CHAPTER 13. The Adult Patient
Vallire D. Hooper and Jacqueline M. Ross
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Identify developmental issues associated with each stage of adulthood.
2. Define health, wellness, and illness.
3. List three types of health and illness behaviors.
4. Identify the effects of the stress response on the body’s adaptation to surgery.
5. List three characteristics unique to the adult learner.
I. DEFINITIONS
A. Growth
1. Increase in body size
2. Change in structure, function, or complexity of body cell content and metabolic and biochemical processes
3. Occurs up to some point of optimum maturity
B. Development
1. Growth responsibility arising at a certain time in the course of development
a. Successful achievement
(1) Satisfaction
(2) Continued success in future tasks
b. Failure
(1) Unhappiness
(2) Disapproval by society
(3) Difficulty with later developmental tasks and functions
C. Maturation and learning
1. Maturation: emergence of genetic potential for changes in
a. Form
b. Structure
c. Complexity
d. Integration
e. Organization
f. Function
2. Learning
a. The process of gaining specific knowledge or skill
b. Acquiring habits and attitude
c. Results from experience, training, and behavioral changes
3. Adequate maturation must be present for learning to occur.
D. Young adulthood
1. Age
a. Young-young adult: 25 to 30 years of age
b. Old-young adult: 31 to 45 years of age
2. Birth date and generation
a. Nexters/Generation Y: born between 1980 and 2000, although dates of generational cohort differ among authors
(1) Racially and ethnically diverse and tolerant
(2) Indulged as children; parents spent more time with children
(3) Blunt with opinions and expressions
(4) Sense of entitlement
(5) Techno-savvy; multitasking
(6) Adaptable to situations and change
(7) College education expected
(8) Defining moments
(a) Oklahoma City bombing—April 19, 1995
(b) Columbine High School shooting—April 20, 1999
(c) World Trade Center (9/11)—September 11, 2001
b. Generation X: born between 1964 and 1979, although dates of generational cohort differ among authors
(1) A very educated group of individuals in the United States
(2) Come from families with the highest divorce rate in the country; drastic increase in single-parent homes
(3) The largest group of latchkey children ever known
(a) Adept at self-management because of lack of attention in childhood
(b) Adept at managing their environments
(c) Comfortable with independent decision-making
(4) Less optimistic about the future; pragmatic
(5) Never feel financially secure
(6) View authority as on same level as self
(7) Value work-life balance
(8) Communicate directly, sometimes almost abruptly
(9) Defining moments
(a) Challenger explosion—January 28, 1986
(b) End of Cold War—1985-1991
(c) Economic turmoil; downsizing and layoffs
(d) Acquired immunodeficiency syndrome (AIDS)—1981
E. Middle age
1. Covers ages 45 to 65
a. Consider the physiologic age and condition of the body
b. Consider psychological age: how old the person acts and feels
2. Age divisions
a. Early middle age: 40 to 55
b. Late middle age: 56 to 64
3. Social class will affect age assignment.
a. Poorer person will perceive prime or midpoint as occurring at an earlier age.
4. Birth date and generation
a. Baby Boomers: born between 1946 and 1964, although definition of years vary among authors
(1) Most were raised in a two-parent home.
(a) Mother’s responsibilities were caring for the children and the home.
(b) Father was the breadwinner, authority figure, and rarely questioned.
(c) Most doted on generation by parents; seek personal gratification; considered the “me” generation
(2) Experienced many social reforms
(a) Civil rights movement
(b) Antiwar protests
(3) Experienced a lot of gains from a thriving economy
(4) Embrace the attitude of “only the best for me”
(5) Classified as workaholics
(a) Take great interest in material rewards
(b) Value promotion and recognition
(6) Committed to making the world a better place; fight for causes
F. Health
1. Defined by the World Health Organization, 1947, as a state of complete physical, social, and mental well-being; not merely the absence of disease
2. Often described on a continuum of wellness and illness
G. Wellness
1. The ability to adapt, relate effectively, and to function at near maximum capacity
2. Need to examine functioning in four areas
a. Physiologic factors: structures and functions of the body
b. Psychological factors: self-concept as affected by various demographic variables
