Wrist and hand
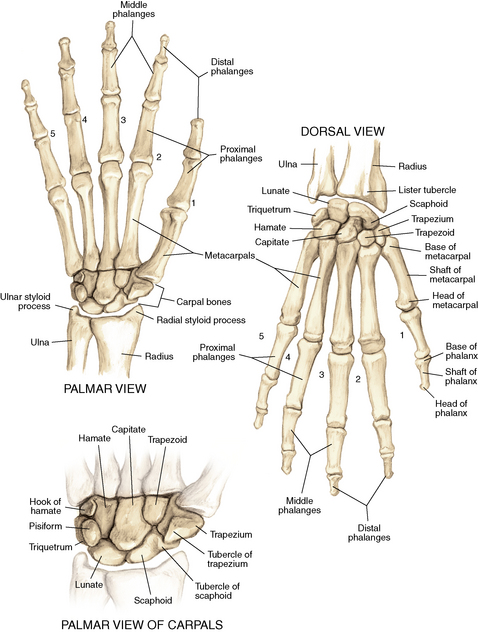
Anatomy
Ligaments: Figure 4-2
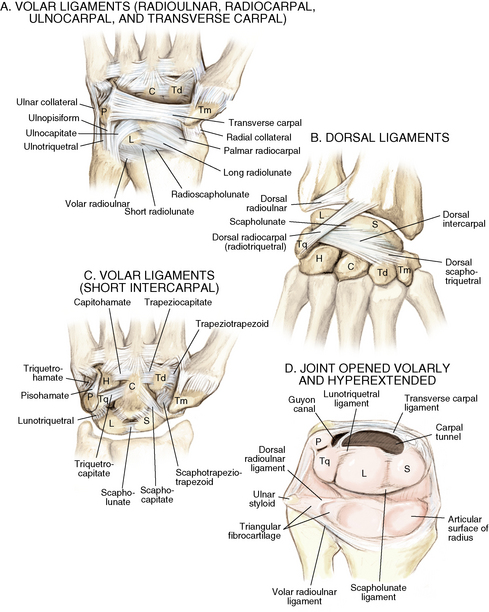
Figure 4-2. A to D, Ligaments of the wrist. Ca, capitate; H, hamate; L, lunate; P, pisiform; S, scaphoid; Td, trapezoid; Tm, trapezium; Tq, triquetrum. (From Chhabra AB: Wrist and hand. In Miller MD, Chhabra AB, Hurwitz S, et al, editors: Orthopaedic surgical approaches, Philadelphia, 2008, Saunders, p 150.)
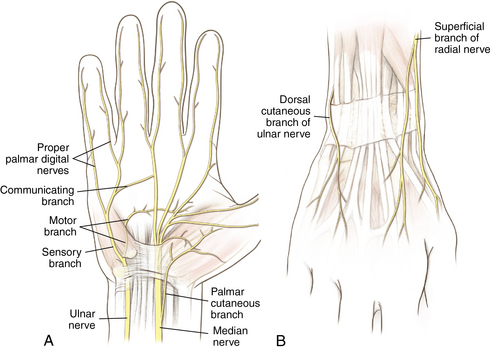
Muscles and tendons: Figures 4-3 through 4-7
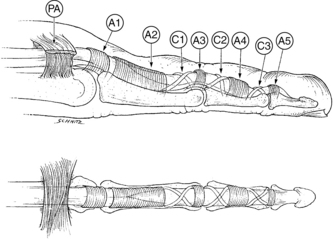
Figure 4-3. Flexor tendon pulley system.
A1 to A5, annular pulleys; C1 to C3, cruciate pulleys; PA, palmar aponeurosis. (From Strickland JW: Flexor tendons: acute injuries. In Green DP, editor: Operative hand surgery, ed 4, New York, 1999, Churchill Livingstone, p 1853.)
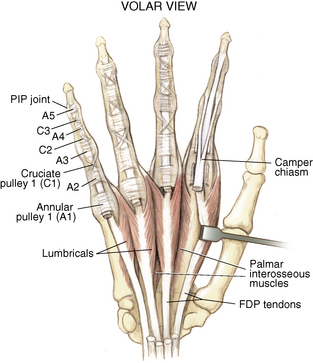
Figure 4-4. Volar muscles of the hand: lumbricals and palmar interossei. FDP, flexor digitorum profundus; PIP, proximal interphalangeal. (From Chhabra AB: Wrist and hand. In Miller MD, Chhabra AB, Hurwitz S, et al, editors: Orthopaedic surgical approaches, Philadelphia, 2008, Saunders, p 154.)
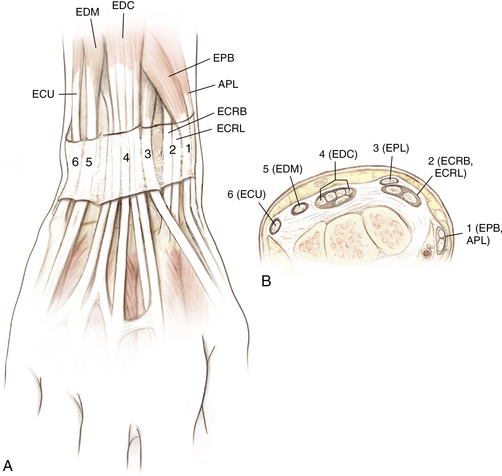
Figure 4-6. A and B, Extensor tendon compartments of wrist. APL, abductor pollicis longus; ECRB, extensor carpi radialis brevis; ECRL, extensor carpi radialis longus; ECU, extensor carpi ulnaris; EDC, extensor digitorum communis; EDM, extensor digiti minimi. (From Chhabra AB: Wrist and hand. In Miller MD, Chhabra AB, Hurwitz S, et al, editors: Orthopaedic surgical approaches, Philadelphia, 2008, Saunders, p 157.)
