Variably distributed (diffuse, lobar, or segmental)
 Enhancing “dot” (portal radicles) at either center or periphery of dilated duct: Central dot sign on CECT
Enhancing “dot” (portal radicles) at either center or periphery of dilated duct: Central dot sign on CECT• ERCP: Dilatation (usually saccular) of large intrahepatic ducts with alternating biliary strictures
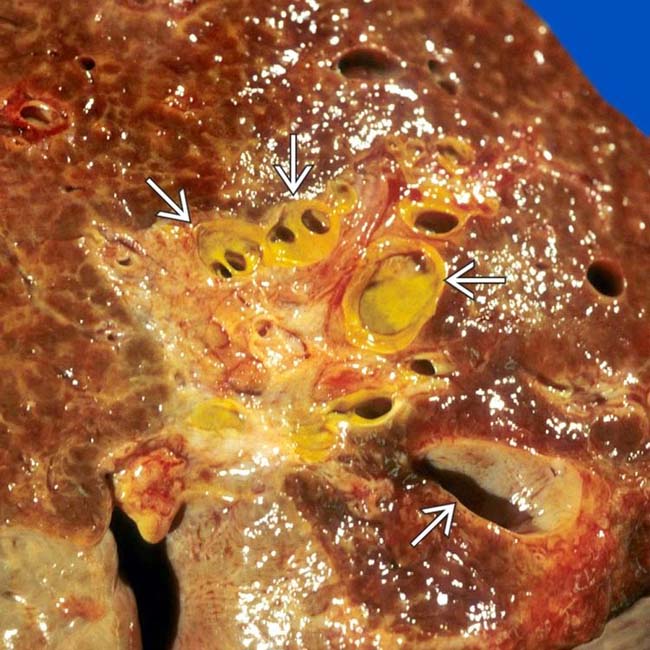
 in a patient with Caroli disease. (Courtesy J. Misdraji, MD.)
in a patient with Caroli disease. (Courtesy J. Misdraji, MD.)
 , a characteristic constellation of findings in Caroli disease.
, a characteristic constellation of findings in Caroli disease.
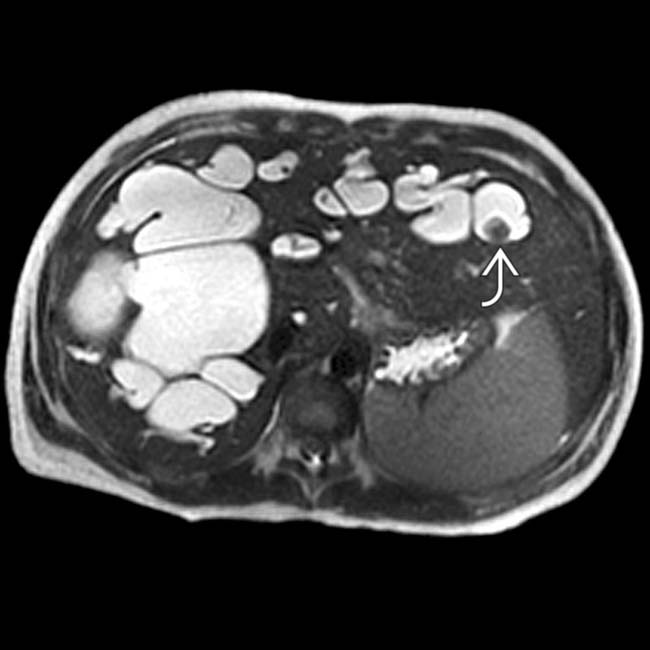
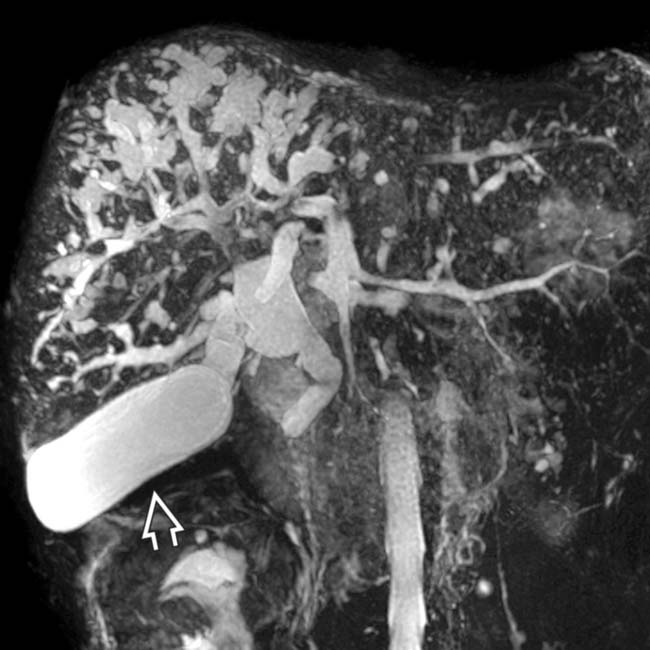
 with the biliary tree, compatible with Caroli disease. The gallbladder is also seen
with the biliary tree, compatible with Caroli disease. The gallbladder is also seen  . This patient was treated with liver transplantation.
