CHAPTER 16. History and Physical Examinations
Rose Ferrara-Love
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. State goals of preoperative history and physical exams.
2. Plan a subjective and objective patient exam.
3. Discuss the importance of completing a system review.
I. THE NURSING HISTORY AND PHYSICAL EXAMINATION
A. General health
1. Questions and observations regarding overall health include:
a. General appearance
b. Height
c. Weight
(1) Often converted to kilograms to facilitate rapid calculation of medication doses in milligram per kilogram (mg/kg) format
(a) Weight in pounds (divided by 2.2 equals weight in kilograms)
(b) Weight in kilograms (multiplied by 2.2 equals weight in pounds)
(2) Obesity
(a) Many freestanding surgical centers enforce weight restrictions because of increased risk of anesthesia complications.
(i) Usually 300 lb (136.4 kg)
(3) Recent unplanned weight loss
d. Recent or current infection
(1) Upper respiratory infections
(2) Lower respiratory infections
e Allergies
(1) Food
(2) Drugs
(3) Environment
f. Nutritional habits
g. Physical handicaps
(1) Use of adjuncts for walking
2. Family history
a. Problems with anesthesia
(1) Malignant hyperthermia (MH)
(a) Anesthetic-related deaths
(b) MH testing
(i) Caffeine-halothane contracture test
3. Physical examination includes observation.
a. Skin
(1) Color
(2) Turgor
(3) Elasticity
(4) Presence of bruises
(a) May necessitate report to authorities if abuse is suspected
(5) Other injuries
(6) Dryness
(7) Lesions
(a) Mucous membrane
(8) Cleanliness
(9) Dental hygiene
b Abnormalities
(1) Posture
(2) Gait
(3) Mobility
(a) Use of wheelchair, walker, or cane should be noted.
(4) Pain at rest
c. Physical characteristics
(1) Potential complications for intubation
(a) Short, stocky neck
(b) Cervical fusion or arthritis
(c) Thick tongue
(d) Temporal mandibular joint disease
(e) Dental or orthopedic abnormalities
d. Vital signs should be obtained to identify aberrancies and for baseline measurements.
(1) Blood pressure
(a) Dynamic measurements that change minute to minute
(i) Response to:
[a] Environment
[b] Physiologic demands
(b) Average ranges
(i) 100 to 135 mm Hg systolic
(ii) 60 to 80 mm Hg diastolic
(c) Orthostatic measurements with underlying cardiac or hypertensive history
(2) Pulse rate
(a) Average range 60 to 100 beats per minute
(3) Respirations
(a) Average rate
(i) 12 to 20 breaths per minute
(ii) 16 to 25 breaths per minute in elderly
(b) Use of accessory muscles of respiration
(c) Shape and symmetry
(d) Sternal abnormalities
(i) Pectus carinatum
[a] Chicken breast or pigeon breast
(ii) Pectus excavatum
[a] Breastbone caves in resulting in sunken chest appearance
(iii) Anterior-posterior diameter increased
[a] May be normal with:
[1] Age
[2] Hyperinflation
(e) Abnormal breathing patterns
(i) Küssmaul
(ii) Cheyne-Stokes
(iii) Biot’s
(4) Temperature (see Chapter 24)
(a) Oral temperatures are considered normal at 96.4° F (35° C).
(b) Rectal temperatures average slightly less than 1° F higher.
(c) Axillary temperatures are approximately 0.5° F to 1° F lower.
(d) Tympanic thermometer readings are approximately 0.5° F to 1° F higher than oral readings.
(e) Temporal thermometer readings are more accurate than tympanic thermometer readings.
(f) Variances in normal ranges
(i) Normal physiologic status
(g) Extrinsic forces
(i) Medication
(ii) Recent exercise
(iii) Effort
(iv) Anxiety
(v) Fear
B. Medication history
1. Medication protocol affects types of medications and anesthetic agents used.
a. Helps avoid untoward drug interactions or withdrawal episodes
2. Include in history form
a. Names
b. Dosages
c. Frequency
(1) Date and time of last dose
(a) Medication reconciliation upon admission and before discharge
d. Length of time prescribed
e. Effects
f. Nonprescription drugs
(1) Aspirin
(a) Prolongs bleeding time
g. Herbal preparations
h. Habit-forming drugs used
(1) Tobacco
(a) Number of pack years
(i) Number of packs per day × number of years
(ii) Attempts to stop
(b) Smokeless tobacco
(i) Amount per day
(2) Alcohol
(a) Type
(b) Amount
(c) Frequency
(d) Changes in reaction to alcohol intake
(3) Recreational
(4) Prescription
i. Side effects
j Allergic reactions
(1) Specific drug
(a) May know only category of drug (i.e., antibiotic)
(b) Identify if related categories will be used in the ambulatory surgery center (ASC).