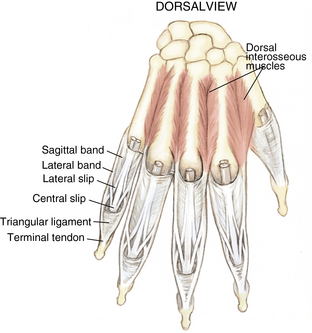
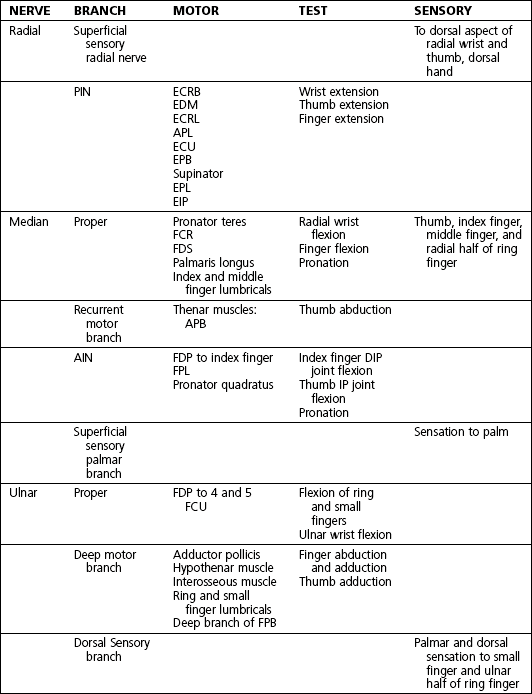
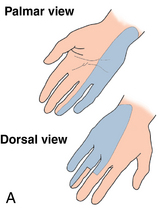
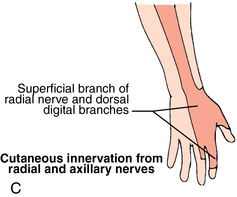
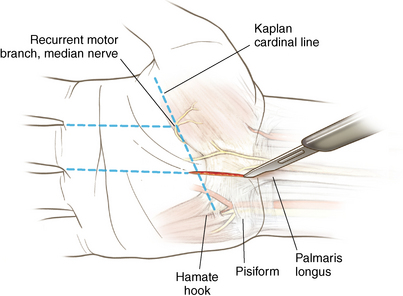
Nerves and arteries: Figures 4-8 through 4-10 and table 4-1
Surface anatomy: Figure 4-11
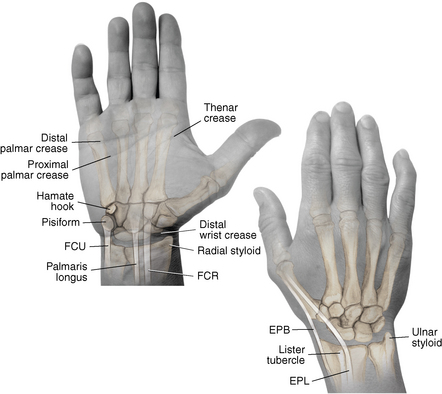
Figure 4-11. Surface anatomy of the hand and wrist.
EPB, extensor pollicis brevis; EPL, extensor pollicis longus; FCR, flexor carpi radialis; FCU, flexor carpi ulnaris. (From Chhabra AB: Wrist and hand. In Miller MD, Chhabra AB, Hurwitz S, et al, editors: Orthopaedic surgical approaches, Philadelphia, 2008, Saunders, p 163.)
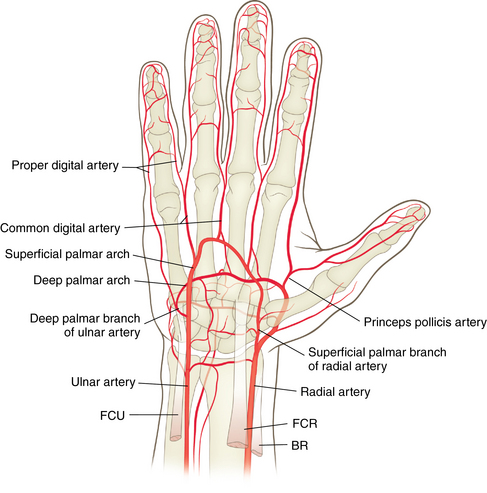
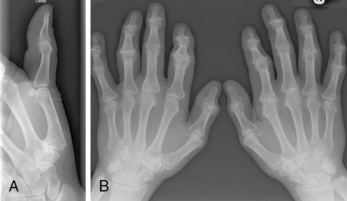
Normal radiographic appearance: Figures 4-12 through 4-14
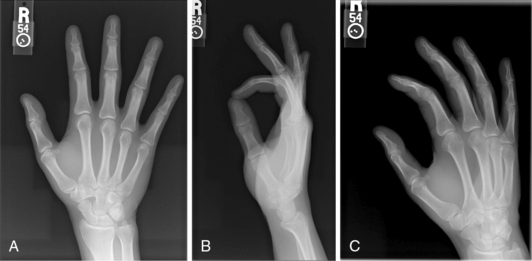
Figure 4-12. Normal radiographs of the hand.
Anteroposterior (A), lateral (B), and oblique (C) views of the hand. (From Hart JA: Overview of the wrist and hand. In Miller MD, Hart JA, MacKnight JM, editors: Essential orthopaedics, Philadelphia, 2010, Saunders, p 303.)
Physical examination
Inspect for scars, muscle atrophy, edema, erythema or deformity.
Palpate specific structures to evaluate complaint:
• Distal radioulnar joint (DRUJ)
• Anatomic snuffbox, scaphoid tubercle
• First extensor compartment, extensor carpi radialis ulnaris, extensor carpi radialis brevis, extensor carpi radialis longus
• Scapholunate (SL) interval (approximately 1 to 3 cm distal from Lister tubercle)
• First carpometacarpal (CMC) joint
• Flexor carpi ulnaris (FCU) tendon
• Extensor carpi ulnaris (ECU) tendon
Normal wrist range of motion (ROM): Table 4-2
Table 4-2.
| Extension | 80 degrees |
| Flexion | 70 degrees |
| Supination | 90 degrees |
| Pronation | 90 degrees |
| Ulnar deviation | 30 degrees |
| Radial deviation | 20 degrees |
Neurovascular examination of the wrist and hand: Table 4-3
Table 4-3.
Neurovascular Examination of the Wrist and Hand
| NERVE | LOCATION OF TEST | TESTS |
| Median nerve | Carpal tunnel | Tinel, Phalen, Durkan test (see page 140) |
| Ulnar nerve | Guyon canal/medial epicondyle | Tinel test |
| Superficial sensory radial nerve | At radial styloid | Tinel test |
| Radial and ulnar artery | At volar wrist | Allen test for dominance or perfusion |
Differential diagnosis of wrist pain: Table 4-4
Table 4-4.
Differential Diagnosis of Wrist Pain
| Radial-sided wrist pain | Distal radius fracture SLL tear Arthritis Scaphoid fracture Extensor tendinitis de Quervain tenosynovitis |
| Ulnar-sided wrist pain | TFCC tear FCU tendinitis Ulnar artery thrombosis Cubital tunnel syndrome Pisotriquetral arthritis ECU tendinitis Distal ulnar fracture Lunotriquetral tear Hook hamate fracture |
| Dorsal wrist pain | Extensor tendinitis Arthritis SLL tear Scaphoid fracture |
| Volar wrist pain | FCU or FCR tendinitis Carpal tunnel syndrome |
Scaphoid fracture
Differential diagnosis
 SL ligament (SLL) injury (see page 129)
SL ligament (SLL) injury (see page 129)
 First extensor compartment tendinitis
First extensor compartment tendinitis
 Occult scaphoid fracture: If there is high level of suspicion for a scaphoid fracture but the initial radiographic findings are negative, place the patient into a thumb spica splint and obtain radiographs again at 3 weeks after injury. If follow-up radiographic findings are negative but patient is still symptomatic, order a magnetic resonance imaging (MRI) scan to evaluate for occult scaphoid fracture or SLL tear.
Occult scaphoid fracture: If there is high level of suspicion for a scaphoid fracture but the initial radiographic findings are negative, place the patient into a thumb spica splint and obtain radiographs again at 3 weeks after injury. If follow-up radiographic findings are negative but patient is still symptomatic, order a magnetic resonance imaging (MRI) scan to evaluate for occult scaphoid fracture or SLL tear.
Treatment options
 Conservative management is reserved for nondisplaced fractures in which patient declines surgery or for patients too ill for surgery.
Conservative management is reserved for nondisplaced fractures in which patient declines surgery or for patients too ill for surgery.
