CHAPTER 15. Preoperative Assessment
Kathleen P. Donohue and Susan M. Andrews
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. List three options available for conducting preoperative assessments and interviews.
2. Identify essential components of preadmission assessment.
3. Explain how the psychological and emotional assessment of a patient will help reduce anxiety on day of surgery.
4. Analyze the learning needs of ambulatory surgery patients.
I. TIMING OF PREOPERATIVE ASSESSMENT
A. Far enough in advance to ensure time for an appropriate evaluation
1. Obtain diagnostic testing and consultative services if needed.
2. Alter current medical regimen if necessary (e.g., anticoagulant therapy, glycemic control, hypertension).
3. Obtain equipment, supplies, and other items necessary for postoperative care.
4. Make arrangements in family schedule (home care, day care, transportation, etc.).
5. Prepare patient physically and emotionally for surgery.
B. Not too far in advance
1. Patient forgets preoperative instructions.
2. Diagnostic test results are outdated.
II. PURPOSE OF PREOPERATIVE ASSESSMENT AND PROGRAMS
A. Decrease potential delays and cancellations on day of surgery.
1. Provide for comprehensive assessments (nursing and anesthesia).
a. Potential problems identified and addressed before surgery
b. Nursing discharge plan
c. Complete systems review
d. Prior surgery, medical, and anesthesia history
e. American Society of Anesthesiologists (ASA) physical status identified
(1) ASA 1 or (P1): healthy patient
(2) ASA 2 or (P2): healthy patient with mild systemic disease
(a) Well-controlled chronic bronchitis
(b) Moderate obesity
(c) Diet-controlled diabetes mellitus
(d) Mild hypertension
(e) Old myocardial infarction (MI)
(3) ASA 3 or (P3): patients with severe systemic disease that limits activity but is not incapacitating
(a) Coronary artery disease with angina
(b) Type I diabetes mellitus
(c) Morbid obesity
(d) Moderate to severe pulmonary insufficiency
(4) ASA 4 or (P4): patients with severe systemic disease that is a constant threat to life
(a) Organic heart disease with marked cardiac insufficiency
(b) Persisting angina
(c) Intractable dysrhythmia
(d) Advanced pulmonary, renal, hepatic, or endocrine insufficiency
(5) ASA 5 or (P5): moribund patients who are not expected to survive without surgery
(a) Ruptured abdominal aortic aneurysm
(b) Major multi-system or cerebral trauma
(6) ASA 6 or (P6): patients declared brain dead whose organs are being harvested
(7) E: the E suffix denotes an emergency surgical procedure.
(8) Ambulatory surgery patients usually fall into the first three categories.
2. Provide for perioperative and perianesthesia teachings.
a. Physician and anesthesia providers are the chief source of information.
b. Preoperative nurse is the primary educator and teacher of the provided information.
c. Encourage patient and family to openly and honestly communicate their:
(1) Needs
(2) Emotions
(3) Concerns
d. Promote patient safety.
(1) Clear understanding of preoperative instructions
3. Provide patient and family opportunity for questions.
a. Clarify patient’s understanding of:
(1) Procedure
(2) Informed consent
(3) Anesthetic approach
(4) Goals/expected outcomes
(5) Personal responsibilities
(6) Comprehensive instructions
(a) Assist with understanding and compliance.
(b) Allow for preparation for transport and postoperative home needs.
(i) Caregiver
(ii) Practice techniques (e.g., emptying drains, dressing changes, crutch walking, injections, etc.)
(c) Physician follow-up care
4. Reduce patient anxiety.
a. Provide clear and concise explanations.
b. Inaccuracies or misinformation may cause fear.
(1) Induction of anesthesia smoother in calm persons
(2) Recovery enhanced when patient less stressed
c. Promote the wellness concept.
III. BENEFITS OF A PREOPERATIVE ASSESSMENT PROGRAM
A. Identify issues needing further work-up before admission to avoid costly delays and cancellations.
1. History and physical
a. Performed within 30 days of the scheduled surgery
b. Completed
c. Updated within 24 hours of surgery
2. Advance directive
a. Need to bring a copy on the day of surgery
b. Opportunity to convey patient’s decision about end of life care, if so desires
3. Identify needed laboratory, diagnostic testing, and/or additional work-ups.
4. Identify any postoperative care needs.
a. Supplies, prescriptions, medication teaching and demonstration (e.g., enoxaparin sodium [Lovenox])
b. Equipment for home use (crutches, walker, continuous passive motion, continuous positive airway pressure, etc.)
c. Arrange for home care services (visiting nurse, home care aide, etc.).
d. Transportation home if outpatient surgery
(1) Avoid unnecessary postoperative stays.
