CHAPTER 14. The Geriatric Patient
Jennifer Allen*
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Identify changes that occur with aging using a systems approach.
2. Describe the demographics of the geriatric patient.
3. Identify potential problems that may occur after a surgical procedure.
4. Discuss the purpose of a preoperative assessment.
5. Identify postoperative priorities in consideration of the physiologic changes that occur with aging.
I. OVERVIEW
A. Geriatric patients present a unique challenge.
B. Physiological changes and pathological conditions mandate utilization of the nursing process.
II. DEFINITION OF GERIATRIC OR OLDER ADULT
A. Age 65 years or older and when one qualifies for retirement income
1. 65 to 74 years: “young-old”
2. 75 to 84 years: “old”
3. 85 years: “old-old”
B. Life expectancy
1. Men: 81 years
2. Women: 84 years
C. Number of older adults in United States is increasing.
1. By 2030, the older population will double to about 72 million people.
a. One in five will be 65 or older.
b. The age group 85 years and older is the fastest growing cohort of the United States population.
c. The 85 and older population is projected to increase from 4.7 million in 2003 to 9.6 million in 2030.
2. Members of minority groups are projected to represent 26.4% of the older population in 2030.
3. More than 2 million Americans celebrated their sixty-fifth birthday in 2003 (5574 per day).
4. Older adults account for one third of all health care costs.
a. Focus is shifting to health promotion and health maintenance.
b. Nurses need to be aware of what health promotion and maintenance practices will benefit the older adult.
c. Recommended health practices
(1) Diet
(2) Exercise
(3) Tobacco cessatation and alcohol reduction
(4) Physical examinations and preventive care
(5) Dental examinations and preventive care
5. There were 50,639 persons aged 100 or more in 2003 (0.17% of total population).
6. Number of centenarians is expected to grow quickly, with estimates of 381,000 by 2030.
D. The Silent Generation, also known as the Veteran Generation (people born before 1946)
1. Comprise 10% of today’s work force
2. Rely on tried and true ways of doing things
3. Core values include:
a. Dedication and sacrifice
b. Hard work
c. Conformity
d. Law and order
e. Respect for authority
f. Patience
g. Duty before reward
h. Adherence to rules
(1) Honor
(a) A keen sense of ethical conduct
(b) One’s word given as a guarantee of performance
4. Veteran generational personality
a. Likes consistency and uniformity
b. Likes things on a grand scale
c. Are conformers
d. Believe in “logic” not “magic”
e. Are disciplined
f. Are past oriented and history absorbers
g. Believe in law and order
E. The Baby Boomers (people born from 1946 though 1964)
1. Comprise approximately 45% of today’s work force and one third of all Americans in 2007
2. Due to size, this group has had and will continue to have a great influence in all areas of society.
3. By 2030, all the baby boomers will be 65 years or older.
4. Unprecedented implications for all areas of society, especially health care
5. There is no typical baby boomer; they are extremely diverse and differ by:
a. As much as 19 birth years
b. Race
c. Culture
d. Socioeconomic status
6. Baby boomers paid their dues and climbed the ladder under the old rules.
7. Core values include:
a. Optimism
b. Team orientation
c. Personal gratification
d. Health and wellness
e. Youth
f. Personal growth
g. Involvement
h. Work
8. Baby Boomer generational personality
a. Dedicated and driven
b. Equate work with self-worth
c. Define themselves through their jobs, achieve identity by work performed
d. Arrive early and leave late
e. Chose profession with intent to make the world a better place
f. Believe you must pay your dues
g. Believe they do not have to grow old and be sedentary
h. Also called the Sandwich Generation, responsible for aging parents while still caring for teenage and college-age children
III. THEORIES OF AGING
A. Biological theories
1. Cellular functioning
2. Stochastic (error) theories
a. Wear and tear theory
b. Cross-linkage theory
c. Free radical theory
(1) Free radical and antioxidants
3. Nonstochastic theories
a. Programed aging theory
b. Gene theory
c. Immunity theory
4. Emerging biological theories
a. Neuroendocrine control or pacemaker theory
b. Caloric restriction (metabolic) theory
B. Sociological theories
1. Role theory
2. Activity theory
3. Disengagement theory
4. Continuity theory
5. Age stratification theory
6. Social exchange theory
7. Modernization theory
C. Psychological theories
1. Jung’s theories of personality
2. Developmental theories of Erikson and Peck
a. Theory of psychosocial development most widely used
b. Emphasis on healthy personality rather than pathologic approach
(1) Stresses rational and adaptive natures of individual
(2) Explains child’s behaviors in mastering developmental tasks
c. Stages of development
(1) Each stage has two components—favorable and unfavorable aspect of conflict.
(2) Progression to next stage depends on resolution of conflict.
(3) Conflict never mastered completely—remains a recurrent problem throughout life.
d. Stage VIII relates to the older adult.
(1) Ego integrity versus despair stage (stage VIII)
(a) Old age
(b) Results from satisfaction with life and acceptance of what has been
(c) Despair is a result of remorse for what might have been.
(d) Ego integrity results in renunciation and wisdom and concern with life in the face of death.
(e) Process achieved through introspection
e. Peck expanded on the original work of Erikson.
(1) Identification of discrete tasks of late life
(2) Achievement of tasks will result in ego integrity.
(3) Tasks represent a movement toward Erikson’s final stage.
3. Maslow’s Hierarchy of Human Needs
a. Focuses on attributes or characteristics that contribute to healthy personality development
b. Concerned with uniqueness and potential of individuals
(1) Humans motivated by two need systems
(a) Basic
(i) Food, water, and shelter
(b) Growth needs—internally motivated and reinforced
(i) Beauty
(ii) Self-fulfillment
(2) Needs arranged in a hierarchy
(a) Lower-level needs assume dominance.
(b) When one level need is satisfied, the next becomes predominant.
(c) Theory does not address developmental stages or shaping of human behaviors.
