Wrist
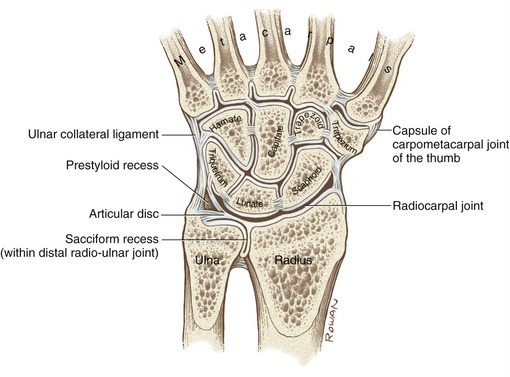
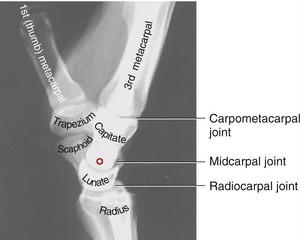
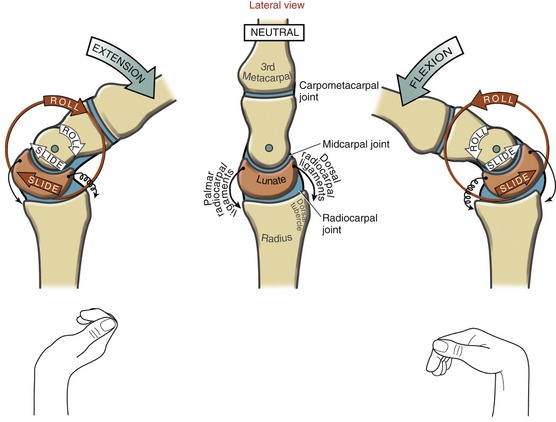
The wrist, or carpus, contains eight carpal bones that, as a group, act as a functional “spacer” between the forearm and hand. In addition to numerous small intercarpal joints, the wrist consists of two primary articulations: the radiocarpal and midcarpal joints (Figure 7-1). The radiocarpal joint is located between the distal end of the radius and the proximal row of carpal bones. Just distal to this joint is the midcarpal joint, joining the proximal and distal rows of carpal bones. The two joints allow the wrist to flex and extend and to move from side to side in motions called radial and ulnar deviation. The nearby distal radio-ulnar joint is considered part of the forearm complex rather than the wrist because of its role in pronation and supination (see Chapter 6).
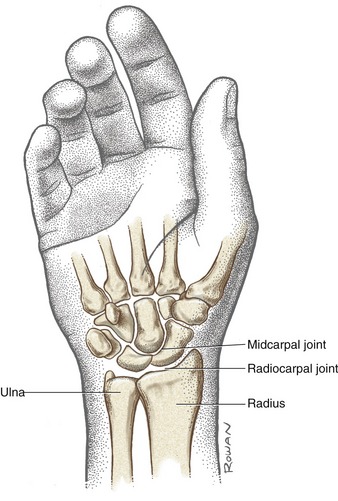
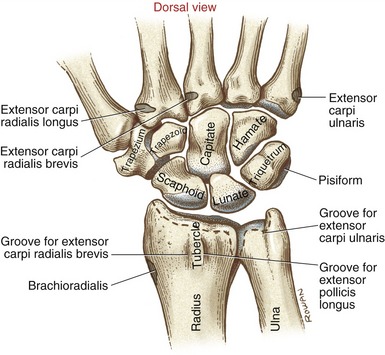
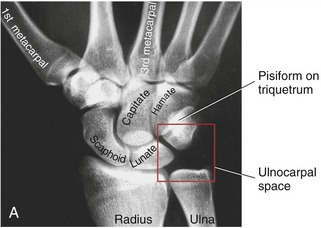
FIGURE 7-1. The bones and major articulations of the wrist.
OSTEOLOGY
The dorsal surface of the distal radius has several grooves and raised areas that help guide or stabilize the tendons that course toward the wrist and hand (Figure 7-2). For example, the palpable dorsal (Lister’s) tubercle separates the tendon of the extensor carpi radialis brevis from the tendon of the extensor pollicis longus.
