. Incidence 1:1000; females greater than males; majority of patients aged 30 to 40 years at time of diagnosis
3. Significance: respiratory obstruction, systemic vascular collapse
4. Etiology: unknown; autoimmune process possibly after trauma to mast cells
5. Perianesthesia considerations:
a. Steroid dose if receiving long-term steroid therapy
b. Careful titration of fluid; accurate intake and output
c. Assess respiratory, renal, cardiovascular status before extubation.
d. Treat with rest, steroids, salicylates.
H. Systemic sclerosis
1. Definition
a. Disease state causing changes in connective tissue that affect synovium, skin, blood vessels, and internal organs
b. Scleroderma: disorder affects only skin
c. Rare chronic autoimmune condition
2. Incidence
a. Women greater than men: 3:1 to 7:1
b. More prevalent in women between ages of 35 and 54 years
c. More prevalent in Native Americans and African Americans
3. Significance
a. Painless edema in hands and fingers
b. Taut and shiny skin that lacks elasticity
c. Loss of range of motion in joints, leading to contractures
d. As sclerosis progresses, process of hardening and fibrosis adversely affects internal organs and structures, including heart and lungs.
4. Etiology: autoimmune, hormones, and environment play a role.
5. Perianesthesia considerations:
a. Proton pump inhibitors to reduce gastric acid preoperatively
b. Skin temperature may be 1.5 ° C lower than core temperature.
c. Maintain fluid and electrolyte balance; may be hypovolemic due to vasoconstriction.
d. May initially see hypertension followed by vasodilatation and hypotension
e. Anticipate potential for difficult airway, hypoxemia, and hypotension.
f. Treatment includes antifibrinolytic agents, anti-inflammatory drugs, immunosuppressive therapy, and vascular drugs.
VII. ENDOCRINE DISEASES (see Chapter 34)
A. Characterized by an overproduction or underproduction of single or multiple hormones
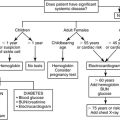
B. Diabetes mellitus (DM)
1. Definition: metabolic dysregulation of glucose metabolism related to insulin deficiency, resistance, and/or abnormal gluconeogenesis
a. Chronic, systemic disease producing altered glucose metabolism and hyperglycemia
b. Insulin-dependent DM (IDDM, type I, ketosis prone) commonly develops in childhood and adolescents.
(1) Patient produces no insulin.
(2) Requires insulin to sustain life
c. Non–insulin-dependent DM (NIDDM, type II nonketosis prone)
(1) Commonly managed with diet and oral hypoglycemic agents
(2) May require insulin
(3) Federal health statistics revealed in 2005
(a) 57 million Americans have prediabetes.
(b) About 2 million U.S. adolescents have prediabetes.
2. Incidence: 23.6 million people in the USA (7.8% of population) have diabetes.
3. Significance: increased risk of macroangiopathy (CAD, cerebrovascular disease, peripheral vascular disease), microangiopathy (retinopathy, nephropathy), and CNS disorder (autonomic nervous system neuropathy, peripheral neuropathy)
4. Etiology
a. IDDM: autoimmune, viral, genetic, environmental
b. NIDDM: genetic, obesity
5. Perianesthesia considerations
a. Treatment: diet, oral hypoglycemic agents (not with IDDM), insulin, exercise, BP control; pancreatic transplant optional if renal disease is end stage in IDDM cases.
b. Ultimate goal: to mimic normal metabolism, avoid hypoglycemia, excessive hyperglycemia, ketoacidosis, and electrolyte disturbances
c. Patients will require glucose-containing IV solutions to prevent hypoglycemia and insulin to prevent ketosis and hyperglycemia.
(1) Goal: blood glucose level of 80 to 110 mg/dL
d. Diabetic patients ideally scheduled early in day to avoid prolonged fasting.
e. Continue insulin on day of surgery (some physicians request half-normal dose—check facility policy); alternative is to hold insulin on day of surgery and to monitor blood glucose levels during surgery.
f. Oral hypoglycemic agents commonly held because hypoglycemia common without caloric intake
g. Obtain preoperative electrocardiogram, electrolytes, glucose (may vary with facility policy).
(1) Most common cause of perioperative morbidity in diabetic patients is ischemic heart disease.
h. Presence of autonomic nervous system dysfunction may increase risk of aspiration and cardiovascular instability.
i. Peripheral neuropathy may influence selection of regional anesthesia.
j. Regional: diabetic nerves may be more prone to edema and ischemia, especially if the vasoconstrictor epinephrine is used. There is decreased perfusion of an already compromised nerve.
k. IV solutions commonly contain potassium.
l. All supplemental insulin to be given IV to prevent unpredictable subcutaneous absorption
m. Limited joint mobility and obesity may make intubation difficult.
n. Infections and end-organ risk substantially increased with blood sugar >250 mg/dL.