IV. PHYSIOLOGIC CHANGES OF AGING: CHANGES IN BOTH STRUCTURE AND FUNCTION
A. Changes that occur with aging are not incidental, they are expected.
1. Changes begin the moment life begins.
2. Changes become more apparent in the fifth or sixth decade.
3. In seventh and eighth decades, physiologic changes are significant and no longer deniable.
4. Changes in aging are predictable, but not the exact time they occur.
5. The timing and degree of aging is affected by heredity, environment, and health maintenance.
B. Functional age is impacted by:
1. Chronic disease processes
2. Personal attitudes and outlook
3. Family and friends network
C. Nervous system
1. Divided in two systems
a. Central nervous system (CNS)
(1) Consists of brain and spinal cord
b. Peripheral nervous system
(1) Consists of cranial nerves and spinal nerves
(2) Includes the somatic nervous system and the autonomic nervous system
c. Many functions occur at an unconscious level.
d. Other activities are done at a conscious level.
2. Neurogenic atrophy and reduction of peripheral nerve fibers
a. Decreased blood flow and CNS activity
(1) Causing slower reaction times
(2) Reduced ability to cope with body stressors
(3) Diminished ability to respond to demands on cardiovascular systems
(4) Prolonged emergence from pharmacologic interventions (e.g., benzodiazepines) and decreased pain perception
b. Decreased cognitive function
(1) Loss of memory and decreased understanding
(2) Lengthening of learning speed
(3) Higher risk of confusion
(4) Short attention span
(5) Decreased sensory abilities
(a) Impaired hearing acuity
(i) Men especially lose high-frequency sounds.
(ii) Deafness
(iii) Decrease in acoustic acuity
(b) Vestibular changes may also alter balance and/or cause vertigo.
(c) Visual precision is reduced.
(i) Lenses fail (as in cataracts).
(ii) Glaucoma
(d) Decreased tactile perception
(e) Acuity of smell diminished
(i) May impair hygiene
(6) Postoperative cognitive dysfunction in the elderly may persist at least 3 months after otherwise uncomplicated surgery.
c. Homeostatic mechanism slows, altering sympathetic and parasympathetic responsiveness.
(1) Decreased sensitivity to baroreceptors
(2) Change in thermoregulation
(a) Affected by autonomic impairment
(b) Changes to skin and blood vessels
(c) Impaired by many chronic medications
(d) Elderly vulnerable to heat stroke and hypothermia
d. Compromised perfusion caused by arteriosclerotic changes
(1) Increased incidence of organic brain syndrome
(2) Increased incidence of cerebrovascular accidents (strokes)
(3) Increased incidence of microemboli
(4) Decreased cerebral blood flow
(5) Decreased cerebral metabolic oxygen consumption
(6) Decreased CNS activity
3. Common disorders
a. Cerebral arteriosclerosis
b. Cerebral vascular accident
c. Parkinson’s disease
d. Dementia
e. Alzheimer’s disease
4. Nursing implications
a. Allow additional time to assimilate information and give responses.
b. Prepare for possible increased length of stay in ambulatory surgery.
c. Encourage use of sensory aids.
(1) Hearing aids
(2) Visual aids
(a) Glasses
(b) Contacts
(c) Magnifying glass
d. Include family member or responsible adult in instructions.
e. Verbal communication
(1) Face patient when speaking.
(2) Raise speaking volume, not pitch.
(3) Speak slowly and clearly.
f. Observe for prolonged or toxic effects of drugs.
(1) Encourage lower doses.
g. Safety measures
(1) Handrails
(2) Other assistive devices
(a) Canes, walkers, nonslip shower chairs
(3) Nonskid footwear
(4) Physical support by caretaker
(5) Observation
D. Respiratory system
1. Includes the nose, pharynx, larynx, trachea, bronchi, bronchioles, alveolar ducts, and alveoli
a. Provides for ventilation and gas exchange
b. Facilitates transfer of oxygen into and removal of carbon dioxide from the blood
c. Depends on the musculoskeletal system and CNS to function
2. Airway
a. Edentia
(1) Impacts patency of airway
(2) Creates difficulty in intubation
b. Decreased bone mass of jaw
3. Anatomic changes
a. Increased anteroposterior diameter
b. Progressive flattening and decreased muscle strength of diaphragm
c. Increased chest wall rigidity
(1) Arthritic changes in rib cage
d. Reduction in alveolar surface
e. Narrowing of intervertebral disks
(1) Reduces total lung capacity by 10%
f. Loss of skeletal muscle mass, leading to wasting of diaphragm and skeletal muscles
g. Loss of teeth changes jaw structure, leading to difficult airway maintenance.
4. Physiologic changes
a. Reduction in pulmonary elasticity
b. Decreased chest wall mobility
c. Loss of alveolar septa, leading to air trapping
d. Decreased pulmonary compliance
e. Increased airway resistance
f. Decreased cough and gag reflex, leading to risk of aspiration
g. Ventilation and perfusion alterations develop.
(1) Decreased tidal volume
(2) Decreased vital capacity
(3) Decreased inspiratory reserve
(4) Decreased cardiac output
(5) Decreased aerobic capacity
(6) Increased dead space
(7) Decreased oxygen and carbon dioxide exchange
(8) Decreased oxygen content of blood
(a) Pa o2 = 100 − (0.4 × Age in years) = mm Hg
(b) For example, in an 80 year old: Pa o2 = 100 − (0.4 × 80) = 68 mm Hg (vs normal Pa o2 of 100 mm Hg)
h. Environmental changes impact the respiratory system.
(1) Smoke
(2) Dust
(a) Air pollution
5. Common disorders
a. Chronic obstructive pulmonary disease (COPD)
b. Influenza
c. Pneumonia
d. Tuberculosis
e. Lung cancer
6. Nursing considerations
a. Airway
(1) Assess airway constantly.
(2) Protect unconscious airway.
(a) Suction oropharynx as needed.
(b) Support and position.
(3) Provide appropriate airways and oxygen delivery supplies.
(4) Inserting dentures can help support the airway.
b. Secretions and effective cough
(1) Position
(a) With head elevated when possible
(b) To maximize chest expansion
(2) Encourage coughing and deep breathing.
(3) Ensure reflexes have returned before administering oral fluids.
c. Oxygenation
(1) Monitor oxygen saturation (e.g., pulse oximeter).
(2) Support with oxygen as necessary.
d. Pain
(1) Alleviate pain.