 Nondisplaced waist fractures have an 88% to 95% healing rate if treated within 3 weeks of injury.
Nondisplaced waist fractures have an 88% to 95% healing rate if treated within 3 weeks of injury.
 A short-arm thumb spica cast is used for a total of 8 to 12 weeks, depending on healing (some argue for long-arm cast).
A short-arm thumb spica cast is used for a total of 8 to 12 weeks, depending on healing (some argue for long-arm cast).
 See the patient in follow-up at 4-week intervals to change the cast, obtain repeat radiographs of the fracture, and assess healing.
See the patient in follow-up at 4-week intervals to change the cast, obtain repeat radiographs of the fracture, and assess healing.
 A computed tomography (CT) scan may be necessary to confirm healing after 8 to 12 weeks.
A computed tomography (CT) scan may be necessary to confirm healing after 8 to 12 weeks.
 The fracture is considered healed if there is radiographic evidence of healing and patient is nontender to palpation at the anatomic snuffbox and scaphoid tubercle or if a CT scan confirms healing.
The fracture is considered healed if there is radiographic evidence of healing and patient is nontender to palpation at the anatomic snuffbox and scaphoid tubercle or if a CT scan confirms healing.
Operative management of acute scaphoid fractures
Informed consent and counseling
 Even with appropriate treatment and good surgical fixation, the rate of nonunion is 5% because of the scaphoid’s tenuous blood supply. Proximal pole scaphoid fractures have the highest incidence of non-union.
Even with appropriate treatment and good surgical fixation, the rate of nonunion is 5% because of the scaphoid’s tenuous blood supply. Proximal pole scaphoid fractures have the highest incidence of non-union.
 Smoking cessation is imperative for fracture healing.
Smoking cessation is imperative for fracture healing.
 The patient can expect to be immobilized for approximately 6 weeks, although the type of immobilization depends on the surgeon’s preference and on fracture fixation.
The patient can expect to be immobilized for approximately 6 weeks, although the type of immobilization depends on the surgeon’s preference and on fracture fixation.
 The patient will require approximately 2 months of outpatient hand therapy to restore motion and strength.
The patient will require approximately 2 months of outpatient hand therapy to restore motion and strength.
Surgical procedures
 Dorsal approach for proximal pole fractures
Dorsal approach for proximal pole fractures
 Volar approach for distal pole and waist fractures
Volar approach for distal pole and waist fractures
 For either approach, placement of a forearm-based thumb spica splint
For either approach, placement of a forearm-based thumb spica splint
Open reduction, internal fixation
 Hardware consists of a cannulated headless compression screw and multiple wires.
Hardware consists of a cannulated headless compression screw and multiple wires.
 Dorsal approach: A small longitudinal incision is made over the proximal pole of the scaphoid. Avoid the superficial sensory radial nerve.
Dorsal approach: A small longitudinal incision is made over the proximal pole of the scaphoid. Avoid the superficial sensory radial nerve.
 Volar approach: A small incision is made over the scaphoid tubercle. Avoid the radial artery during exposure.
Volar approach: A small incision is made over the scaphoid tubercle. Avoid the radial artery during exposure.
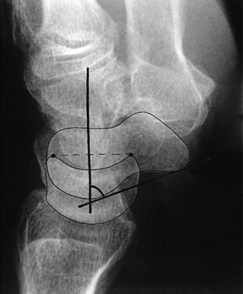
Percutaneous internal fixation: Figure 4-16
 This technique may be used preferentially for nondisplaced scaphoid fractures. The procedure is similar to the open technique, just performed percutaneously. With the patient’s wrist flexed, a guidewire is placed down the central axis of the scaphoid. The guidewire is also used to measure the appropriate screw length. After fluoroscopic confirmation of adequate reduction, a screw is placed for fixation. Place the patient in a thumb spica splint following surgery.
This technique may be used preferentially for nondisplaced scaphoid fractures. The procedure is similar to the open technique, just performed percutaneously. With the patient’s wrist flexed, a guidewire is placed down the central axis of the scaphoid. The guidewire is also used to measure the appropriate screw length. After fluoroscopic confirmation of adequate reduction, a screw is placed for fixation. Place the patient in a thumb spica splint following surgery.
Estimated postoperative course
• Sutures are removed, and a wound check is performed.
• Radiographs consist of wrist PA, lateral, oblique, and navicular views.
• Immobilization: The patient is placed into a removable thumb spica splint.
• Therapy referral: Start edema control and gentle finger and wrist ROM only.
• Note: Some surgeons prefer cast immobilization in a thumb spica cast during the initial postoperative period, especially if the fracture was difficult to reduce or especially comminuted.
• The patient returns for a motion check.
• Radiographs consist of wrist PA, lateral, and scaphoid views.
• Therapy: If healing is present, progress therapy to more aggressive wrist ROM, wean from the splint, and start gradual weight bearing.
• If no healing is noted, continue gentle ROM and have the patient wear the brace at all times until healing is evident on radiographs.
• The patient returns for a motion check.
• Assess for tenderness at the anatomic snuffbox and scaphoid tubercle.
• Radiographs consist of wrist PA, lateral, and scaphoid views.
• If the injury is healed and no pain is noted on examination, release the patient to regular activities without restrictions.
• If no evidence of healing is seen on radiographs, consider use of a bone stimulator and possibly obtain a CT scan to evaluate for healing.
• Nonunion occurs if there has been no healing by 6 months postoperatively.
Distal radius fractures
Classification
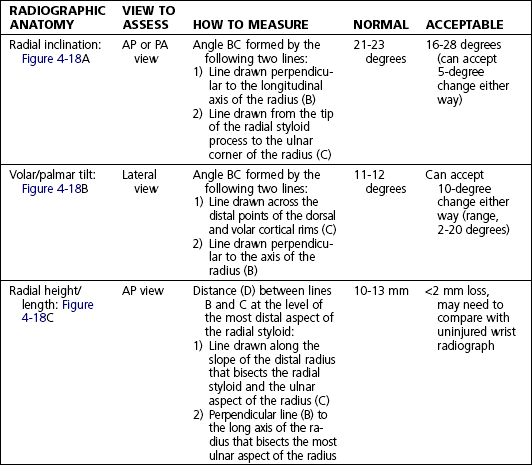
Describe the fracture in terms of displacement, comminution, radial length, surface tilt, and articular step-off (Figure 4-18 and Table 4-6).
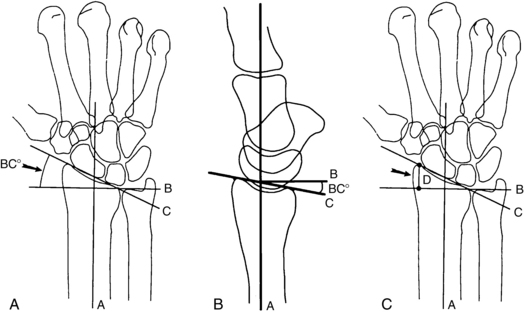
Figure 4-18. How to determine whether a distal radius fracture meets operative criteria. A, Radial inclination. B, Volar tilt. C, Radial height. (Adapted from Baratz ME, Larsen CF. Wrist and hand measurements and classification schemes. In Gilula LA, Yin Y (eds). Imaging of the wrist and hand, Philadelphia, Saunders, 1996.)