(2) Specific reaction
(a) True allergy or expected side effect
(3) Usually documented in red
(a) Highly visible
(i) On medical record
(b) On patient identification band
(4) Environmental and food allergies
(a) Allergy to eggs may have possible cross-sensitivity with propofol.
(b) Allergy to bananas, kiwis, peaches, water chestnuts may have link with latex allergies.
(i) Cutaneous exposure (i.e., latex)
[a] Anesthesia masks, head straps, rebreathing masks, tourniquets, ECG patches, adhesive tape, surgical gloves
[b] Other sources: elastic bandages, rubber positioning rings, rubber shoes, elastic clothing, balloons, Koosh balls, sporting equipment
(ii) Mucous membrane
[a] Nasogastric tubes, balloons, nipples, pacifiers, products used in dentistry, urinary catheters, glove contact with vaginal mucosa, enema kits, rectal pressure catheters (especially in patients with spina bifida and impaired bowel control)
[b] Other sources: condoms
(iii) Inhalation
[a] Often associated with glove powder
(iv) Internal tissue
[a] Intraoperative resulting from surgical gloves contacting the peritoneum or internal organs
(v) Intravascular
[a] Disposable syringes, medication aspirated from vials with latex stoppers, injection of medication via ports of intravenous tubing (latex can leech into solutions injected)
C. Nutrition status
1. Weight history
a. Typical day’s diet
(1) Salt
(2) Saturated fats
(3) Food habits
(a) Ethnicity
(4) Dentition
2. Physiologic processes dependent upon proper nutrition
a. Wound healing
b. Oxygen transport
c. Enzyme synthesis
d. Clotting factors
e. Resistance to infection
3. Diseases associated with poor nutrition
a. Crohn’s disease
b. Malignancies
c. Chronic obstructive pulmonary disease
d. Ulcerative colitis
4. Indications of malnutrition
a. Anorexia
b. Recent weight loss
c. Dull hair
d. Brittle nails
e. Diagnostic tests
(1) Decreased lymphocytes
(2) Decreased serum albumin and transferrin levels
5. Obesity complicates:
a. Administration of anesthesia
(1) Requires higher-than-normal levels of anesthetic agents
(a) Fat-soluble agents tend to prolong effects.
(2) Increased stress on cardiovascular system
(a) Increased oxygen needs
(b) Increased carbon dioxide production
(i) Associated with increased body mass
b. Technical aspects of performing procedure
(1) Often difficult to intubate
(a) Difficult to maintain airway
(i) Increased risk of aspiration
(ii) Increased intra-abdominal pressures
(b) Gastric contents higher in volume and more acidic
(2) Problems with positioning
(a) Weight of abdominal and chest contents can cause respiratory embarrassment when in Trendelenburg position.