(2) Use anxiety- and stress-reduction tactics.
E. Cardiovascular system
1. Comprises the heart, blood, blood vessels, and the lymphatics
a. Transports oxygen- and nutrient-enriched blood to the organs
b. Transports waste products to the excretory organs
2. Cardiovascular disease is the leading cause of death of older adults in the United States.
3. Most changes are caused by arteriosclerotic changes.
a. Loss of large artery elasticity
(1) Coronary
(2) Aorta
(3) Carotid
(4) Iliac
(5) Femoral
(6) Popliteal
(7) Renal
b. Decreased organ perfusion and decreased compensatory regulation from loss of elasticity
c. Vessel fragility
d. Increase in systolic blood pressure
4. Loss of tissue elasticity
a. Organ perfusion decreases
(1) Myocardium
(2) Decreases optimal regulation of all body systems
b. Peripheral circulation impaired
(1) Lowers tolerances to stress response (heart workload increases)
(2) Along with decreased collagen, increases difficulty of venipuncture
(a) Aging collagen makes tough “rolling” veins.
(b) Loss of elasticity is likely to cause bleeding around site during and after venipuncture.
(3) Higher risk for bruising
(4) Increases peripheral vascular resistance
(a) Restricts left ventricular ejection
(b) Promotes cardiac hypertrophy
(5) Potential for orthostatic hypotension
c. Increased susceptibility to clotting disorders
(1) Stroke
(2) Thrombosis
(3) Embolism
5. Cardiac conduction system
a. Decreased heart rate
(1) Resulting from increased parasympathetic activity
(2) Resulting from degenerative changes in conduction system
b. Dysrhythmias and blocks occur more frequently.
c. Can lead to CNS changes
d. Myocardial changes
(1) Left ventricular hypertrophy
(2) Increased myocardial irritability, leading to dysrhythmias
(3) Fibrosis of endocardial lining, leading to endocardial thickening and rigidity, decreased contractility
(4) Calcification of valves, leading to valve incompetence
6. Altered hemodynamics
a. Pump effectiveness diminishes because of atrophy of myocardial fibers.
b. Decrease in cardiac output (1% per year after 30 years of age)
c. Slower circulation time
d. Prolonged onset of action and clearing times for drugs
e. Increased blood pressure
f. Systolic blood pressure increases with aging, reflecting development of poorly compliant arterial walls.
g. Heart rate decreases, suggesting increase in activity of parasympathetic nervous system.
h. Slowed circulation time, leading to slower onset of drug effects
i. Decreased cardiac reserve; stressors
(1) Fever
(2) Tachycardia
(3) Exertion
(4) Anxiety
(5) Hypoxemia
(6) Pain
7. Orthostatic hypotension
a. Decreased blood vessel tone, leading to peripheral pooling of blood, increased risk for deep vein thrombosis
b. Baroreceptor failure
c. Medications (most common cause)
(1) Antihypertensives
(2) Diuretics
(3) Tricyclic antidepressants
(4) Phenothiazines
(5) Alcohol
d. Decreased tolerance to volume changes
8. Common disorders
a. Coronary artery disease
b. Coronary valve disease
c. Congestive heart failure
d. Peripheral vascular disease
9. Nursing considerations
a. Observe responses to medications.
(1) Allow adequate time for response before repeating.
(2) Use lower range of medication dosage and encourage team to use lower dosages.
b. Monitor for cardiac inadequacy.
(1) Lungs
(a) Provide adequate oxygenation.
(i) Encourage deep breathing.
(ii) Watch for fluid overload while ensuring adequate hydration.
(2) Heart
(a) Assess heart sounds.
(b) Cardiac monitoring for arrhythmias
(c) Assess lung sounds.
(d) Avoid extremes of blood pressure.
(i) Watch for orthostatic changes.
(e) Encourage slow position changes.
(f) Vascular considerations
(i) Gentle venipunctures
(g) Avoid tourniquets where possible.
(i) Minimize use of automatic blood pressure devices.
(ii) Adequate pressure on sites after venipuncture or catheter removal
(h) Encourage early ambulation.
F. Integumentary system
1. The largest organ of the body, includes the skin, hair, and nails
2. Loss of subcutaneous fat
a. Compromises thermoregulation
b. Increased risk of hypothermia
c. Loss of padding for bony prominences
3. Increase in overall body fat (especially women)
a. Increased availability of lipid storage sites
(1) Reservoir for lipid-soluble (fat-soluble) drugs: diazepam, midazolam, enflurane
(2) Prolongs drug action
4. Loss of sweat glands
5. Decreased skin pigmentation caused by decreased production of melanocytes; pallor does not equal anemia
6. Epidural atrophy and loss of collagen
a. Increases risk of skin breakdown and injury
b. Decreases skin elasticity and turgor
7. Common disorders
a. Basal cell carcinoma
b. Pressure ulcers
c. Inflammation and infection
d. Hypothermia
8. Nursing considerations
a. Provide warmed blankets and warm environment during and after operative event.
b. Protect skin with:
(1) Proper positioning
(2) Padding on bony prominences
(3) Use paper or other nontearing skin tape.
c. Remember, loss of pigmentation mimics pallor.
(1) Do not rely on skin color to assess for anemia or cardiac distress.
d. Provide careful positioning and safety instructions.
G. Musculoskeletal system
1. Multifunctional and complex system made up of bones, joints, tendons, ligaments, and muscles
a. Age-related changes are not life-threatening, but may affect the ability to function and ultimately the quality of life.
2. Osteoporosis: inappropriately low bone mass for age, gender, and race
a. Leads to decline in bone matrix
b. Peak bone mass around 30 to 40 years of age
c. Mineral content of bone (bone density) decreases.