Initial treatment
 The distal radius is the most commonly fractured bone in the arm. The fracture pattern determines surgical versus nonsurgical treatment. If the fracture is nondisplaced or if the fracture has been successfully closed reduced and splinted and the fingers are sensate with good perfusion, then the injury can wait several days for evaluation by an orthopaedist. If the patient’s fingers are numb and/or not well perfused or the fracture is not able to be reduced, the patient should have an immediate surgical evaluation.
The distal radius is the most commonly fractured bone in the arm. The fracture pattern determines surgical versus nonsurgical treatment. If the fracture is nondisplaced or if the fracture has been successfully closed reduced and splinted and the fingers are sensate with good perfusion, then the injury can wait several days for evaluation by an orthopaedist. If the patient’s fingers are numb and/or not well perfused or the fracture is not able to be reduced, the patient should have an immediate surgical evaluation.
Treatment options
 Conservative management is reserved for nondisplaced fractures or stable reduced fractures or for patients too ill for surgery.
Conservative management is reserved for nondisplaced fractures or stable reduced fractures or for patients too ill for surgery.
 Nondisplaced fractures require casting for 6 to 8 weeks in a short-arm cast.
Nondisplaced fractures require casting for 6 to 8 weeks in a short-arm cast.
 Generally, after 6 weeks of immobilization, patients may progress with ROM.
Generally, after 6 weeks of immobilization, patients may progress with ROM.
• Stable reduced fractures require 3 weeks in a sugar tong splint with weekly radiographs in the splint to ensure that fracture alignment is maintained. If the reduction is lost, surgery is recommended. If fracture reduction is maintained for 3 weeks, transition the patient to a short-arm cast with radiographs immediately following new cast placement to ensure alignment.
• The fracture is considered healed if there is radiographic evidence of healing and the patient is nontender over the distal radius. This usually occurs in approximately 2 to 3 months, depending on the severity of the original injury.
Operative management of acute distal radius fractures
Codes
Informed consent and counseling
 Smoking cessation is important for fracture healing.
Smoking cessation is important for fracture healing.
 The patient can expect to be immobilized for approximately 6 weeks, but the type of immobilization depends on the surgeon’s preference and on fracture fixation.
The patient can expect to be immobilized for approximately 6 weeks, but the type of immobilization depends on the surgeon’s preference and on fracture fixation.
 The patient may require several sessions of outpatient hand therapy to restore motion and strength.
The patient may require several sessions of outpatient hand therapy to restore motion and strength.
Surgical procedures
Open reduction, internal fixation: See figure 4-19
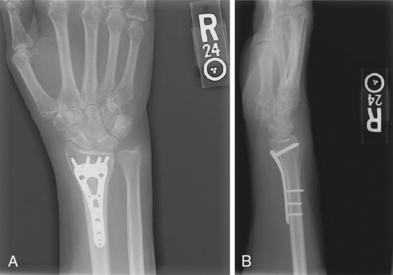
Figure 4-19. Surgical fixation of a displaced distal radius fracture with a volar locking plate. Posteroanterior (A) and lateral (B) views.
 Hardware consists of a volar plate and screws.
Hardware consists of a volar plate and screws.
 Volar approach: A longitudinal incision is made directly superficial to the flexor carpi radialis (FCR) tendon. An interval is developed between the FCR and the radial artery. Blunt deep dissection is carried down to the pronator quadratus muscle, which is sharply incised on the radial border and elevated off the periosteum of the radius to expose the fracture. Sometimes the brachioradialis tendon insertion must be released to decrease the deforming forces on the fracture. A volar plate and screws are used, and intraoperative fluoroscopy confirms reduction and hardware placement. The patient is placed in a volar short-arm splint postoperatively.
Volar approach: A longitudinal incision is made directly superficial to the flexor carpi radialis (FCR) tendon. An interval is developed between the FCR and the radial artery. Blunt deep dissection is carried down to the pronator quadratus muscle, which is sharply incised on the radial border and elevated off the periosteum of the radius to expose the fracture. Sometimes the brachioradialis tendon insertion must be released to decrease the deforming forces on the fracture. A volar plate and screws are used, and intraoperative fluoroscopy confirms reduction and hardware placement. The patient is placed in a volar short-arm splint postoperatively.
Estimated postoperative course
• Sutures are removed, and a wound check is performed.
• Possible radiographs include wrist PA, lateral, and oblique views.
• Immobilization: The patient is placed into a removable spica splint.
• Therapy referral: Start edema control and gentle finger and wrist motion only. Some clinicians start therapy at 3 to 5 days postoperatively.
• Note: Some surgeons prefer cast immobilization in a short-arm cast during the initial postoperative period, especially if the fracture was difficult to reduce or especially comminuted.
Trigger finger
Physical examination
 Tenderness to palpation directly over the A1 pulley, located at the volar base of each finger just proximal to the metacarpophalangeal (MCP) joint flexion crease
Tenderness to palpation directly over the A1 pulley, located at the volar base of each finger just proximal to the metacarpophalangeal (MCP) joint flexion crease
 Palpable or visible locking or catching with flexion (the examiner may need to flex the finger, including the distal interphalangeal [DIP] joint, passively to reproduce triggering)
Palpable or visible locking or catching with flexion (the examiner may need to flex the finger, including the distal interphalangeal [DIP] joint, passively to reproduce triggering)
 Palpable nodularity on the flexor tendon at the level of the A1 pulley
Palpable nodularity on the flexor tendon at the level of the A1 pulley
Initial treatment
 Triggering may affect more than one digit, with a higher incidence in patients with diabetes and thyroid disease. There is about an 80% cure rate after the first cortisone injection; if the first injection is unsuccessful, a second injection may be done 3 to 6 weeks later. If triggering is still present after the second injection, consider surgical intervention.
Triggering may affect more than one digit, with a higher incidence in patients with diabetes and thyroid disease. There is about an 80% cure rate after the first cortisone injection; if the first injection is unsuccessful, a second injection may be done 3 to 6 weeks later. If triggering is still present after the second injection, consider surgical intervention.
Treatment options
Operative management
Informed consent and counseling
 The patient will have sutures in place for 10 to 14 days.
The patient will have sutures in place for 10 to 14 days.
 The patient will likely be able to move the finger immediately following surgery.
The patient will likely be able to move the finger immediately following surgery.
 Depending on the surgeon’s preference, the patient may require one to two sessions of outpatient hand therapy.
Depending on the surgeon’s preference, the patient may require one to two sessions of outpatient hand therapy.
 Wound sensitivity may occur postoperatively, but it usually improves with time.
Wound sensitivity may occur postoperatively, but it usually improves with time.
Surgical procedures
 Local anesthetic can be injected before the skin incision is made.
Local anesthetic can be injected before the skin incision is made.
 A small, transverse incision is made over the level of the A1 pulley.
A small, transverse incision is made over the level of the A1 pulley.
 The skin and subcutaneous tissues are incised to expose the flexor tendon sheath.
The skin and subcutaneous tissues are incised to expose the flexor tendon sheath.
 Identify and protect the neurovascular bundles.