C. Adrenocortical insufficiency (Addison’s disease)
1. Definition: absence of cortisol and aldosterone owing to destruction of adrenal cortex
2. Incidence: 1 in 100,000 in United States; affects all ages; no race or gender predominance
3. Significance: endocrine or hormonal disorder and metabolic alterations
4. Etiology: autoimmune, tuberculosis (TB), acquired immunodeficiency syndrome (AIDS), adrenal hemorrhage in anticoagulated patient
5. Perianesthesia considerations
a. Steroid dose may be increased for patients undergoing surgical procedure because patients are unable to increase release of endogenous cortisol to meet physiologic stress; can lead to cardiovascular collapse.
b. Most minor ambulatory procedures require no change of steroid dose.
c. Instruct patient to take steroid medication on morning of surgery.
d. Correct hypovolemia, hyperkalemia, hyponatremia, hypoglycemia.
e. May administer benzodiazepine before surgery
f. Chest x-ray for pneumothorax if adrenalectomy
g. Increased pancreatitis seen with left adrenalectomy
h. Cardiac dysrhythmias with hyperkalemia
i. Perioperative steroids may:
(1) Decrease wound healing
(2) Increase infections
(3) Increase stress ulcers
(4) Increase glucose intolerance
(5) Increase BP
j. Treatment: corticosteroid replacement
VIII. HEMATOLOGIC DISEASES (see Chapter 29)
A. Anemia
1. Definition: deficiency of erythrocytes (red blood cells)
a. Females: hemoglobin <11.5 g/dL (hematocrit 36%)
b. Males: hemoglobin <12.5 g/dL (hematocrit 40%)
2. Incidence: common
3. Significance: will compromise oxygen delivery to cells
4. Etiology
a. Iron deficiency anemia: due to inadequate intake of iron rich foods or absorption deficiency; seen most commonly in premenopausal women, infants, children, and adolescents
b. Pernicious anemia: caused by a deficiency of intrinsic factor, which is necessary for absorption of vitamin B 12
c. Folic acid deficiency anemia
d. Acute blood loss anemia: seen with gastrointestinal or genitourinary trauma and coagulopathies
e. Chronic disease in adults (renal failure and cancer)
f. Aplastic anemia: bone marrow fails to produce blood cells.
g. Sickle cell anemia: hereditary; affects primarily persons of African, Hispanic, Mediterranean, or Middle East descent
5. Perianesthesia considerations
a. No minimally accepted standard of hemoglobin concentration required for surgery
b. Low hemoglobin level does not require transfusion.
c. Low hemoglobin level does not compromise wound healing.
d. Low hemoglobin level does not increase risk of infection.
e. Decision to transfuse intended only to increase oxygen-carrying capacity
f. Patients with compromised oxygenation not candidates for ambulatory surgery
g. Keep patient warm postoperatively, prevent shivering.
h. Maintain high PaO 2.
i. Avoid hyperventilation or acute alkalosis.
B. Sickle cell anemia
1. Definition: chronic hemoglobinopathy with varying quantities of hemoglobin S (normal is hemoglobin A), resulting in vascular occlusion and compromised tissue oxygenation
2. Incidence:
a. 8% to 10% of all African Americans with sickle cell trait (defined as hemoglobin S concentration <50%)
b. 0.2% of all African Americans with sickle cell disease (hemoglobin S 70%-98%)
c. 1 in 500 African Americans
d. Also present in persons from India and Saudi Arabia
3. Significance: characterized by chronic hemolysis (anemia) and acute vasoocclusive crisis that causes organ failure and can be life threatening
4. Etiology: inherited, autosomal recessive
5. Perianesthesia considerations
a. Patients in sickle cell crisis inappropriate for ambulatory surgery
b. Patients with sickle cell trait not at increased risk during perioperative period
c. Patient with sickle cell disease must be free of infection, hydrated, and hemodynamically stable preoperatively.
d. Obtain sickle cell lab test in all African Americans younger than 15 years.
(1) If by age 15, patient has never been tested nor had sickle cell disease diagnosed, can omit lab test.
