XGC cannot be confidently distinguished from gallbladder carcinoma radiologically
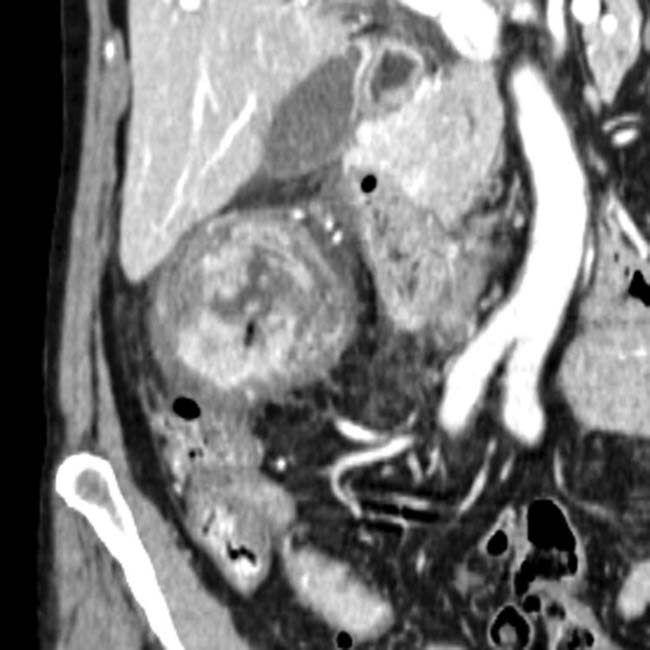
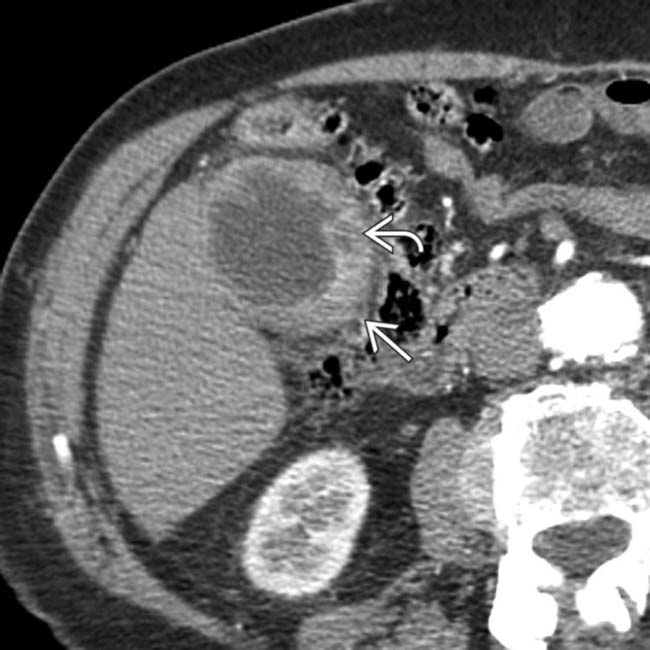
• CT: GB wall may be focally or diffusely thickened
 and an intramural abscess
and an intramural abscess  . A portion of the adjacent liver
. A portion of the adjacent liver  was resected because of the high intraoperative suspicion of GB cancer. Pathology revealed xanthogranulomatous cholecystitis (XGC).
was resected because of the high intraoperative suspicion of GB cancer. Pathology revealed xanthogranulomatous cholecystitis (XGC).
 , with an indistinct border with the liver. While the appearance was concerning for gallbladder cancer, this was found to be XGC at cholecystectomy.