(1) After 40 years of age
(2) For men, 0.5% per year
(3) About 1.0% per year for women
d. Skeletal support compromised
e. Bone reabsorption exceeds bone formation.
f. Increased risk of fractures, pain, skeletal deformities
(1) Repair of hip fractures is one of top five surgeries done in elderly patients.
g. Decrease in flexibility
h. Risk factors
(1) Age
(2) Female
(3) Low body weight
(4) White race
(5) Cigarette smokers
3. Degenerative changes in vertebrae increase difficulty of spinal anesthesia and intubation.
a. Degeneration of bone causes
(1) Pathologic changes
(a) Vertebral degeneration
4. Kyphoscoliosis
a. Limits chest expansion and capacity
b. Limits success in establishing spinal or epidural injection
c. Compression fractures
d. Increased potential for pathologic fracture
e. Higher incidence of traumatic fractures (falls especially)
5. Osteoarthritis
a. Specific cause unknown, but there is demonstrated relationship with:
(1) Advancing age
(2) Wear and tear of joints throughout life span
b. Structural changes in the joint
(1) Probably starts in cartilage
(2) Leads to:
(a) Reduced mobility of joint
(b) Difficult ambulation
(c) Potential for falls
(d) Pain
(e) Less flexibility
c. May compromise intraoperative positioning
6. Common disorders
a. Osteoporosis
b. Degenerative joint disease
c. Fractures
7. Nursing considerations
a. Careful positioning throughout perioperative experience
(1) Support for back
(2) Alignment
(3) Protection of bony processes
b. Observe for prolonged or toxic effects of regional agents.
c. Provide for pain relief.
d. Assist patient with physical tasks related to strength.
(1) Moving
(2) Ambulation
(3) Exercise
(a) Gentle movement
(b) Encourage frequent activity.
e. Safety concerns
(1) Concerted fall prevention program
(a) Fall risk assessment with individualized plan
(b) Environmental assessment
(i) Floor surfaces may be slippery, wet, or uneven.
(ii) Poor lighting or blinding light
(iii) Bathrooms not fall proof
(iv) Cluttered hallways and patient rooms
(c) Support when walking: cane, walker, rails
(d) Treaded (skid-resistant) footwear
(e) Education for patient and caretakers
(i) Potential for accidental falls: use skid-resistant slippers, handrails
(ii) Other safety measures: side rails, bed alarms
H. Digestive system
1. Includes the GI tract and accessory organs that assist in the digestive process
a. Begin to identify age-related changes in the fifth decade
b. GI tract includes the mouth, pharynx, esophagus, stomach, small and large intestine.
c. Accessory organs include the liver, gall bladder, and exocrine pancreas.
2. Decreased salivation
3. Decreased peristalsis
a. Gastric emptying delayed
b. Increased risk of aspiration
c. Increased problem of constipation
4. Decreased hepatic blood flow resulting from arteriosclerotic changes
5. Decreased microsomal enzyme activity
a. Delayed drug metabolism (e.g., fentanyl, vecuronium)
6. Decreased absorption of orally administered drugs and nutrients (e.g., ferrous sulfate iron and calcium)
7. Malnutrition possible
a. Can increase perioperative morbidity
b. Can compromise postoperative recovery and wound healing
c. Most reliable indicator of malnutrition is hypoalbuminemia.
8. Common disorders
a. Hiatal hernia
b. Gastroesophageal reflux disease
c. Diverticulitis
d. Hemorrhoids
e. Colon cancer
9. Nursing considerations
a. Careful administration of oral fluids and food
(1) Start with small amounts.
(2) Begin when sitting up if possible.
b. Elevate head of bed for most effective gastric emptying.
c. Consider ulcers with complaint of chest pain.
(1) Observe for prolonged or toxic drug effects.
I. Renal and genitourinary systems
1. Includes two kidneys, two ureters, bladder, and urethra
a. The urinary system is responsible for the removal of waste and excess fluid from the body.
b. The kidneys are highly vascular.
(1) Produce the hormone erythropoietin, which stimulates red blood cell production.
(2) Produce the enzyme renin, which helps regulate blood pressure.
(3) Continuously filter blood and regulate water, salts, and maintain acid-base balance.
2. Decreased bladder capacity (200 mL)
3. Decreased muscle tone and weakened sphincters
a. Especially in women after multiple obstetric deliveries
b. May result in incontinence
c. Increased residual urine
4. Enlarged prostate (men) may result in urinary incontinence and retention.
5. Atrophic changes of vagina and urethral mucosa in women
6. Decreased renal plasma flow
7. Decreased glomerular filtration rate
a. Resulting from decreased blood flow
b. Decreases 1% to 1.5% per year after 30 years of age
c. Results in decreased renal metabolism
(1) Decreased clearance of medications and metabolites
(2) Examples: fentanyl, vecuronium, midazolam
8. Response time to correct fluid and electrolyte balance increased
a. May increase risk of fluid overload
b. Decreased ability to concentrate urine
c. Inability to conserve sodium, leading to hyponatremia
d. Decreased activity of renin or aldosterone, leading to hyperkalemia
9. Common disorders
a. Urinary incontinence
b. Urinary tract infection
c. Chronic renal failure
10. Nursing implications
a. Observe for fluid imbalance.
(1) Monitor intake and output.
(2) Encourage oral fluids postoperatively.
b. Observe for effects of electrolyte imbalance.
(1) Monitor and/or observe for cardiac dysrhythmias, electrocardiogram (ECG) changes.
(2) Consider that hyponatremia may be a cause of confusion.
c. Observe for prolonged medication effect.
(1) Use lower dosage range of medications, and encourage smaller medication dosage by team.
(2) Provide support for toileting needs.
(a) Toilet frequently (offer urinal or bedpan).
(b) Assist to bathroom.
(c) Facilitate genitourinary hygiene.
(d) Provide protection for bedding and clothing.
(e) Reassure and support emotionally.
(f) Regard privacy to diminish embarrassment.
J. Endocrine system
1. The endocrine system works in conjunction with the neurological system to regulate and integrate body activities.
2. Includes the pituitary gland, thyroid gland, parathyroid gland, adrenal glands, and endocrine pancreas
3. Decreased ability to metabolize glucose
a. Results in glucose intolerance
b. Pancreatic function declines.
(1) Increased incidence of adult-onset diabetes mellitus
(2) Greatest between 60 and 70 years of age
c. Plasma renin concentrating ability decreases 30% to 50%.
4. Decreased production of renin, aldosterone, and testosterone
5. Decreased vitamin D absorption
6. Increased activation and increased plasma concentration of antidiuretic hormone
7. Common disorders
a. Diabetes mellitus
b. Hypoglycemia
c. Hypothyroidism
10. Nursing implications
a. Monitor laboratory values.
b. Educate the patient.
