Chapter 55 Medical-Legal Considerations
The ASA Closed Claims Project
I Historical Perspective
Anesthesiologists have a long-standing appreciation for risks associated with airway management. During the past 60 years, a variety of studies have demonstrated that events involving the respiratory system are a prominent cause of adverse outcomes in anesthesia practice.1–8 A few examples help illustrate this point. The Anesthesia Study Commission, which investigated anesthesia-related fatalities in metropolitan Philadelphia during the period 1935–1944, identified respiratory factors such as airway obstruction, hypoxia, and aspiration as the probable cause of death in approximately 19% of cases.7 A large, multicenter study by Beecher and Todd, conducted about a decade later when curare and other muscle relaxants were first entering clinical practice, led to the recognition of excess mortality associated with perioperative respiratory depression.1 In the 1970s, Utting and colleagues analyzed a 7-year series of anesthesia accidents reported to the Medical Defence Union of the United Kingdom (UK).8 Of 227 cases resulting in death or brain damage, 36% involved adverse respiratory events such as esophageal intubation, ventilator misuse, and aspiration.
Critical-incident studies have offered a similar picture. A landmark study in the late 1970s by Cooper and colleagues revealed that 29% of reported incidents were related to respiratory events such as airway mismanagement or failure and misuse of ventilators and breathing circuits.2 A decade later, the Australian Incident Monitoring Study provided a detailed analysis of the first 2000 cases voluntarily submitted since the late 1980s.6 In their collection of critical incidents, problems with ventilation accounted for 16% of reports from anesthesiologists in Australia and New Zealand.
II the Closed Claims Perspective
Claims represent only a small fraction of all adverse outcomes arising from medical care. The Harvard Medical Practice Study of patients in New York State in 1984 reported that approximately 4% of patients sustained an iatrogenic injury during hospitalization,9 but only 1 of every 8 injured patients filed a malpractice claim. Similar findings were described 10 years earlier by the Medical Insurance Feasibility Study in California.10 These small fractions make it unlikely that claims can be regarded as representing a cross section of all adverse outcomes.
A detailed description of data collection procedures for the Closed Claims Project has been reported previously.11,12 In brief, each claim file is reviewed by a practicing anesthesiologist, and a standardized form is used to record detailed information on characteristics of patients, surgical procedures, anesthetic agents and techniques, involved personnel, sequence of events, standard of care, critical incidents, clinical manifestations, responsibility, and outcome. Standard of care is rated on the basis of reasonable and prudent practices at the time of the event. Practice patterns that may have evolved at a later date are not retrospectively applied when the standard of care is rated. An adverse outcome is deemed preventable with better monitoring if the reviewer finds that the use—or better use—of any monitor would probably have prevented the outcome, whether or not such a monitor was available at the time of the event. An acceptable level of interrater reliability has been established for reviewer judgments on the standard of care and preventability of adverse outcomes with better monitoring.13
A Principal Features of Adverse Respiratory Outcomes and High-Frequency Adverse Respiratory Events
1 Basic Features
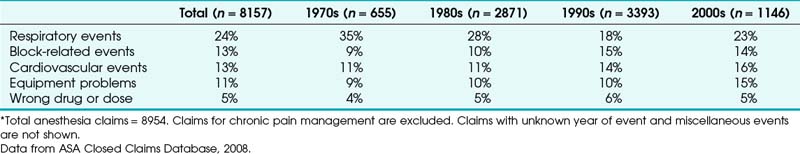
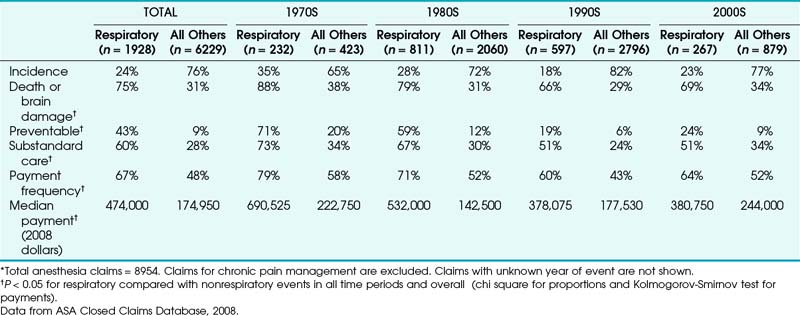
Adverse respiratory events constitute the single largest source of injury in the Closed Claims Project (Table 55-1). A detailed analysis of these events was initiated when the database reached a total of 1541 claims.14 The contrast between adverse respiratory events and other claims was particularly unfavorable. Respiratory event–related claims were (and still are) characterized by a high frequency of devastating outcomes and costly payments (Table 55-2).
