Wrist and Hand
A. Bobby Chhabra, Aaron M. Freilich
Regional Anatomy and Surgical Intervals
Regional Anatomy
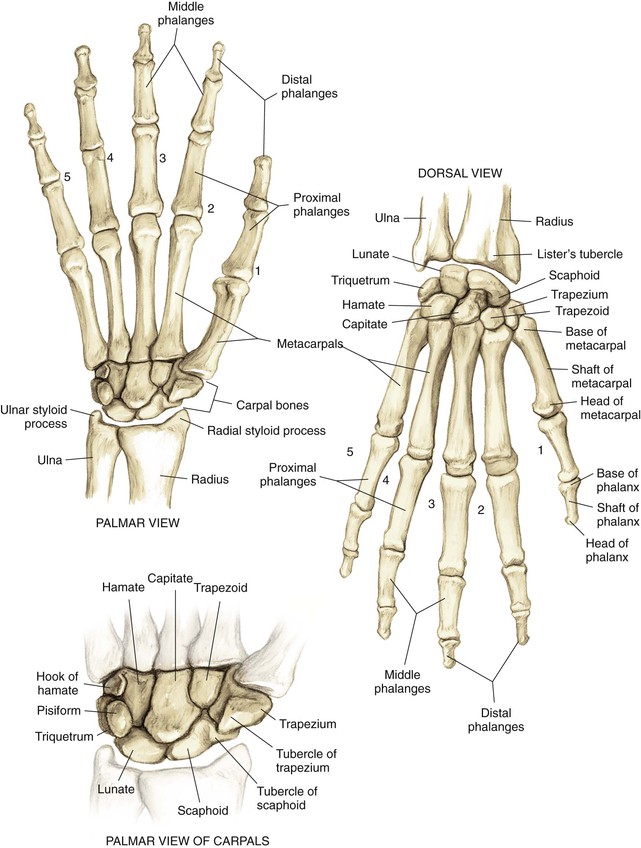
Osteology (Fig. 4-1)
Distal Radius
Phalanges
• Insertion of the flexor digitorum superficialis (FDS) on the volar surface at the base
• Insertion of the central slip of the extensor hood on the dorsal surface
• Insertion of the flexor digitorum profundus (FDP) on the volar surface
• Insertion of the terminal extensor tendon on the dorsal surface
Arthrology
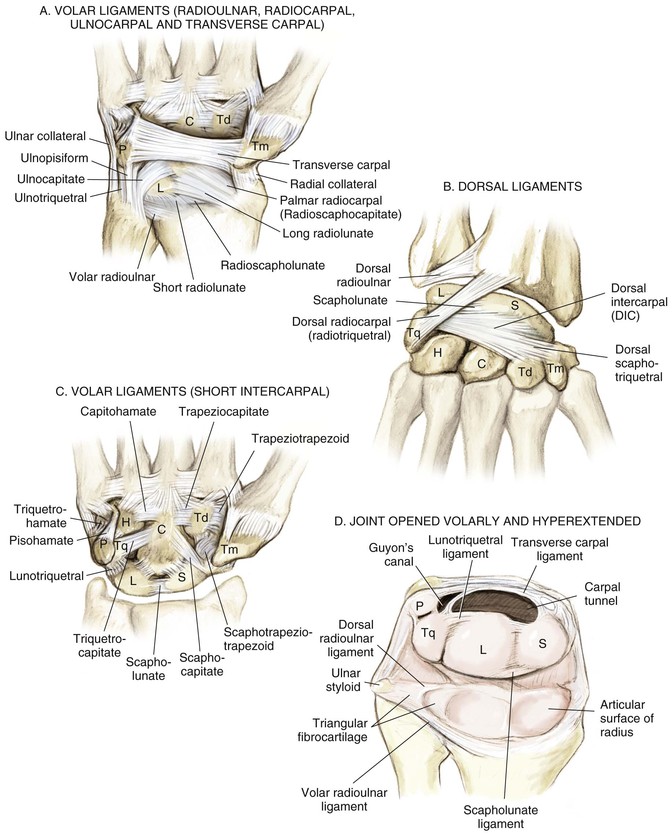
Radiocarpal Joint (Fig. 4-2, A and B)
The distal radius articulates with the proximal carpal row
Extrinsic volar and dorsal ligaments
Radioscaphocapitate, long and short radiolunate, ulnar collateral ligaments (part of the TFCC)
Dorsal ligaments (dorsal intercarpal and dorsal radiocarpal)
Distal Radioulnar Joint
The ulna articulates with the radius in the sigmoid notch
Distal radioulnar ligaments of the TFCC are the major stabilizers of the distal radioulnar joint
• Located on the articular surface of the distal ulna and the very ulnar aspect of the distal radius
• The central portion of the triangular fibrocartilage is thin and avascular
• The periphery is vascularized and amenable to repair
Interosseous Joints/Ligaments (See Fig. 4-2, C and D)
Extrinsic Wrist Ligaments (See Fig. 4-2, A and B)
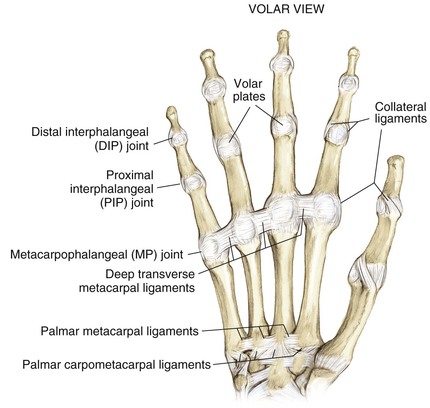
Carpometacarpal Joints (Fig. 4-3)
Metacarpophalangeal (MCP) joints
Proximal interphalangeal (PIP) joints
Distal interphalangeal (DIP) joints
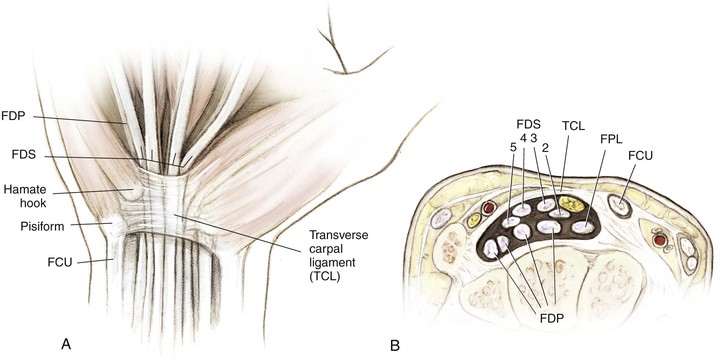