(2) Potential unsafe transportation plans
e. Responsible adult (18 years or older), especially for first 24 hours
B. Allows for preoperative diagnostic screening
1. Based on specific individualized clinical indicators or risk factors (Figure 15-1)
a. Age
b. Preexisting disease or illness
c. Surgical procedure being performed
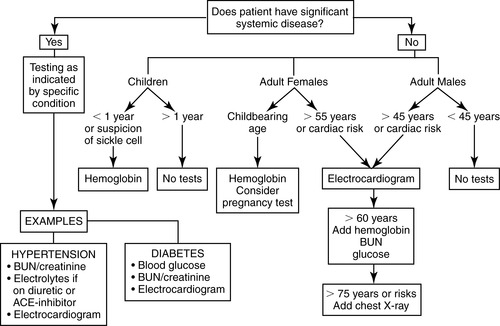 |
| FIGURE 15-1 ▪
Preadmission testing algorithm.
|
C. Allows for identification of potential safety issues
1. Patient and family history
a. Malignant hyperthermia
b. Pseudocholinesterase deficiency
c. Allergies including latex allergy/sensitivity
(1) Notify operating room (OR) before of day of surgery.
d. Use of narcotics for chronic pain
e. Use of street drugs/herbals
f. History of postoperative/postdischarge nausea and vomiting (PONV/PDNV)
2. Mobility issues
3. Ability to care for self if lives alone
4. Quality and amount of caregiver assistance
5. Ability and willingness to comply with preoperative instructions
a. Fasting and nothing by mouth (NPO) requirements
b. Smoking cessation
c. Necessary preoperative preparations
D. Allows for medication review and education
1. Current medications reviewed
a. Medication reconciliation starts preoperatively.
b. Name, dose, frequency
c. Herbals, supplements and over-the-counter medications
(1) Ask about specific supplements used. Patients often do not consider these “medications.”
2. Preoperative medication instructions
a. Some medications may be stopped before surgery as determined by surgeon and/or anesthesia provider.
(1) Anticoagulant therapy and nonsteroidal anti-inflammatory drugs, aspirin
(a) How handled may be procedure or physician specific
(2) Aspirin can affect platelet adhesiveness for up to 7 days.
(3) Coumadin often discontinued 48 hours before surgery.
(a) Clotting studies done immediately before surgery
(b) Closely monitor patients receiving long-term therapy for signs of bleeding.
(4) Dipyridamole (Persantine) usually stopped 2 days before surgery
(5) Indomethacin, tricyclic antidepressants, phenothiazines, furosemide, and steroids can interfere with platelet function.
(6) Herbals and supplements
(a) Feverfew, garlic, ginger, ginkgo, ginseng, and vitamin E may increase bleeding, particularly in patients already taking anticoagulants.
(b) Ginseng may cause an increase in heart rate and blood pressure.
(c) Licorice, some mixture types may increase blood pressure.
(d) Goldenseal and vitamin E may exacerbate high blood pressure in people who already have hypertension.
3. Some medications may be held the day of surgery as determined by surgeon and/or anesthesia provider.
a. Diuretics, insulin, oral hypoglycemic medications, etc.
b. Monoamine oxidase inhibitor (MAOI) antidepressants
(1) Usually discontinued before anesthesia
(2) Interaction with anesthetic drugs can result in a release of epinephrine and dopamine.
4. Medications that may be taken the day of surgery as determined by surgeon and/or anesthesia provider
a. Cardiac, antihypertensive (may be held if contain diuretics)
b. Beta-blockers
c. Calcium channel blockers
d. Anticonvulsants
e. Chronic pain medications
E. Provide preoperative teaching.
1. Procedure-specific instructions in nonmedical jargon
a. Provide information in easy-to-understand language at the level of the patient’s understanding.
b. Reinforce verbal instructions with written handouts whenever possible.
c. Video aids for patients to take home are an excellent teaching reinforcement tool.