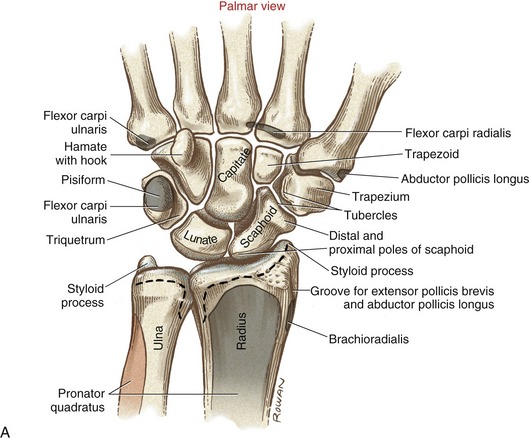
The palmar or volar surface of the distal radius is the location of the proximal attachments of the wrist capsule and the thick palmar radiocarpal ligaments (Figure 7-3, A). The styloid process of the radius projects distally from the lateral side of the radius. The styloid process of the ulna, sharper than its radial counterpart, extends distally from the posterior-medial corner of the distal ulna.
The distal articular surface of the radius is concave in both medial-lateral and anterior-posterior directions (see Figure 6-26, B). Facets are formed in the articular cartilage from indentations made by the scaphoid and lunate bones of the wrist.
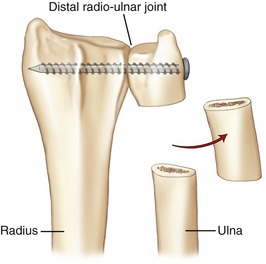
Fractures of the distal end of the radius with a dorsal displacement of the distal fragment are very common. A frequent mechanism for this injury is a fall over an outstretched hand. A fracture that heals in an abnormally aligned fashion can significantly alter the congruence, or fit, of both the distal radio-ulnar joint and the radiocarpal joint of the wrist.36,59 Depending on the nature of the incongruence, the joints may become unstable (especially the distal radio-ulnar joint) or may develop degenerative arthritis from altered contact pressure at the articular surfaces.
Abnormal alignment of the distal radius also can change the relationship between the axis of rotation of the forearm and the interosseous membrane. If the misalignment is severe, the interosseous membrane may restrict the full extent of pronation or supination.36
The distal end of the radius has two configurations of biomechanical importance. First, the distal end of the radius angles about 25 degrees toward the ulnar (medial) direction (Figure 7-4, A). This ulnar tilt allows the wrist and hand to rotate farther into ulnar deviation than into radial deviation. As a result of this tilt, radial deviation of the wrist is limited by impingement of the lateral side of the carpus against the styloid process of the radius. Second, the distal articular surface of the radius is angled about 10 degrees in the palmar direction (see Figure 7-4, B). This palmar tilt accounts, in part, for the greater amounts of flexion than extension at the wrist.
Carpal Bones
From a radial (lateral) to ulnar direction, the proximal row of carpal bones includes the scaphoid, lunate, triquetrum, and pisiform. The distal row includes the trapezium, trapezoid, capitate, and hamate (Figures 7-2 and 7-3).
SCAPHOID
The naming of the scaphoid is based on its vague resemblance to a boat (scaphoid from the Greek skaphoeides, like a boat). Most of the “hull” or undersurface of the boat rides on the radius; the cargo area of the “boat” is filled with part of the head of the capitate (see Figure 7-3, A). The scaphoid contacts four carpal bones and the radius.
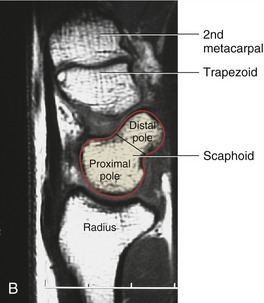
The scaphoid has two convex surfaces called poles. The proximal pole articulates with the scaphoid facet of the radius (see Figure 6-26, B). The distal pole has a slightly rounded surface, which articulates with the trapezium and trapezoid. The distal pole projects obliquely palmarly, which can be well appreciated from a sagittal plane slice provided by magnetic resonance imaging (MRI) (see Figure 7-3, B). The distal pole has a blunt tubercle, which is palpable at the palmar base of the thenar musculature. Because of its elongated shape, the scaphoid is functionally and anatomically associated with both rows of carpal bones.7
The distal-medial surface of the scaphoid is deeply concave to accept the lateral half of the prominent head of the capitate bone (see Figure 7-3, A). A small facet on the scaphoid’s medial side articulates with the lunate. This articulation, reinforced primarily by the scapholunate ligament, provides an important mechanical link within the proximal row of carpal bones—a point to be revisited later in this chapter.