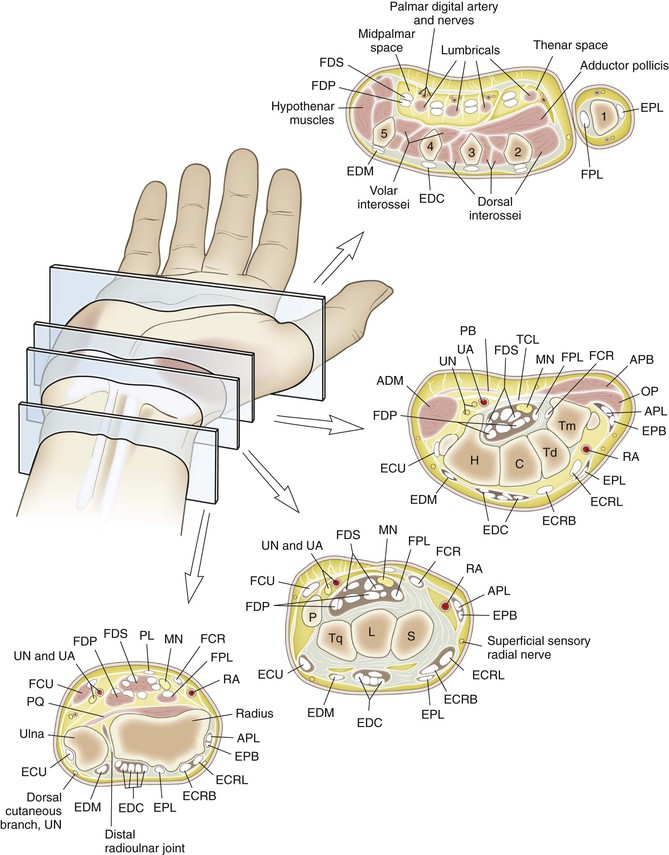
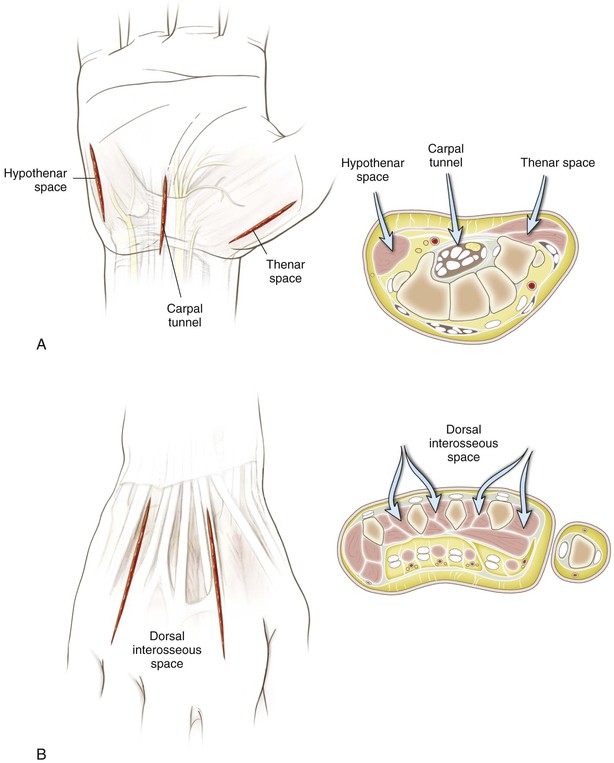
• Flexor tendon relationship in carpal tunnel
• The FDS to digits 3 and 4 lies volar to tendons 2 and 5 (Fig. 4-5, A and B)
• The FDP lies dorsal to the FDS in the forearm
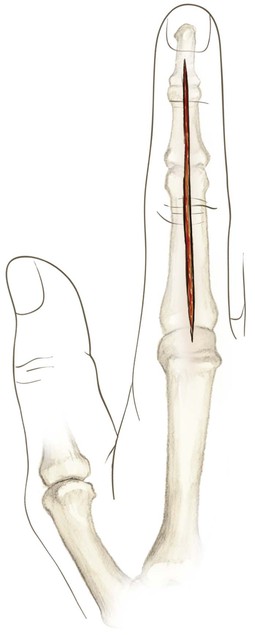
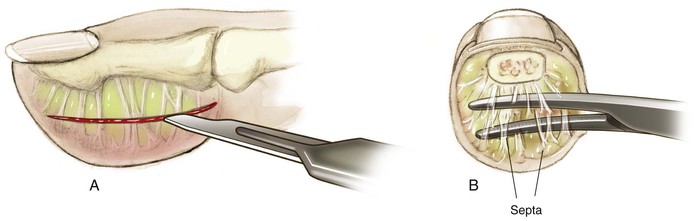
• Camper’s chiasm—crossing of the FDS and FDP tendons at the level of the proximal phalanx; from the forearm to Camper’s chiasm, the FDS lies volar to the FDP; in the finger, the FDS splits and attaches onto the middle phalanx; the FDP emerges from between the chiasm volarly and continues to its attachment on the distal phalanx (see Fig. 4-4, A)
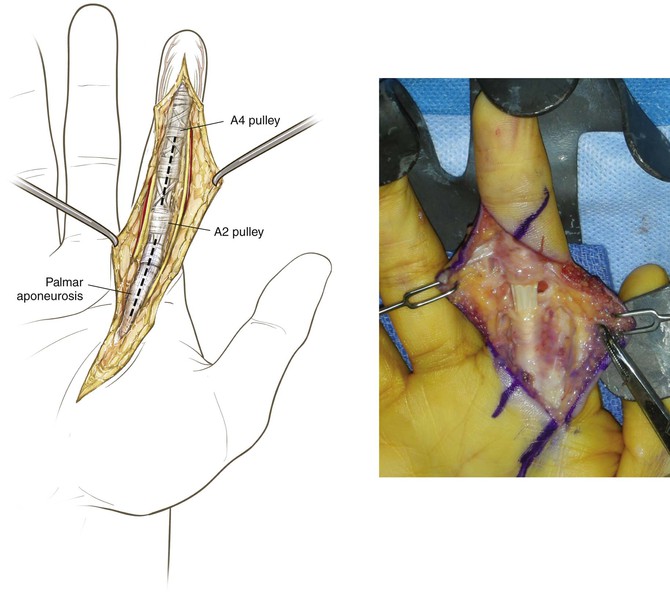
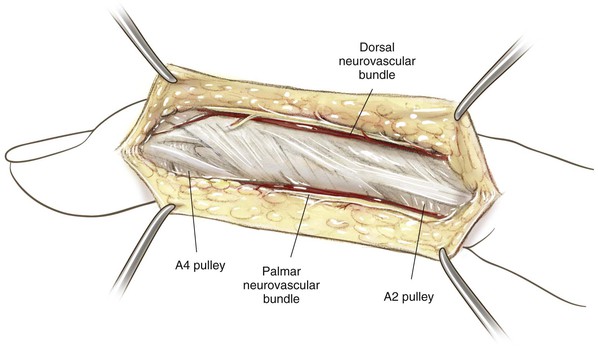
• Finger flexor pulley system (see Figure 4-4, B)
• Five annular ligaments and four cruciate ligaments
• A2 and A4 are crucial and prevent bowstringing of the flexor tendon
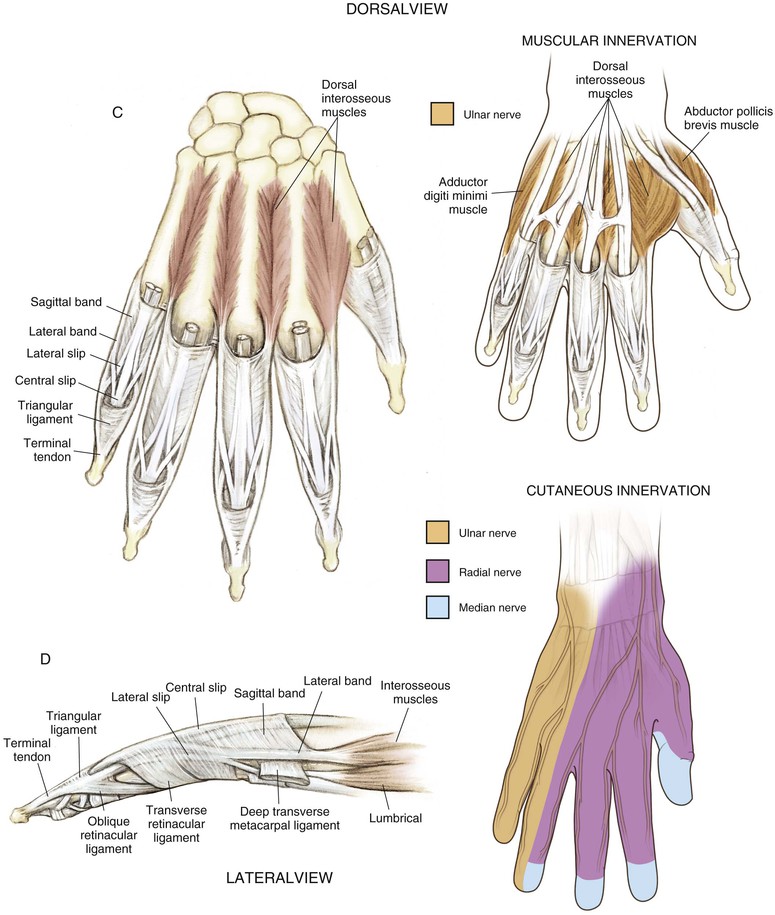
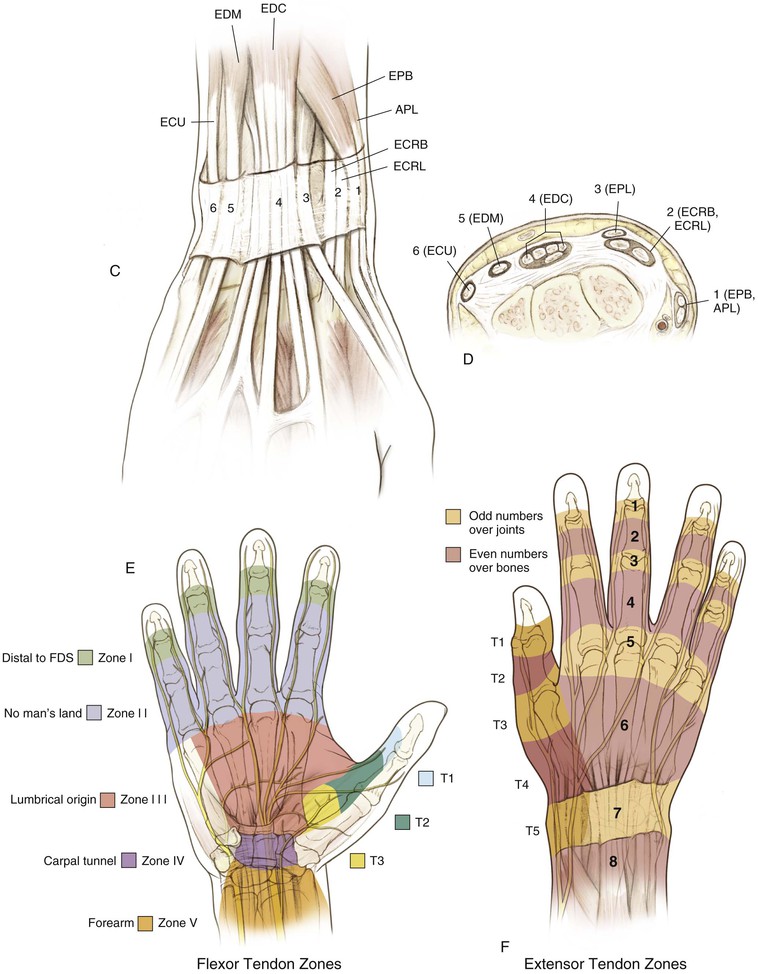
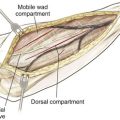
• Extensor tendon compartments (Table 4-1; see Fig. 4-5, C and D)
Table 4-1
Extensor Tendon Compartments
| COMPARTMENT | TENDONS |
| 1 | EPB |
| APL | |
| 2 | ECRL |
| ECRB | |
| 3 | EPL |
| 4 | EIP |
| EDC | |
| 5 | EDM |
| 6 | ECU |
APL, Abductor pollicis longus; ECRB, extensor carpi radialis brevis; ECRL, extensor carpi radialis longus; ECU, extensor carpi ulnaris; EDC, extensor digitorum communis; EDM, extensor digiti minimi; EIP, extensor indicis proprius; EPB, extensor pollicis brevis; EPL, extensor pollicis longus.