, with an indistinct border with the liver. While the appearance was concerning for gallbladder cancer, this was found to be XGC at cholecystectomy.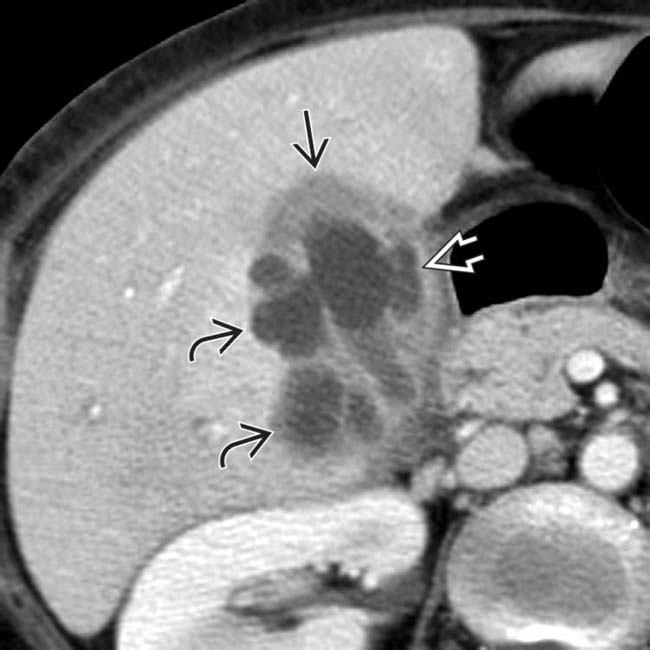
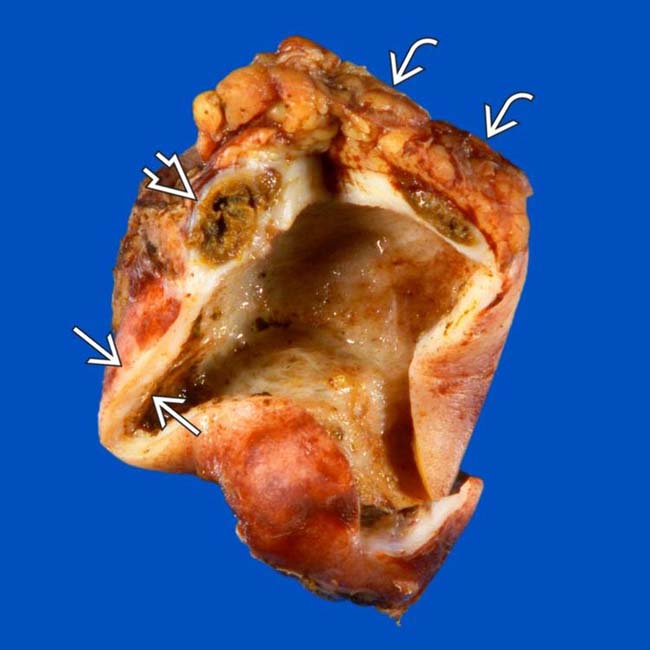
 , intramural low attenuation
, intramural low attenuation  , and several pericholecystic collections
, and several pericholecystic collections  . Low-attenuation intramural nodules in XGC are due to either abscesses or xanthogranulomas.
. Low-attenuation intramural nodules in XGC are due to either abscesses or xanthogranulomas.
 . While this was worrisome for carcinoma, XGC was confirmed at surgery.
. While this was worrisome for carcinoma, XGC was confirmed at surgery.IMAGING
General Features
CT Findings
• Imaging findings overlap with acute cholecystitis, chronic cholecystitis, and gallbladder carcinoma
 Low-attenuation intramural nodules and bands corresponding to foamy cell infiltrate and areas of necrosis/abscess
Low-attenuation intramural nodules and bands corresponding to foamy cell infiltrate and areas of necrosis/abscess
 Low-attenuation intramural nodules and bands corresponding to foamy cell infiltrate and areas of necrosis/abscess
Low-attenuation intramural nodules and bands corresponding to foamy cell infiltrate and areas of necrosis/abscess
MR Findings
• Thickened wall often demonstrates delayed enhancement on T1WI C+ with preservation of continuous mucosal enhancement
DIFFERENTIAL DIAGNOSIS
Gallbladder Carcinoma
• Unlike XGC, frequently results in obstruction of common duct, direct invasion of liver, and bulky periportal lymphadenopathy
CLINICAL ISSUES
Presentation

 and intramural low attenuation
and intramural low attenuation  .
.
 , sludge
, sludge  , and a stone within the GB neck
, and a stone within the GB neck  (and focal fatty sparing
(and focal fatty sparing  ). Preoperative differentiation between GB carcinoma and xanthogranulomatous cholecystitis (XGC) is often difficult, but the absence of ductal dilatation may suggest a chronic inflammatory process rather than neoplasia.