(1) Age
(2) Sex
(3) Race
(4) Education
(5) Economic status
(6) Other
c. Sociocultural factors
(1) Interrelationships with others
(2) Environmental factors
(3) Lifestyle
d. Developmental factors: related to completion of developmental tasks
H. Disease
1. A state of non-health
2. Biological dysfunction present
3. Major focus of the medical model
4. Can be legitimized by the health care provider
I. Illness
1. The patient’s personal perspective of the disease state
2. Related to the psychosocial impact of the disease on the individual
3. Individual influences on perception of illness severity
a. Personality
b. Demographic characteristics
c. Presence of support systems
J. Learning
1. Process of acquiring wisdom, knowledge, or skill
2. Overt changes in behavior may be observed.
K. Teaching
1. Process of sharing knowledge and insight
2. Facilitating another to learn knowledge, insight, and skills
L. Health education
1. Transmits information, motivates, and helps people adopt and maintain healthful practices and lifestyles
2. Is concerned with the environment, professional training, and research to maintain and evaluate the process
3. Traditionally focuses on what the professional thinks is good or needed by the patient
4. Positive approaches generally more effective than fear
II. STAGES OF ADULTHOOD
A. Young adulthood
1. Developmental issues
a. Settling down
b. Must enter and successfully manage multiple new roles simultaneously
(1) Work
(2) School
(3) Marriage
(4) Home
(5) Child rearing
c. Primary tasks
(1) Finding an occupation
(2) Establishing a new family
(a) Often done without extended family in area
(b) Will change jobs and locations more frequently than previous generations
2. Sociocultural issues
a. Consistent positive influences
(1) Abundance of material goods and technology
(2) Rapid social changes
(3) Sophisticated medical care
(4) Accepting of diversity
b. Constant threats
(1) Terrorist attacks
(2) Pollution
(3) Overpopulation
(4) Loss of natural resources
c. Instant media coverage and internet access make the world small and outer space a not-so-distant place.
(1) All information is easily accessible and readily available.
(2) Instant, up close, and continuous coverage of traumatic events may cause psychological stress.
(a) Depression
(b) Panic and anxiety disorders
(c) Posttraumatic stress disorder
(d) Information overload
d. Other influences
(1) Changes in women’s roles
(2) Decreasing birth rates
(3) Increasing longevity
(4) Cultural and ethnic diversity
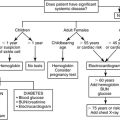
3. Issues affecting response to ambulatory surgery (Box 13-1)
BOX 13-1
DEVELOPMENTAL ISSUES AS RELATED TO AMBULATORY SURGERY
| Young Adulthood | Middle Age |
|---|---|
|
▪ Little or no insurance coverage
▪ Needs to return to work or school as soon as possible
▪ May need help with care of home, children, or parents
▪ May expect sophisticated medical technology to be able to fix anything with very little “down” time
|
▪ Physical condition often better indicator of surgical/anesthesia response than chronological age
▪ More financially stable
▪ Better insurance coverage
▪ May be balancing many professional, civic, and family responsibilities
|
B. Middle age
1. Developmental and sociocultural issues
a. Becoming one of the largest segments of the population
(1) Earn the most money
(2) Pay a major portion of the bills and taxes
b. Yield much power in
(1) Government
(2) Politics
(3) Education
(4) Religion
(5) Science
(6) Business
(7) Communication
c. Common experiences
(1) Good physical and mental health
(2) Personal freedom
(3) Good command of self and the environment
2. Issues affecting response to ambulatory surgery (Box 13-1)
III. HEALTH, WELLNESS, AND ILLNESS
A. Health care and prevention
1. Levels of health care
a. Health promotion: activities to improve or maintain optimum health
b. Disease prevention: actions to prevent disease or disability
c. Diagnosis and treatment: emphasizes early recognition and treatment of health problems
d. Rehabilitation: designed to limit incapacity caused by health problems as well as to prevent recurrences
2. Levels of prevention
a. Primary prevention: ways to prevent illness
b. Secondary prevention: early identification and treatment of health problems
c. Tertiary prevention: activities designed to return the physically or emotionally compromised person to the highest possible level of health
3. Ambulatory arena now involved in all levels of health care and prevention
IV. HEALTH AND ILLNESS BEHAVIOR
A. Health behavior
1. Activities undertaken by those believing themselves to be healthy
2. Purpose: to prevent disease or detect it in an asymptomatic stage
3. Examples
a. Breast self-exam
b. Regular exercise
c. Prudent heart living
d. Routine checkups
e. Ambulatory procedures
(1) Routine screening colonoscopy
(2) Follow-up cardiac catheterization in nonsymptomatic patient
B. Illness behavior
1. Activities carried out in response to a set of symptoms by those who feel ill
2. Allow individuals to determine their state of health and need for treatment
3. Limited to health-seeking behavior to identify and/or assess the changes occurring or to search for a solution
4. Influences affecting illness behavior
a. Recurrence of symptoms
(1) The more frequent or severe the symptoms, the more likely that outside help will be sought.