Identify and protect the neurovascular bundles.
 Identify and release the A1 pulley in its entirety.
Identify and release the A1 pulley in its entirety.
 Preserve the A2 pulley to prevent bowstringing.
Preserve the A2 pulley to prevent bowstringing.
 Local anesthesia is used so that the patient can actively flex and extend the digit following A1 pulley release, thus confirming successful release of the pulley.
Local anesthesia is used so that the patient can actively flex and extend the digit following A1 pulley release, thus confirming successful release of the pulley.
 Place the patient in a soft hand dressing following surgery.
Place the patient in a soft hand dressing following surgery.
Estimated postoperative course
Scapholunate ligament tear
Physical examination
 Tenderness to palpation at the SL interval (palpated on the dorsal wrist approximately 1 to 3 cm distal to Lister tubercle)
Tenderness to palpation at the SL interval (palpated on the dorsal wrist approximately 1 to 3 cm distal to Lister tubercle)
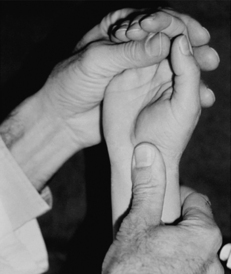
 Positive Watson maneuver (Fig. 4-21)
Positive Watson maneuver (Fig. 4-21)
• Watson maneuver tests for SLL instability. The examiner places his or her thumb firmly on the patient’s volar wrist over the scaphoid tubercle and applies pressure. With the other hand, the examiner moves the patient’s wrist from ulnar to radial deviation. A positive test result occurs when there is a palpable “clunk” with pain. The presence of a clunk alone is not a positive test result.
• The clunk occurs when the scaphoid has dissociated from the lunate because of an SLL tear and hits against the dorsal lip of the radius during the maneuver.
Imaging
 Order wrist radiographs: PA, lateral, oblique, clenched fist, and scaphoid (navicular) views.
Order wrist radiographs: PA, lateral, oblique, clenched fist, and scaphoid (navicular) views.
 Clenched fist views may show widening of the SL interval (>3 to 4 mm is abnormal; must compare with the contralateral side) (Fig. 4-22).
Clenched fist views may show widening of the SL interval (>3 to 4 mm is abnormal; must compare with the contralateral side) (Fig. 4-22).
 The lateral view may show an SL angle greater than 60 degrees (an increased SL angle is also known as dorsal intercalated segment instability or DISI). The normal angle is 30 to 60 degrees (Fig. 4-23).
The lateral view may show an SL angle greater than 60 degrees (an increased SL angle is also known as dorsal intercalated segment instability or DISI). The normal angle is 30 to 60 degrees (Fig. 4-23).
 The PA view may reveal a scaphoid ring sign (Fig. 4-24).
The PA view may reveal a scaphoid ring sign (Fig. 4-24).

Figure 4-24. Scaphoid ring sign (arrowheads).
Double arrow, SL interval. (From Green DP, Hotchkiss RN, Pederson WC, et al, editors: Green’s operative hand surgery. In Marc Garcia-Elias and William B. Geissler, editors: Carpal Instability, ed 5, Philadelphia, 2005, Churchill Livingstone p 557.)
 MRI can help to identify SL injuries, but sensitivity and specificity vary depending on the quality of MRI and the expertise and experience of the radiologist.
MRI can help to identify SL injuries, but sensitivity and specificity vary depending on the quality of MRI and the expertise and experience of the radiologist.
 The gold standard for diagnosis of a tear is wrist arthroscopy.
The gold standard for diagnosis of a tear is wrist arthroscopy.
Classification
Stages of instability resulting from ligament injury
Scapholunate advanced collapse (SLAC): Figure 4-25
This term refers to a predictable pattern of osteoarthritis of the wrist that results from a chronic untreated SL tear. The radioscaphoid joint is first affected, followed by the lunatocapitate joint (Fig. 4-26).
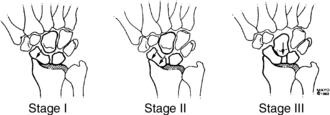
Figure 4-26. Stages of scapholunate advanced collapse (arrows). Note with advancing stage, capitate migrates proximally. (From Shin AY, Moran SL: Carpal instability including dislocation. In Trumble T, Budoff J, Cornwall R, editors: Hand, elbow, and shoulder: core knowledge in orthopaedics, Philadelphia, 2006, Mosby, p 151.)
Initial treatment
 SLL instability is the most common form of carpal instability. Complete tears should be treated surgically within 6 weeks. Complete SLL tears left untreated will lead to wrist arthritis (SLAC wrist). Partial SLL tears may be treated with casting and/or cortisone injections. If symptomatic after conservative treatment, patients with partial SLL tears may undergo wrist arthroscopy for staging, débridement, and treatment planning.
SLL instability is the most common form of carpal instability. Complete tears should be treated surgically within 6 weeks. Complete SLL tears left untreated will lead to wrist arthritis (SLAC wrist). Partial SLL tears may be treated with casting and/or cortisone injections. If symptomatic after conservative treatment, patients with partial SLL tears may undergo wrist arthroscopy for staging, débridement, and treatment planning.
Treatment options
 Conservative management is reserved for patients with partial tears or chronic complete tears with evidence of static instability or patients too ill for surgery.
Conservative management is reserved for patients with partial tears or chronic complete tears with evidence of static instability or patients too ill for surgery.
• Partial tears: Cast immobilization for 4 to 6 weeks is indicated. If immobilization does not provide relief, consider radiocarpal wrist injection.
• Chronic injuries (>6 months) respond poorly to surgical repair. Consider symptom control with splinting and radiocarpal cortisone injections as needed. Patients should be counseled that arthritic changes and loss of motion will be expected.
• Salvage procedures for symptomatic injuries that are identified late (chronic injuries) include proximal row carpectomy and total wrist fusion (for stages 3 and 4). Surgery should be suggested only after conservative treatment has failed.
Surgical procedures
 Surgical options are numerous and include:
Surgical options are numerous and include:
• Ligament reconstruction with dorsal capsulodesis (uses portion of dorsal wrist capsule to tether the scaphoid and prevent it from subluxing)
 Diagnostic wrist arthroscopy is used to confirm the diagnosis, to stage the injury, and to assist with the decision for repair option.
Diagnostic wrist arthroscopy is used to confirm the diagnosis, to stage the injury, and to assist with the decision for repair option.
Estimated postoperative course
 The postoperative course depends on the type and extent of the procedure.
The postoperative course depends on the type and extent of the procedure.
 If the SL is pinned, the patient is usually casted, and the pins are removed 6 to 8 weeks postoperatively.
If the SL is pinned, the patient is usually casted, and the pins are removed 6 to 8 weeks postoperatively.
 All procedures require postoperative rehabilitation with a hand therapist.
All procedures require postoperative rehabilitation with a hand therapist.
Kienbock disease
Imaging: Figure 4-27

Figure 4-27. Radiograph of stage IIIa Kienbock disease.
The lunate shows increased sclerosis and collapse. (From Thaller JB: Kienbock’s disease. In Miller MD, Hart JA, MacKnight JM, editors: Essential orthopaedics, Philadelphia, 2010, Saunders, p 318.)