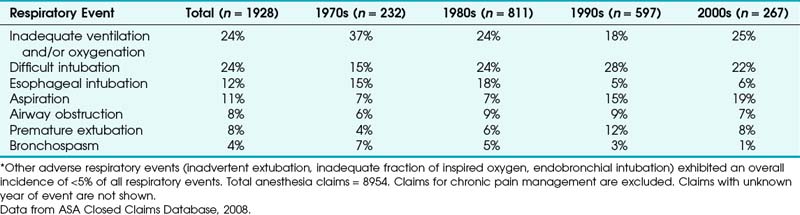
Just three mechanisms of injury accounted for almost two thirds of all claims for adverse respiratory events (Table 55-3). These mechanisms were inadequate ventilation (24% of cases), esophageal intubation (12%), and difficult intubation (DI; 24%). In the 1990s, after the adoption of pulse oximetry and end-tidal CO2 (EtCO2) as monitoring standards, DI (28%) and inadequate ventilation (18%) remained the most common adverse respiratory events, but esophageal intubation (5%) had decreased greatly compared with earlier decades (see Table 55-3). Evaluation of claims from the early 2000s suggests that this profile of adverse respiratory events is staying the same.
TABLE 55-3 Most Common Adverse Respiratory Events as Proportion of All Respiratory Events in Decade*
A detailed display of outcome and payment data for the three most common types of adverse respiratory events since 1990 (inadequate ventilation, DI, and aspiration) is shown in Table 55-4. Death and permanent brain damage were more frequent in claims for respiratory events compared with nonrespiratory events (P < 0.05). Claims for inadequate ventilation exhibited the highest proportion of death and brain damage (89%, see Table 55-4). Overall, payment for respiratory-related claims ranged from $1260 to $11 million (in 2008$). Most claims (61%) resulted in payment. Claims for adverse respiratory events typically involved healthy adults undergoing nonemergency surgery with general anesthesia (GA) (Table 55-5).
TABLE 55-4 Outcome, Payment, and Frequency for the Most Common Adverse Respiratory Events Occurring in 1990 or Later*
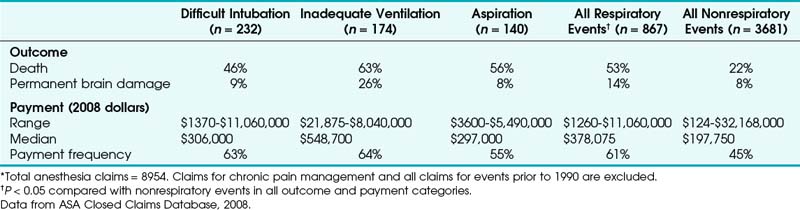
TABLE 55-5 Basic Clinical Features of Cases Involving Adverse Respiratory Events Occurring in 1990 or Later*
| Feature | Respiratory Events (n = 867) | All Others (n = 3681) |
|---|---|---|
| Age in years (mean ± SD) | 47.2 ± 19.8 | 45.5 ± 18.7 |
| Pediatric | 8% | 5% |
| ASAPS 1-2 | 42% | 53% |
| Emergency | 26% | 18% |
| Gender | ||
| Female | 51% | 59% |
| Male | 49% | 41% |
| Primary anesthetic | ||
| General | 81% | 62% |
| Regional | 4% | 27% |
| Monitored anesthesia care (MAC) | 8% | 6% |
| Other† | 7% | 6% |
ASAPS, American Society of Anesthesiologists Physical Status; SD, standard deviation.