b. Visibility and consequences
(1) The more apparent the symptoms, the more illness behavior exhibited
(2) If the disorder is attached to stigma, the individual will be less likely to seek help.
(3) Help will usually be sought for life-threatening symptoms.
c. Perceived seriousness or severity
(1) Disorders perceived as serious lead to earlier illness behavior.
(2) Influences on perception of symptom severity
(a) Social class
(b) Health belief system
(c) Hierarchy of other needs and desires
d. Availability of treatment and the medical care system
(1) Distance, costs, convenience, time, effort, and fear of outcome affect willingness to seek help.
(2) Individual subordination by the health care system also affects willingness to seek treatment.
e. Knowledge and significance of symptoms
(1) Lack of knowledge of symptom significance often influences the individual to seek help.
f. Cultural and social expectations
(1) Cultural and ethnic backgrounds affect symptom interpretation and notion of when it is acceptable to seek health care.
(2) Lower classes are more influenced by symptoms interfering with important roles.
(3) The elderly use more health care services.
(4) Women seek medical attention more frequently than men.
(5) Those with a lack of access to care encounter issues with prevention and detection.
C. Sick role behavior
1. Activities undertaken by individuals who consider themselves ill for the purpose of getting well
2. Learned and influenced by evaluation and legitimization from others
3. Assumed when one accepts being ill, initiates some form of action, and demonstrates a desire to be well again
4. Major role components divided into rights and obligations
a. Rights
(1) Exemption from normal responsibilities
(a) Dependent on the nature and severity of the illness
(b) Requires validation or legitimization by others and the physician
(c) Once legitimized, person obligated to avoid responsibilities
(2) Right to be cared for
(a) Person not expected to recover by an act of will or decision
(b) Is not responsible for becoming sick and therefore has a right to be cared for
(c) Physical dependency and the need for emotional support are acceptable.
b. Obligations
(1) Obligation to want to become well
(a) Being ill is seen as undesirable.
(b) The sick role can result in secondary gains.
(c) Motivation to recover is of primary importance.
(2) Obligation to seek and cooperate with technically competent help
(a) The individual needs the technical expertise that health care professionals can provide.
(b) Cooperation with these professionals for the goal of getting well is mandatory.
5. Ambulatory implications
a. Patient may need to be educated that sick role behavior is acceptable and often expected after ambulatory procedures.
b. Ambulatory procedures often reduce the amount of time spent in the sick role.
V. STRESS RESPONSE SYNDROME
A. Definitions
1. Stress
a. A socio-psychophysiologic phenomenon
b. A composite of intellectual, behavioral, metabolic, and other physiologic responses to a stressor or stressors of internal or external origin
c. Influenced by environmental, psychological, and social factors
d. Uniquely perceived by the individual
2. Stressors (stress agents)
a. May be internal or external
b. Examples
(1) Cold
(2) Heat
(3) Infectious organisms
(4) Disease processes
(5) Fever
(6) Pain
(7) Imagined events
(8) Intense emotional involvement
3. Stress response
a. Initiated in response to a stressor
b. Is protective and adaptive by nature
c. Regulated by the nervous and endocrine systems
(1) Sympathetic nervous system (SNS)
(2) Pituitary gland
(3) Adrenal gland
d. The magnitude of the response depends on the perceived severity of the threat.