. This patient was treated with liver transplantation.IMAGING
General Features
• Morphology
 Segmental saccular dilatation of large intrahepatic bile ducts separated by normal or dilated bile ducts
Segmental saccular dilatation of large intrahepatic bile ducts separated by normal or dilated bile ducts
 Segmental saccular dilatation of large intrahepatic bile ducts separated by normal or dilated bile ducts
Segmental saccular dilatation of large intrahepatic bile ducts separated by normal or dilated bile ducts
MR Findings
• T1 hypointense, T2 hyperintense, nonenhancing cysts variably distributed in liver
 Due to communication with biliary tree, cysts fill with contrast in hepatobiliary phase when using hepatobiliary contrast agent (e.g., gadoxetate [Eovist])
Due to communication with biliary tree, cysts fill with contrast in hepatobiliary phase when using hepatobiliary contrast agent (e.g., gadoxetate [Eovist])
 Due to communication with biliary tree, cysts fill with contrast in hepatobiliary phase when using hepatobiliary contrast agent (e.g., gadoxetate [Eovist])
Due to communication with biliary tree, cysts fill with contrast in hepatobiliary phase when using hepatobiliary contrast agent (e.g., gadoxetate [Eovist])Ultrasonographic Findings
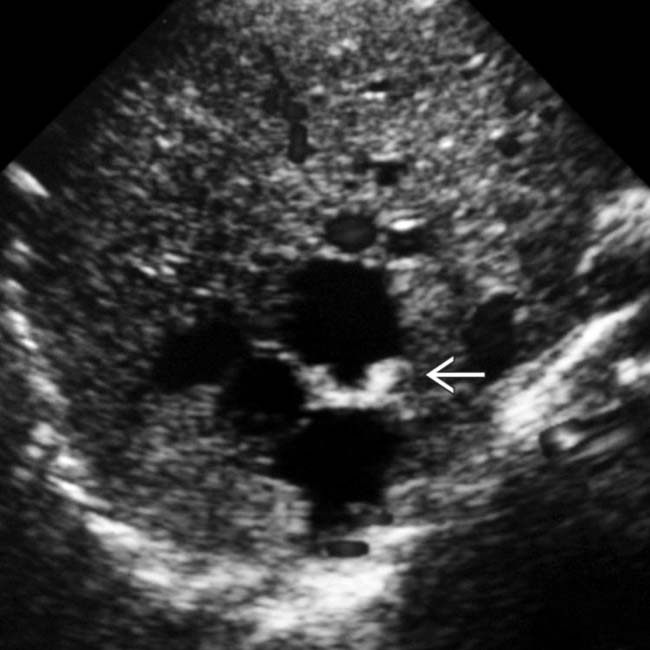
• Dilated intrahepatic bile ducts: Communication between cysts and biliary tree may be difficult to demonstrate on US
• Echogenic septa may completely or incompletely traverse dilated lumen of bile ducts (intraductal bridging sign)
• Small portal venous branches may be partially or completely surrounded by dilated IHBD (US correlate of central dot sign
DIFFERENTIAL DIAGNOSIS
AD Polycystic Hepatic Disease
Recurrent Pyogenic Cholangitis
• Disease characterized by formation of pigment stones throughout biliary tree, with resultant biliary strictures and repeated bouts of cholangitis
• Dilatation of both intra- and extrahepatic bile ducts, usually of cylindrical morphology (not saccular)
PATHOLOGY
General Features
• Etiology
• Genetics
• Embryological anatomy
 Ductal plate malformation: Incomplete remodeling of ductal plate leading to persistence of embryonic biliary ductal structures
Ductal plate malformation: Incomplete remodeling of ductal plate leading to persistence of embryonic biliary ductal structures
 Ductal plate malformation: Incomplete remodeling of ductal plate leading to persistence of embryonic biliary ductal structures
Ductal plate malformation: Incomplete remodeling of ductal plate leading to persistence of embryonic biliary ductal structuresCLINICAL ISSUES
Presentation
• Most common signs/symptoms

 , a classic imaging finding in Caroli disease.