2. Need for compliance with preoperative instructions
a. Arrival time
b. Leave valuables at home.
c. Bring needed documents (medication list, advance directive, any paperwork from surgeon, picture identification, etc.).
d. Need for responsible adult, at least first 24 hours postoperative
e. Transportation
f. Diet, NPO, and smoking restrictions
(1) No gum or hard candy
(a) Increases stomach acid secretions
(2) Small amounts of clear liquids morning of surgery can reduce stomach acid secretions.
(3) Refrain from smoking for at least 8 hours or per facility policy.
(a) Reduces amount of carbon monoxide in blood
(b) Promotes better oxygenation during anesthesia
(c) Reduces upper airway irritation
(d) Reduces bronchospastic tendency
(e) Reduces gastric volumes
3. What type of clothing to wear
a. Front button-down shirt for eye cases, skirt or loose fitting pants for leg surgery, etc.
b. Refrain from wearing makeup, nail polish.
4. Need for surgical preoperative preparations (e.g., bowel prep, antiseptic shower, no shaving of operative site, etc.)
5. Review of preoperative and postoperative expectations
6. Importance of caregiver support
7. Postoperative pain management
F. Patient/family satisfaction
1. Convenient for patient
2. Informative
3. Allows patient and family to ask questions and express concerns
IV. TYPES OF PREOPERATIVE ASSESSMENTS AND PROGRAMS
A. Hospital or freestanding ambulatory surgery center in-person interview
1. Advantages
a. Formal program
b. May have nursing, anesthesia, other health care team and diagnostic testing at same time and place
c. Decreases delays and cancellations day of surgery
(1) Able to take corrective actions on recognized complications or problems
d. Allows patient and families the opportunity to see facility, meet staff, ask questions
e. Allows interviewer to assess patient’s level of understanding, apprehension, etc.
f. Able to identify potential issues (e.g., language, other communication barriers, physical disabilities that may affect preparation time day of surgery)
2. Disadvantages
a. Some patients precluded
(1) Time constraints
(2) Transportation issues
(3) Travel distance
(4) Physical limitations
(5) Emergent or add-on cases
b. Cost
(1) Staff
(2) Physical space
B. Surgeon or primary care provider (PCP) office in-person interview
1. Advantages
a. Saves patient’s time
b. Decreases need to repeat information
(1) Preoperative interview done at time of history and physical, consent.
c. Allows patient to ask surgeon questions directly at time of preoperative work-up
d. PCP may perform clearance for comorbidities at the same time as preoperative work-up.
e. Diagnostic testing may be completed during visit.
f. Consultations performed, if needed
2. Disadvantages
a. No opportunity for patient and family to visit surgical facility
b. Preoperative staff does not meet patient before the day of surgery.
C. Phone interview
1. Advantages
a. May be screening tool to identify high-risk patients
b. Potential to be done at patient’s convenience
c. Saves any patient inconvenience of an in-person visit
d. Patient able to ask questions
2. Disadvantages
a. Potential of required testing not being completed
b. May have difficulty in contacting patients at a convenient time and location where they can speak freely
c. May be difficult to assess patient’s level of understanding
d. Unable to perform a physical assessment
e. Anesthesia interview may not be performed until immediately before surgery.
f. Patient may not be a proper candidate for a phone interview.
D. Web-based assessment and teaching programs
1. Facility based
a. Specifically designed by facility
(1) Forms and format
b. May include virtual preoperative tour
2. Independent web based
a. Purchased service
3. Process
a. Patient accesses a designated secure website to complete a medical history.
b. RN reviews questionnaire for completeness and need to follow-up with patient.
c. Program may offer preoperative teaching module.
4. Advantage (Box 15-1)
a. Patient convenience
(1) Completes information at own time and pace
(2) No travel or lost work time
BOX 15-1
ADVANTAGES OF COMPUTER-BASED PREOPERATIVE EDUCATION
▪ Consistency: Quality and content is standardized.
▪ Individualized instruction: Patients proceed at their own paces and can repeat and review information.
▪ Privacy: Only the patients see incorrect answers, avoiding embarrassment over incorrect or personal answers.