* P < 0.05 for respiratory compared with nonrespiratory events in all categories (chi square test for proportions, t-test for age). Total anesthesia claims = 8954. Claims for chronic pain management and all claims prior to 1990 are excluded.
† Includes combined regional and general anesthesia, standby, and unknown.
Data from ASA Closed Claims Database, 2008.
2 Inadequate Ventilation
The largest class of adverse respiratory events was inadequate ventilation. The distinguishing feature in this group of claims was the reviewer’s inability to identify a specific mechanism of injury. In part, the inability to assign a mechanism of injury may reflect uncertainty on the part of the original health care providers. Because most adverse events occurred before the widespread use of pulse oximetry and capnometry, the uncertainty may be due to the limitations of traditional clinical signs, such as chest excursion, reservoir bag motion, and breath sounds. With increasing use of quantitative measures of ventilation, fewer cases have been assigned to the category of inadequate ventilation. These events have declined in occurrence from 37% of all respiratory events in the 1970s to 25% in the 2000s (see Table 55-3). It is also possible that a delayed rather than contemporaneous approach to the investigation of adverse outcomes is not powerful enough to provide an understanding of many events.
3 Esophageal Intubation
In 1990, we performed an in-depth analysis of 94 closed claims for esophageal intubation.14 Almost all (92%) of these claims occurred during the period 1975–1985, before routine use of intraoperative capnometry. The single most striking finding was that detection of esophageal intubation required at least 5 minutes in most cases (97%). Our immediate reaction was simply, “What took so long?” We wondered whether such delays in detection were caused by incompetence or negligence (e.g., intubation performed by a legally blind physician, minimal attention to the patient during the procedure), but we found only eight claims (9%) that could be explained in such a way.
Using this information, we constructed a best-case scenario by assuming that auscultation led to a correct diagnosis in the 3 cases in which it actually did so, as well as in the 61 cases in which there was no information about its role or the information was unclear. Using this approach of constructing a hypothetical situation to demonstrate the greatest possible benefit, auscultation is still associated with a misdiagnosis rate of 32% (30 of 94 cases). Although the limitations of auscultation are well known,15 we think these claims emphasize the importance of confirming intubation with the quantitative and ongoing information provided by capnometry.
Another indirect test of ventilation is cyanosis. Almost all of the esophageal intubation claims that we studied took place before pulse oximetry became part of the ASA Standards for Basic Anesthetic Monitoring. The human eye is relatively insensitive to the changes in skin color that occur during arterial desaturation,16,17 so it is not surprising that cyanosis preceded the recognition of esophageal intubation in only 34% of cases. One might also expect cardiovascular clues to accompany hypoxemia or hypercarbia and that these clues might alert the anesthesiologist to the possibility of esophageal intubation. Indeed, at least one major hemodynamic derangement was recorded in 79 (84%) of the 94 claims for esophageal intubation, and this knowledge preceded the recognition of esophageal intubation in 60 claims (65%). In order of frequency, the abnormalities included bradycardia, asystole, hypotension, unspecified dysrhythmia, tachycardia, and ventricular fibrillation (Table 55-6). Such changes certainly have the potential to serve as cues, but when they are extremely severe (e.g., ventricular fibrillation, asystole) they draw attention away from the underlying problem and leave very little time for effective remedies. These features point to the importance of confirmatory tests that provide early, direct, and ongoing confirmation of ventilation through the ETT.
TABLE 55-6 Major Hemodynamic Derangements Accompanying Esophageal Intubation Claims*
| Hemodynamic Derangement | Percent of Claims (n = 94) |
|---|---|
| Bradycardia | 57 |
| Asystole | 55 |
| Hypotension | 49 |
| Unspecified dysrhythmia | 10 |
| Tachycardia | 5 |
| Ventricular fibrillation | 1 |
* Percentages sum to more than 100 because of multiple derangements. Total anesthesia claims = 1541.
Data from ASA Closed Claims Database, 1990. Table adapted from Caplan RA, Posner KL, Cheney FW, et al: Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology 72:828, 1990.