(3) Difficult to perform venipuncture
c. Patient’s recovery
(1) Electrolyte and fluid balance essential for homeostasis (see Table 16-1)
(a) Regulates cardiac rhythm
(b) Muscle strength
(c) Distribution and metabolism of drugs
(i) Mental alertness
| Electrolyte Normal Value | Physiologic Functions | Excess | Deficiency |
|---|---|---|---|
| Potassium (K) 3.5-5.5 mEq/L | —Nerve conduction —Muscle contraction —Enzyme action for cellular energy production —Regulates intercellular osmolality |
—Generalized muscle weakness, flaccidity; can affect respiratory muscles, paresthesia —Cardiac: bradycardia, ventricular ectopy and fibrillation, third degree heart block, asystole (>7.0 mEq/L) —ECG changes: flat or absent P wave, wide ORS, peaked T wave, prolonged PR interval |
—Muscle weakness, flaccidity, fatigue, leg cramps, ↓ deep tendon reflexes, shallow respirations, weak, thready pulse, hypotension —Cardiac: atrial dysrhythmias, premature ventricular contractions (PVCs), atrioventricular (AV) blocks, cardiac arrest (<2.5 mEq/L) —ECG changes: flat or inverted T wave, depressed ST segment, U wave present, potentiates digitals toxicity, premature atrial contractions (PACs) or PVCs —Abdominal cramping, anorexia, malaise, nausea and vomiting, muscle weakness, headache, confusion, lethargy, convulsions, coma |
| Sodium (Na) 135-145 mEq/L | —Transmission and conduction of nerve impulses —Regulates vascular osmolality —Regulates neuromuscular activity via sodium pump |
—Excitement; thirst; dry, sticky tongue and mucous membranes; oliguria; flushed skin; confusion; lethargy; coma; convulsions; hypo- or hypertension; elevated temperature | —Abdominal cramping, anorexia, malaise, nausea and vomiting, muscle weakness, headache, confusion, lethergy, convulsions, coma |
| Calcium (Ca) 8.5-10.5 mg/dl | —Nerve and muscle activity —Myocardial contractility —Maintains cell permeability —Converts prothrombin to thrombin —Formation of teeth and bones |
—Lethargy, depression, apathy, anorexia, nausea and vomiting, muscle weakness, headache, confusion, decreased attention span, slurred speech, hypertension —Cardiac: heart block, PVCs, idioventricular rhythms, cardiac arrest —ECG changes: shortened QT interval |
—Anxiety, excitement, hyperreflexia, grimacing, numbness and tingling of lips or fingers, muscle cramps and spasms, laryngospasm, convulsions, tetany, dysrhythmias including ventricular tachycardia (VT) —Positive Trousseau’s sign: carpal spasm after inflation of blood pressure cuff on upper arm to 20 mm Hg over systolic for 3 minutes, shows tetany —Positive Chvostek’s sign: abnormal facial spasm when facial nerve is tapped at the angle of the jaw —ECG changes: prolonged QT interval |
(2) Signs of dehydration
(a) Loss of skin turgor
(b) Listlessness
(c) Orthostatic hypotension
(d) Rapid and thready pulse
(e) Dryness of mucous membranes
(f) Thirst
(3) Cardiovascular
(a) Symptoms of cardiac disease
(i) Chest pain or tightness
(b) Palpitations
(c) Chronic fatigue
(d) Loss of appetite
(e) Angina
(f) Swelling of the ankles
(g) Paroxysmal nocturnal dyspnea
(h) Exhaustion
(4) Particular importance
(a) Recent cardiac surgery
(b) Myocardial infarction (MI)
(i) Considered most important indicator of anesthesia morbidity
(c) Generally elective, non-urgent surgery postponed for at least 6 months after an MI
(d) Angina
(e) Aortic stenosis
(f) Poorly controlled dysrhythmias
(g) Congestive heart failure (CHF)
(h) Extremes in blood pressure (high or low)
(i) Presence of pacemaker
(5) Physical examination parameters
(a) Apical pulse
(i) Rate
(b) Rhythm
(c) Quality
(d) At least one blood pressure reading
(e) Palpation of peripheral pulses
(f) Observation for edema
(g) Clubbing of fingers
(h) Cyanosis
(i) Distention of neck veins
(j) General energy level
(k) Respiratory ease
(l) Auscultation of heart for murmurs
(i) Systolic murmur over right sternal border, second intercostal space may indicate presence of aortic stenosis.
(ii) Associated with unexpected dysrhythmias
(m) Diminished stroke volume
6. Cardiac drugs
a. Maintain normal routine preoperatively.
(1) Do not skip doses.