▪ Time efficiency: It reduces professional time spent presenting information common to most patients.
▪ Accessibility: It can be used at any time, for inpatients as well as outpatients.
From Burden N, Quinn DMD, O’Brien D, et al: Ambulatory surgical nursing, Philadelphia, 2000, WB Saunders, p. 349.
5. Disadvantages
a. Decreased opportunity to build rapport with patient
(1) No one available to answer questions or provide explanations
b. Possible lack of Internet access
c. Potential anxiety over privacy issues
d. Potential for actual breech of privacy
e. Web instructions unfriendly to user
E. Questionnaires
1. Advantages
a. Patient completes an abbreviated history.
(1) RN reviews to determine whether an in-person interview and/or diagnostic testing is warranted.
(2) Healthy patients are contacted by phone to review preoperative instructions.
2. Disadvantages
a. Same disadvantages as with phone interview
F. Preoperative group sessions
1. Advantages
a. May be general or pertinent to specific patient populations
b. May include various team departments
(1) Admissions
(2) OR
(3) Perianesthesia care units
(4) Anesthesia
(5) Social services
(6) Case manager
(7) Financial counselor
(8) Rehabilitation
(9) Visiting nurse services
c. Patients may benefit from talking with patients who are having same procedure and/or who have undergone same procedure (major surgeries).
d. Allows nurse to instruct multiple patients at one time
e. Use of return demonstration of any postoperative equipments (e.g., pain management pumps)
f. Helpful to review clinical pathway and expectations for the specific surgical procedure
g. Patient and family have opportunity to ask questions and express concerns.
2. Disadvantages
a. Patient may be unable to attend.
b. Length of time for group session
c. Patient may feel uncomfortable asking questions in group setting.
d. Attention to and time spent with individual patients may be limited.
G. Preoperative tours for pediatric population
1. Benefits of program
a. Provides information to patient and family
b. Allows for education to be personalized as needed
c. Decreases anxiety by reviewing perioperative process and answering questions
d. Allows child to see and become familiar with the area before the day of surgery
e. Opportunity for child to practice “leaving parents” to go into procedure room and then reunite
(1) Builds trust
(2) Many children’s hospitals allow parents to accompany child in the OR until after induction is completed.
2. Types of programs
a. May be group or individual
b. Tour includes hands-on familiarization with common equipment.
(1) Blood pressure cuff
(2) Thermometer
(3) Face mask (able to select “flavor” of mask)
(4) Casting materials, slings, crutches, etc.
c. Theme tours through perioperative areas (safari, circus, etc.)
d. “Dress-up” programs
e. Role playing
f. Procedure specific (e.g., cardiac, urological, orthopedic, etc.)
H. Preoperative tours for adult population
1. Benefits of program
a. Useful for patients undergoing major surgery
b. May be individual or as a group
c. Review of preoperative and postoperative expectations
d. Allows for patient and family to ask questions
e. Allows patient and family to see where family will wait
I. Additional alternatives
1. Preoperative videos
a. Can be generalized or surgery specific
b. Can focus on specific population (pediatric or adult)
c. Allows viewing at own home in familiar surroundings
d. Can be reviewed numerous times until patient is comfortable with content
2. Educational pamphlets and brochures
a. Distribute to patient at time of preoperative assessment.
b. Can be brief or detailed
c. Provide pictures for ease of understanding.
V. IMPORTANCE OF PREOPERATIVE ASSESSMENT
A. Goals
1. Provide patient and family with necessary information for a positive surgical experience; may be verbal and/or written.
2. Assess patient’s understanding of and potential compliance with instructions.
3. Obtain vital information to avoid delays or cancellations on day of surgery.
4. Provide for a smoother, more efficient patient flow on day of surgery.
B. Does not matter which method is used as long as end result of a patient ready for surgery is achieved
1. Different approaches may meet varied patient and family needs.
VI. SCHEDULING SURGERY
A. Based on:
1. Surgeon’s availability
2. Slots available in OR schedule
3. Patient’s needs
a. Emotional and physical
(1) May not want a prolonged delay for someone extremely anxious
(2) Children and diabetic patients need to maintain nutrition and medication schedules.