(2) Most commonly diagnosed in childhood
e. Anesthetic goal: avoid acidosis secondary to hypoventilation, maintain oxygenation, prevent circulatory stasis, maintain body temperature.
f. Treatment: minimize factors that cause sickling, including hypoxia, acidosis, hypothermia, hemoglobin concentration <8.5 g/dL, dehydration, pain, and infection.
g. Postoperative goal: maintain oxygenation, maintain intravascular fluid volume, maintain body temperature, use analgesics.
(1) Palliative care for painful crisis
(2) Simple and exchange transfusions
(3) Hydroxyurea to increase fetal hemoglobin
C. The anticoagulated patient
1. Definition: administration of oral anticoagulant to induce alterations in coagulation to prevent thrombus formation
2. Incidence: 600,000 cases of pulmonary embolism, with 10% resulting in death
3. Significance: used in patients with thromboembolism, hypercoagulable states, cancer, mechanical heart valves, and atrial fibrillation
4. Etiology: balance between risk of bleeding and thromboembolism, with risk increasing in major and emergency surgeries
5. Perianesthesia considerations
a. Increased risk of surgical bleeding
b. Heparin or low-molecular-weight heparins (LMWHs) used acutely for short-term action
(1) LMWHs have the same effect on factor X as heparin but less effect on thrombin.
(2) LMWHs are given subcutaneously or IV, and onset of action is rapid. Patients can administer LMWHs to themselves.
c. Oral anticoagulants ideally stopped 4 to 5 days before elective procedure
(1) May not be possible for patients with prosthetic valves
(2) INR should be 1.5 or less.
(3) Used for long-term therapy
d. Obtain PT day of surgery.
e. Consider bleeding time and platelet count.
f. Inquire about use of aspirin and NSAIDs in addition to Coumadin use.
g. Increased risk of cerebrovascular accident in patients with atrial fibrillation off Coumadin
IX. INFECTIOUS DISEASES
A. Human immunodeficiency virus (HIV) infection, AIDS
1. Definition: destruction of lymphocytes with decline in immune function
2. Incidence: 2006 Statistics show per 100,000 population; black male, ages 30-39 with highest incidence
3. Significance: increased risk of opportunistic infections in CNS, GI tract, lungs
4. Etiology: HIV spread via sexual activity, blood transfusions, IV drug use, fetal transmission, needlestick
5. Perianesthesia considerations
a. Meticulous attention to universal precautions
b. Chest x-ray to rule out interstitial pneumonitis
c. Must consider extent of organ system involvement when approving ambulatory status (pneumonia, dementia, cardiomyopathy, renal dysfunction)
d. Treatment: supportive, antiretroviral drugs either alone or in combination with other antiretrovirals, prophylaxis against opportunistic infections by administering pneumococcal vaccine, hepatitis B vaccine, influenza vaccine, isoniazid, trimethoprim-sulfamethoxazole
e. Asymptomatic patient who is HIV positive will respond in normal manner to anesthetic agents.
B. TB
1. Definition: bacterial pulmonary infection characterized by asymptomatic conversion of a TB skin test or presence of fever and nonproductive cough in an “at-risk” patient
2. Incidence: 100 in 100,000 population; greater in males than in females; increased risk with elderly in nursing homes, HIV-positive patients, homeless, prisoners, Asian and Latin American immigrants
3. Significance: can affect bones, joints, meninges, kidney, and skin
4. Etiology: Mycobacterium tuberculosis via droplet aerosol transmission (coughing and sneezing)
5. Perianesthesia considerations
a. Highest risk of disease within 8 to 12 weeks of exposure
b. Treatment: isoniazid, rifampin, and ethambutol in combination, varying with severity of disease
c. Rifampin colors urine, tears, and secretions orange.
d. Isoniazid can cause peripheral neuritis and hypersensitivity—can prevent with pyridoxine.
e. Compliance issues predominate with number of drugs and length of treatment.
f. Not infectious after 2 weeks of therapy and negative acid-fast bacilli culture
g. Chest x-ray will show infiltrate with or without effusion.
h. Homeless patients will have significant discharge limitations.
i. Patients with active TB require respiratory isolation.
j. Limit traffic, use disposable equipment, wear protective clothing, and remove nonessential equipment in surgical suite when patients done.