Cross-sectional anatomy (see Fig. 4-9) at the following levels: (1) distal radioulnar joint, (2) proximal carpal row, (3) distal carpal row, and (4) proximal metacarpal.
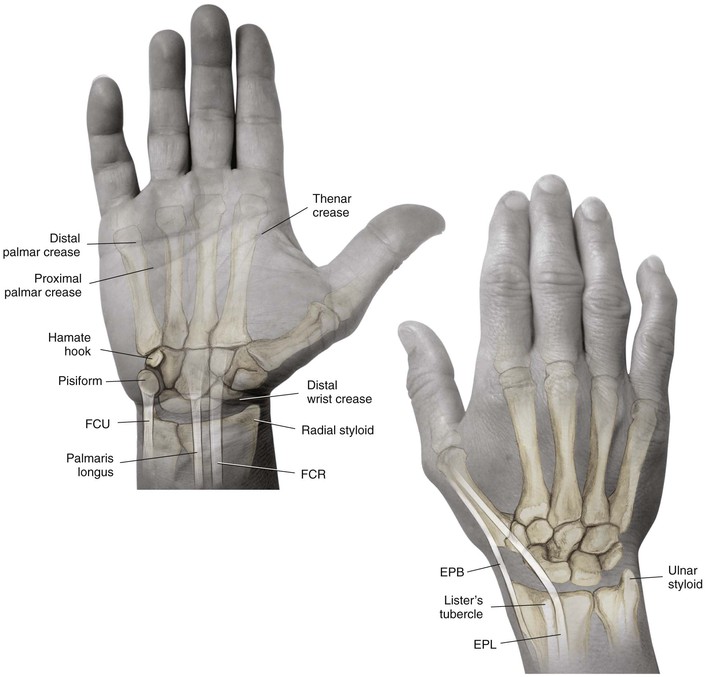
Landmarks (see Fig. 4-10): palpable anatomic landmarks: the pisiform, the hook of the hamate, Lister’s tubercle, and the palmaris.
Muscles
Best considered in groups (Table 4-2)
Table 4-2
Hand Musculature
| GROUP | MUSCLES | ORIGIN | INSERTION | INNERVATION | ACTION |
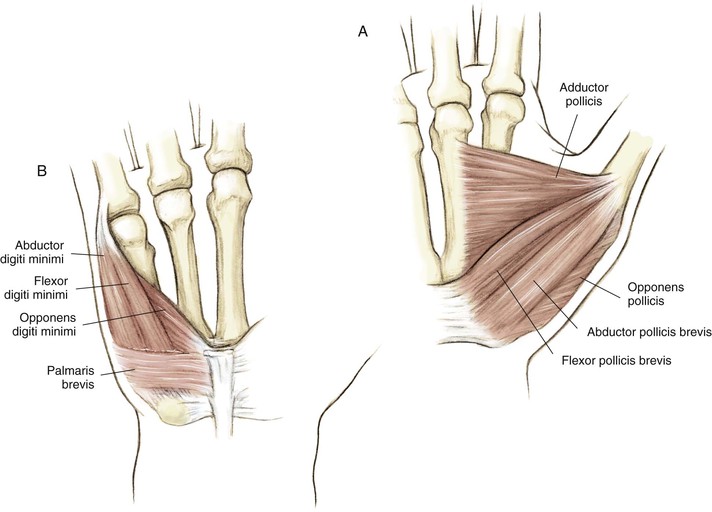
| Thenar | Opponens pollicis | Flexor retinaculum and tubercle of trapezium | Radial border of the first metacarpal | Recurrent motor branch of the median nerve | Thumb opposition |
| Abductor pollicis brevis | Scaphoid tubercle and flexor retinaculum | Base of the thumb proximal phalanx and the tendon of EPL | Recurrent motor branch of the median nerve | Thumb abduction | |
| Flexor pollicis brevis | Flexor retinaculum and tubercle of trapezium | Base of the thumb proximal phalanx | Dual innervation—deep head ulnar, superficial head median nerves | Flexion of the thumb MCP joint | |
| Adductor pollicis | Transverse head—third MC; oblique head—trapezium, trapezoid, capitate, and bases of the second and third MC | Ulnar side of the thumb proximal phalanx base | Deep branch of the ulnar nerve | Thumb adduction | |
| Hypothenar | Abductor digiti minimi | Pisiform and pisohamate ligament, flexor retinaculum | Fifth digit proximal phalanx base and extensor hood | Deep branch of the ulnar nerve | Abducts the fifth digit |
| Flexor digiti minimi | Hook of hamate and flexor retinaculum | Fifth digit proximal phalanx base | Deep branch of the ulnar nerve | Flexes the fifth digit at the MCP joint | |
| Opponens digiti minimi | Hook of hamate and flexor retinaculum | Ulnar border of the fifth MC shaft | Deep branch of the ulnar nerve | Opposes the fifth finger | |
| Intrinsic hand muscles | Lumbrical muscles | FDP tendons—first and second lumbricals are unipennate and arise on radial side of tendon; third and fourth lumbricals are bipennate and arise from adjacent tendons | Radial side of the extensor hood at the level of the proximal phalanx | First and second—median nerve; third and fourth—deep branch of the ulnar nerve | Flex MCP and extend PIP joints |
| DI muscles | 4 muscles—bipennate on metacarpal shafts | Proximal phalanges and extensor hood; first DI—radial side of index finger; second DI—radial side of middle finger; third DI—ulnar side of middle finger; fourth DI—ulnar side of ring finger | Deep branch of the ulnar nerve | Abduct from the axis of the middle finger; flex MCP joints and extend PIP joints | |
| PI muscles | 3 muscles—unipennate on MC shafts; first PI—ulnar shaft of the second MC; second PI—radial shaft of the fourth MC; third PI—radial shaft of the fifth MC | Proximal phalanges and extensor hoods; first PI—ulnar side of index finger; second PI—radial side of ring finger; third PI—radial side of small finger | Deep branch of the ulnar nerve | Adduct toward the middle finger; flex MCP joints and extend PIP joints |
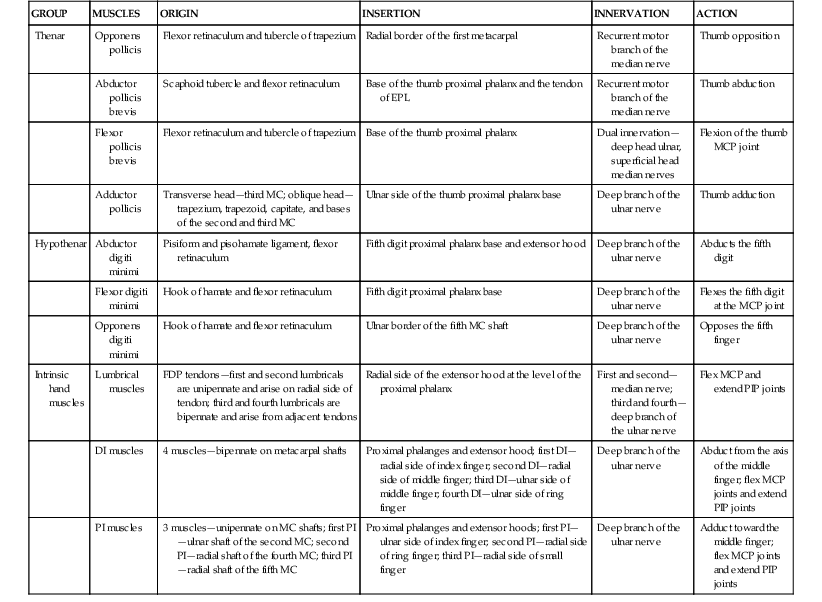
DI, Dorsal interossei; EPL, extensor pollicis longus; FDP, flexor digitorum profundus; MC, metacarpal; MCP, metacarpophalangeal; PI, palmar interossei; PIP, proximal interphalangeal.
