β-adrenergic receptor blocking agents
The β1-adrenergic receptor located on the cardiac sarcolemma is coupled to adenyl cyclase via a G protein. When activated, adenyl cyclase converts adenosine triphosphate (ATP) to cyclic adenosine monophosphate (cAMP), a secondary intracellular messenger, that stimulates protein kinase A to phosphorylate membrane calcium channels, leading to an increase in cytoplasmic Ca2+. The consequences of β1-adrenergic stimulation are positive inotropy, chronotropy, dromotropy, and lusitropic relaxant effect (the latter by increasing the reuptake of cytosolic calcium into the sarcoplasmic reticulum). Because the secondary messenger cAMP is metabolized by phosphodiesterase, phosphodiesterase inhibitors augment β1 activity, which is manifested by sympathomimetic effects. Because of inhibition of G protein (e.g., vagal [muscarinic] stimulation), the coupling with adenyl cyclase is interrupted, resulting in attenuation of the effects described previously—the similar effects observed with inhibition of the β-receptor itself (Figure 91-1).
Indications for β-adrenergic receptor blockade
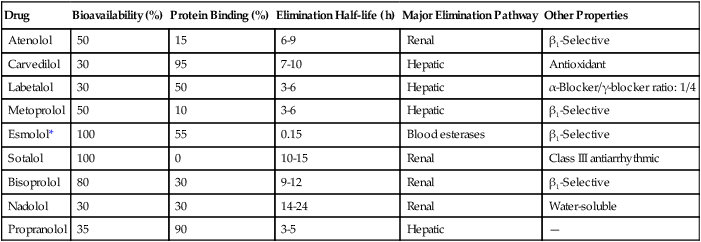
Because of their negative dromotropy, inhibitory effects in the sinus and atrioventricular nodes, and other antiarrhythmic properties (Table 91-1), β-adrenergic receptor blocking agents are recommended to acutely and chronically treat a number of tachyarrhythmias. They are indicated to treat supraventricular tachycardias, to control the rate in patients with atrial fibrillation, and to treat ventricular tachyarrhythmias (specifically metoprolol and sotalol [class III antiarrhythmic]). β-Adrenergic receptor blocking agents also counteract the arrhythmogenic effects of excess catecholamine stimulation, as seen, for example, in patients after myocardial infarction.
Table 91-1
Characteristics of Commonly Used β-Adrenergic Receptor Blocking Agents
| Drug | Bioavailability (%) | Protein Binding (%) | Elimination Half-life (h) | Major Elimination Pathway | Other Properties |
| Atenolol | 50 | 15 | 6-9 | Renal | β1-Selective |
| Carvedilol | 30 | 95 | 7-10 | Hepatic | Antioxidant |
| Labetalol | 30 | 50 | 3-6 | Hepatic | α-Blocker/γ-blocker ratio: 1/4 |
| Metoprolol | 50 | 10 | 3-6 | Hepatic | β1-Selective |
| Esmolol* | 100 | 55 | 0.15 | Blood esterases | β1-Selective |
| Sotalol | 100 | 0 | 10-15 | Renal | Class III antiarrhythmic |
| Bisoprolol | 80 | 30 | 9-12 | Renal | β1-Selective |
| Nadolol | 30 | 30 | 14-24 | Renal | Water-soluble |
| Propranolol | 35 | 90 | 3-5 | Hepatic | — |
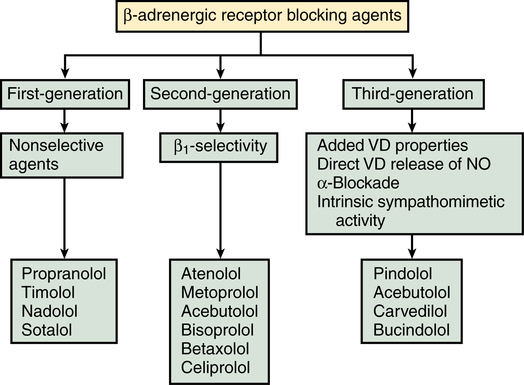
Pharmacology of β-adrenergic receptor blocking agents
Multiple β-adrenergic receptor blocking agents are available, differing in β1 cardioselectivity, lipid solubility, and whether or not they have intrinsic sympathomimetic activity (see Table 91-1).
Side effects
Abrupt discontinuation of β-adrenergic receptor blocking agents is associated with rebound hypertension and tachycardia, which can result in myocardial ischemia or infarction. With respect to specific side effects, labetalol has been associated with an increase in concentration of liver enzymes, an increased concentration of antinuclear and antimitochondrial antibodies, pruritus of the scalp, and positive tests for pheochromocytoma because it interferes with assays of metanephrine and catecholamines. Contraindications to the use of β-adrenergic receptor blocking agents are listed in Box 91-1.