, a classic imaging finding in Caroli disease.
 . Hepatic and renal fibrosis was the cause of liver and renal failure and portal hypertension in this patient.
. Hepatic and renal fibrosis was the cause of liver and renal failure and portal hypertension in this patient.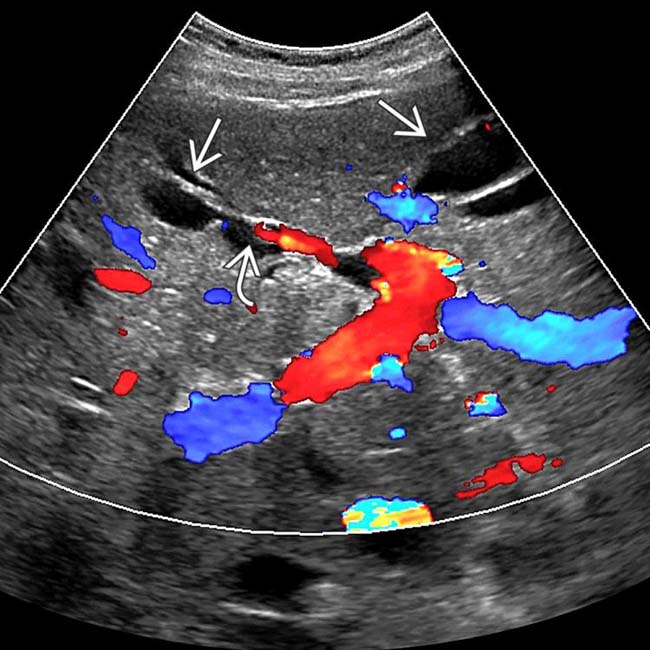
 . Note eccentric color Doppler “dot” within the medial segmental branch of the left duct
. Note eccentric color Doppler “dot” within the medial segmental branch of the left duct  , similar to the central dot sign more commonly described on CT or MR.
, similar to the central dot sign more commonly described on CT or MR.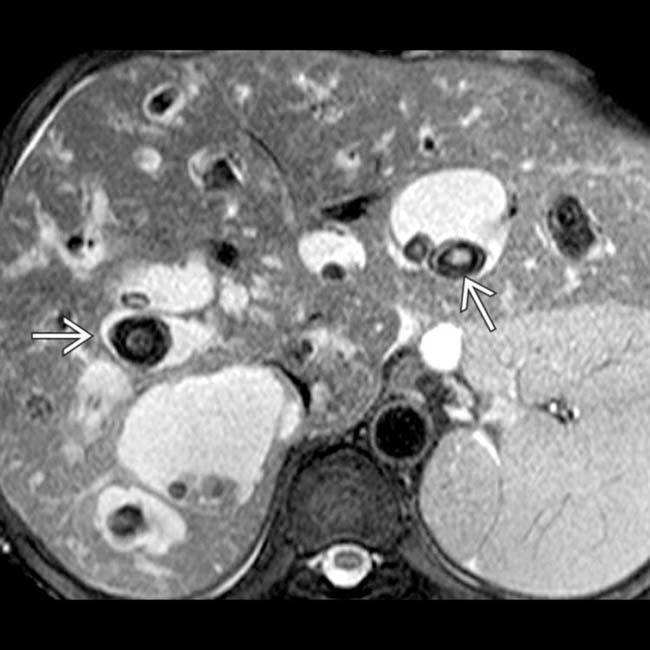
 .