Hypothenar Muscles
(See Fig. 4-6, B)
Intrinsic Muscles
(See Fig. 4-4, A and C)
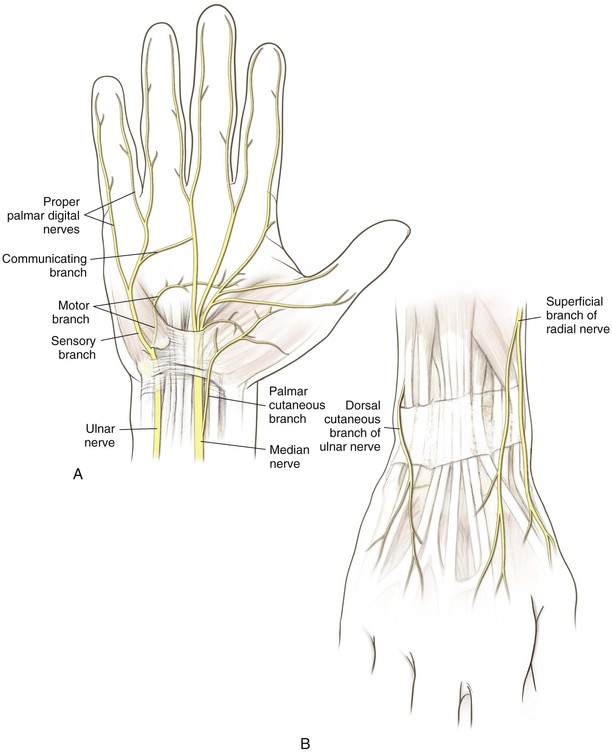
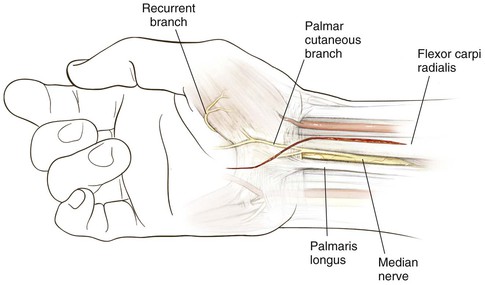
Nerves (Fig. 4-7, A)
Median Nerve
Gives off a sensory palmar branch approximately 6 cm proximal to the radial styloid
The median nerve enters the hand through the carpal tunnel
Gives off a recurrent motor branch with a variable course
• 80% branches distal to the TCL and enters the thenar musculature in a recurrent manner
• 15% branches subligamentously
Ulnar Nerve
Hazards
Nerves
The palmar cutaneous branch of the median nerve is at risk during the Henry approach
The dorsal sensory ulnar nerve branch is at risk during TFCC repairs
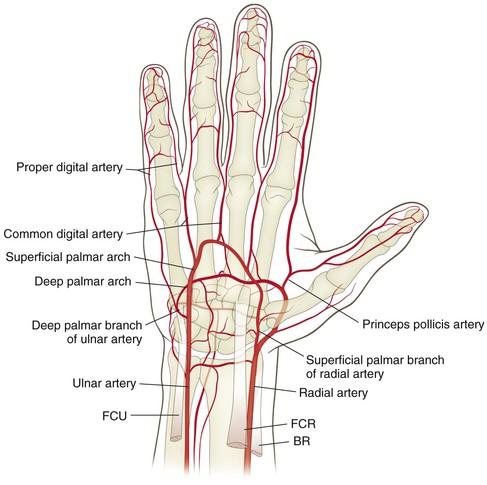
Vascular
The radial artery is at risk during the distal volar Henry approach
The ulnar artery is at risk during exposure of the ulnar distal forearm and the distal ulnar shaft
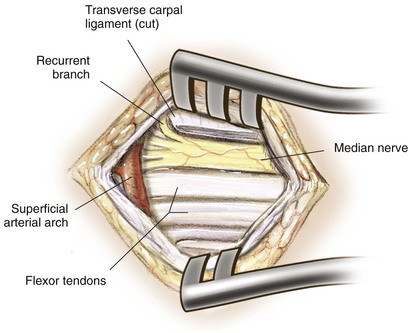
The superficial palmar arch is at risk during carpal tunnel release and exposures in palm
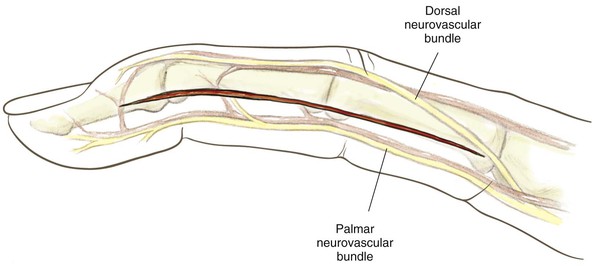
Proper digital arteries are at risk during midlateral approaches to finger and volar exposures
Palpable Anatomic Landmarks of the Hand and Wrist
Surgical Approaches to the Wrist
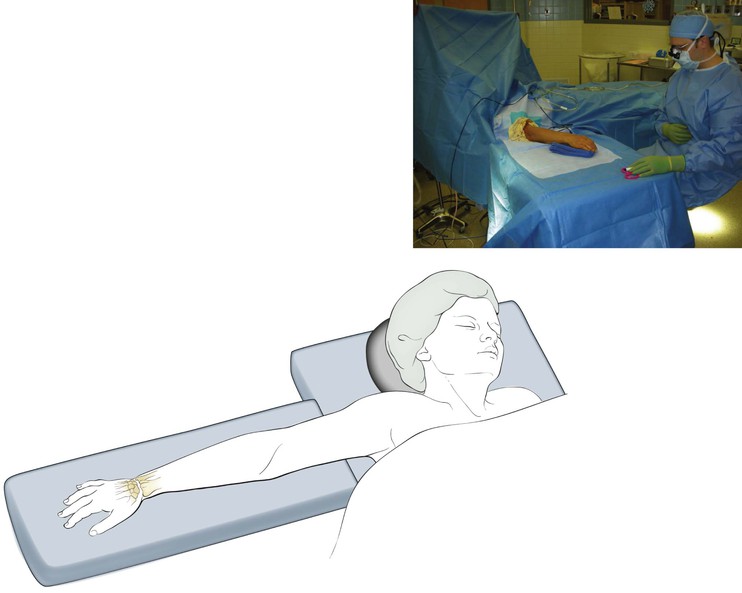
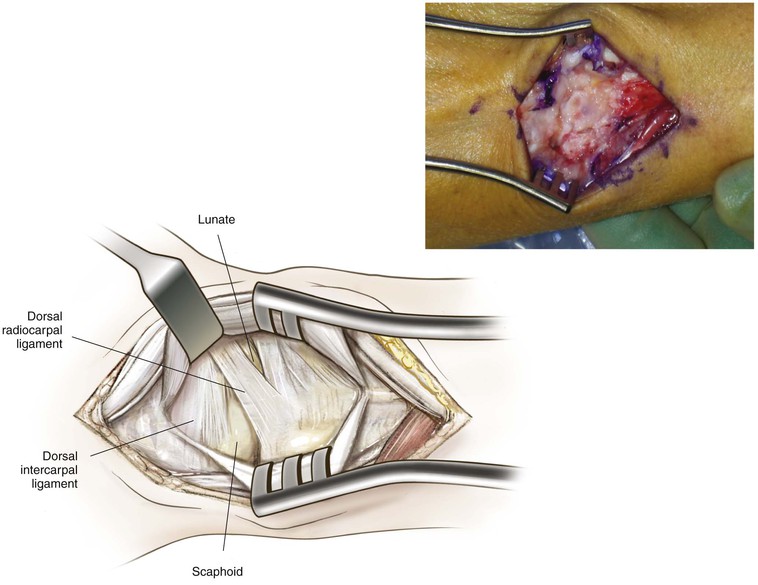
Dorsal Approach to the Forearm, Wrist, and Carpus (Video 4-1)
Indications
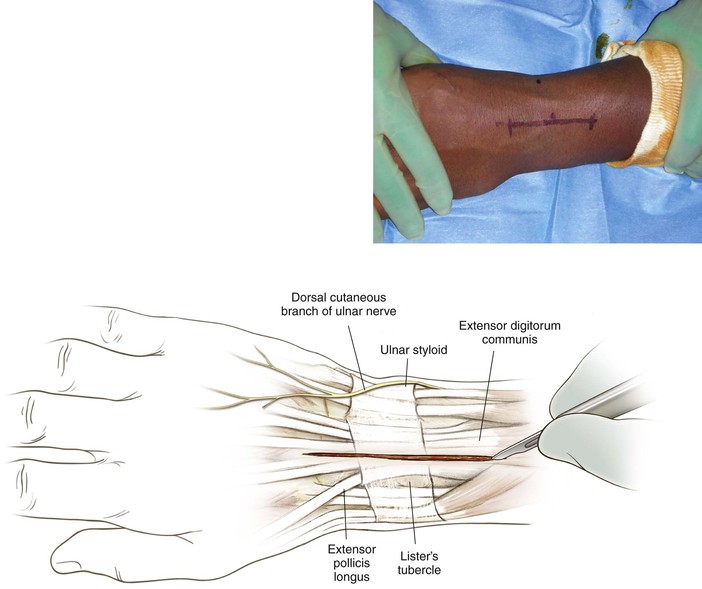
Superficial Dissection (Fig. 4-13)
Deep Dissection
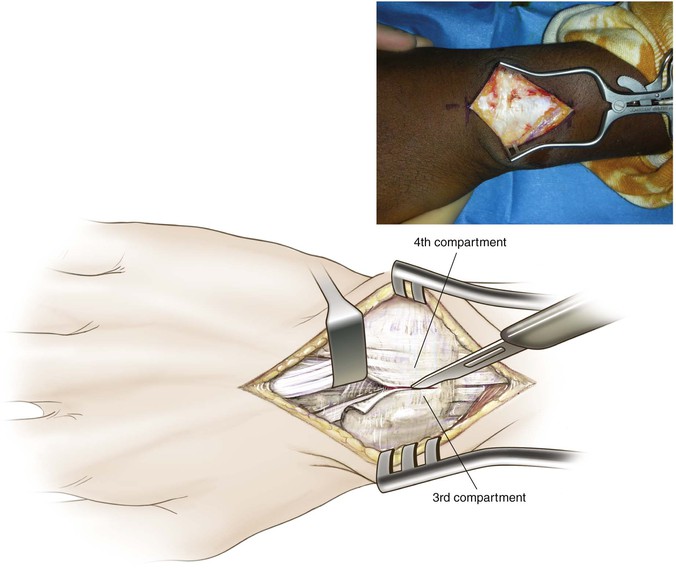
Incise the extensor retinaculum between the third and fourth compartments (see Fig. 4-13)
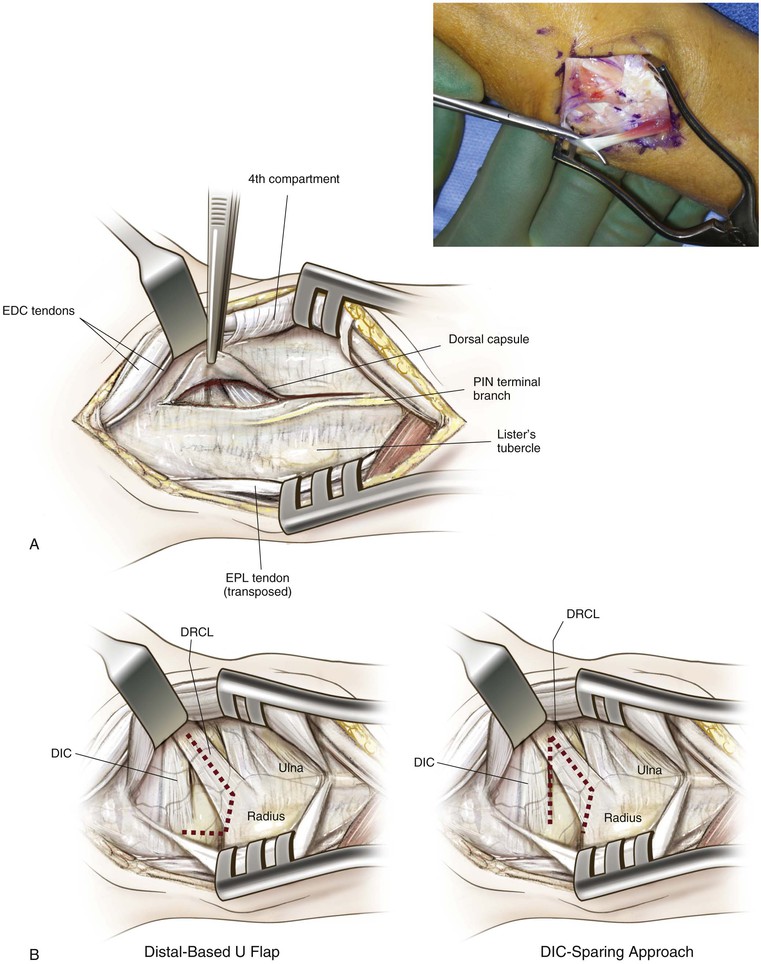
Transpose the EPL and dissect under the extensor compartments but above the joint capsule
• The posterior interosseous nerve terminal branch is in the floor of the fourth extensor compartment
• A posterior interosseous nerve neurectomy can be performed at this point if indicated (Fig. 4-14)
Retract the third and fourth extensor compartments to expose the dorsal extrinsic wrist ligaments and joint capsule (see Fig. 4-14)
Incise the dorsal capsule over the distal radius and extend the incision distally to expose the distal radius, radiocarpal joint, and carpal bones (Fig. 4-15; see Fig. 4-14)