(1) Dietary requirements
(2) Blood glucose self-testing
K. Hematologic and immune system
1. Decreased bone marrow production
2. Decreased T-cell function
3. Increased autoantibodies
4. May see anemia and autoimmune diseases (see Chapter 29)
L. Sensory changes
1. Visual changes
a. Decreased visual acuity
b. Decreased peripheral vision
c. Decreased accommodation (presbyopia)
d. Retinal vascular changes
e. Cataract formation
f. Increased incidence of glaucoma
2. Auditory changes
a. Decreased sensitivity to sound (presbycusis)
b. Loss of high-pitched sound perception
c. Impairment of sound localization
3. Tactile changes
a. Decreased sensation
b. Decreased response to pain
4. Taste and smell acuity decreases.
M. Laboratory changes
1. Decreased potassium
a. Medications, diuretics
b. Diet deficient in potassium
2. Decreased sodium
a. Dilutional
b. True decrease
c. Renal failure
3. Decreased hemoglobin
a. Blood loss (GI and postmenstrual uterine bleeding)
b. Malabsorption of iron
c. Malnutrition
N. Neuropsychiatric changes
1. Acute brain syndrome
a. Physiologic
b. Rapid onset
c. Reversible
d. Possible causes—always rule out hypoxemia first!
(1) Medication intolerance
(2) Metabolic disturbance
(3) Electrolyte imbalance
(a) Hypernatremia and hyponatremia
(4) Nutritional deficit
(5) Depression
(6) Stress, fear, anxiety
2. Chronic brain syndrome
a. Associated with arteriosclerosis
b. Degenerative changes
(1) Alzheimer’s disease
(2) Cerebrovascular accident (stroke)
(3) Dementia
3. Depression
a. Causes: isolation, illness, loss, biochemical changes
b. Symptoms: fatigue, insomnia, anorexia, somatic changes
O. Pathophysiologic conditions in elderly
1. Of people 75 years of age, 86% have one or more of the following chronic conditions
a. Cardiovascular: hypertension, atherosclerosis, dysrhythmias, valve disease
b. Cerebral: cerebrovascular accident, cognitive degeneration
c. Pulmonary: COPD, asthma
d. Endocrine: diabetes mellitus, hypothyroidism
e. Neurologic: Parkinson’s disease
f. Musculoskeletal: arthritis
g. Sensory: visual and hearing loss
h. Hepatic: cirrhosis
2. Physical status changes increase anesthetic and surgical risk.
V. PSYCHOSOCIAL CONSIDERATION FOR THE ELDERLY
A. Maintain and promote autonomy.
1. Independence
a. Encourage performance of self-care.
b. Address issues of concern.
(1) Advance directives
(2) Quality-of-life issues
c. Talk with, not “around,” the patient.
d. Inquire about preferences.
(1) Name use (e.g., “What do you prefer that I call you?”)
(2) Time schedules (eating, sleeping, etc.)
2. Competence
a. Reduced ability to provide self-care leads to depression and reduced self-worth
b. Abilities to perform may alter with time of day, health status, and life events
c. Elders require more practice with new skills.
d. Repetition and clarification enhance learning
B. Encourage self-acceptance.
1. Maintain patient dignity.
2. Invite expression of fears.
a. Death and dying
b. Change in body image and function
3. Review coping mechanisms.
4. Present patient with decision alternatives when possible.
C. Time concept is altered.
1. Employ tactics for time orientation.
a. Time perception of elapsed time
b. Past, present, and future
D. Social awareness
1. Older adults are experiencing life role changes.
a. May outlive friends and family (especially old-old)
b. Caregivers become the patients (drastic role change when other party is already ill and debilitated).
2. Encourage participation of significant others.
VI. ELDER ABUSE (USUALLY RELATED TO FAMILY OR OTHER CAREGIVER)
A. Types
1. Material and financial
2. Physical
a. Sexual
b. Beating, slapping, kicking
c. Neglect
(1) Passive
(2) Active (especially old-old)
(3) Self
d. Emotional
e. Verbal
(1) Threatening physical abuse or isolation
(2) Humiliation
(3) Intimidation
f. Withholding (e.g., care, food, company)
g. Abandonment
B. Detection
1. Physical assessment and evidence of bodily harm
a. Bruises
b. Skin tears
c. Burns
d. Evidence of restraint
2. Emotional abuse (difficult to assess)
a. Fear of violence
b. Social isolation
C. Mandatory reporting
1. Different laws in each state
D. Resources
1. Adult protection programs
2. Domestic violence programs
3. Services
a. Financial advocacy
b. Social advocacy
c. Religious groups
VII. PHARMACOLOGIC ALTERATIONS IN AGING
A. Pharmacokinetics
1. Study of drug actions; includes absorption, distribution, metabolism, and excretion
2. Determines the concentration of drugs in the body
B. Pharmacodynamics
1. Describes the interaction of chemicals in medications being consumed and the receptors in the body
a. Responses to medications are less predictable in the older adult.
b. Pathologic changes may affect the response to medications.
c. Receptors may respond normally to some medications and not to others.
d. Receptors may be more sensitive and lead to an increased risk for toxicity.
C. The Beers criteria are guidelines for nurses to use to increase awareness of potentially inappropriate medications and possible adverse drug reactions in geriatric patients.
D. Alterations in organs responsible for drug metabolism and clearance
1. Lungs
2. Kidneys
3. Liver
E. Protein binding of medications impaired
1. Increases amount of available (free, unbound) drug
a. Free drug is active drug, increasing drug effects.