4. Survival depends on one’s ability to balance between stressors and adaptive capacities.
B. General adaptation syndrome
1. Developed by Hans Selye
2. Most widely accepted and frequently used physiologic theory of stress and adaptation
3. Three stages
a. Alarm stage
(1) Begins with the first exposure to the stressor
(2) Fight or flight mechanism activated
(a) Heart rate increases.
(b) Cardiac output increases.
(c) Stroke volume increases.
(d) Peripheral vasoconstriction
(e) Increased perspiration
(f) Gastrointestinal upset
(3) In most situations, the body’s defensive forces are mobilized to deal with the stressor.
(4) Death can occur if the stressor is strong enough to result in exhaustion of the body’s adaptive mechanisms and energy supply.
b. Stage of resistance or adaptation
(1) Reflects “adaptation” as the body fights back
(2) Psychological mobilization occurs.
(3) Influences on ability to adapt
(a) Physical functioning
(b) Coping skills
(c) Total number of stressors experienced
c. Stage of exhaustion
(1) A progressive breakdown of compensatory mechanisms and homeostasis
(2) Occurs only if the stress becomes overwhelming, is not removed, or if the individual is ineffective in coping with it
(3) All energy for adaptation exhausted
(4) Physiologic and psychological collapse will ensue.
C. Physiologic responses to stress
1. The initial response is stimulated by the central nervous system.
2. Information is then forwarded to the hypothalamus, which integrates and coordinates the homeostatic adjustments.
3. Hypothalamus stimulates the autonomic nervous system and the anterior and posterior pituitary.
4. The physiologic responses to hypothalamic stimulation and their effects on the surgical patient are listed in Table 13-1.
| SNS, sympathetic nervous system; BP, blood pressure; ACTH, adrenocorticotropin hormone; ADH, antidiuretic hormone. | ||||
| Responding Organ/ System | Organ/ System Action | Physiologic Response | Surgical Adaptation | Surgical Maladaptation |
|---|---|---|---|---|
| Autonomic nervous system | Triggers the SNS to stimulate exocrine glands | Sweating | No impact | No impact |
| Triggers the SNS to stimulate epinephrine and norepinephrine release | Decreases insulin and increases glucagon release | Increased amino acids for wound healing; increased wound healing |
Negative nitrogen balance that may negatively impact tissue repair unless reversed
Development of excessive scar tissue and adhesions
Increased blood sugar is detrimental to diabetics.
Increased heat loss may result in hypothermia, shivering, and increased oxygen demand.
|
|
| Constriction of vascular smooth muscle Increase in BP |
Shifts blood away from periphery to the vital organs Decreases blood loss by increasing clotting |
May decrease renal perfusion Increased thrombus formation |
||
| Increased heart rate and contractility Bronchodilation |
Increased myocardial perfusion Increased oxygen and perfusion to vital organs |
Increased workload for heart;may lead to heart failure Hypertension |
||
| Increased oxygen exchangeImproved ventilation | No maladaptation as a result of bronchodilatation | |||
| Kidneys are stimulated to release renin | Increased blood volume helps to reduce hypovolemia | Hypervolemia Hypertension |
||
| Converted to aldosterone by angiotensin II. | Maintenance of BP and cardiac output | Circulatory overload Heart failure | ||
| Aldosterone results in sodium and water retention at the renal tubules, resulting in increased blood volume. | Prolonged anti-inflammatory response may lead to infection. See above for other maladaptive responses. | |||
| Anterior pituitary | Releases ACTH Stimulates the adrenal cortex to release aldosterone and cortisol |
Aldosterone results in increased blood volume. Cortisol results in increase in blood glucose and protein and fat catabolism. | Increased blood sugar Increased wound healing Increased energy Increased anti-inflammatory responses |
|
| Posterior pituitary | Stimulates the release of vasopressin/ADH | Causes sodium and water retention at the renal tubules:
Results in increased blood volume
|
See above | See above |
D. Psychosocial responses to stress
1. Primary theory is the stress-appraised event theory by Lazarus.
a. Looks at stress and adaptation from the viewpoint of cognition, perception, and transaction
(1) The way the individual interprets the situation will determine whether he or she perceives it as stressful.
b. Positive and negative events can result in stress.
c. Emphasis is on the process or dynamics of what is happening.