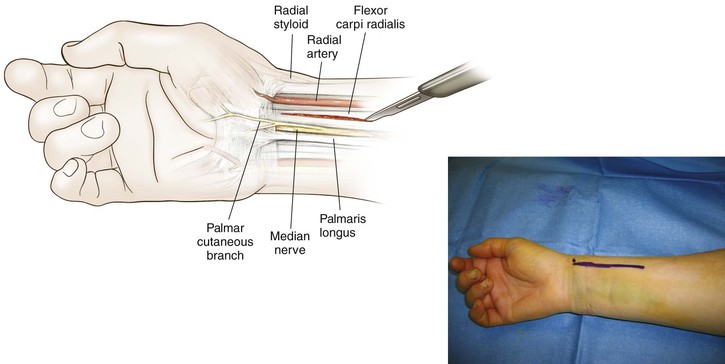
Volar (Henry) Approach to the Wrist
Indications
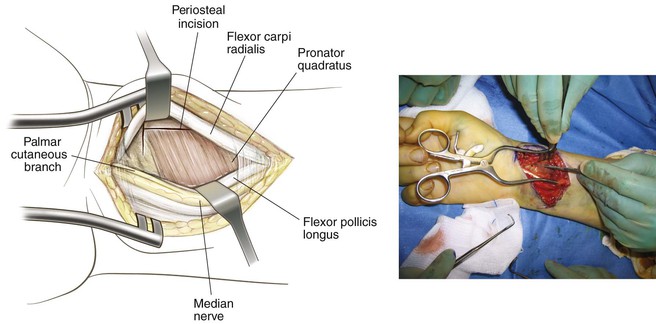
Superficial Dissection (Fig. 4-18)
Incise skin and subcutaneous tissue
• Identify the FCR tendon and radial artery
• Stay on the radial side of the FCR tendon to prevent injury to palmar cutaneous nerve branches
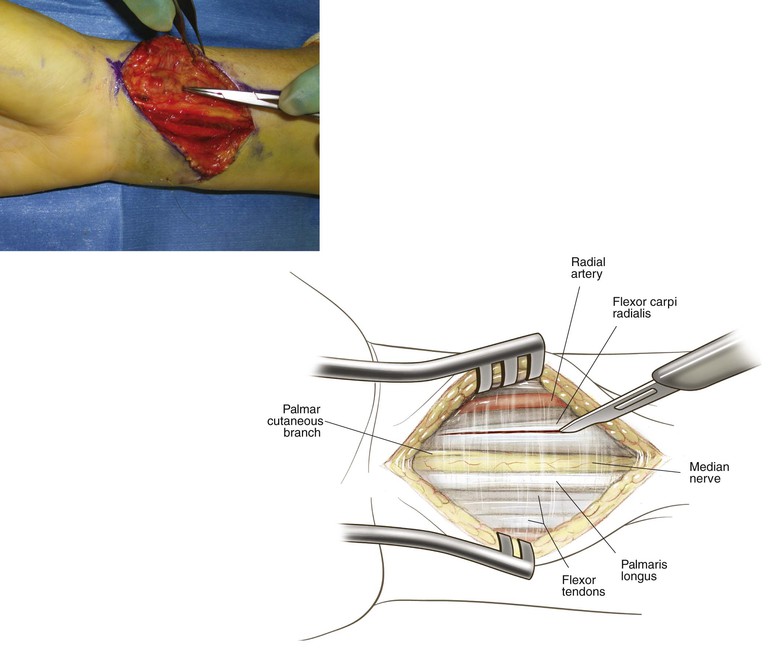
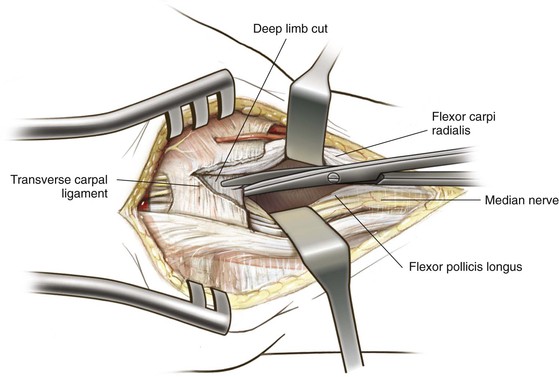
Dissect through the floor of the FCR sheath to expose underlying tendons and identify the median nerve deep to the palmaris longus tendon (Fig. 4-19)
Deep Dissection (See Fig. 4-19)
Retract the FCR radially to protect the radial artery, and retract the FPL and flexor tendons ulnarly to protect the median nerve
• The FCR can be retracted ulnarly if exposure dictates this retraction
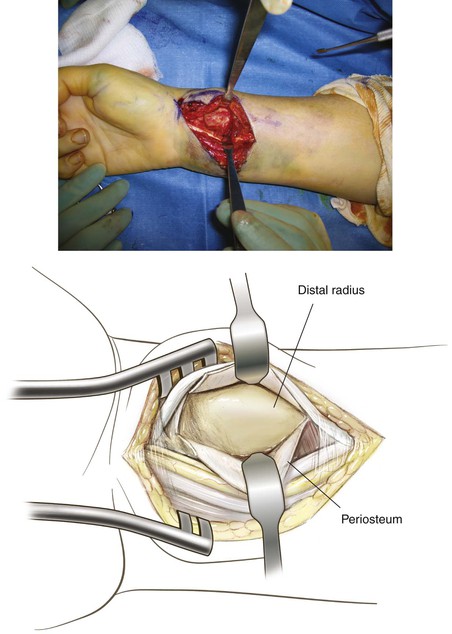
Sharply elevate the pronator quadratus to expose the subperiosteally volar wrist capsule and distal radius
• Hohmann retractors are placed after exposure of the radius (Fig. 4-20)
Extensile Approach (for Exposure of Median Nerve, Distal Radius, and Carpus; Fig. 4-21)
The incision is extended ulnarly at an angle across the wrist crease
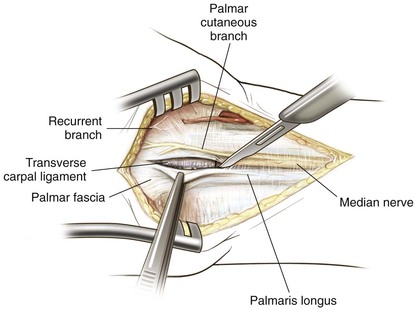
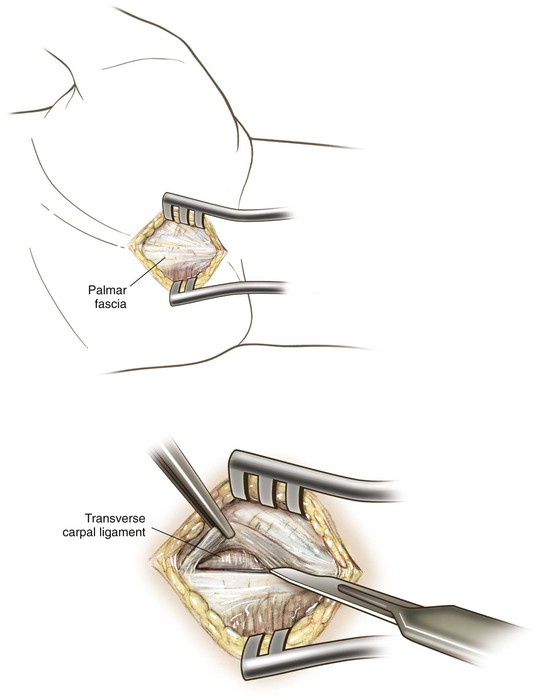
Expose the palmaris longus and palmar fascia (Fig. 4-22)
The palmaris longus tendon is identified
• Release the fascia of the palmaris longus tendon and retract tendons ulnarly to expose the median nerve (Fig. 4-23)
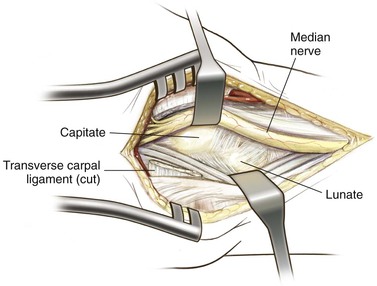
Remain on the ulnar aspect of the median nerve and divide the TCL, protecting the median nerve at all times (Fig. 4-24)
Identify the palmar cutaneous nerve branch and the recurrent motor branch and protect them during exposure
• Retraction of tendons provides access to the volar ligaments and carpus (Fig. 4-25)
Alternate Distal Radius Exposure with Release of the Carpal Tunnel (Hybrid Flexor Carpi Radialis Approach)
Incision
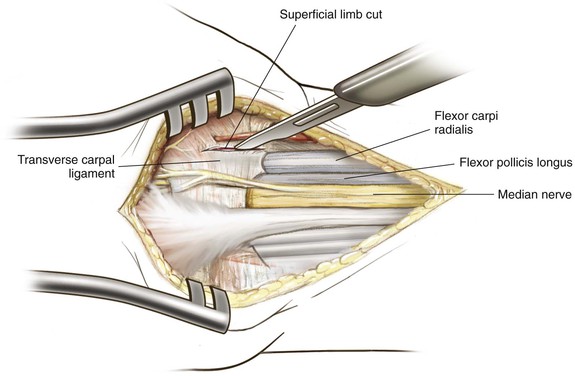
Deep Dissection (Fig. 4-27)
The FPL tendon is identified and retracted ulnarly
Dissection is carried distally, releasing the radial attachments of the TCL