 Order wrist radiographs: PA, lateral, and oblique views.
Order wrist radiographs: PA, lateral, and oblique views.
 Evaluate for negative ulnar variance (defined as the distal ulna being shorter than the distal radius). This finding is a risk factor for Kienbock disease because it increases the amount of force transmitted across the radiolunate joint.
Evaluate for negative ulnar variance (defined as the distal ulna being shorter than the distal radius). This finding is a risk factor for Kienbock disease because it increases the amount of force transmitted across the radiolunate joint.
 Consider MRI if the diagnosis not clear on radiographs or to assist in staging the disease.
Consider MRI if the diagnosis not clear on radiographs or to assist in staging the disease.
Classification: table 4-7
Table 4-7.
Classification and Treatment of Kienbock Disease
| STAGE | RADIOGRAPHIC FINDINGS |
| Stage I | Normal radiographs or linear fracture; abnormal and nonspecific bone scan; on magnetic resonance imaging, lunate shows low signal intensity on T1-weighted images and high or low signal on T2-weighted images |
| Stage II | Lunate sclerosis, one or more fracture lines with possible early collapse of lunate on radial border |
| Stage IIIa | Lunate collapse with normal carpal alignment and height |
| Stage IIIb | Fixed hyperflexion of scaphoid, carpal height decreased, proximal migration of capitate |
| Stage IV | Severe lunate collapse with intra-articular degenerative changes seen at midcarpal joint and/or radiocarpal joint |
From Allan CH, Joshi A, Lictman DM: Kienbock’s disease: diagnosis and treatment, J Am Acad Orthop Surg 9: 128–136, 2001.
Initial treatment
 Kienbock disease is more common in men than in women and usually affects patients 20 to 40 years old. It is usually unilateral. Although the cause is unknown, isolated or repetitive trauma to a lunate predisposed to the disease may lead to necrosis. Treatment is based on symptoms and stage of the disease, and prognosis is very difficult to predict.
Kienbock disease is more common in men than in women and usually affects patients 20 to 40 years old. It is usually unilateral. Although the cause is unknown, isolated or repetitive trauma to a lunate predisposed to the disease may lead to necrosis. Treatment is based on symptoms and stage of the disease, and prognosis is very difficult to predict.
Treatment options (based on stage) table 4-7
 Stage I: immobilization with cast or external fixator for up to 3 months
Stage I: immobilization with cast or external fixator for up to 3 months
 Stages II and IIIa with negative ulnar variance:
Stages II and IIIa with negative ulnar variance:
• Revascularization procedures using insertion of vascularized pedicle bone graft into lunate
• Alternative treatment options include radial wedge osteotomy or capitate shortening
 Stage IIIa with negative ulnar variance: foregoing procedures, in addition to radius shortening osteotomy, ulnar lengthening, or capitate shortening
Stage IIIa with negative ulnar variance: foregoing procedures, in addition to radius shortening osteotomy, ulnar lengthening, or capitate shortening
 Stage IIIb: scaphotrapeziotrapezoid (STT) or scaphocapitate joint fusion with or without lunate excision, radius shortening osteotomy, or proximal row carpectomy
Stage IIIb: scaphotrapeziotrapezoid (STT) or scaphocapitate joint fusion with or without lunate excision, radius shortening osteotomy, or proximal row carpectomy
Operative management
Informed consent and counseling
 Even with appropriate treatment and good surgical technique, the disease may progress.
Even with appropriate treatment and good surgical technique, the disease may progress.
 Smoking cessation is imperative for healing.
Smoking cessation is imperative for healing.
 The patient can expect to be immobilized for approximately 6 weeks, but the type of immobilization depends on the surgeon’s preference.
The patient can expect to be immobilized for approximately 6 weeks, but the type of immobilization depends on the surgeon’s preference.
 The patient will require approximately 2 to 3 months of outpatient hand therapy to improve motion and strength.
The patient will require approximately 2 to 3 months of outpatient hand therapy to improve motion and strength.
Triangular fibrocartilage complex tear
History
 A fall in ulnar deviation or twisting mechanism may cause this injury.
A fall in ulnar deviation or twisting mechanism may cause this injury.
 The patient reports ulnar-sided wrist pain and increased pain with wrist positions that mimic injury.
The patient reports ulnar-sided wrist pain and increased pain with wrist positions that mimic injury.
 The patient may report weakness or sense of instability at the wrist.
The patient may report weakness or sense of instability at the wrist.
 The patient may have a history of distal radius malunion with ulnar positive variance.
The patient may have a history of distal radius malunion with ulnar positive variance.
Physical examination
 Examination may reveal a prominent ulnar styloid, edema, or ecchymosis over the ulnar side of the wrist.
Examination may reveal a prominent ulnar styloid, edema, or ecchymosis over the ulnar side of the wrist.
 Tenderness to palpation is noted on the ulnar side of the wrist.
Tenderness to palpation is noted on the ulnar side of the wrist.
 Positive fovea sign: This sign consists of palpable tenderness in the soft depression proximal to triquetrum and between the FCU tendon and the ECU tendon.
Positive fovea sign: This sign consists of palpable tenderness in the soft depression proximal to triquetrum and between the FCU tendon and the ECU tendon.
 Positive ulnar grind test: The examiner extends, axially loads, and ulnarly deviates wrist; a positive test result is pain with this motion.
Positive ulnar grind test: The examiner extends, axially loads, and ulnarly deviates wrist; a positive test result is pain with this motion.
 Piano key test for stability of the DRUJ: The examiner places one hand on the patient’s radius and then applies dorsal pressure over the ulnar head with the opposite hand. Compare with contralateral side. Increased motion or pain with motion on injured side is a positive test result.
Piano key test for stability of the DRUJ: The examiner places one hand on the patient’s radius and then applies dorsal pressure over the ulnar head with the opposite hand. Compare with contralateral side. Increased motion or pain with motion on injured side is a positive test result.
Imaging
 Order wrist radiographs: PA, lateral, and oblique views.
Order wrist radiographs: PA, lateral, and oblique views.
 This injury may be associated with ulnar positive variance (defined as ulna >4 mm longer than the radius) and ulnocarpal impaction syndrome (distal ulna abuts the lunate and causes degeneration of the TFCC over time) (Fig. 4-28).
This injury may be associated with ulnar positive variance (defined as ulna >4 mm longer than the radius) and ulnocarpal impaction syndrome (distal ulna abuts the lunate and causes degeneration of the TFCC over time) (Fig. 4-28).

Figure 4-28. Measuring ulnar positive variance. Radiograph shows ulnar positive variance. (From Rynders SD, Chhabra AB: Triangular fibrocartilage complex injuries. In Miller MD, Hart JA, MacKnight JM, editors: Essential orthopaedics, Philadelphia, 2010, Saunders, p 323.)
 Assess for DRUJ widening compared with the uninjured wrist on the PA view.
Assess for DRUJ widening compared with the uninjured wrist on the PA view.
 MRI, with or without contrast, is recommended for evaluating TFCC injuries. The quality of scans and the radiologist’s experience play a role in accurately diagnosing a tear. Studies suggest an accuracy rate of approximately 64% with MRI with an arthrogram. The gold standard for diagnosis is wrist arthroscopy (Fig. 4-29).