2. Cognitive appraisal
a. The mental process used by the person to assess an event in relation to his or her well-being and available coping resources and options
b. Evaluative forms
(1) Irrelevant appraisal
(a) Occurs if the event is considered to be of no concern or impact on the current level of well-being
(2) Benign-positive appraisal
(a) Occurs if the event is considered as indicative of a positive state of affairs
(b) The event shows that all is well.
(3) Stressful appraisal
(a) Occurs with a negative evaluation of the present or future state of well-being
(b) Occurs in three forms
(i) Harm–loss: damage or injury has already taken place.
(ii) Threat: harm or loss has not yet occurred but is expected.
(iii) Challenge
[a] The possibility for growth or mastery is perceived.
[b] The opportunity for gain outweighs the possible risk of harm.
3. Coping modes
a. Defined as those efforts used to manage the environmental and internal demands exceeding personal resources; mobilized in response to an event perceived as stressful
b. Accomplished by eight coping modes
(1) Escape–avoidance
(a) Wishful thinking and other behavioral efforts to escape or avoid the problem
(2) Confrontive
(a) Aggressive efforts to alter the situation
(b) Involves some degree of hostility and risk taking
(3) Distancing
(a) Attempt to detach from the situation and thus minimize the significance
(4) Self-control
(a) Strive to regulate one’s feelings and actions
(5) Seeking social support
(a) Seek information, tangible and emotional support
(6) Accepting responsibility
(a) Acknowledge one’s own role in the problem
(b) Attempt to rectify the situation
(7) Planful problem solving
(a) Deliberate and analytical approach to altering the situation
(8) Positive reappraisal
(a) An effort to focus on the positive side or opportunity for personal growth
E. Behavioral responses to stress
1. Anger, hostility, antagonism, noncompliance
2. Depression, apathy, crying, inability to concentrate
3. Grief, shock, denial, withdrawal
4. Acceptance, information seeking, planning, decision-making
F. Factors affecting response to stressors
1. Nature of specific stressors encountered
2. What the stressors mean to the patient
a. May differ based on past experience and development
b. Ill patients may become less mature, less discriminating, and less reality oriented.
3. Patient’s characteristic mode of coping with stress
a. Depends on personality
b. Threat of hospitalization or surgery may be responded to by:
(1) An aggressive manner
(2) Resignation
(3) Seeking constant information
4. Patient’s current psychological resources
a. Determines the person’s resiliency and ability to endure the stress without decompensation
b. Affected by:
(1) Level of self-esteem and social support
(2) Presence or absence of any underlying depression or chronic anxiety
5. Hardiness factor
a. A personality characteristic
(1) A sense of control over one’s life
(2) Involvement and commitment to productive activities
(3) Anticipation of change as an exciting positive challenge
b. Acts as a buffer between stress and illness
VI. STRESS MANAGEMENT
A. Assessment of current level of stress
B. Intervention
1. Physical relaxation and stress management
a. Progressive relaxation
b. Acupuncture and acupressure
c. Biofeedback
d. Massage
e. Therapeutic touch
2. Cognitive methods of relaxation and stress management
a. Thought stopping
b. Positive self-talk
c. Assertive communication training
d. Laughter, humor, play, tears
e. Guided imagery
3. Time and resource management
4. Other nursing interventions
a. Acknowledge individual feelings and behaviors.
b. Develop trusting relationship.
c. Involve family and significant others.