LUNATE
Like the scaphoid, the lunate’s proximal surface is convex, fitting into the concave facet on the radius (see Figure 6-26, B). The distal surface of the lunate is deeply concave, giving the bone its crescent moon–shaped appearance (see Figure 7-3, A). This articular surface accepts two convexities: the medial half of the head of the capitate and part of the apex of the hamate.
CAPITATE
The capitate is the largest of all carpal bones. This bone occupies a central location within the wrist, making articular contact with seven surrounding bones when considering the metacarpals (see Figure 7-3, A). The word capitate is derived from the Latin root meaning head, which describes the shape of the bone’s prominent proximal surface. The large head articulates with the deep concavity provided by the scaphoid and lunate. The capitate is well stabilized between the hamate and trapezoid by short but strong ligaments.
TRAPEZIUM
A slender and sharp tubercle projects from the palmar surface of the trapezium. This tubercle, along with the palmar tubercle of the scaphoid, provides attachment for the lateral side of the transverse carpal ligament (see Figure 7-5). Immediately medial to the palmar tubercle is a distinct groove for the tendon of the flexor carpi radialis.
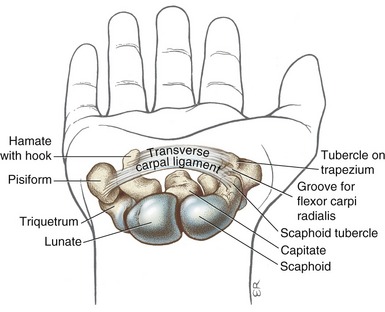
Carpal Tunnel
As illustrated in Figure 7-5, the palmar side of the carpal bones forms a concavity. Arching over this concavity is a thick fibrous band of connective tissue known as the transverse carpal ligament. This ligament is connected to four raised points on the palmar carpus, namely, the pisiform and the hook of the hamate on the ulnar side, and the tubercles of the scaphoid and the trapezium on the radial side. The transverse carpal ligament serves as a primary attachment site for many muscles located within the hand and the palmaris longus, a wrist flexor muscle.
ARTHROLOGY
Joint Structure and Ligaments of the Wrist
JOINT STRUCTURE
As illustrated in Figure 7-1, the two primary articulations within the wrist are the radiocarpal and midcarpal joints. Many other intercarpal joints also exist between adjacent carpal bones (see Figure 7-7). Intercarpal joints contribute to wrist motion through small gliding and rotary motions. Compared with the large range of motion permitted at the radiocarpal and midcarpal joints, motion at the intercarpal joints is relatively small but nevertheless essential for normal wrist motion.
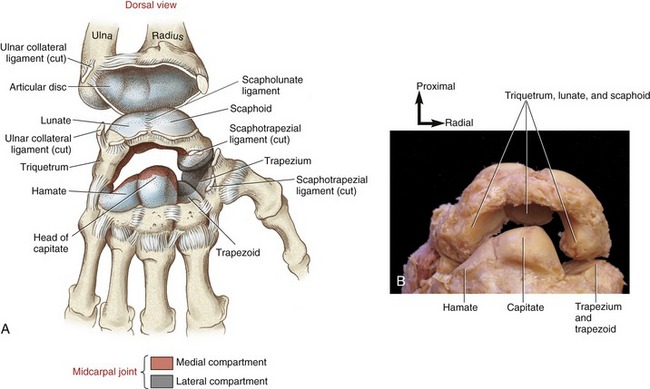
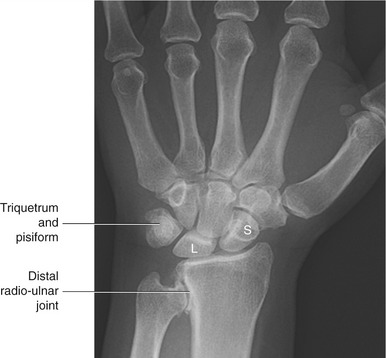
Radiocarpal Joint: The proximal components of the radiocarpal joint are the concave surfaces of the radius and an adjacent articular disc (Figures 7-7 and 7-8). As described in Chapter 6, this articular disc (also called the triangular fibrocartilage) is an integral part of the distal radio-ulnar joint. The distal components of the radiocarpal joint are the convex proximal surfaces of the scaphoid and the lunate. The triquetrum is also considered part of the radiocarpal joint because at full ulnar deviation its medial surface contacts the articular disc.