(a) Beta-blockers
(b) Calcium channel blockers
(c) Antihypertensives
D. Peripheral vascular disease
1. Inspection
a. Skin color
b. Hair distribution
c. Edema
d. Varicosities
(1) Stasis ulcers
(2) Capillary refill time
2. Palpation
a. Peripheral pulses
(1) Characteristics
(a) Absent = 0
(b) Weak, thready = 1+
(c) Normal = 2+
(d) Full, bounding = 3+
b. Rigidity of vessels
(1) Palpable vibration (thrill)
3. Auscultation
a. Bruit
(1) Humming sound from narrow or bulging artery
4. Symptoms
a. Peripheral cyanosis
b. Pain
c. Cold
d. Intermittent claudication
e. Central vessel involvement
(1) Confusion
(2) Transient blindness
(3) Hemiparesis
5. Nursing interventions
a. Intraoperative passive range of motion
b. Use of padding of bony prominences intraoperatively
(1) Heels
(2) Elbows
(3) Shoulders
(4) Hips
(5) Coccyx
c. Encouragement of active exercises before and after surgery
d. Use of antiembolism stockings
e. Explanation of symptoms of thrombophlebitis
f. Encouragement of adequate fluid intake
g. Have patient immediately report any of the following symptoms postoperatively:
(1) Pain in the leg, especially increased calf pain when foot is dorsiflexed (positive Homans’ sign)
(2) Fever
(3) Chills
(4) Swelling
(5) Redness
(6) Heat
(7) Tenderness in leg
E. Respiratory (see Chapter 31)
1. History
a. Infectious or chemical influences
b. Smoking habits
c. Chronic cough
d. Previous lung surgery
e. Emphysema
(1) Patients may not admit to emphysema as a disease.
(2) Look for symptomatology.
(a) Dyspnea
(i) Minimal exertion
(b) Rest
(c) Chronic cough
(d) Barrel chest
(e) Elevation of shoulders
(f) Pursed lip breathing
(g) Cyanosis
(h) Clubbing of fingers
(i) Tachypnea
(j) Predisposition to respiratory infections
(3) Shortness of breath
(4) Current or past episodes of:
(a) Pneumonia
(b) Tuberculosis
(c) Bronchitis
(d) Asthma
2. Physical examination
a. Auscultation of the chest
(1) Crackles
(a) Typically short, explosive, discontinuous sounds
(b) May be heard in patients with:
(i) Pulmonary emphysema
(c) Bronchiti
(d) Asthma
(e) Pulmonary congestion
(i) Caused by CHF
(2) Rhonchi
(a) Coarser, rattling sounds with lower pitch
(i) Generally heard over large airways
(3) Wheezes
(a) Continuous, musical sound
(i) Asthma or emphysema
(b) Particularly expiration
b. Baseline breath sounds
(1) Comparison for postanesthetic findings
(a) Aspiration
(b) Fluid overload
(c) Bronchospasm
c. Baseline oximetry readings
(1) Observation of:
(a) Rate
(b) Depth
(c) Ease of breathing
d. Cyanosis
e. Symmetry of chest movements
f. Use of accessory muscles
g. Production of sputum
h. Upper airway including anatomic structures
(1) Short, stocky neck
(2) Excessive skin or fat on back of neck
(3) Thick tongue
(4) Previous cervical fusion
(5) Temporal mandibular joint disease
(6) Down syndrome
(a) Thick, protruding tongue
(b) Skin folds on posterior neck
(c) Instability of atlantalaxial joint in cervical spine
(i) Found in approximately 10% to 20% of persons with Down syndrome
(ii) Dislocation or subluxation of this joint can occur with hyperextension of neck.
(d) Cervical cord compression with nerve damage and possible death in 5% to 10% of those predisposed
F. Neurologic (see Chapter 33)
1. Assessment
a. General affect
(1) Behavior
(2) Speech patterns
(3) Orientation
(4) Gait
b. Fine motor movements
(1) Writing
(2) Cough
(3) Blink
(4) Swallow
(5) Pupil reflexes
c. Motor abilities
(1) Muscle strength
(2) Vision
(3) Hearing
d. Presence of:
(1) Headache
(2) Dizziness
(3) Paralysis
(4) Seizures
(5) Loss of motor control
e. Preexisting neurologic deficit
(1) More complete examination
(a) Cerebral
(b) Motor
(c) Cranial nerves (see Chapter 33)
(i) Table 16-2 describes abnormalities in function of the cranial nerves.