MRI, with or without contrast, is recommended for evaluating TFCC injuries. The quality of scans and the radiologist’s experience play a role in accurately diagnosing a tear. Studies suggest an accuracy rate of approximately 64% with MRI with an arthrogram. The gold standard for diagnosis is wrist arthroscopy (Fig. 4-29).
Classification*
Treatment options (based on classification)
 Class 1A: Options include rest, immobilization in a Muenster cast, anti-inflammatory medication, and local steroid injections.
Class 1A: Options include rest, immobilization in a Muenster cast, anti-inflammatory medication, and local steroid injections.
 If symptoms persist, an arthroscopic débridement may be necessary
If symptoms persist, an arthroscopic débridement may be necessary
 Class 1B and 1C: Initial treatment consists of a volar splint, short-arm cast, or Muenster cast for 6 weeks followed by an additional 4 to 6 weeks of activity modification (e.g., no heavy lifting). Most Class 1B injuries respond to conservative measures. If symptoms persist or instability is present, surgery is indicated. Surgery may include open or arthroscopic repair.
Class 1B and 1C: Initial treatment consists of a volar splint, short-arm cast, or Muenster cast for 6 weeks followed by an additional 4 to 6 weeks of activity modification (e.g., no heavy lifting). Most Class 1B injuries respond to conservative measures. If symptoms persist or instability is present, surgery is indicated. Surgery may include open or arthroscopic repair.
 Class 1D: These tears are frequently associated with distal radius fractures. This injury usually heals with appropriate treatment of the fracture.
Class 1D: These tears are frequently associated with distal radius fractures. This injury usually heals with appropriate treatment of the fracture.
Class 2: Degenerative tears
 Severity and progression vary.
Severity and progression vary.
 Treatment options include activity modification, anti-inflammatory medications, wrist splinting, and cortisone injection into the wrist joint. If these measures fail, wrist arthroscopy for débridement of the tear is indicated. Often, an ulnar-shortening osteotomy is performed if there is underlying ulnar positive variance.
Treatment options include activity modification, anti-inflammatory medications, wrist splinting, and cortisone injection into the wrist joint. If these measures fail, wrist arthroscopy for débridement of the tear is indicated. Often, an ulnar-shortening osteotomy is performed if there is underlying ulnar positive variance.
Surgical procedures
Arthroscopic debridement and repair:
 The affected arm is positioned in a traction tower with 15 lb of traction across the wrist.
The affected arm is positioned in a traction tower with 15 lb of traction across the wrist.
 Use the 3-4 portal (between third and fourth dorsal extensor compartments) for visualization and classification of the tear while a probe is placed in the 4-5 portal (between the fourth and fifth dorsal extensor compartments).
Use the 3-4 portal (between third and fourth dorsal extensor compartments) for visualization and classification of the tear while a probe is placed in the 4-5 portal (between the fourth and fifth dorsal extensor compartments).
 A shaver is used to débride class 1A tears.
A shaver is used to débride class 1A tears.
 Many different techniques for TFCC repairs are used. In general, the camera can be placed in 6R portal and the shaver placed in 3-4 portal to débride synovitis. Then an incision is made in line with the 6U portal (just ulnar to the ECU tendon). Sutures are passed through a cannula in the 3-4 portal into the TFCC and out through the capsule into the 6U incision. Tie sutures down over the capsule (take care not to entrap branches of the ulnar dorsal sensory nerve). For TFCC repairs, the patient should be placed in a long-arm splint with the forearm supinated 45 degrees.
Many different techniques for TFCC repairs are used. In general, the camera can be placed in 6R portal and the shaver placed in 3-4 portal to débride synovitis. Then an incision is made in line with the 6U portal (just ulnar to the ECU tendon). Sutures are passed through a cannula in the 3-4 portal into the TFCC and out through the capsule into the 6U incision. Tie sutures down over the capsule (take care not to entrap branches of the ulnar dorsal sensory nerve). For TFCC repairs, the patient should be placed in a long-arm splint with the forearm supinated 45 degrees.
Osteoarthritis of the wrist and hand
 Osteoarthritis usually affects the first CMC joint, PIP and DIP joints. Less commonly, the MCP joints are affected. Its predilection for the wrist joint is usually the result of a previous injury such as a remote ligament sprain or previous carpal or radius fracture.
Osteoarthritis usually affects the first CMC joint, PIP and DIP joints. Less commonly, the MCP joints are affected. Its predilection for the wrist joint is usually the result of a previous injury such as a remote ligament sprain or previous carpal or radius fracture.
 The patient may report pain, edema, stiffness, or deformity of the affected joint.
The patient may report pain, edema, stiffness, or deformity of the affected joint.
 Pain may be worse in the morning and after repetitive activities.
Pain may be worse in the morning and after repetitive activities.
Physical examination
Imaging: Figure 4-30
Classification
First carpometacarpal joint arthritis
 Eaton stages of first CMC joint osteoarthritis†
Eaton stages of first CMC joint osteoarthritis†
Stage 1: normal joint with exception of possible widening from synovitis
Stage 2: joint space narrowing with debris and osteophytes smaller than 2 mm
Stage 3: joint space narrowing with debris and osteophytes larger than 2 mm
Stage 4: scaphotrapezial joint space involvement in addition to narrowing of the CMC joint
Treatment options
Operative management of distal interphalangeal, proximal interphalangeal, metacarpophalangeal, and first carpometacarpal osteoarthritis
Codes
Informed consent and counseling
 Arthrodesis or joint fusion is a pain-relieving surgical procedure that renders the joint immobile.
Arthrodesis or joint fusion is a pain-relieving surgical procedure that renders the joint immobile.
 A risk of nonunion is reported in smokers; smoking is considered a relative contraindication.
A risk of nonunion is reported in smokers; smoking is considered a relative contraindication.
 For first CMC joint arthroplasty with interposition, recovery may take up to 3 to 6 months and involves a period of immobilization.
For first CMC joint arthroplasty with interposition, recovery may take up to 3 to 6 months and involves a period of immobilization.
 There is a risk of nail deformity with DIP joint surgical interventions.
There is a risk of nail deformity with DIP joint surgical interventions.
 Almost all surgical interventions for arthritis require postoperative therapy.
Almost all surgical interventions for arthritis require postoperative therapy.
Carpal tunnel syndrome
Carpal tunnel syndrome (CTS) is compression of the median nerve at the wrist and is the most common compression neuropathy of the upper extremity.
History
 Numbness and tingling occur in the thumb, index finger, middle finger, and the radial half of the ring finger.
Numbness and tingling occur in the thumb, index finger, middle finger, and the radial half of the ring finger.
 Some patients report numbness or tingling in all fingers.
Some patients report numbness or tingling in all fingers.
 Symptoms are worse at night, with nocturnal awakening or when driving.
Symptoms are worse at night, with nocturnal awakening or when driving.
 The patient reports feeling the need to shake out the hands to get relief, also known as the “flick sign.”
The patient reports feeling the need to shake out the hands to get relief, also known as the “flick sign.”
Physical examination
 Inspect for thenar atrophy of the abductor pollicis brevis (suggestive of severe involvement).
Inspect for thenar atrophy of the abductor pollicis brevis (suggestive of severe involvement).