The superficial limb is released along the FCR tendon sheath and off the trapezial ridge
The deep limb is released by sharp dissection along the volar-radial FPL sheath
Complete release of the carpal tunnel is confirmed with digital palpation
The pronator quadratus is released as previously described, exposing the distal radius
Exposure of the Median Nerve in the Palm and Distal Aspect of the Forearm (Video 4-2)
Indications
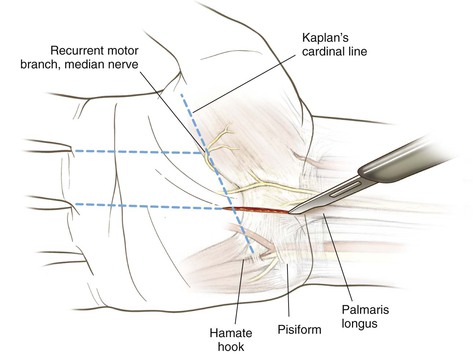
Incision (Fig. 4-29)
Draw Kaplan’s cardinal line from the hook of the hamate to the first web space
Hyperflex the MCP joint of the ring finger past 90 degrees, and flex the PIP and DIP joints to 90 degrees
• From here, the incision extends proximally approximately 2 cm
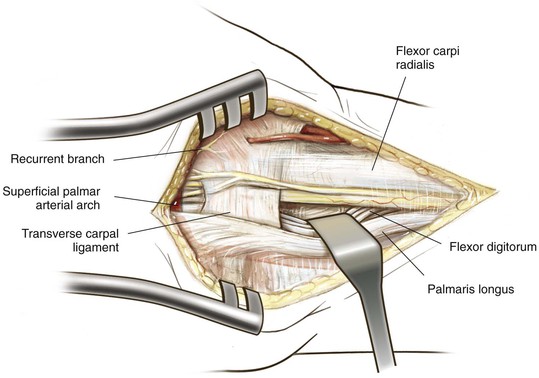
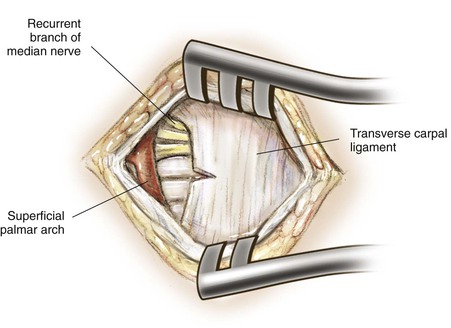
Superficial Dissection (Fig. 4-30)
Deep Dissection (Fig. 4-31)
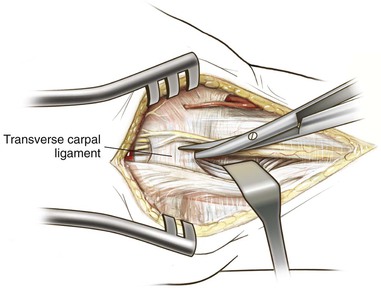
A small, sharp incision is made in the distal aspect of the TCL
• Protect the superficial palmar arch
• Stay in line with the radial aspect of the ring finger to avoid injury to the recurrent motor branch
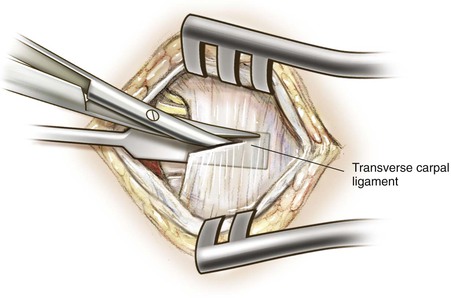
Slide the elevator into the carpal tunnel beneath the TCL to protect the underlying median nerve (Fig. 4-32)
Using scissors with tips pointed ulnarly to protect the median nerve, continue cutting the TCL distal to proximal, then distally (see Fig. 4-32)
Visualize the recurrent motor branch of the median nerve as it enters the thenar musculature and superficial palmar arch to confirm that they are intact (Fig. 4-33)
Proximal Extension
The incision can be extended proximally at an angle across the wrist crease to expose the median nerve in the distal forearm (see Figs. 4-23, 4-24, and 4-25)
• Stay on the ulnar side of the nerve to protect the palmar cutaneous nerve
• Extension of the incision in the forearm can be used to perform a fasciotomy of the volar forearm
Alternate Carpal Tunnel Release: Endoscopic Approach
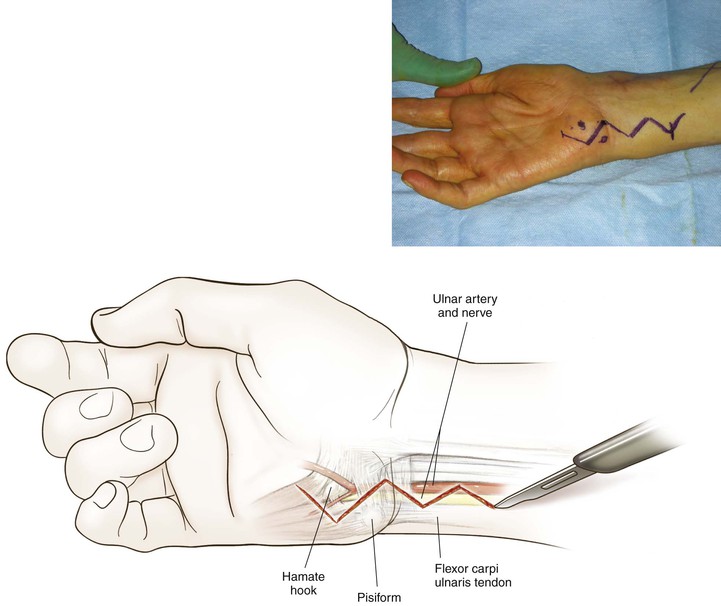
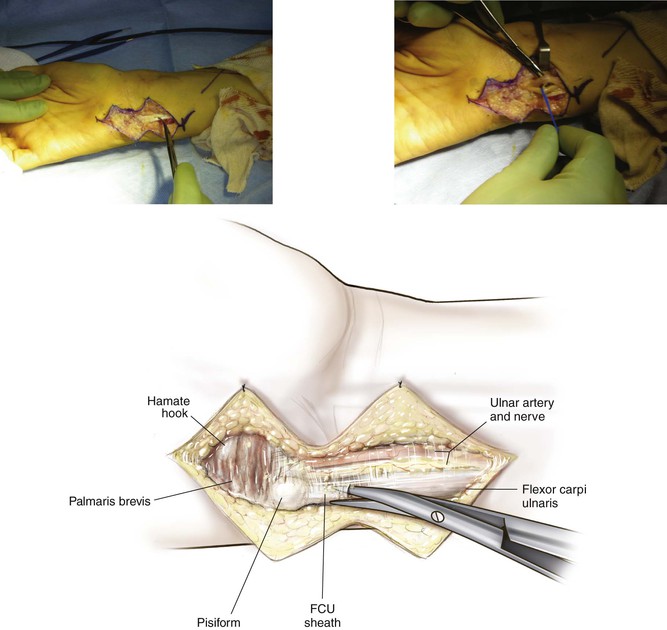
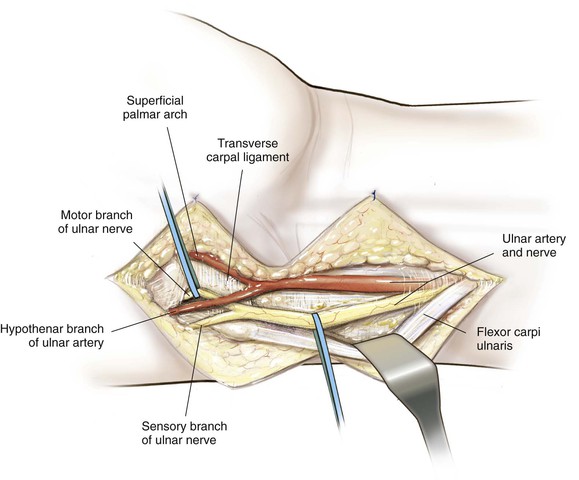
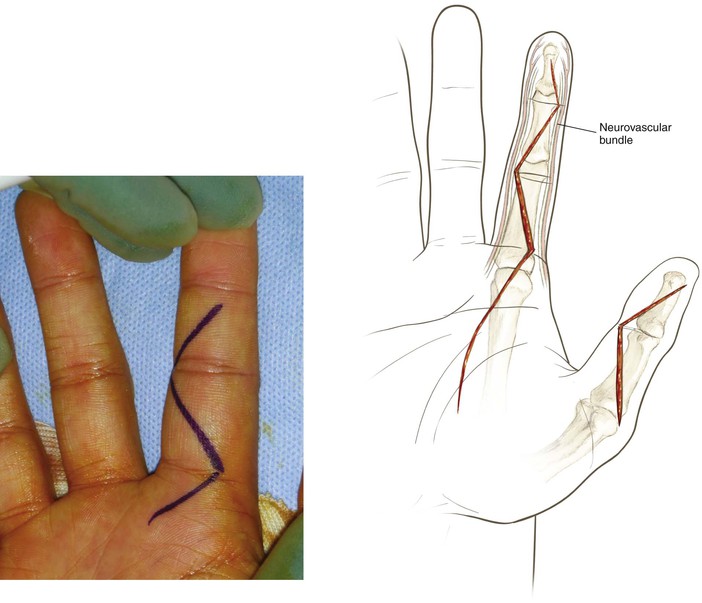
Approach to the Ulnar Nerve and Artery in the Distal Forearm and Palm (Video 4-3)
Indications
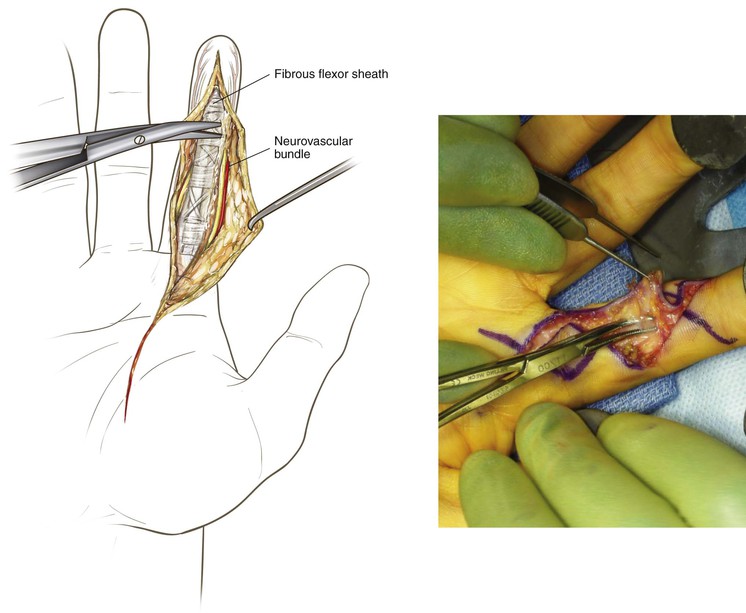