| *S, sensory; M, motor. |
||||
| From Quinn DMD: Ambulatory surgical nursing core curriculum, Philadelphia, 1999, WB Saunders. | ||||
| Name | Type* | Function | Test Abnormality | |
|---|---|---|---|---|
| I | Olfactory | S | Smell | Coffee, tobacco |
| II | Optic | S | Vision | Visual acuity, pupillary reaction, visual fields |
| III | Oculomotor | M | Eye movement | Ptosis; lateral and downward deviation of eye |
| IV | Trochlear | M | Eye movement | Medial and upper deviation of eye |
| V | Trigeminal (3 branches—opthalmic, maxillary, mandibular) | S | From skin of face and cornea | Loss of sensation on one side of face |
| M | Muscle movement | Temporal and masseter muscles movement loss | ||
| VI | Abducens | M | Eye movement | Medial deviation of eyeball |
| VII | Facial | S | Tastes—anterior tongue | Inability to grimace on one side of face |
| M | Muscles of facial expression | |||
| VIII | Acoustic auditory vestibulocochlear | S | Hearing | Watch ticking; whispered voice |
| S | Equilibrium | Vertigo; nystagmus | ||
| IX | Glossopharyngeal | S | Taste of posterior portion of tongue | Loss of gag reflex; deviation of uvula toward the unaffected side |
| M | Pharyngeal muscles | |||
| X | Vagus | S | From thoracic and abdominal organs | As with IX plus hoarseness |
| M | Pharyngeal and laryngeal muscles plus thoracic and abdominal organs | |||
| XI | Spinal accessory | M | Sternocleidomastoid and trapezius muscles | Inability to shrug one shoulder or to move chin to one side against pressure of examiner’s hand |
| XII | Hypoglossal | M | Tongue movement | Deviation of tongue to affected side |
(d) Reflex functions
G. Sensory and prosthetic
1. Patients may not provide accurate information about sensory deficits.
a. Embarrassment
b. Vanity
c. Assessment skills
(1) Hearing loss
(a) Patient may lean or turn toward conversation.
(b) Answer questions inappropriately or not at all
(c) Watch interviewer’s lips
(d) Provide interpreter in American Sign Language if patient is knowledgeable in use.
(i) Provide information and answers to questions that patient can understand.
(2) Visual impairment
(a) Difficulty seeing documents
(b) Should have instructions, consents, and other forms read to them before having them signed
2. Note that this occurred on patient record.
a. Emphasis is to ensure effective communication and understanding between patient and staff throughout surgical experience.
b. Patient must be able to understand instructions and explanations.
(1) May need sensory aids such as:
(a) Hearing aids
(b) Glasses or contact lenses
(c) Electronic voice stimulator
(d) Historically banned from operating room
(i) Current wellness-centered care approach brings more liberal policy.
(ii) As long as there is no threat to patient safety, potential for loss or harm to device, these devices are often allowed to remain with the patient.
(iii) Decision usually made by anesthesiologist
(e) Reassures patients that they may retain these devices and promotes psychological health
(f) May retain dentures, wigs, prosthetic limbs, and bras
(i) Essential for self-image and security
(ii) If they must be moved, reassure patients that they will be returned as soon as possible.
(iii) Personal privacy and dignity will be maintained.
(iv) Some ASCs are reevaluating the policy of removing dentures from all patients.
[a] Unless having general anesthesia, usually not necessary
c. Documentation of presence of:
(1) Loose or chipped teeth
(2) Permanent bridgework
(a) Avoid accidental injury during airway or tube insertion.
(b) Identify potential complications of airway management.
(c) Establish preexisting problems for legal reasons.
H. Musculoskeletal (see Chapter 42)
1. History
a. Arthritis
b. Scoliosis
c. Osteoporosis
d. Sciatica
e. Vertebral disc problems
f. Amputations
g. Prior fractures
h. Frequent falls
2. Physical assessment
a. Muscle strength
b. Gait
c. Mobility
d. Range of motion
e. Use of orthopedic appliances or prostheses
f. Need for assistive devices
(1) Walker
(2) Cane
(3) Wheelchair
I Integumentary
1. Assessment
a. Observation
(1) Color
(2) Temperature
(3) Texture
(4) Dryness
(5) Turgor
(6) Loss of elasticity
(a) Normal change in aging
(b) Can also indicate dehydration
(7) Integrity
(a) Easy bruising or petechiae
(i) Could indicate hematologic problems
(8) Jaundice
(a) Could indicate history of hepatitis
(9) Cyanosis or mottling
(a) May indicate serious vascular or cardiac disease
J. Communicable diseases
1. Scabies
2. Pediculosis (lice)
3. Impetigo
a. Presence of rash, especially in children
4. Tuberculosis
a. Making a comeback with advent of human immunodeficiency virus
b. Newer strains often drug resistant
5. History of:
a. Recent fever
b. Upper respiratory symptoms
c. Measles (rubeola)
d. German measles (rubella)
e. Chickenpox (varicella)
(1) Treatment before admission to ASC
(2) Isolation
(3) Other people, including patients in contact, could contract disease or infestation.