.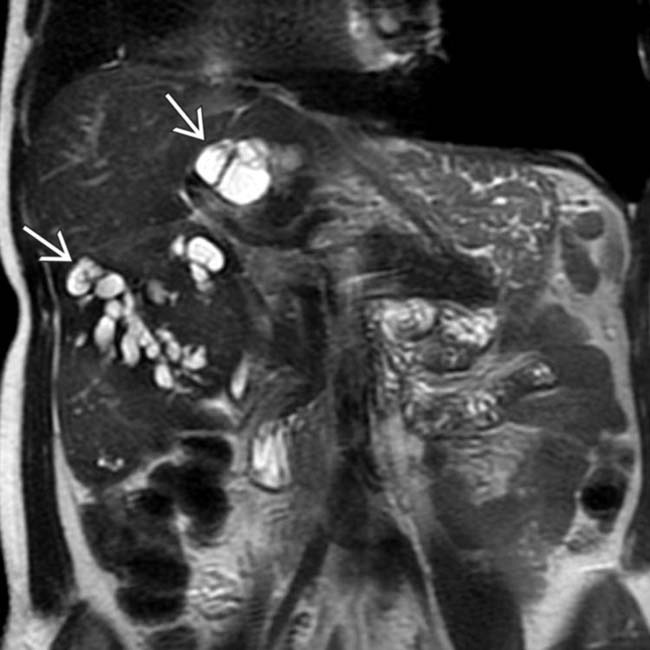
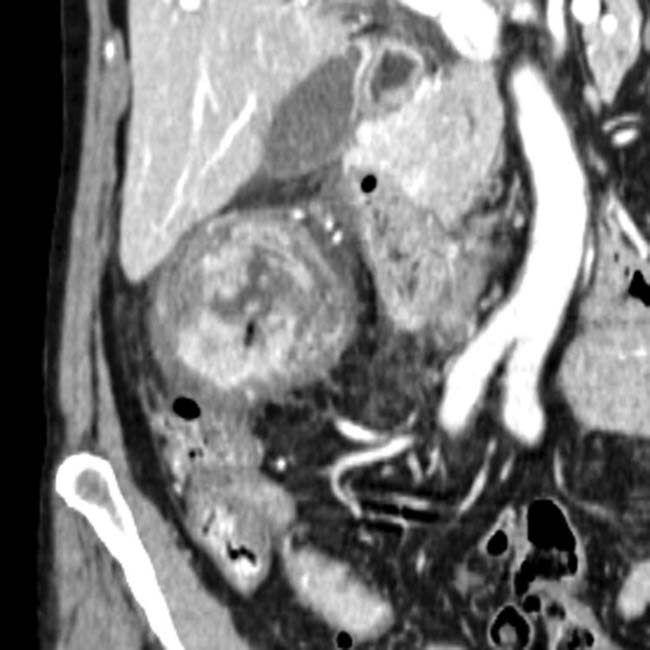
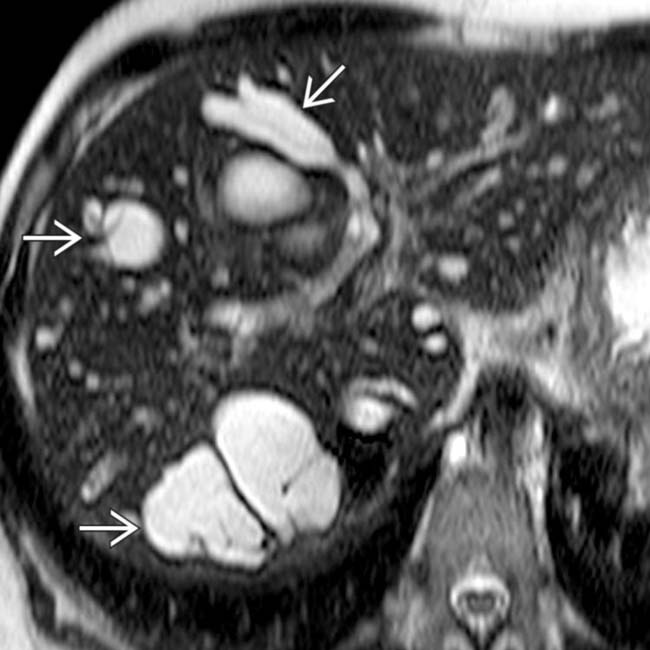
 predominantly in the right hepatic lobe which communicate with the biliary tree, compatible with Caroli syndrome.