Is injury from undetected esophageal intubation no longer a concern? As shown in Table 55-3, claims for esophageal intubation decreased considerably in the 1990s and later compared with the prior two decades. A few claims for esophageal intubation still enter the database, but they usually involve cases in which capnometry was unavailable or not used or the procedure took place in a remote location.18
4 Difficult Intubation
An evidence-based guideline for management of the difficult airway (DA) has been developed by the ASA.19 Key features of this guideline are discussed in Chapter 10. The impact of this set of guidelines on claims involving DA management was studied in the ASA Closed Claims Project.20 DA problems were encountered during all phases of anesthesia management, including preinduction, induction, maintenance, emergence, postanesthesia care unit (PACU) care, and intensive care unit settings. Death and brain damage were more common in DA claims arising from procedures performed outside the operating room (OR) or the PACU and in the settings of difficult mask ventilation (DMV); “cannot intubate, cannot ventilate” (CICV) emergencies; or persistent intubation attempts.20
5 Aspiration
An in-depth analysis of claims for pulmonary aspiration was conducted in 1991, when such claims accounted for 3% of the database (56 cases).21 Almost all cases (95%) occurred in patients who received GA. The aspirated material was gastric contents in 88% of these cases; other cases involved aspiration of blood, pus, or teeth. Approximately one third (34%) of aspirations took place during anesthetic induction just before endotracheal intubation. In 6 of these cases, aspiration occurred during a rapid-sequence induction; in another 6, the aspiration occurred under circumstances in which the reviewer believed that rapid-sequence induction was indicated but in which it was not used. Another one third of aspiration cases (36%) took place during the maintenance phase of mask GA. Only 2 cases (4%) occurred during the maintenance phase of endotracheal GA. Aspiration occurred in one of these cases when the ETT was removed to facilitate the passage of a nasogastric tube. In the other instance, aspiration occurred while an ETT with a leaking cuff was being replaced with a new tube. The remaining cases (18%) took place during emergence from anesthesia.
Two clinical factors—pregnancy and emergency surgical status—were particularly prevalent in claims for aspiration. Obstetric patients accounted for 12% of the overall database but represented 29% of all aspiration claims (P < 0.05) in the 1991 study.21 This trend changed dramatically in subsequent years, with aspiration occurring in fewer than 1% of obstetric claims from 1990 or later.22 Emergency surgery patients accounted for 19% of the database in 1991 but represented 45% of all aspiration claims (P < 0.01). It is also noteworthy that 23% of aspiration claims involved a problem with airway management, such as DI (9 cases) or esophageal intubation (4 cases). This relationship was previously reported by Olsson and colleagues.23
Overall, aspiration accounted for only 3% of claims in the database. This is consistent with the observation by Warner and colleagues that the incidence of aspiration in more than 200,000 patients who underwent elective or emergency surgery during 1985–1991 was very low (1 in 3216).24 These observations suggest that current strategies used to prevent aspiration in the United States are generally successful, particularly in obstetric patients.
B Low-Frequency Adverse Respiratory Events
1 Basic Features
The foregoing discussion focused on the most common mechanisms of respiratory injury in the closed claims database. A formal study of low-frequency adverse respiratory events was conducted in 1991, when the ASA Closed Claims Project database had reached 2046 cases.21 Although these events were much less common (each category representing no more than 5% of the overall database), sufficient claims were collected to permit the identification of recurrent themes that might contribute to liability. Five categories of events have been studied in depth, each category containing at least 40 claims and together encompassing 300 claims, or about 15% of the overall database. These categories are airway trauma, pneumothorax, airway obstruction, aspiration, and bronchospasm. Death or brain damage occurred in almost half (47%) of these cases, and the median payment was $60,000 (Table 55-7). Airway trauma was reanalyzed in detail in 1999.25 Aspiration now represents one of the most common adverse respiratory events.