F. Storage of lipid-soluble medications increased
1. Unpredictable clearance and elimination
G. Prolonged action and elimination of medications
1. Require decreased doses of medications
2. Increased risk of cumulative drug effects
3. Increased risk of adverse drug reactions
H. Issues and trends in medication usage
1. Polypharmacy is a situation when multiple medications are taken at the same time.
a. May be multiple medications of the same class for chronic illness
b. May be related to multiple chronic illnesses
c. May be due to the addition of over-the-counter medications and supplements added to the prescribed medications
2. Financing medication use
3. Self-prescribing
4. Drug-herbal interactions
5. Drug-food interactions
6. Drug-drug interactions
7. Adverse drug reactions
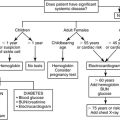
VIII. CONSIDERATIONS BEFORE SURGERY (Box 14-1)
A. Advantages of ambulatory surgery for the elderly
1. Decreased risk of nosocomial infections
a. Wound infections
b. Respiratory infections
2. Decreased incidence of mental confusion
a. Environment less disruptive
b. Decreased disruption in personal routine
3. Minimized length of stay away from home environment
4. Cost-effectiveness
B. Disadvantages of ambulatory surgery for the elderly
1. Compliance to the plan of care
a. Diminishing abilities
(1) Cognitive (e.g., forgetfulness)
(a) Unable to complete care regimen
(b) Unable to cope with changes in routine
(i) New medication protocols
(ii) Care related to procedure
(2) Physical
(a) Diminished stamina and strength for self-care
(b) Increased potential for falls
(c) Unaware of wound contamination
b. Lack of support system at home
(1) Transportation issues and other logistic issues
(2) Financial concerns (unable to obtain medications, supplies)
(3) Lack of caregiver or significant other
(4) Reduced or nonexistent circle of friends (especially in the old-old)
C. Preoperative assessment (see Chapter 15)
1. To obtain precise baseline
a. Consider physiologic not chronologic age.
b. Age alone does not determine risk.
2. To obtain information about preexisting disease
a. Especially with ambulatory patients
b. Includes medications used and appropriateness of use
c. Acute versus chronic conditions
d. Skin and pressure ulcer risk assessment
e. Previous surgical history
(1) Allow patient enough time to discuss history.
(2) Past tolerance to surgical procedures
(3) History of nausea and vomiting
(4) History of malignant hyperthermia
(5) Include accompanying adult in discussion as appropriate.
f. Risk assessment
(1) Coexisting diseases increase with age.
(2) General health status
(a) American Society of Anesthesiologists Status Classification
(3) Functional health status
(a) Complications more common in inactive patients
(4) Nutritional status
(a) Healing is delayed if undernourished.
(b) Decreased albumin level is a risk for increased complications and mortality.
(c) Serum albumin is warranted if poor nutrition is suspected.
(5) Psychological status
(a) Social support systems
(b) Will to live
(c) Dementia
(6) Heart disease
(a) Cardiac complications such as myocardial infarction and heart failure increase risk of complications and possible deaths.
(b) Any rhythm other than sinus rhythm
(c) Risk increased if premature atrial contractions are present
(d) Symptoms of heart failure (e.g., jugular vein distention, a third heart sound)
(e) Hypertensive and cardiac medications should not be withdrawn before surgery.
(7) Carotid artery disease
(8) Pulmonary disease
(a) Increases the risk of perioperative complications
(b) Smoking history
(c) Severe COPD increases risk of surgery.
(i) Ineffective cough
(ii) Inability to clear secretions
(d) Emphysema
(9) Liver disease
(a) Poor surgical outcome likely
(b) Coagulopathies
(10) Renal disease
(a) Assess by measuring blood urea nitrogen and serum creatinine.
(b) Dehydration should be corrected preoperatively.
(11) Sleep disorders
(a) Obstructive sleep apnea
(i) Characterized by repetitive cessation of respiration (>10 seconds) during sleep
(ii) May experience hypopnea
(iii) Excessive daytime sleepiness
(iv) Assessment should include information from sleeping partner.
(v) Therapy is dependent on the severity of sleep apnea.
(b) Insomnia
3. To review or obtain laboratory information
a. Anemia common
b. Electrolyte imbalance
(1) Hypokalemia resulting from diuretics
(2) Hyponatremia resulting from inability to conserve sodium
(3) Glucose levels in diabetic patients
4. To identify special needs
a. Prostheses
b. Language and communication barriers
c. Mobility aids
d. Barriers to ambulatory patient returning home
(1) Transportation
(2) Caregiver availability, ability to care for self
(3) Access to follow-up care
5. To anticipate postoperative sequelae and to reduce risk factors
6. To begin patient teaching
7. To maximize preoperative physical status
a. Pulmonary function
b. Nutritional status, including hydration
c. Medication protocol
8. Perioperative beta-blockade management
a. Beta-blocker use is appropriate when:
(1) Prescribed preoperatively, continue beta-blockers perioperatively
(2) High or intermediate risk of cardiac complications undergoing emergent, vascular, or other major surgery
(3) Consider beta-blockade for older adults at low risk of cardiac complications undergoing vascular surgery.
(4) Begin beta-blockade several days to 1 week before surgery to achieve heart rate less than 70 beats per minute.
(5) Continue after surgery with a goal of less than 80 beats per minute in the postoperative period.
(6) Withhold if:
(a) Heart rate less than 55 beats per minute or systolic blood pressure less than 100 mm Hg
(b) Patient has asthma, decompensated heart failure, or third-degree heart block.
D. Multidisciplinary assessment
1. PACU nurse
2. Anesthesiologist
3. Surgeon
4. Medical consultation as needed
BOX 14-1
COMMON SURGICAL PROCEDURES PERFORMED ON THE GERIATRIC PATIENT
▪ Ophthalmic: cataract, vitrectomy
▪ Genitourinary: cystoscopy, transurethral resection of the prostate
▪ Orthopedic: open reduction and internal fixation—hip, joint replacement
▪ Cardiovascular: pacemaker, carotid endarterectomy
▪ General: herniorrhaphy
IX. INTRAOPERATIVE CONSIDERATIONS FOR THE OLDER ADULT
A. Sensory
1. Avoid loud noises.
a. Music
b. Conversation not including the patient
2. Allow patient to keep sensory aids if possible.
3. Maintain voice, tactile, or visual contact with awake patient.
B. Environment
1. Remember thermostatic needs.
a. Increased risk when core body temperature falls below 96.8° F (36° C)
2. Protective measures
a. Raise room temperature.
b. Use warming blankets or devices.
c. Warm anesthetic gases, solutions, IV fluids.
d. Cover patient’s head.