VII. HEALTH PROMOTION AND PREVENTION
A. Activities designed to improve or maintain optimum health
B. Likelihood to participate in such behaviors influenced by internal and external cues
1. Internal cues include bodily states such as feeling good or energetic.
2. External cues
a. Interactions with significant others
b. Impact of media communication
c. Visual stimuli from the environment
C. Strategies include:
1. Physical, physiologic
a. Proper nutrition
b. Balance of exercise and rest
c. Cessation of destructive health habits (smoking, alcohol, or drug abuse)
d. Health screening
2. Emotional
a. Effective communication
b. Promotion of self-esteem, self-confidence, security
c. Anxiety reduction measures
d. Crisis resolution
3. Cognitive
a. Coping methods
b. Visualization and imagery
c. Health education
4. Social
a. Family, friend, peer relations
b. Group associations and processes
c. Maintenance of cultural ties
5. Spiritual and moral
a. Values clarification
b. Acknowledgment of meaning and purpose of life
c. Establishment of belief system
d. Establishment of moral and ethical behaviors
VIII. PREOPERATIVE HEALTH HISTORY INTERVIEW (see Chapter 15)
A. Should focus on age-specific issues in addition to general preoperative assessment and preparation
B. Young adulthood
1. Generally a healthy population
2. Pertinent health problems include:
a. Upper respiratory infection
b. Influenza
c. Essential hypertension
d. Mitral valve prolapse
e. Iron deficiency anemia
f. Simple diarrhea
g. Cystitis
h. Acute pyelonephritis
i. Chronic fatigue syndrome
j. AIDS
k. Hepatitis B
l. Cervical, breast, and testicular cancer
C. Middle age
1. Variety of health problems may begin to develop.
2. Pertinent health problems include:
a. Sinusitis
b. Hiatal hernia
c. Duodenal peptic ulcer disease
d. Angina pectoris
e. Secondary hypertension
f. Hyperthyroidism
g. Hyperuricemia or gout
h. Diabetes mellitus type II
i. Acute and chronic prostatitis
j. Lumbosacral strain
IX. HEALTH TEACHING–LEARNING (see Chapter 3)
A. Teaching is a critical nursing intervention that is crucial to successful outcomes in the ambulatory setting.
1. Teaching and learning processes are related.
2. Teaching–learning process is easily integrated into the nursing process.
B. Phases of the teaching–learning process
1. Assessment
a. Begins with an assessment of the nurse’s teaching abilities
b. Gather information about the patient, his or her learning needs, and his or her readiness to learn.
(1) Patient’s level of understanding, ability to comprehend, and any obstacles to learning (sensory losses, language barriers) should be identified during the general psychosocial assessment.
(2) Assessment should also include patient’s interest level, attentiveness, and current understanding about upcoming procedure.
c. A realistic teaching plan should be established based on:
(1) Patient’s current level of knowledge
(2) Nurse’s ability to provide the new information needed by the patient
d. A plan to identify and dispel patient misconceptions should also be included
2. Diagnosis
a. Diagnose the patient’s learning needs.
b. Set teaching priorities.
3. Planning
a. Set goals with the patient.
b. Determine behavioral objectives.
c. Select teaching and evaluation methods.
(1) Content and type of information
(2) Type of media used
(3) Who will be involved?
(4) The environment and time frame in which it will be provided
4. Intervention
a. Use appropriate strategies for instruction.
5. Evaluation
a. Evaluate patient outcomes.
b. Revise and reevaluate as needed.
C. Characteristics of the adult learner
1. Readiness to learn is determined by life tasks, roles, and immediate problems.
2. Application of learning is related to the relevancy of the problems.
3. Orientation to learning is independent and self-directed.
4. Value of experiences
a. Experiences are internalized.
b. Experiences provide a foundation for further learning.
c. May contribute to resistance to change
5. Rate of learning
a. Resistant to learning nonrelevant material
b. Aging process increases time needed to complete some learning tasks.
6. Barriers to learning
a. Family, work, or community responsibilities may compete with learning time and energy.
b. Anxieties about self-image may also threaten ability to learn.
7. Cultural differences
a. Unique beliefs should be respected.
b. Use interpreters and/or audiovisual aids for persons who do not speak English.
c. Be knowledgeable of cultures, ethnic groups, and religions commonly encountered in your environment.
8. Educational background
a. Identify level of formal education attained by the patient.
b. Remember that level of formal education does not equate with one’s ability to learn.
c. Determine patient’s reading level.
d. Determine patient’s health knowledge.
e. Determine patient’s feelings about education and learning.
f. Use pictures for patients with low literacy skills.