2 Airway Trauma
Airway trauma was the most common type of low-frequency airway event, accounting for 266 of 4460 claims, or 6% of the overall database, in the 1999 study.25 DI was associated with 103 (39%) of these claims. The most frequent sites of injury were the larynx, pharynx, and esophagus (Table 55-8), which together accounted for 70% of injuries associated with airway trauma claims. Esophageal and tracheal injuries were more likely than other airway trauma claims to be associated with DI. In contrast, laryngeal and temporomandibular joint (TMJ) injuries were rarely associated with DI. Pharyngeal and esophageal injuries most commonly consisted of lacerations or perforations leading to mediastinitis or mediastinal abscess. The most common laryngeal injuries were vocal cord paralysis (30 cases), granuloma (15 cases), and arytenoid dislocation (7 cases). None of the 27 TMJ injuries was associated with DI.
TABLE 55-8 Distribution of Airway Trauma Sites and Presence of Concomitant Difficult Intubation
| Location of Injury (% of Total) | Difficult Intubation (% of Site) | |
|---|---|---|
| Larynx | 87 (33%) | 17 (20%)* |
| Pharynx | 51 (19%) | 26 (51%) |
| Esophagus | 48 (18%) | 30 (62%)* |
| Trachea | 39 (15%) | 25 (64%)* |
| Temporomandibular joint | 27 (10%) | 0 (0%)* |
| Nasopharynx, nose | 13 (5%) | 4 (31%) |
* P < 0.05 compared with other sites combined. Total anesthesia claims = 4460.
Data from ASA Closed Claims Database, 1999. Table adapted from Domino KB, Posner KL, Caplan RA, et al: Airway injury during anesthesia: A closed claims analysis. Anesthesiology 91:1703, 1999.
Although it is easy to understand how DI may lead to trauma of the larynx, it is less apparent why laryngeal injuries appeared to be so infrequently associated with DI. The reasons for vocal cord paralysis, granuloma, and arytenoid dislocation with routine intubation were not apparent from the data available in the claim file. Similarly, it is curious that TMJ injury was present only with routine intubation. One might expect that TMJ injury would be more commonly associated with DI, in which forces applied to the jaw during airway manipulation and laryngoscopy might be more intense or prolonged than those encountered during routine intubation. These observations suggest that many injuries to the larynx and TMJ may be related to predisposing factors or underlying characteristics of patients that we do not yet understand. A similar phenomenon was observed in the review of closed claims for peripheral nerve injuries.26,27
3 Pneumothorax
Pneumothorax was the second most common type of low-frequency airway event.21 Clinical activities that were not directly or clearly related to airway management were associated with 43 (64%) of the 67 claims for pneumothorax (Table 55-9). In particular, five types of nerve blocks (supraclavicular, intercostal, stellate ganglion, interscalene, and suprascapular) were responsible for 40% of pneumothorax claims. Airway instrumentation was associated with pneumothorax in 19% of cases. The actual mechanism of pneumothorax was not anatomically proved in most cases but was usually attributed to laryngoscopy, ETT placement, or bronchoscopy on the basis of clinical events and reviewer judgments. Barotrauma was the cause of pneumothorax in 11 claims (16%), mostly arising from obstruction of the expiratory limb of a mechanical ventilator or the use of excessive tidal volumes (7 cases).
TABLE 55-9 Clinical Factors Associated with Pneumothorax Claims*
| Clinical Factor | Claims | Total (%) |
|---|---|---|
| Airway Related | ||
| Airway instrumentation | 13 | 19 |
| Barotrauma | 11 | 16 |
| Non–airway Related | ||
| Regional block | 27 | 40 |
| Central line | 5 | 7 |
| Spontaneous or unknown | 5 | 7 |
| Other | 6 | 9 |
| Total | 67 | 100 |
* Total anesthesia claims = 2046.
Data from ASA Closed Claims Database, 1991. Table adapted from Cheney FW, Posner KL, Caplan RA, et al: Adverse respiratory events infrequently leading to malpractice suit: A closed claims analysis. Anesthesiology 75:932, 1991.