predominantly in the right hepatic lobe which communicate with the biliary tree, compatible with Caroli syndrome.
 of multiple ducts in the right hepatic lobe. Note the diffusely low attenuation of the parenchyma in the involved portions of the liver, likely on the basis of hepatic fibrosis and edema from cholangitis.
of multiple ducts in the right hepatic lobe. Note the diffusely low attenuation of the parenchyma in the involved portions of the liver, likely on the basis of hepatic fibrosis and edema from cholangitis.
 .
.
 of many intrahepatic ducts, many of which contain low signal intensity calculi
of many intrahepatic ducts, many of which contain low signal intensity calculi  in this patient with Caroli disease.
in this patient with Caroli disease.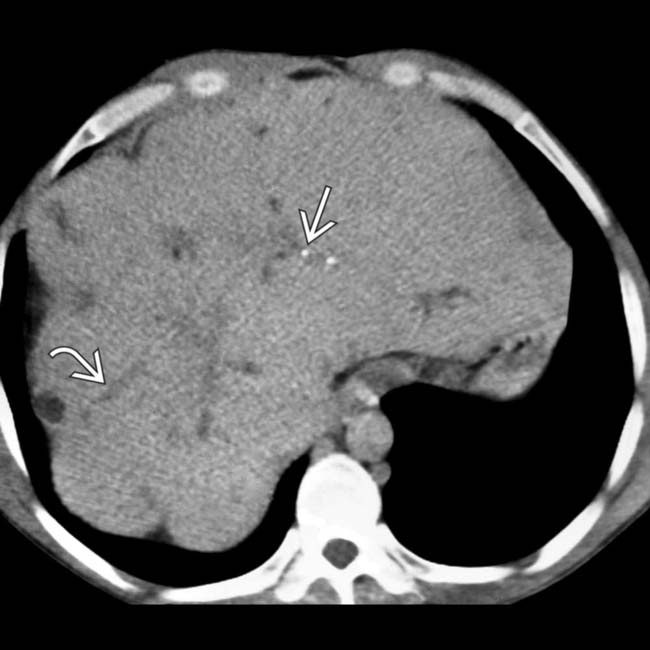
 are irregularly dilated and contain calculi
are irregularly dilated and contain calculi  .
.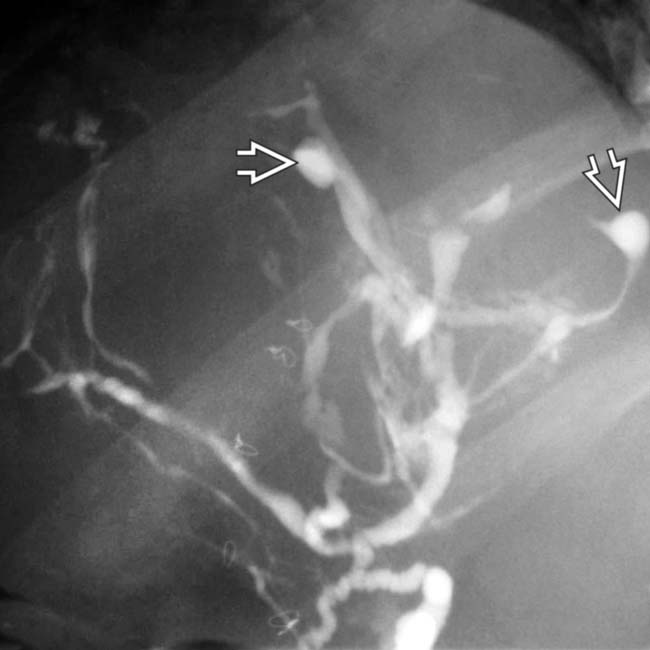
 of the intrahepatic ducts (Caroli disease) with distortion and displacement of the ducts, probably due to the congenital hepatic fibrosis.