C. Positioning
1. Change slowly and gently; avoid extremes.
2. Lift patient! Do not pull!
3. Support back of neck (e.g., prevent discomfort from kyphosis or arthritis).
4. Pad and support to protect pressure points.
D. Circulation: remember that hypotension and slowed circulation predispose patient to thrombus formation and emboli.
1. Use antiembolitic stockings or sequential compression devices.
a. Especially high-risk patient
b. Prolonged (greater than 2 hours) procedures
2. Observe for points of pressure that might inhibit blood flow to extremities.
E. Nurse-monitored local anesthesia; monitoring notes
1. Older adults do not tolerate fluid or blood loss well.
a. When patient approaches hypovolemia, small changes can have large impact.
b. Monitor fluid loss and output carefully.
2. Impending crisis may be indicated by fluctuations in cardiac rate and rhythm.
X. ANESTHETIC OPTIONS FOR OLDER ADULT PATIENT (see Chapter 22)
A. General anesthesia
1. Smooth induction and rapid recovery
2. Inhalation requirements less
a. Minimum alveolar concentration decreases by 4% per year after 40 years of age.
3. Delayed clearance or metabolism of IV anesthetic agents
a. Decrease dose of barbiturates, benzodiazepines, opioids.
4. Increased risk of hypothermia
5. If edentulous, may be difficult to ventilate by mask
6. Arthritis may limit cervicospinal mobility for intubation.
B. Regional anesthesia
1. Minimal physiologic alterations
2. Decreased cardiopulmonary complications
3. Less postoperative confusion
4. Provides postoperative analgesia
5. Spinal anesthesia
a. Lower abdomen and lower extremity surgery
b. Duration prolonged in older adult
c. Hypotension may be pronounced.
d. May be complicated by musculoskeletal changes
e. Low incidence of spinal headaches
6. Epidural anesthesia
a. Less hypotension
b. Greater cardiovascular stability
c. Reduced anesthetic dose requirements
C. Intravenous sedation and analgesia
1. Increased sedating effects of benzodiazepines
2. Increased respiratory depressant effects of narcotics
3. Because of coexisting diseases, may not be appropriate for RN to administer intravenous moderate sedation
D. Ambulatory surgery
1. Minimizes separation from family and environment
2. May be appropriate depending on type of surgery
a. Must consider risks of anesthetic, surgery, home care
XI. POSTANESTHESIA PRIORITIES FOR THE OLDER ADULT PATIENT IN PHASE I (Box 14-2)
A. Reduction of morbidity and mortality
B. Ventilation
1. Promote optimal gas exchange.
a. Provide high-humidity oxygen.
b. Promote deep breathing and coughing.
c. Prevent atelectasis.
d. Elevate head of bed to facilitate lung expansion.
2. Prevent respiratory infections.
a. Sterile suctioning of endotracheal tube
b. Protect patient from aspiration.
c. Promote deep breathing (prevent pneumonia).
3. Monitor for compromised function.
a. Observe for residual drug effects.
b. Maintain artificial airways.
c. Use pulse oximetry monitoring.
d. Consider preexisting disease.
C. Fluid balance (see Chapter 21)
1. Correct preoperative dehydration.
a. Nothing by mouth status
b. Diuretic therapy
c. Poor nutritional status
d. Presence of nausea and vomiting
2. Prevent fluid overload.
a. Assess preexisting cardiopulmonary disease.
b. Monitor intake and output.
c. Assess breath sounds.
3. Monitor urine output.
a. Decreased bladder capacity
b. Urinary retention (men), incontinence (women)
c. Perioperative diuretics
d. Perioperative fluid intake
e. Decreased awareness of distension
D. Activity—“stir-up” routine
1. Promotes circulation and ventilation
2. Permits assessment of neurologic status
a. Deviations from preoperative status
3. Monitor for orthostatic hypotension when mobilizing outpatients.
a. Mobilize more slowly than younger adults.
E. Thermoregulation (see Chapter 24)
1. Rewarm patient.
2. Document temperature.
3. Normothermia promotes cardiovascular stability.
F. Comfort (see Chapter 26)
1. Positioning
a. Care in turning; turn frequently
b. Anatomic and surgical alignment
c. Pad bony prominences
2. Skin care
a. Avoid excessive tape application.
b. Remove tape and ECG leads carefully.
c. Dry wet skin promptly.
d. Hold venipuncture sites after removal of needle.
e. Remove skin preparation solutions to decrease irritation.
3. Pain management
a. Titrate narcotics
b. Pain increases myocardial oxygen demand.
c. Consider decreased sensory response to pain.
d. Evaluate presence of residual preoperative or anesthetic drugs.
4. Psychological support
a. Reorientation
b. Avoid sensory deprivation and overload.
c. Avoid use of restraints.
d. Continue verbal and tactile communication.
e. Provide hearing aids, glasses, and dentures.
f. Provide simple, clear instructions—ascertain patient’s level of understanding.
g. Rule out hypoxemia as cause of postoperative agitation.
h. Maintain dignity and respect.
5. Social support
a. Family visitation in PACU phase I
BOX 14-2
EXAMPLES OF RELATED NURSING DIAGNOSIS CATEGORIES
▪ Impaired gas exchange
▪ Potential for infection
▪ Ineffective breathing pattern
▪ Alteration in fluid volume (excess or deficiency)
▪ Ineffective thermoregulation: hypothermia
▪ Knowledge deficit: preoperative/postoperative information
▪ Alteration in comfort: pain; nausea/vomiting
▪ Sensory-perceptual alteration
▪ Ineffective airway clearance
▪ Impaired physical mobility
▪ Self-care deficit
▪ Impaired communication: hearing loss/verbal/foreign language barrier
XII. POSTANESTHESIA PHASE II AND EXTENDED OBSERVATION PHASE (see Chapter 52)
A. Physical status
1. Ensure safety.
a. Orient/reorientation
b. Ambulate carefully.
(1) Sit on edge of stretcher to gain balance.
(2) Provide physical support for walking.
(a) Use orthopedic and prosthetic devices as necessary.
(b) Lower stretcher
(c) Step stool with caution (they tip!)