 Positive Tinel sign: Percussion over the median nerve at the wrist flexor crease reproduces paresthesias in the fingers.
Positive Tinel sign: Percussion over the median nerve at the wrist flexor crease reproduces paresthesias in the fingers.
 Positive pressure test: Direct compression over the median nerve reproduces paresthesias in the fingers.
Positive pressure test: Direct compression over the median nerve reproduces paresthesias in the fingers.
 Positive Phalen test: Wrist flexion for 1 to 2 minutes reproduces paresthesias in the fingers (note: keep the elbow extended during this test to prevent compression at the elbow).
Positive Phalen test: Wrist flexion for 1 to 2 minutes reproduces paresthesias in the fingers (note: keep the elbow extended during this test to prevent compression at the elbow).
 Two-point discrimination may be diminished in the median nerve distribution (5 mm considered normal).
Two-point discrimination may be diminished in the median nerve distribution (5 mm considered normal).
Further diagnostic testing
Initial treatment
 CTS is the most common compression neuropathy and is more common in women and patients with diabetes mellitus. The syndrome is progressive; therefore, it is important to diagnose and treat it appropriately to prevent permanent damage to the nerve and the muscles it innervates.
CTS is the most common compression neuropathy and is more common in women and patients with diabetes mellitus. The syndrome is progressive; therefore, it is important to diagnose and treat it appropriately to prevent permanent damage to the nerve and the muscles it innervates.
 CTS may occur during pregnancy and is usually temporary and self-limited after delivery. Carpal tunnel surgery should be avoided during pregnancy.
CTS may occur during pregnancy and is usually temporary and self-limited after delivery. Carpal tunnel surgery should be avoided during pregnancy.
Treatment options
Operative management
Informed consent and counseling
 Even with appropriate treatment and good surgical release, there may be residual paresthesias, depending on the severity of disease.
Even with appropriate treatment and good surgical release, there may be residual paresthesias, depending on the severity of disease.
• If the patient has concomitant cervical nerve root compression in addition to CTS, he or she may not gain full relief of symptoms in the upper extremity.
 The patient may be immobilized for a period of roughly 2 weeks postoperatively and can return to most strenuous activities by 4 to 6 weeks.
The patient may be immobilized for a period of roughly 2 weeks postoperatively and can return to most strenuous activities by 4 to 6 weeks.
Surgical procedures
Open carpal tunnel release: Figure 4-31
 Determine the location of incision: Draw a Kaplan cardinal line from the hook of the hamate to the first web space.
Determine the location of incision: Draw a Kaplan cardinal line from the hook of the hamate to the first web space.
 A volar palmar incision is made along radial border of the ring finger to the ulnar side of the palmaris longus to avoid injury to the palmar cutaneous branch of the median nerve.
A volar palmar incision is made along radial border of the ring finger to the ulnar side of the palmaris longus to avoid injury to the palmar cutaneous branch of the median nerve.
 Protect the recurrent motor branch of the medial nerve (the point at which the line from the radial aspect of the middle finger intersects with the Kaplan line). This branch has a variable course.
Protect the recurrent motor branch of the medial nerve (the point at which the line from the radial aspect of the middle finger intersects with the Kaplan line). This branch has a variable course.
 Use sharp dissection through the subcutaneous tissues and the longitudinal fibers of the superficial palmar fascia, and expose the transverse fibers of the transverse carpal ligament (TCL).
Use sharp dissection through the subcutaneous tissues and the longitudinal fibers of the superficial palmar fascia, and expose the transverse fibers of the transverse carpal ligament (TCL).
 Place a blunt instrument such as a Freer or hemostat under the TCL to protect the median nerve beneath, and sharply incise along the entire length.
Place a blunt instrument such as a Freer or hemostat under the TCL to protect the median nerve beneath, and sharply incise along the entire length.
De quervain tenosynovitis
History
 This disorder is associated with repetitive tasks involving the thumb and wrist.
This disorder is associated with repetitive tasks involving the thumb and wrist.
 The patient reports pain over the radial wrist and thumb that is worse with thumb abduction and/or extension.
The patient reports pain over the radial wrist and thumb that is worse with thumb abduction and/or extension.
 This condition is often seen in pregnancy or in patients with newborns as a result of cradling infants in arms (“new mom’s tendinitis”).
This condition is often seen in pregnancy or in patients with newborns as a result of cradling infants in arms (“new mom’s tendinitis”).
Physical examination
 Edema and tenderness are noted at the first dorsal extensors extending to the radial styloid.
Edema and tenderness are noted at the first dorsal extensors extending to the radial styloid.
 Positive Finkelstein test (Fig. 4-32): The thumb is clasped into the palm, and the wrist is passively ulnarly deviated. A positive test result consists of severe pain.
Positive Finkelstein test (Fig. 4-32): The thumb is clasped into the palm, and the wrist is passively ulnarly deviated. A positive test result consists of severe pain.
 Pain occurs with thumb motion or active radial deviation.
Pain occurs with thumb motion or active radial deviation.
 Occasionally, this disorder is associated with a ganglion cyst over the first dorsal compartment.
Occasionally, this disorder is associated with a ganglion cyst over the first dorsal compartment.
Differential diagnosis
 Intersection syndrome (inflammation and pain at the point where the first extensor compartment tendons cross over the second extensor compartment tendons [the extensor carpi radialis longus and the extensor carpi radialis brevis tendons, proximal to Lister tubercle of the distal radius])
Intersection syndrome (inflammation and pain at the point where the first extensor compartment tendons cross over the second extensor compartment tendons [the extensor carpi radialis longus and the extensor carpi radialis brevis tendons, proximal to Lister tubercle of the distal radius])
Initial treatment
 de Quervain tenosynovitis is more common in female patients, especially after childbirth. It is an inflammatory condition that is exacerbated by overuse. Treatment may include a thumb spica splint, hand therapy, and/or a cortisone injection. Although effective, cortisone injections in this area may cause subcutaneous fat atrophy and/or skin hypopigmentation at the injection site.
de Quervain tenosynovitis is more common in female patients, especially after childbirth. It is an inflammatory condition that is exacerbated by overuse. Treatment may include a thumb spica splint, hand therapy, and/or a cortisone injection. Although effective, cortisone injections in this area may cause subcutaneous fat atrophy and/or skin hypopigmentation at the injection site.
Surgical procedure
First dorsal compartment release
 Approach via the first extensor compartment radially with a short transverse incision.
Approach via the first extensor compartment radially with a short transverse incision.
 Divide the extensor retinaculum longitudinally.
Divide the extensor retinaculum longitudinally.
 Protect the SSRN and its branches, and avoid excessive dissection.
Protect the SSRN and its branches, and avoid excessive dissection.
 Release the first dorsal compartment on its dorsal margin.
Release the first dorsal compartment on its dorsal margin.
 Identify the EPB and all slips of the APL.
Identify the EPB and all slips of the APL.
 Be aware of anatomic variations (the compartment may have a longitudinal septum, the APL often has two or more slips with various insertions, and the EPB is absent in 5% to 7% of extremities).
Be aware of anatomic variations (the compartment may have a longitudinal septum, the APL often has two or more slips with various insertions, and the EPB is absent in 5% to 7% of extremities).