Deep Dissection (Fig. 4-36)
Carefully divide the palmar fascia over the neurovascular structures
The motor branch dives around the hook of the hamate to innervate the intrinsic muscles
• The sensory branch innervates the radial aspect of the ring finger and small finger
For decompression of the Guyon canal, all branches of the ulnar nerve should be decompressed
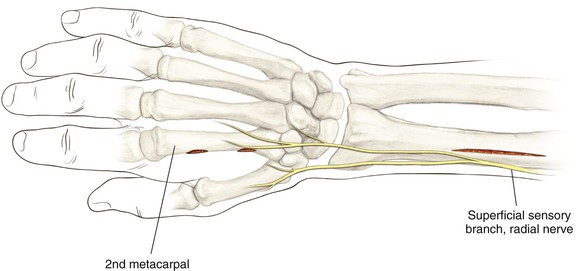
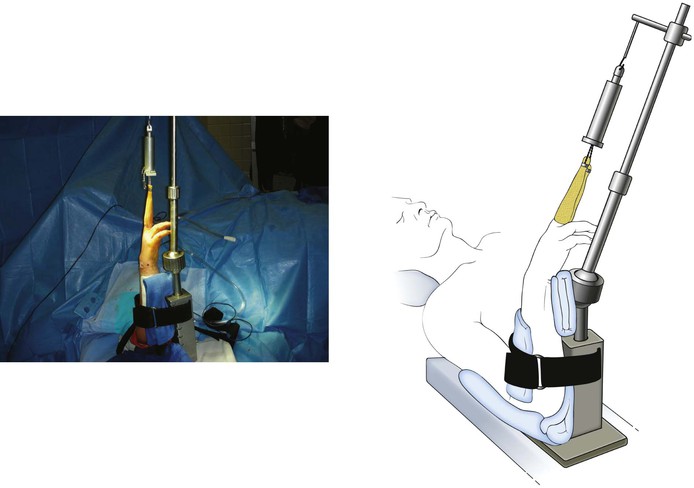
Approach to Apply an External Fixator for the Wrist
Indications
Superficial Dissection (Fig. 4-38)
Skin and subcutaneous tissues overlying the second metacarpal are sharply incised
• Blunt dissection is performed to expose the metacarpal shaft
• The extensor mechanism is protected
Skin and subcutaneous tissues overlying the distal radius are sharply incised
• Blunt dissection is carried down to expose the distal radius
• The superficial sensory radial nerve should be identified and protected
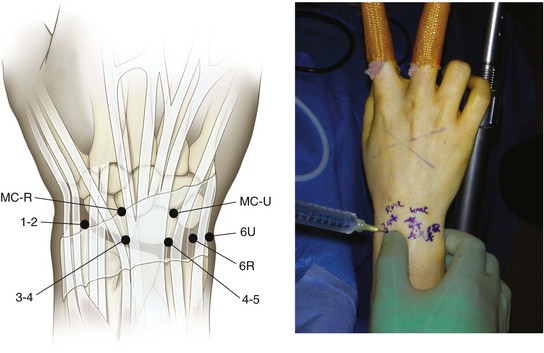
Wrist Arthroscopy
Indications
Dissection
Longitudinal skin incisions are carefully made at the 3-4 interval
• A blunt cannula is carefully introduced into the joint
• An arthroscopic camera is placed, and inflow is connected
• A spinal needle is placed at the 6R interval for outflow
• A diagnostic examination is initiated
Begin the examination radially and progress ulnarly
• Evaluate the radial recess, radial styloid (Fig. 4-42), volar ligaments, scaphoid articular surface, distal radius articular surface (see Fig. 4-42), scapholunate ligament, long and short radiolunate ligaments, lunate (see Fig. 4-42), TFCC, ulnar ligament complex, and dorsal capsule for ganglions (see Fig. 4-42)
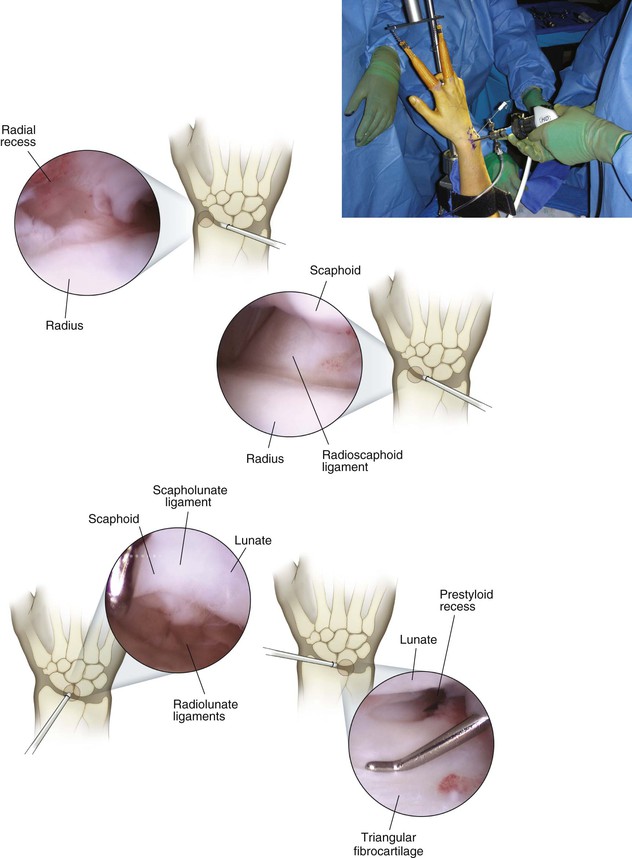
The 4-5 portal is created under direct visualization
• A blunt cannula is gently placed, making sure not to injure the carpal bones
• A probe and shaver are placed through the portal
• The arthroscopic portal can be switched, and the shaver and probe can be placed into the 3-4 portal if needed
• The 6R portal as an alternative viewing and working portal is created under direct visualization
• Allows access/view of TFCC and lunotriquetral ligament disease
A cannula is placed gently to avoid injury to the carpal bones