of the intrahepatic ducts (Caroli disease) with distortion and displacement of the ducts, probably due to the congenital hepatic fibrosis.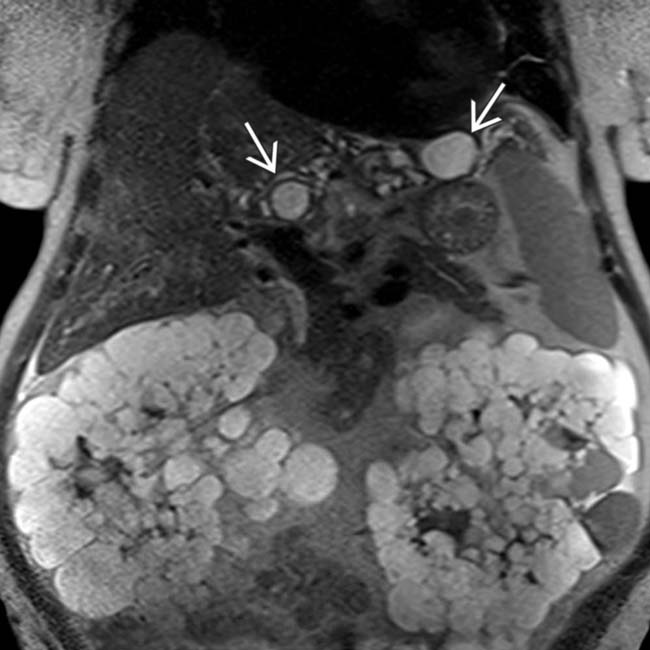
 clustered in the left hepatic lobe in a patient with Caroli syndrome. Note the cystic replacement of the kidneys due to concurrent autosomal dominant polycystic kidney syndrome.
clustered in the left hepatic lobe in a patient with Caroli syndrome. Note the cystic replacement of the kidneys due to concurrent autosomal dominant polycystic kidney syndrome.
 and innumerable, coalescent hyperintense biliary hamartomas
and innumerable, coalescent hyperintense biliary hamartomas  .
.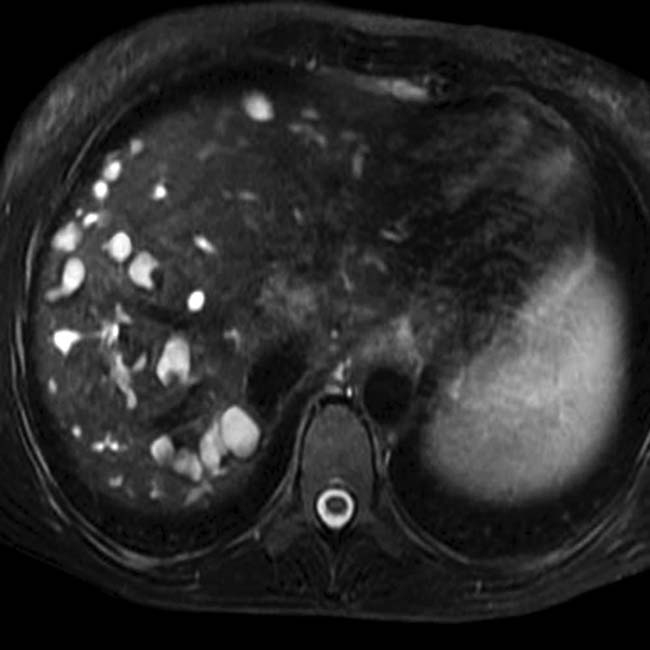
 . Ductal dilatation extends to the periphery of the liver.