D. Domains of learning
1. Cognitive: concerns the learner’s knowledge and understanding
2. Affective: concerned with the learner’s attitudes, emotions, and ways of adjusting to an illness
3. Psychomotor: concerned with motor skills
E. Goals of teaching
1. To forewarn or provide information
2. To teach skills (Foley catheter care, dressing changes, etc.)
3. Assist in decision-making and planning.
4. Family involvement in patient care
5. Reinforcement of existing knowledge
6. Explain procedures, follow-up, and medications.
7. Discuss future events, expectations.
8. Advice about home health follow-up, home management
9. Encourage change, provide alternative behaviors or thoughts.
F. Maximizing teaching–learning effectiveness
1. Allow sufficient time.
2. Choose appropriate time and environment.
3. Confirm patient readiness.
a. Preoperative: admission details taken care of
b. Postoperative: pain controlled, stable, awake, family present
4. Actively involve the learner.
5. Use creativity in approaches.
6. Encourage learner to contribute to ideas.
7. Use humor or novelty to help learner relax and retain the content.
8. Organize material logically and present it in manageable amounts.
9. Highlight or point out important information.
10. Differentiate between similar concepts and contrasting information.
11. Allow practice as much as possible, giving constructive feedback.
G. Common barriers to effective teaching–learning
1. Providing false reassurance
2. Invading privacy
3. Minimizing or ignoring feelings
4. Not listening
5. Giving wrong information
6. Violating trust relationship
7. Noisy environment
8. Lack of privacy
9. Physiologic distraction (pain, nausea, vomiting, etc.)
10. Health literacy issues
a. Refers to individuals’ ability to understand their health care issues and effectively care for themselves within the health care system
b. Encompasses the skills that patients require to improve their health and navigate within the health care environment
c. Assume that literacy level 3 to 4 years below last completed year of education.
d. Lower income and blue-collar workers tend to have lower health literacy.
e. Essential in promotion of self-care
BIBLIOGRAPHY
1. Berman, A.; Snyder, S.J.; Kozier, B.; et al., Kozier & Erb’s fundamentals of nursing: Concepts, process, and practice. ed 8 ( 2008)Pearson Education.
2. Burmeister, W.L., In: Hiring/developing future leadersPresented at Southern Company training session, Birmingham, AL. ( 2000).
3. Cutilli, C.C., Health literacy in geriatric patients: An integrative review of the literature, Orthop Nurs 26 (1) ( 2007) 43–48.
4. Hooper, V.D., The next generation, J Perianesth Nurs 17 (3) ( 2002) 219–221.
5. Kupperschmidt, B.R., Understanding generation X employees, J Nurs Adm 28 (12) ( 1998) 36–43.
6. Lancaster, L.; Stillman, D., When generations collide: Who they are. Why they clash. How to solve the generational puzzle at work. ( 2003)Harper Business, New York.
7. Lubkin, I.M.; Larson, P.D., Chronic illness: Impact and interventions. ed 5 ( 2002)Jones & Bartlett, Boston.
8. McCance, K.L.; Huether, S.E., Pathophysiology: The biologic basis for disease in adults and children. ed 5 ( 2006)Mosby, St Louis.
9. Meisenhelder, J.B., Anniversary responses to terrorism, Am J Nurs 102 (9) ( 2002) 24AA; 24EE.
10. Mitchell, S., American generations: Who they are, how they live, what they think. ed 3 ( 2000)New Strategist Publications, Ithaca, NY.
11. Nielsen-Bohlman, L.; Panzer, A.M.; Kindig, D.A.; , the Committee on Health Literacy, Health literacy: A prescription to end confusion. ( 2004)National Academies Press, Washington, DC.
12. Strauss, W.; Howe, N., Generations. ( 1990)William Morrow & Company, New York.
13. Taylor, C.R.; Lillis, C.; LeMone, P.; et al., Funda-mentals of nursing: The art & science of nursing care. ed 6 ( 2008)Lippincott Williams & Wilkins, Philadelphia.
14. Taylor, R.B.; David, A.K.; Johnson, T.A.; et al., Family medicine: Principles & practice. ed 6 ( 2003)Springer-Verlag, New York.
15. Tulgan, B., Managing generation X: How to bring out the best in young talent. ( 2000)W.W. Norton & Company, New York.
16. Watson, D.S., Wanted: a few good nurses, AORN J 76 (1) ( 2002) 8–11.
17. White, L., Foundations of nursing. ed 2 ( 2005)Thomson Delmar.
18. Zemke, R.; Raines, C.; Filipczak, B., Generations at work. ( 2000)Amacon, New York.
19. Zimmerman, P.G., Generation X staff, J Emerg Nurs 26 (2000) 492–495.