4 Airway Obstruction
Airway obstruction accounted for 56 claims, or approximately 3% of the database.21 Most cases (89%) occurred during GA. Obstruction was attributed to an upper airway site in 39 claims (70%), although an exact cause or site was identifiable in only half of these claims. Laryngospasm was the most common cause of upper airway obstruction, accounting for 11 (28%) of 39 cases. Other causes of upper airway obstruction included foreign body (4 cases), laryngeal polyps (2 cases), laryngeal edema (1 case), and pharyngeal hematoma (1 case). In 10 cases of upper airway obstruction, emergency tracheostomy was performed.
5 Bronchospasm
Adverse outcomes arising from bronchospasm accounted for 40 claims, or almost 2% of the database.21 Most of these claims (80%) occurred during the administration of GA as the primary anesthetic technique. Almost half (48%) of the patients had a medical history that included asthma, chronic obstructive pulmonary disease, smoking, or some combination of these. In cases involving the administration of GA, the first occurrence of bronchospasm was more often at the time of intubation (69%) than during maintenance (25%) or emergence (6%).
Bronchospasm claims were also notable in cases that involved a difficult differential diagnosis. The claims files in the 1991 study indicated that clinicians had difficulty distinguishing between bronchospasm and the presence of esophageal intubation (6 cases) or pneumothorax (4 cases). EtCO2 monitoring was not used in any of the 6 cases in which the failure to make a correct and timely differential diagnosis between esophageal intubation and bronchospasm led to an adverse outcome. EtCO2 is now an ASA standard for verification and monitoring of ETT placement, and bronchospasm appears to be on a steadily declining trend (see Table 55-3). However, it is important to recognize that failure to differentiate between bronchospasm and esophageal intubation may still occur in cases in which bronchospasm is so severe that ventilation is impossible and CO2 cannot reach the detector in clinically useful amounts. In this circumstance, fiberoptic bronchoscopy can be helpful.
C Emerging Trends from the ASA Closed Claims Project
In 1999, an examination of trends was conducted.11 At that point, the database consisted of more than 4000 claims drawn from 35 U.S. insurance organizations. Two major trends were evident. First, there was a general decrease in the severity of injury that was specifically characterized by a declining incidence of claims for death and brain damage. For example, 56% of claims between 1970 and 1979 involved death or brain damage, compared with only 31% of those between 1990 and 1994. Second, the contribution of adverse respiratory events to death and brain damage declined. During the earliest interval, 1970–1979, 56% of claims for death and brain damage arose from respiratory system events. This percentage decreased to 49% in 1980–1989 and to 38% from 1990 onward.
Is the presence of these monitors reflected in the pattern of liability for closed claims? This question was explored in 2006, when the overall database contained 6894 cases.28 Claims for death and brain damage between 1975 and 2000 were analyzed. Respiratory events declined from approximately 50% of death and brain damage claims before 1986 to 28% by 1992. A downward trend in claims for death and brain damage and a similar downward trend in the proportion of respiratory events leading to these claims preceded the introduction of pulse oximetry and EtCO2 monitoring into anesthetic practice. These decreases seemed to be unrelated to the increase in the proportion of claims in which these monitors were used.28
New trends in adverse respiratory events are now emerging outside the traditional arena of GA in the OR. An analysis of closed claims from 1990 or later that were associated with monitored anesthesia care (MAC) revealed that respiratory depression after an absolute or relative overdose of sedative or opioid drugs was the most common specific mechanism leading to claims (21%).29 Most of these claims involved death or brain damage. Improved respiratory monitoring (capnography, improved vigilance, audible alarms) might have prevented almost half of these claims. One quarter of these claims arose from procedures performed in the endoscopy suite.