(3) Encourage, while allowing patient to find own pace of movement.
c. Return all sensory aids before ambulation.
d. Monitor neuromuscular status.
2. Psychological interventions
a. Promote wellness concept.
(1) Return clothes and belongings promptly.
(2) Reunite with family members, responsible adult, significant others.
b. Communicate with patient expecting:
(1) Slower thought processes, movements, and responses
(2) Old does not mean stupid!
3. Home preparation
a. Include support persons when reviewing home instructions.
b. Verify plans for home support.
(1) Ascertain patient, family, or responsible adult’s understanding of and ability to comply with discharge instructions.
(2) Older adult caring for older adult may not be adequate or responsible.
(3) Arrange time and place for postoperative contact.
(a) Recovery issues evaluation
(i) Consider tool easily understood by patient.
(ii) Introducing a Likert-type scale to patient before surgery would be beneficial.
(iii) Discuss possible topics of postoperative telephone contact.
c. Instruct on return to normal preoperative medication regimen.
d. Instructions
(1) Avoid sedating medications.
(2) Provide clear verbal instructions.
(3) Provide large-print written instructions.
(a) Large, simple diagrams or pictures
(4) Ascertain understanding (patient and other care providers as necessary).
(a) By demonstration
(b) Return demonstration
(5) Repeat instructions.
BIBLIOGRAPHY
1. American Society of Anesthesiologists, Syll-abus on geriatric anesthesiology. ( 2008) ; Available at:www.asahq.org/clinical/geriatrics/syllabus.htm; Accessed January 6.
2. Ang, P.; Knight, H.; Matadial, C.; et al., Managing acute postoperative pain: Is 3 hours too long?J Perianesth Nurs 19 (5) ( 2004) 312–330; quiz 331-333.
3. Beers, M.H.; Berkow, R., The Merck manual of geriatrics. ( 2000)Whitehouse Station, NJ, Merck Research Laboratories.
4. Capezuti, E.; Zwicker, D.; Mezey, M.; et al., Evidence-based geriatric nursing protocols for best practice. ed 3 ( 2008)Springer Publishing, New York.
5. Centers for Disease Control and Prevention–National Center for Health Statistics, Health, United States, 2006: Special excerpt: Trend tables on 65 and older population. ( 2008) ; Available at:www.cdc.gov/nchs/data/hus/hus06_SpecialExcerpt.pdf; Accessed January 27.
6. Drain, C.; Odom-Forren, J., PeriAnesthesia nursing: A critical care approach. ( 2008)WB Saunders, Philadelphia.
7. Ebersole, P.; Hess, P.; Touhy, T.A.; et al., Toward healthy aging. ed 7 ( 2008)Mosby, St Louis.
8. Gould, E., Tips for effective communication with older adults, Breathline 25 (2) ( 2005) 15.
9. Hart, S.M., Generational diversity impact on recruitment and retention of registered nurses, J Nurs Adm 36 (1) ( 2006) 10–12.
10. Hartford Institute for Geriatric Nursing, New York University College of Nursing, ConsultGeriRn. ( 2008) ; Available at:www.consultgerirn.org; Accessed January 27.
11. Iacono, M., Osteoporosis: A national public health priority, J Perianesth Nurs 22 (3) ( 2007) 175–180; quiz 181-182.
12. Laney, M.; Bayley, E., Incidence of adult immunization for influenza and pneumonia in a preadmission testing unit, J Perianesth Nurs 17 (5) ( 2002) 325–336.
13. Mamaril, M., The epidemiology of our aging population, Breathline 23 (4) ( 2003) 2.
14. Mamaril, M., Assessing neurological changes in the aging patient, Breathline 24 (2) ( 2004) 7.
15. Mamaril, M., Cardiac changes in the aging patient, Breathline 24 (2) ( 2004) 7.
16. Mamaril, M., Polypharmacy in the geriatric population, Breathline 24 (6) ( 2004) 5.
17. Mamaril, M., Advocating cultural sensitivity in older adults, Breathline 25 (5) ( 2005) 3.
18. Mamaril, M., Nursing considerations in the geriatric surgical patient: the perioperative continuum of care, Nurs Clin North Am 41 (2) ( 2006) 313–328.
19. (Editors: Mamaril, M.; Saufl, N.) Focus Issue: Geriatric Care. J Perianesth Nurs 19 (6) ( 2004) 371–443.
20. Martin, C., Bridging the generation gap, Nursing 34 (12) ( 2004) 62–63.
21. McKenney, K., Anesthesia considerations in older adults, Breathline 24 (5) ( 2004) 7.
22. Mezey, M.D.; Berkman, B.J.; Callahan, C.M.; et al., The encyclopedia of elder care. ( 2004)Prometheus Books, Amherst, NY.
23. Molony, S.L., In: Beers’criteria for potentially inappropriate medication use in the elderly ( 1999); Try This Series Issue 16 Available at:www.hartfordign.org/publications/trythis/issue16.pdf; Accessed January 21, 2008.
24. Rakel, B.; Herr, K., Assessment and treatment of postoperative pain in older adults, J Perianesth Nurs 19 (3) ( 2004) 194–208.
25. Reuben, D.B.; Herr, K.A.; Pacala, J.T.; et al., Geriatrics at your fingertips 2007-2008. ed 9 ( 2007)American Geriatrics Society, New York.
26. Swearingen, S.; Liberman, A., Nursing generations expanded look at the emergence of conflict and its resolution, Health Care Manag (Frederick) 23 (1) ( 2004) 54–64.
27. US Census Bureau, 65+ in the United States: 2005: Current population reports. ( 2008) ; Available at:www.census.gov/prod/2006pubs/p23–209.pdf; Accessed January 6.
28. US Department Health and Human Services, A profile of older Americans: 2004. ( 2008) ; Available at:www.aoa.gov/prof/Statistics/profile/2004/2004profile.pdf; Accessed January 4.
28. US Department of Health and Human Services, US Census Bureau, Population (2000). ( 2007) ; Available at:www.aoa.dhhs.gov/agingstatsdotnet/Main_Site/Data/2000_Documents/Population.pdf; Accessed December 30.
29. Wold, G.H., Basic geriatric nursing. ( 2008)Mosby, St Louis.