. Ductal dilatation extends to the periphery of the liver.
 . Note the end-stage kidneys
. Note the end-stage kidneys  , all findings are due to congenital fibropolycystic disease of the liver and kidneys.
, all findings are due to congenital fibropolycystic disease of the liver and kidneys.
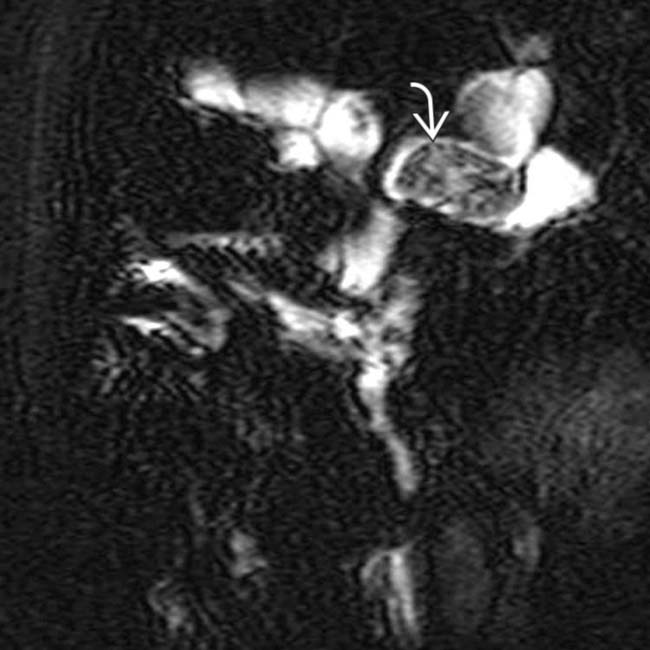
 , representing the portal triads.
, representing the portal triads.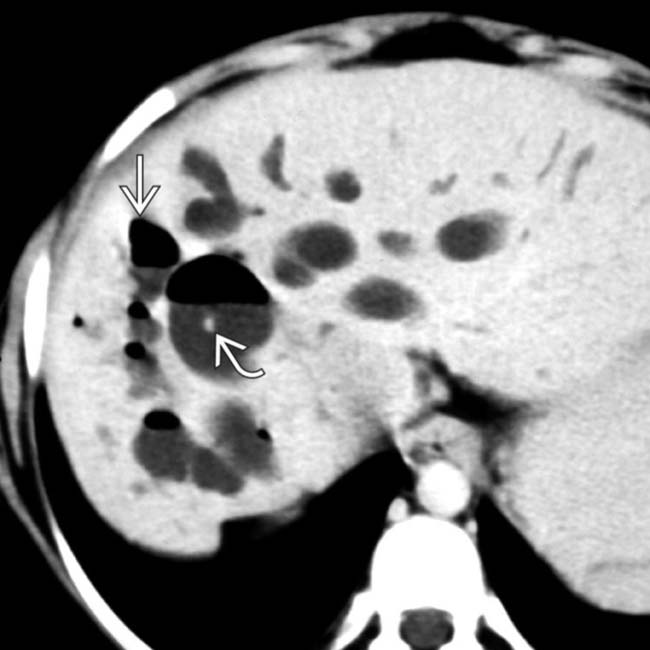
 , and others exhibit the “central dot” sign
, and others exhibit the “central dot” sign  .
.
 within 1 of the cystic spaces noted in the right lobe. This is the “central dot” sign, with dilated bile ducts wrapped around. Also note the enlarged spleen and renal allograft
within 1 of the cystic spaces noted in the right lobe. This is the “central dot” sign, with dilated bile ducts wrapped around. Also note the enlarged spleen and renal allograft  .
.






 .
.











































































 .
.
 .
.