• The ulnar midcarpal portal is created under direct visualization with a blunt trocar
• The capitohamate joint is identified and is an easily recognizable landmark (Fig. 4-43)
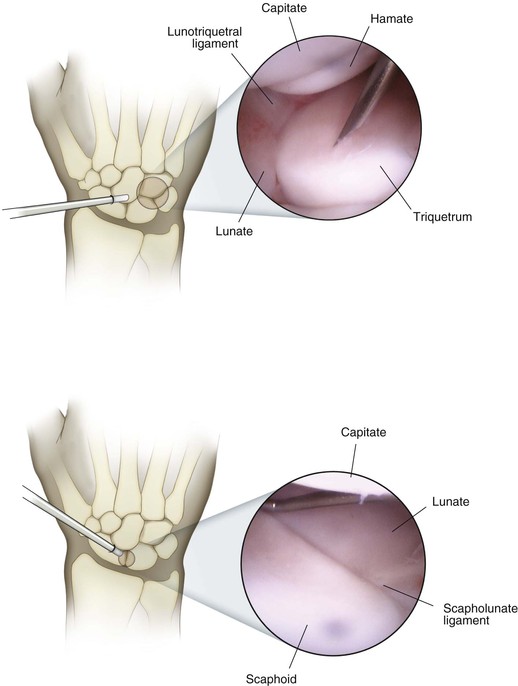
• Volar to the capitohamate joint is the lunotriquetral ligament
• Radially, the scapholunate ligament is identified (see Fig. 4-43)
• The probe is used to evaluate the competency of these ligaments
Closure
Hazards
The dorsal cutaneous ulnar nerve branch is at risk with placement of a 6U portal
The radial artery and superficial sensory radial nerve are at risk with 1-2 portal placement
The extensor tendons can be damaged if appropriate intervals are not used for each portal
Cartilaginous injury to carpal bones or the distal radius can occur with aggressive portal placement
Surgical Approaches to the Hand
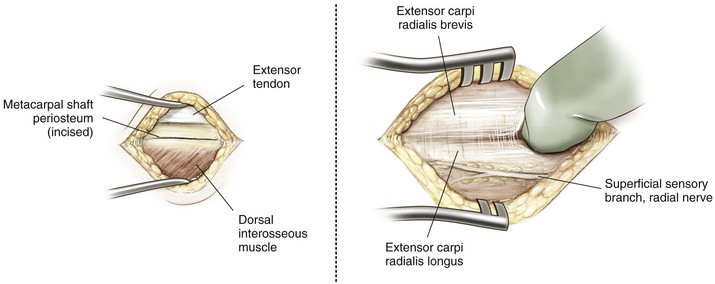
Dorsal Approach to Metacarpals (Video 4-4)
Indications
Deep Dissection
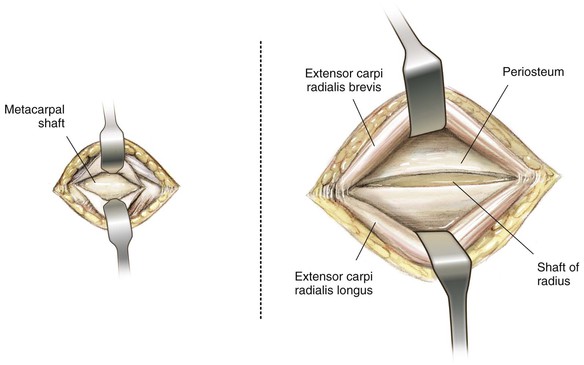
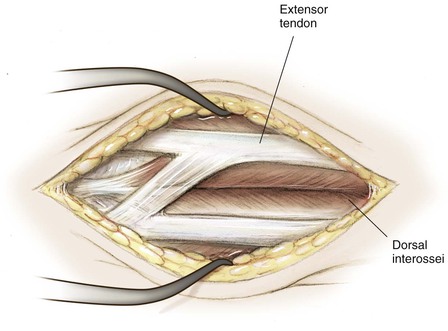
Gently retract the extensor tendon to expose the metacarpal shaft (Fig. 4-46)
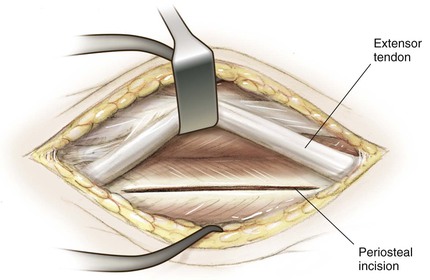
Perform subperiosteal dissection under the extensor mechanism to expose the metacarpal shaft
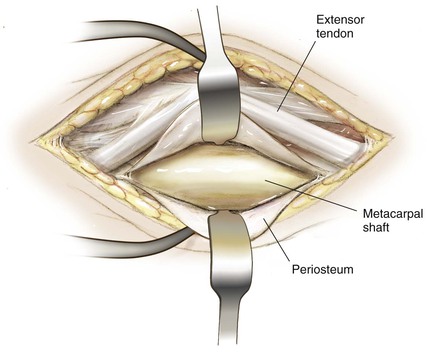
Place small Hohmann retractors to expose the metacarpal shaft (Fig. 4-47)
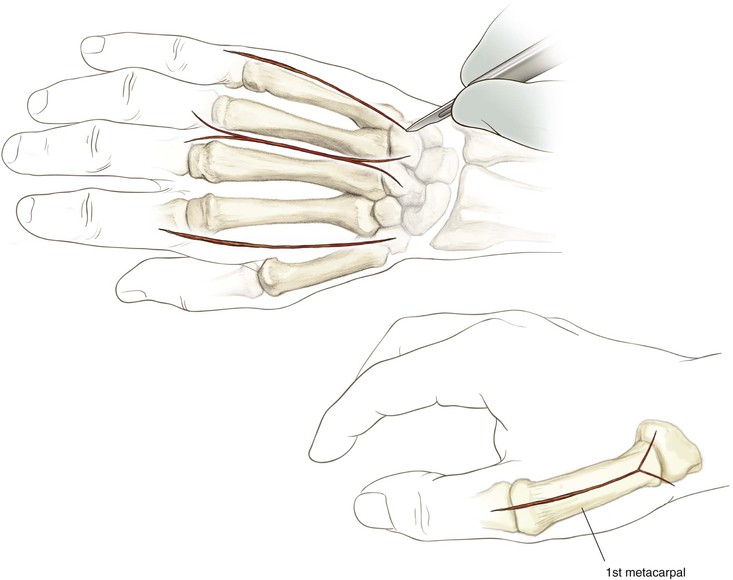
Dorsal Approach to the Fingers (Video 4-5)
Indications
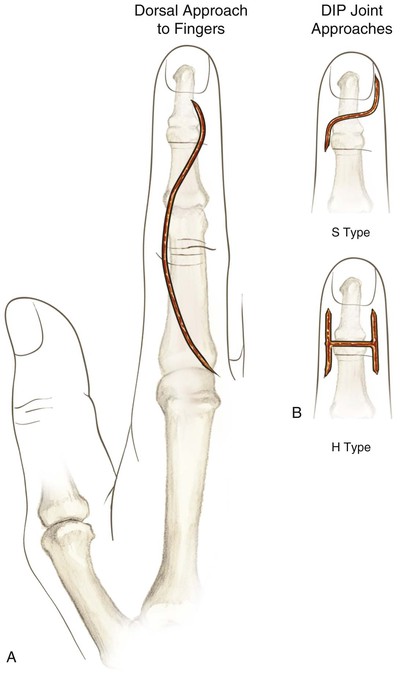
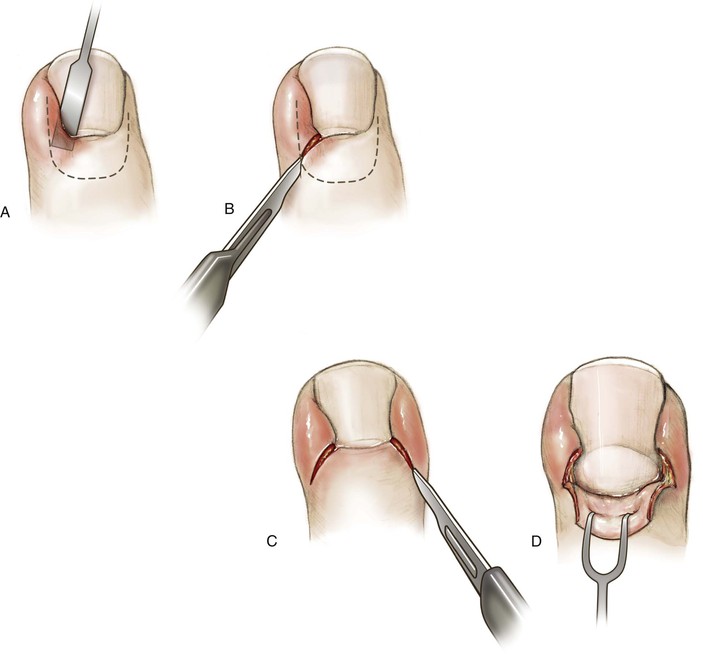
Superficial Dissection (Fig. 4-49)
The extensor hood is incised longitudinally along the radial side and elevated with the extensor tendon to expose the dorsal capsule of the MCP joint
• Subperiosteal dissection is performed to expose the proximal phalanx
• Care should be taken to prevent injury to the central slip insertion
• Small Hohmann retractors are placed
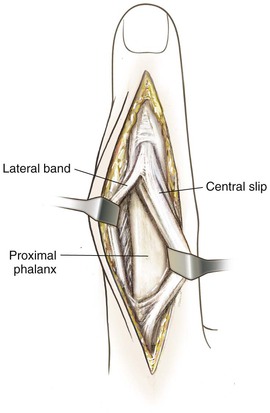
• The middle phalanx can be exposed in a similar manner by dissecting between the central slip and lateral band; the PIP joint can be exposed carefully by gently elevating the extensor tendon to expose the dorsal capsule; insertion of the central slip must be protected (Fig. 4-50)