(4) Wound infection potential as result of self-contamination
K. Gastrointestinal (see Chapter 35)
1. History
a. Previous surgery
(1) Diversional surgery
(2) Colostomy
b. Gastrointestinal bleed
c. Cancer
d. Hiatal hernia
e. Chronic diarrhea or constipation
f. Presence of postoperative nausea and vomiting (PONV)
(1) If predisposition known, psychological and pharmacological interventions can be initiated to prevent occurrence.
(2) PONV unpleasant but potential for aspiration strong
g. Aspiration risk
h. Pyloric obstruction
i. Intestinal obstruction
j. Esophageal diverticula
k. Diminished pharyngeal reflexes
l. Obesity
m. Advanced pregnancy
n. Unknown compliance with nothing by mouth (NPO) requirements
2. Assessment
a. Mouth
b. Pharynx
c. Esophagus
d. Stomach
e. Large intestine
f. Small intestine
g. Pancreas
h. Liver
i. Gallbladder
L. Renal and hepatic (see Chapter 37)
1. Many anesthetic drugs are metabolized in the kidneys and liver.
2. History or presence of renal or hepatic disease is of great concern.
a. Pseudocholinesterase
(1). Enzyme necessary for metabolism of succinylcholine and ester-type local anesthetics
3. Kidney function
a. Excretion of urine
b. Influences fluid and electrolyte and acid–base balance
c. Nitrogenous wastes from protein metabolism are excreted.
d. Electrolytes are maintained.
(1) Sodium, potassium, chloride
(2) Excretion of some drugs also dependent on kidney function
4. Liver function
a. Metabolism of bilirubin
b. By-products of red blood cell breakdown
c. Protein synthesis
(1) Particularly albumin
(2) Patients with chronic liver disease have decreased serum protein levels.
d. Drug biotransformation
(1) Protein-bound drugs (thiopental and bupivacaine) have fewer sites to bind.
(2) Unbound portions remain active in bloodstream, creating prolonged or enhanced effects.
5. Physical assessment
a. Renal disease
(1) May not be evident until 50% or more function is lost
b. Liver disease
(1) Jaundice
(2) Spider angiomata
(3) Ecchymosis
(4) Ascites
(5) Pedal edema
(6) Scleral icterus
6. History
a. Cirrhosis
(1) Chronic alcohol or drug abuse
(2) Idiopathic
b. Hepatitis
c. Immune disorders
d. Extreme forms of dieting
e. Liver or kidney insufficiency or failure
f. Extremes in blood pressure
g. Anemia
h. Electrolyte imbalance
i. Depression
M. Endocrine (see Chapter 34)
1. Diverse diseases; can affect many processes necessary for tolerance of anesthesia and surgery
2. Hormones regulate:
a. Response to stress
b. Rate of metabolism
c. Blood pressure
d. Pulse rates
e. Blood glucose levels
f. Urine production
g. Electrolyte balance
h. Table 16-3 lists principal hormones and symptoms from imbalances.