(3) Procedures requiring prolonged postoperative observation should be done early in the day.
b. Urgency of surgical procedure
c. Third-party reimbursement
d. Patient’s and family’s schedule
e. Completeness of the preoperative process before the day of surgery
(1) If incomplete should not be scheduled as a first case
(a) Need for completion of work-up day of surgery may delay OR start time.
VII. PATIENT TYPES
A. Morning ( am) admissions, outpatient observation patients (short stays: 23:59) extended recovery, and day surgery patients
1. Cost savings for institution
2. Diagnostic testing and preoperative assessment done as outpatient
3. am admissions and outpatient observation patients
a. Admitted to hospital either before or after surgery
b. Transferred from PACU to an inpatient, extended recovery, or observation room
4. Day surgery patients
a. Discharged day of surgery
VIII. DAY OF SURGERY GENERAL PREPARATION
A. Expedite processes to avoid OR delays or cancellations.
B. Nursing process
1. Follow regulatory guidelines (see Chapter 7).
2. Complete patient’s assessment, obtain actual height and weight.
3. Assess patient for changes since preoperative evaluation interview.
a. Some changes may result in case being cancelled.
(1) Abnormal vital signs including pulse oximetry
(2) Upper respiratory infections (cough, congestion, fever)
(3) Skin disruptions, bruises
(a) Especially on or near surgical site
b. Assess for risk of PONV/PDNV.
4. Emotional support
a. Atmosphere
(1) Ensure privacy.
(2) Calm and unhurried demeanor
(3) Soft music
(4) Subdued lighting, warm colors, painting on the walls
b. Familiarize patient and family with area.
(1) Patient’s room
(2) Waiting area
(3) Where family can go for food and drinks
(4) Approximate length of procedure
(5) How often and how family will be updated on patient’s status
(6) Liaison person/nurse, if available
(7) PACU visitation policy
5. Assess patient for compliance with preoperative instructions.
a. Notify surgeon and/or anesthesia care provider of any noncompliance issues.
(1) NPO status
(2) Smoking status
(3) Current patient’s medical condition (e.g., fever)
(4) Medications taken and/or held
(5) Availability of home caregiver
(6) Transportation if outpatient
6. Nursing has role of primary educator.
a. Clarify patient’s understanding of:
(1) Procedure
(2) Anesthetic approach
(3) Goals/expected outcomes
(4) Personal responsibilities
7. Preparation for the OR
a. Hospital gowns required for most procedures
(1) Some institutions make exceptions for minor surgery (e.g., eye, breast biopsies, hand surgery can keep on undergarments or pants).
(2) Some allow patients to wear undergarments.
(a) No nylon due to static electricity
b. Dentures, partials, eyeglasses, hearing aides
(1) Some institutions allow these items to go with patient to OR holding area.
c. Jewelry
(1) Instruct to remove all jewelry.
(a) Be aware body piercings can be on any body part.
(i) May cause arcing—electrosurgical burns
d. Securing of clothes and personal items
(1) Give any valuables to family to keep.
(2) Some institutions have lockers for clothing.
(3) Others give to family or stay on the patient’s bed.
e. Surgical Care Improvement Project (SCIP) recommend whenever possible hair should be left at the surgical site.
(1) There is a relationship between shaving and increased wound infections.
(2) If hair removal is necessary, remove with clippers or depilatories.
(a) Electrical or battery powered
(b) Disposable or disinfect between patients
(c) Perform outside the OR (e.g., preoperative area).
f. IV access
(1) Policies vary from facility to facility.
(2) May be responsibility of preoperative admitting nurse, anesthesia provider, intravenous team, etc.
(3) Needle gauge dependent on patient need
(a) Outpatients usually 20 gauge
(b) Patients with small, fragile veins may require a smaller gauge.
(c) am admit patients who may require blood transfusion, an 18 gauge may be recommended.
g. Preoperative medications
(1) May be used to reduce anxiety
(2) May be used to reduce risk for nausea, vomiting, and gastric acidity
(3) Standards for antibiotic prophylaxis
(a) SCIP recommendations
(i) Within 60 minutes of incision
(ii) Selection according to surgical procedure
(iii) Time challenge due to changes in surgery schedule
(iv) Some must be given over 1 to 2 hours.
(v) Discontinuation within 24 hours
(vi) Collaborative effort between nursing and anesthesia
(4) Prophylaxis for preventing subacute bacterial endocarditis
(a) Generally give before dental, gastrointestinal, genitourinary, oral, and respiratory procedures.