Analysis of claims from 1990 or later associated with procedures outside the OR found that adverse respiratory events were more common in remote locations and were often judged as preventable by better respiratory monitoring.18 A 2009 ASA Statement on Respiratory Monitoring During Endoscopic Procedures provided guidance on CO2 monitoring and airway management during endoscopic procedures.30 Since July 2011, the ASA Standards for Basic Anesthetic Monitoring have provided additional specificity about the use of CO2 monitoring: “During moderate or deep sedation the adequacy of ventilation shall be evaluated by continual observation of qualitative clinical signs and monitoring for the presence of exhaled CO2 unless precluded or invalidated by the nature of the patient, procedure, or equipment.31
As mentioned previously, evidence-based guidelines for management of the DA have been developed by the ASA.19 Clinicians often worry that the proliferation of practice guidelines will lead to a general increase in liability. It is important to remember that modern, evidence-based guidelines have a relatively flexible place in medical practice that differs from that of standards. Standards are typically used for straightforward aspects of care that command high levels of agreement and acceptance. Noncompliance implies an action that is outside a clearly recognized norm; in some instances, such actions may be accompanied by sanctions. Guidelines are employed for more complex aspects of care that cannot be precisely codified and accepted in a near-uniform fashion. Guidelines are intended as recommendations that can assist the anesthesiologist and the patient in making decisions about health care. Guidelines may be accepted, modified, or even rejected according to specific clinical needs and constraints. This means that not following a guideline, under some clinical conditions, can still be a decision that is consistent with reasonable and prudent practice. In DA malpractice claims, the ASA guideline for management of the DA has rarely been an issue in litigation. In the few claims in which the guideline was a factor, it was used for the defense more often than for the plaintiff.20
IV Clinical Pearls
• Anesthesiologists have a long-standing appreciation for risks associated with airway management.
• Adverse respiratory events constitute the single largest source of injury in the ASA Closed Claims Project database.
• Claims for adverse respiratory events are characterized by devastating patient injuries and high liability payments.
• The most common adverse respiratory events in claims since 1990 are difficult intubation (DI), inadequate ventilation, and aspiration
• The occurrence of injuries related to inadequate ventilation has been decreasing, but DI remains a recurring problem.
• Adverse respiratory events are emerging as a source of patient injury during monitored anesthesia care (MAC), especially in remote locations outside the operating room (OR).
All references can be found online at expertconsult.com.
11 Cheney FW. The American Society of Anesthesiologists Closed Claims Project: What have we learned, how has it affected practice, and how will it affect practice in the future? Anesthesiology. 1999;91:552–556.
14 Caplan RA, Posner KL, Ward RJ, et al. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990;72:828–833.
18 Metzner J, Posner KL, Domino KB. The risk and safety of anesthesia at remote locations: The US closed claims analysis. Curr Opin Anaesthesiol. 2009;22:502–508.
19 Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–1277.
20 Peterson GN, Domino KB, Caplan RA, et al. Management of the difficult airway: A closed claims analysis. Anesthesiology. 2005;103:33–39.
21 Cheney FW, Posner KL, Caplan RA. Adverse respiratory events infrequently leading to malpractice suits: A closed claims analysis. Anesthesiology. 1991;75:932–939.
25 Domino KB, Posner KL, Caplan RA, et al. Airway injury during anesthesia: A closed claims analysis. Anesthesiology. 1999;91:1703–1711.
28 Cheney FW, Posner KL, Lee LA, et al. Trends in anesthesia-related death and permanent brain damage: A closed claims analysis. Anesthesiology. 2006;105:1081–1086.
29 Bhananker SM, Posner KL, Cheney FW, et al. Injury and liability associated with monitored anesthesia care: A closed claims analysis. Anesthesiology. 2006;104:228–234.
1 Beecher HK, Todd DP. A study of the deaths associated with anesthesia and surgery based on a study of 599,548 anesthesias in ten institutions, 1948-1952, inclusive. Ann Surg. 1954;140:2–34.
2 Cooper JB, Newbower RS, Long CH, et al. Preventable anesthetic mishaps: A study of human factors. Anesthesiology. 1978;49:399–406.
3 Harrison GC. Death attributable to anaesthesia: A ten-year survey, 1967-1976. Br J Anaesth. 1978;50:1041–1046.
4 Holland R. Anaesthesia-related mortality in Australia. Int Anesthesiol Clin. 1984;22:61–72.
5 Keenan RL, Boyan CP. Cardiac arrest due to anesthesia: A study of incidence and causes. JAMA. 1985;253:2373–2377.
6 Russell WJ, Webb RK, Van Der Walt JH, et al. Problems with ventilation: An analysis of 2000 incident reports. Anaesth Intensive Care. 1993;21:617–620.