). Preoperative differentiation between GB carcinoma and xanthogranulomatous cholecystitis (XGC) is often difficult, but the absence of ductal dilatation may suggest a chronic inflammatory process rather than neoplasia.
 as well as focal mural low attenuation
as well as focal mural low attenuation  . At pathology, the low attenuation corresponded to an area of necrosis filled with foamy macrophages. Note the increased hepatic perfusion, representing a THAD
. At pathology, the low attenuation corresponded to an area of necrosis filled with foamy macrophages. Note the increased hepatic perfusion, representing a THAD  .
.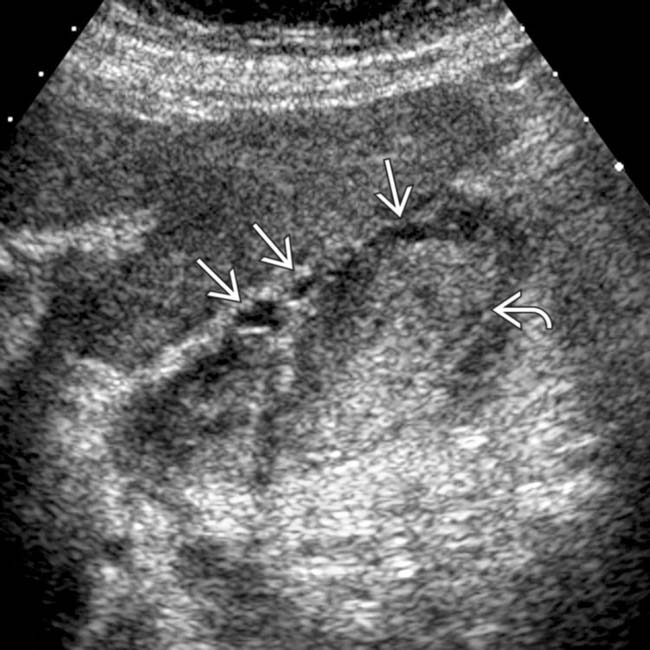
 , and sludge filling the GB lumen
, and sludge filling the GB lumen  .
.



























































 and intramural low attenuation
and intramural low attenuation  .
.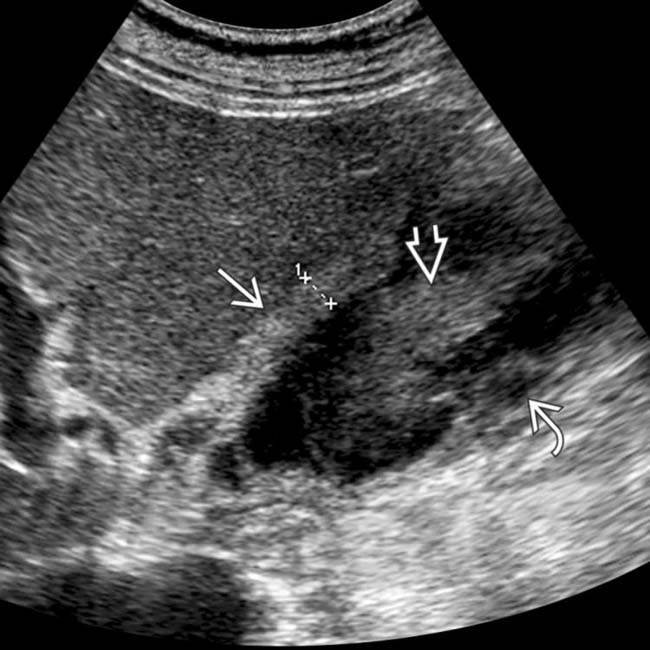
 , sludge
, sludge  , and intramural hypoechogenicity
, and intramural hypoechogenicity  . Laparoscopic cholecystectomy confirmed chronic XGC. Note that the extensive adhesions and wall thickening associated with chronic inflammation often necessitate open cholecystectomy.
. Laparoscopic cholecystectomy confirmed chronic XGC. Note that the extensive adhesions and wall thickening associated with chronic inflammation often necessitate open cholecystectomy.