(5) SCIP recommendations for beta-blockers
(6) SCIP recommendations for glucose control
C. Documentation
1. Essential that initial assessment be complete and accurate
a. Some ambulatory surgery centers use abbreviated assessments (focused assessments).
2. Update information with specific day-of-surgery assessment.
a. Specific and unusual findings, actions taken, disposition of patient’s belongings, family contact information, IV information including missed attempts, vital signs including pulse oximetry, height, weight, etc.
3. Essential that history and physical be complete and updated within 24 hours of surgical procedure
4. Essential that surgery consent be complete, accurate, dated, and signed by all individuals
a. Legal responsibility of surgeon and anesthesia providers (if separate anesthesia consent)
(1) Accurately identifies procedure being performed
(2) Include explanation of procedure, risks, benefits, outcomes, potential complications, and options to proposed surgery/anesthesia.
(3) Words and names should be spelled correctly.
(4) Avoid abbreviations.
(5) No blank areas
(6) No erasures, white outs, or obliterations
(7) Language that patient understands
(8) Changes or additions should be written clearly.
(9) Person making change should initial and date changed area(s).
(10) Patient should also initial and date changed area(s).
(a) Significant changes are best done with new consent form.
b. Role of the nurse in obtaining consents
(1) Actual consent for surgery occurs when the surgeon and patient agree to proceed.
(2) Explanation of the procedure, including risks, benefits, outcomes, and potential complications, is the surgeon’s responsibility.
(3) Some institutions require that the nurse facilitates the process of obtaining the patient’s consent on the form as well as witnessing the patient’s signature.
(4) According to the American Nurses Association, the nurse has a moral and ethical obligation to ensure that:
(a) Patients do not feel pressured or forced into treatment.
(b) Patients receive accurate information that is understood by them.
(c) Patients understand that the consent can be withdrawn at any time.
(d) Patients understand what is being done.
(i) If patient understands, the nurse may obtain signature on consent form and witness that signature.
(ii) If patient does not indicate understanding or is unsure about other aspects of surgery or anesthesia, notify the surgeon or anesthesia provider before obtaining signature.
(iii) Document incident and subsequent conversation in patient’s record.
c. Special consents
(1) Anesthesia consents should be obtained by the anesthesia provider.
(2) Additional consents may be required for:
(a) Sterilization procedures
(b) Termination of pregnancy
(c) Implantation of investigational devices
(d) Photographing procedure
(e) Laparoscopic procedures
(f) Release of information to another physician and/or facility
(g) Study patients
d. More institutions using computerized charting
(1) Provides for more continuity
(2) Information easier to share between providers
D. Handoff to anesthesia, holding or operating room
1. The Joint Commission (TJC) National Patient Safety Goals (NPSG)
a. Communication between caregivers
b. Method determined by facility
(1) Face to face
(2) Phone
(3) Written report
(4) Combination of above
c. Process includes opportunity to ask questions.
2. Seen by anesthesia provider before surgery
a. May be done in preoperative department or preoperative holding
(1) Regional anesthesia (nurse’s role)
(a) Provide emotional support.
(b) Position so patient can see nurse.
(c) Maintain eye contact.
(d) Hold hand for physical contact or support as needed.
(e) Supportive conversation
(2) Monitored anesthesia care
(3) Local anesthesia
(4) General anesthesia
3. Prevention of hypothermia
a. SCIP recommendations
b. Starts in preoperative area
c. Start with normothermia.
d. Use warming techniques.
(1) Warmed blankets
(2) Warmed IV fluids
(3) Increased ambient room temperature
(4) Socks, head coverings
(5) Limited skin exposure
IX. REGULATORY
A. The Joint Commission
1. NPSGs
a. Change yearly
(1) Goals that directly impact preoperative phase
(a) Patient identification
(b) Correct site surgery
(c) Medication reconciliation
(d) Communications, handoffs
(e) Infections
(f) Surgical fires
(g) Medication safety
(h) Patient involvement in their care
(i) Falls
(2) Some goals dropped off the list and others added each year
2. Core measures
a. SCIP
(1) Antibiotic timing
(a) Within 1 hour of surgical incision
(b) Discontinue within 24 hours after surgery end time; 48 hours for cardiac procedures.