| BMR, basal metabolic rate. | ||
| Hormone | Hyposecretion | Hypersecretion |
|---|---|---|
| Thyroid hormone | Children—cretinism | Hyperthyroidism, ↑ BMR, always hungry, irritable, tachycardia, weight loss |
| Adults—myxedema, ↓ BMR, tiredness, mentally slow, bradycardia | ||
| Parathyroid hormone | Spontaneous discharge of nerves, spasms, tetany, death | Weak, brittle bones; kidney stones |
| Insulin | Diabetes mellitus | Hypoglycemia |
| Adrenocortical hormones | Addison’s disease (body does not synthesize enough glucose, unable to deal with stress, sodium loss in urine may lead to shock) | Cushing’s disease (edema gives full moon face, fat around trunk, ↑ blood glucose levels, depressed immune response) |
3. Diabetes
a. Complications secondary to diabetic condition
(1) Delayed wound healing
(2) Retinopathy
(3) Kidney failure
(4) Peripheral artery disease
(5) Potential for:
(a) Ketoacidosis
(b) MI
(c) Severe hypoglycemia
b. Requires special instructions especially with regard to insulin and diet on day of surgery
(1) Often asked to bring own insulin to ASC
(2) May be asked to bring own food if ASC does not serve food or serves only donuts or sweet rolls for postoperative nourishment
N. Hematologic (see Chapter 29)
1. Disorders of the blood may involve:
a. Red blood cells
(1) Anemia
(2) Sickle cell anemia
(3) Thalassemia
(4) Polycythemia
b. Lymphocytes and plasma cells
(1) Agranulocytosis
(2) Leukemia
(3) Multiple myeloma
c. Lymph nodes and spleen
(1) Lymphoma
(2) Infectious mononucleosis
d. Platelets and clotting factors
(1) Hemorrhagic disorders
(2) Purpura
(3) Coagulation disorders
(a) Hemophilia
(b) Hypoprothrombinemia
2. Physical examination
a. Observation
(1) Petechiae and bruising
(2) Pallor and cyanosis
(a) Skin and mucous membranes
(3) Hepatomegaly
(4) Splenomegaly
3. History of:
a. Fatigue
b. Lassitude
c. Easy bruising
d. Frequent nosebleeds
e. Hematuria
f. Blood in stools
g. Excessive bleeding after minor injuries or dental extractions
4. Leukemia and acquired immunodeficiency syndrome
a. May be scheduled in ASC to avoid hospitalization and subsequent nosocomial infections
II. PSYCHOSOCIAL ASSESSMENT
A. Evaluation of emotional, cognitive, social, and cultural assessments occurs during physical assessment.
B. Emotional assessment
1. Most patients express a moderate to high degree of anxiety and fear facing surgery.
a. Patients have a right to feel anxiety.
(1) Placating or belittling the situation seen as demeaning to the patient
(2) Credibility of staff undermined by this approach
2. Anxiety and fear are similar but different.
a. Anxiety is described as a vague, unknown, or unidentified source evoked by a threat to one’s existence or personality.
b. Fear is related to a more specific person or occurrence.
(1) Some common fears related to surgery are:
(a) Possibility of not waking up after anesthesia
(b) Having a mask placed on the face
(c) Regaining consciousness during the surgery
(d) Making a fool of oneself
(e) Feeling the operation
(f) Anticipated postoperative pain
(g) Outcome of surgery
c. Ambulatory surgery would seem to provoke less fear and anxiety, but this is not the case.
(1) Home recuperation can add additional pressure.
(a) Fear of facing emergencies at home without medical attention
(b) Concern about family members who would have to care for them
(c) Inadequate pain medication
(d) Need to have another adult for transportation and home support
(i) Threat to independence
(e) Embarrassment at having to ask for help
(f) Problems of obtaining other person to provide support
(g) Pressure of arriving on time
(i) Many people do not sleep the night before for fear of not waking in time.
(h) May be primary caregiver for spouse
(i) Concern over their care while in surgery and during recuperation period
3. Preoperative interview important
a. Assess emotional state.
(1) Objective observations
(a) General appearance
(b) Nervousness
(c) Decreased attention span
(d) Lack of eye contact
(e) Increase heart rate
(f) Lack of self-confidence
(g) Decreased concentration
(h) Rapid speech patterns
(i) Diaphoresis
(j) Dry mouth
(k) Clammy skin
(l) Pressure of arriving on time
(m) Nausea
(n) Urinary frequency
(o) Hyperventilation
(p) Precordial chest pain
(2) Subjective information
(a) Patient
(b) Family
(3) Provide answers to questions.
(a) Information and support allow patient to gain understanding of upcoming surgery.
(b) Trust develops with surgical staff.
(c) By allowing patient to express feelings, staff can help patients to identify coping mechanisms to deal with rational and irrational fears.
(d) Anxiety can influence amount of teaching patients understand.
(i) Mildly anxious patients receive the most complete instructions.
(ii) Moderately anxious patients receive less information.
(iii) Give more attention to their specific areas of concern.
(iv) Severely anxious patients should receive only basic information.
(v) Need encouragement to verbalize fears
(e) Patients in state of panic are unable to learn.
(f) No instructions should be given.
(g) Physician should be notified of patient’s status.
(4) Cognitive assessment
(a) Evaluate patient’s understanding of procedure.
(b) Ask open-ended questions to elicit and encourage patient’s response in own words.
(c) Avoid yes and no answers.
(d) Evaluate before having patient sign consent.
(e) Patient and/or family must be sufficiently intelligent and responsible to provide care.