X. SUBSTANCE ABUSE
A. Illicit drug use
1. Definition: self-administration of drug(s) that deviate(s) from accepted medical or social use, which, if sustained, can lead to physical and psychological dependence
2. Incidence: varies with drug; includes alcohol, cocaine, opioids, barbiturates, benzodiazepines, amphetamines, marijuana, hallucinogens
3. Significance: physical withdrawal requires inpatient hospitalization—should not be attempted in perioperative period.
4. Etiology: biological, social, environmental, psychological factors
5. Perianesthesia considerations
a. Can manifest cross-tolerance to drugs, making it difficult to predict anesthetic and/or analgesic requirements; usually increased
b. May have concomitant problems of HIV, hepatitis, TB, malnutrition
c. Frequently has associated personality disorders
d. Patients acutely affected by substances not candidates for ambulatory surgery
e. Treatment: medical management of withdrawal, behavioral, and supportive counseling
XI. OBESITY (see Chapter 48)
A. Definition: weight >20% above ideal body weight
1. Morbidly obese: double normal body weight
B. Incidence: 20% to 30% of adult men, 30% to 40% of adult women; greater in females than in males; all ages
C. Significance: may have concomitant heart disease, diabetes, pulmonary insufficiency
D. Etiology: food intake greater than energy expenditure; genetic, endocrine, acquired disease
E. Perianesthesia considerations
1. Increased risk of aspiration; administer metoclopramide, H 2 antagonist.
2. Decreased use of positive pressure ventilation to preoxygenate to prevent distention and vomiting
3. Increased difficulty in intubation
4. May be chronically hypoxemic and hypercarbic; sleep apnea common
5. Increased duration of action of lipid-soluble drugs
6. Increased morbidity from cardiovascular disease
7. Increased risk of deep venous thrombosis—consider antiembolism precautions.
8. Increased risk of wound infection
9. Respiratory insufficiency, pneumonia, and thromboembolic phenomena avoided postoperatively by:
a. Minimal sedation
b. Appropriate pain control
c. Early ambulation
10. Treatment: medically supervised weight loss with nutritional counseling, increase exercise and activity; surgical: gastric stapling or bypass or intestinal bypass
BIBLIOGRAPHY
1. Atlee, J., Complications in anesthesia. ed 2 ( 2007)Saunders, Philadelphia.
2. Burden, N.; Quinn, D.; O’Brien, D.; et al., Ambulatory surgical nursing. ( 2000)Saunders, Philadelphia.
3. Cole, D.; Schlunt, M., Adult perioperative anesthesia: The requisites in anesthesiology. ( 2004)Mosby, Philadelphia.
4. Dennison, R., Pass CCRN. ed 3 ( 2007)Mosby, St Louis.
5. Drain, C.; Odom-Forren, J., Perianesthesia nursing: A critical care approach. ( 2009)Saunders, Philadelphia.
6. Faust, R., Anesthesiology review. ed 3 ( 2002)Churchill Livingstone, New York.
7. Fleisher, L., Evidence-based practice of anesthesiology. ( 2004)Saunders, Philadelphia.
8. Gutierrez, K.; Peterson, P., Saunders nursing survival guide: Pathophysiology. ed 2 ( 2007)Saunders, St Louis.
9. Moore, K.; Dalley, A., Clinically oriented anatomy. ed 5 ( 2006)Lippincott Williams & Wilkins, Philadelphia.
10. Morton, P.; Fontaine, D.; Hudak, C.; Gallo, B., Critical care nursing: A holistic approach. ed 8 ( 2005)Lippincott Williams & Wilkins, Philadelphia.
11. Nagelhout, J.; Zaglaniczny, K.L., Nurse anesthesia. ed 3 ( 2005)Saunders, Philadelphia.
12. Rathmell, J.; Neal, J.; Viscomi, C., Regional anesthesia: The requisites in anesthesiology. ( 2004)Saunders, Philadelphia.
13. Roisen, M.; Fleischer, L., Essence of anesthesia practice. ed 2 ( 2002)Saunders, Philadelphia.
14. Sladen, R.; Coursin, D.; Ketzler, J.; Playford, H., Anesthesia and co-existing disease. ( 2007)Cambridge University Press, Cambridge, N.Y.
15. Springhouse, Critical care nursing made incredibly easy. ( 2004)Lippincott Williams & Wilkins, Philadelphia.
16. Springhouse, Pathophysiology: A 2-in-1 reference for nurses. ( 2005)Lippincott Williams & Wilkins, Philadelphia.
17. Stoelting, R.; Dierdorf, S., Handbook for anesthesia and co-existing disease. ed 2 ( 2002)Churchill Livingstone, New York.
18. Stoelting, R.; Miller, R., Basics of anesthesia. ed 5 ( 2007)Churchill Livingstone, Philadelphia.