(2) Cardiac patients with controlled 6 am postoperative serum glucose
(3) Appropriate hair removal
(a) Clipping or depilatory
(b) No shaving
(4) Normothermia for immediate postoperative colorectal patients
(5) Beta-blocker therapy
(6) Venous thromboembolism
B. Patient Self-Determination Act
1. An amendment to the Omnibus Budget Reconciliation Act of 1990
a. Medicare and Medicaid providers such as hospitals must provide adult patients written information about their rights under state law.
(1) To participate in and direct their health care choices
(2) To agree to or refuse medical or surgical treatment
(3) To prepare an advance directive
(a) Living will
(b) Durable power of attorney
(c) Right to direct end-of-life decisions
b. Providers must supply information on their policies that govern the utilization of these rights.
c. Currently freestanding surgical centers are not required to participate.
(1) Some are supplying this information.
C. Health Insurance Portability and Accountability Act
1. Took effect April 2003
2. Involves three separate sets of rules to protect patients’ health information
a. Transactions
b. Security
c. Privacy
D. National Standards on Culturally and Linguistically Appropriate Services
1. Culturally competent
2. Access services
a. Currently mandated federal requirements for all recipients of federal funds
(1) Standard 4: health care organizations must offer and provide language assistance services, including bilingual staff and interpreter services, at no cost to each patient/consumer with limited English proficiency at all points of contact, in a timely manner during all hours of operation.
(2) Standard 5: health care organizations must provide to patients/consumers in their preferred language both verbal offers and written notices informing them of their right to receive language assistance services.
(3) Standard 6: health care organizations must assure the competence of language assistance provided to limited English-proficient patients/consumers by interpreters and bilingual staff.
(4) Standard 7: health care organizations must make available easily understood patient-related materials and post signage in the languages of the commonly encountered groups and/or groups represented in the service area.
3. Organizational supports for cultural competence
BIBLIOGRAPHY
1. American Society of Anesthesiologists, ASA physical status classification system. ( February 11, 2008) ; Available at:www.asahq.org/clinical/physicalstatus.htm; Accessed.
2. American Society of Anesthesiologists, What you should know about your patients’ use of herbal medicine and other dietary supplements. ( February 11, 2008) ; Available at:www.asahq.org/patientEducation/herbPhysician.pdf; Accessed.
3. American Society of PeriAnesthesia Nurses, Standards of perianesthesia nursing practice 2008-2010. ( 2009)American Society of PeriAnesthesia Nurses, Cherry Hill, NJ.
4. Ascension Health, Patient self-determination act (PSDA). ( February 17, 2008) ; Available at:www.Ascensionhealth.org/ethics/public/issues/patient_self; Accessed.
5. Association of Operating Room Nurses, AORN standards: Recommended practice and guidelines. ( 2007)Association of Operating Room Nurses, Denver, CO.
6. Burden, N.; Quinn, D.M.D.; O’Brien, D.; et al., Ambulatory surgical nursing. ed 2 ( 2000)WB Saunders, Philadelphia.
7. Michigan Health and Hospital Association Service Corporation Core Options, The Joint Commission/core measures. ( February 17, 2008) ; Available at:www.coreoptions.com/new_site/jcahocore.html; Accessed.
8. Ireland, D., Redi-Ref 2004 ambulatory/PACU/pediatrics. ( 2004)American Society of PeriAnesthesia Nurses, Cherry Hill, NJ.
9. Oshodi, T., Clinical skills: an evidence based approach to preoperative fasting, Br J Nurs 13 (2004) 958–962.
10. Spaulding, N.J., Reducing anxiety by preoperative education: make the future familiar, Occup Ther Int 10 (4) ( 2003) 278–293.
11. The Joint Commission, National patient safety goals. ( February 6, 2008) ; Available at:www.jointcommission.Org/PatientSafety/NationalPatientSafetyGoals/08; Accessed.
12. U.S. Department of Health and Human Services, OPHS Office of Minority Health, National standards for culturally and linguistically appropriate services in health care. ( February 11, 2008) ; Available at:www.Omhrc.gov/assets/pdf/checked/Executive.pdf; Accessed.