(f) Understand and comply with preoperative and postoperative instructions.
(g) Knowledge of hygiene
(h) Nutrition requirements
(i) Complying with NPO status
C Illiteracy
1. Written instructions of no use to person who cannot read or understand what is read
2. Estimated more than 23 million Americans are illiterate
a. Cannot read at the level most health care information is written (fifth-grade level)
(1) Many may be able to sign name without reading form.
(a) Clear verbal instructions particularly important
b. Language barrier
(1) English as a second language
(a) Need for interpreter to provide information
(i) Preferably not a family member
(ii) May be protecting patient by withholding information they feel patient should not know
D. Social assessment
1. Concept of ambulatory surgery is family based and home based.
a. Patients need strong support system.
b. Equally important are those persons responsible for aftercare.
2. Evaluation of home situation important during preoperative planning process
a. Elderly patients
(1) Surgical patient may be healthier of couple (spouse/companion).
(a) Often require outside help
(i) Neighbors
(b) Other family members
(c) Home health provider
(d) Physical environment of home
(i) Number of stairs
(e) Bathroom location
(f) May need to use social services to provide discharge planning
(g) Proximity of home to surgical center
E. Cultural assessment
1. Cultural and ethnic beliefs play role in patient’s attitudes about health care.
a. Difficult to separate beliefs from modern health care
b. May be considered superstitions by health care workers
(1) Spiritual control over body
(2) Faith healing
(3) Being one with the environment
c. Health care workers must respect patient’s cultural beliefs.
III. DIAGNOSTIC ASSESSMENT
A. 1970s and 1980s
1. Many ASCs cared for essentially healthy individuals.
a. Diagnostic practices were limited to few tests.
(1) Fingerstick hemoglobin and hematocrit screen
(2) Dipstick urinalysis
(a) Provided sufficient data to safely administer anesthesia
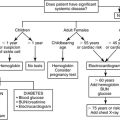
B. Today—sicker patients having surgery on an outpatient basis
1. Diagnostic requirements now include a variety of basic and complex testing.
a. Often same requirements as hospitalized counterparts
2. Preoperative testing is done to reduce risks associated with anesthesia and surgery.
a. Provides information about whether the patient can tolerate surgical procedures
C. Debate over amount and type of preoperative testing
1. Cost-effectiveness
a. Current trend toward ordering only those tests specifically indicated by abnormal clinical symptoms or history
2. Clinical thoroughness
a. Diagnostic testing is expensive.
(1) Benefit thought to outweigh expense
(a) Offers early detection of previously undiagnosed diseases
(b) Provides information regarding patient’s general health and ability to tolerate surgery
BIBLIOGRAPHY
1. Allen, G.C.; , North American Malignant Hyperthermia Registry of MHAUS, The sensitivity and specificity of the caffeine-halothane contracture test: a report from the North American Malignant Hyperthermia Registry, Anesthesiology 88 (3) ( 1998) 579–588.
2. Burden, N.; Quinn, D.M.D.; O’Brien, D.; et al., Ambulatory surgical nursing. ( 2000)WB Saunders, Philadelphia.
3. Delgan, J.H.; Vallerand, A.H., Davis’s drug guide for nurses. ed 20 ( 2009)Davis, Philadelphia.
4. Dennison, R.D., Pass CCRN. ed 3 ( 2007)Mosby, St Louis.
5. Drain, C.; Odom-Forren, J., Perianesthesia nursing: A critical care approach. ed 5 ( 2009)WB Saunders, Philadelphia.
6. Fagerlund, K.; Salwyc, E.; Temple, M., A national survey of certified registered nurse anesthetists knowledge, beliefs, and assessment of herbal supplements in the anesthesia setting, AANA J 73 (5) ( 2005) 368–377.
7. Fischback, F., Manual of laboratory and diagnostic tests. ed 8 ( 2008)Lippincott, Philadelphia.
8. Flanagan, K., Preoperative assessment: safety considerations for patients taking herbal products, J Perianesth Nurs 16 (1) ( 2001) 19–26.
9. Hooper, T., Mosby’s pharmacy technician: Principles and practice. ed 2 ( 2007)Saunders, Philadelphia.
10. Lewis, S.M.; Heitkemper, M.M.; Dirksen, S.R., Medical-surgical nursing: Assessment and management of clinical problems. ed 7 ( 2008)Mosby, St Louis.