7 Ruth HS, Haugen FP, Grove DD. Anesthesia Study Commission: Findings of eleven years’ activity. JAMA. 1947;135:881–884.
8 Utting JE, Gray TC, Shelly FC. Human misadventure in anaesthesia. Can Anaesth Soc J. 1979;26:472–478.
9 Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients: Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324:370–376.
10 Hiatt HH, Barnes BA, Brennan TA, et al. A study of medical injury and medical malpractice: An overview. N Engl J Med. 1989;321:480–484.
11 Cheney FW. The American Society of Anesthesiologists Closed Claims Project: What have we learned, how has it affected practice, and how will it affect practice in the future? Anesthesiology. 1999;91:552–556.
12 Cheney FW, Posner K, Caplan RA, et al. Standard of care and anesthesia liability. JAMA. 1989;261:1599–1603.
13 Posner KL, Sampson PD, Caplan RA, et al. Measuring interrater reliability among multiple raters: An example of methods for nominal data. Stat Med. 1990;9:1103–1115.
14 Caplan RA, Posner KL, Ward RJ, et al. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990;72:828–833.
15 Birmingham PK, Cheney FW, Ward RJ. Esophageal intubation: A review of detection techniques. Anesth Analg. 1986;65:886–891.
16 Comroe JH, Jr., Botelho S. The unreliability of cyanosis in the recognition of arterial anoxemia. Am J Med Sci. 1947;214:1–6.
17 Coté CJ, Goldstein EA, Coté MA, et al. A single-blind study of pulse oximetry in children. Anesthesiology. 1988;68:184–188.
18 Metzner J, Posner KL, Domino KB. The risk and safety of anesthesia at remote locations: The US closed claims analysis. Curr Opin Anaesthesiol. 2009;22:502–508.
19 Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–1277.
20 Peterson GN, Domino KB, Caplan RA, et al. Management of the difficult airway: A closed claims analysis. Anesthesiology. 2005;103:33–39.
21 Cheney FW, Posner KL, Caplan RA. Adverse respiratory events infrequently leading to malpractice suits: A closed claims analysis. Anesthesiology. 1991;75:932–939.
22 Davies JM, Posner KL, Lee LA, et al. Liability associated with obstetric anesthesia: A closed claims analysis. Anesthesiology. 2009;110:131–139.
23 Olsson GL, Hallen B, Hambraeus-Jonzon K. Aspiration during anaesthesia: A computer-aided study of 185,358 anaesthetics. Acta Anaesthesiol Scand. 1986;30:84–92.
24 Warner MA, Warner ME, Weber JG. Clinical significance of pulmonary aspiration during the perioperative period. Anesthesiology. 1993;78:56–62.
25 Domino KB, Posner KL, Caplan RA, et al. Airway injury during anesthesia: A closed claims analysis. Anesthesiology. 1999;91:1703–1711.
26 Cheney FW, Domino KB, Caplan RA, et al. Nerve injury associated with anesthesia: A closed claims analysis. Anesthesiology. 1999;90:1062–1069.
27 Kroll DA, Caplan RA, Posner K, et al. Nerve injury associated with anesthesia. Anesthesiology. 1990;73:202–207.
28 Cheney FW, Posner KL, Lee LA, et al. Trends in anesthesia-related death and permanent brain damage: A closed claims analysis. Anesthesiology. 2006;105:1081–1086.
29 Bhananker SM, Posner KL, Cheney FW, et al. Injury and liability associated with monitored anesthesia care: A closed claims analysis. Anesthesiology. 2006;104:228–234.
30 ASA Committee on Ambulatory Surgical Care. Statement on respiratory monitoring during endoscopic procedures. Available at http://www.asahq.org/For-Healthcare-Professionals/Standards-Guidelines-and-Statements.aspx (accessed March 2012)
31 ASA Committee on Standards and Practice Parameters. Standards for basic anesthetic monitoring. Available at http://www.asahq.org/For-Healthcare-Professionals/Standards-Guidelines-and-Statements.aspx (accessed March 2012)