The thick articular surface of the distal radius and the articular disc accept and disperse the forces that cross the wrist. Approximately 20% of the total compression force that crosses the radiocarpal joint passes through the articular disc. The remaining 80% passes directly through the scaphoid and lunate to the radius.58 The contact areas at the radiocarpal joint tend to be greatest when the wrist is partially extended and ulnarly deviated.42 This is also the wrist position at which maximal grip strength is obtained.
Midcarpal Joint: The midcarpal joint is the articulation between the proximal and distal rows of carpal bones (see Figure 7-8). The capsule that surrounds the midcarpal joint is continuous with each of the many intercarpal joints.
The midcarpal joint can be divided descriptively into medial and lateral joint compartments.78 The larger medial compartment is formed by the convex head of the capitate and apex of the hamate, fitting into the concave recess formed by the distal surfaces of the scaphoid, lunate, and triquetrum (see Figure 7-8). The head of the capitate fits into this concave recess much like a ball-and-socket joint.
The lateral compartment of the midcarpal joint is formed by the junction of the slightly convex distal pole of the scaphoid with the slightly concave proximal surfaces of the trapezium and the trapezoid (see Figure 7-8). The lateral compartment lacks the pronounced ovoid shape of the medial compartment. Cineradiography of wrist motion shows less movement at the lateral than the medial compartment.52 For this reason, subsequent arthrokinematic analysis of the midcarpal joint focuses on the medial compartment.
WRIST LIGAMENTS
Many of the ligaments of the wrist are small and difficult to isolate. Their inconspicuous nature should not, however, minimize their extreme kinesiologic importance. Wrist ligaments are essential to maintaining the natural intercarpal alignment and for transferring forces within and across the carpus. Muscle-produced forces stored in stretched ligaments provide important control to the complex arthrokinematics of the wrist. Ligaments also supply sensory feedback to activated muscles.28 Ligaments damaged through injury and disease leave the wrist vulnerable to weakness, deformity, instability, and degenerative arthritis.
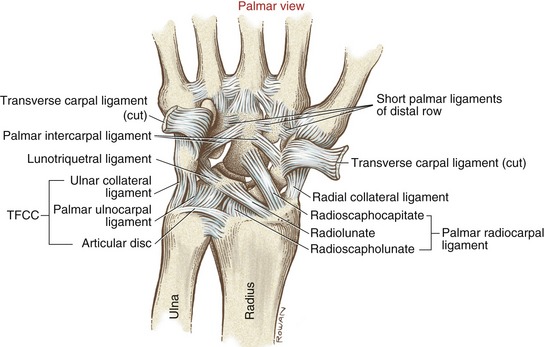
Wrist ligaments are classified as extrinsic or intrinsic (Box 7-1). Extrinsic ligaments have their proximal attachments on the forearm but attach distally within the wrist. As noted in Box 7-1, the triangular fibrocartilage complex (introduced previously in Chapter 6) includes structures associated with the wrist and the distal radio-ulnar joint. Intrinsic ligaments have both their proximal and distal attachments within the wrist. More detailed or alternative descriptions of these ligaments can be found in other sources.6,78
Extrinsic Ligaments: A fibrous capsule surrounds the external surfaces of both the wrist and the distal radio-ulnar joint. Dorsally, the capsule thickens slightly to form the dorsal radiocarpal ligament (Figure 7-9). This ligament is thin and not easily distinguishable from the capsule itself. In general, the dorsal radiocarpal ligament courses distally in an ulnarly direction, attaching primarily between the distal radius and the dorsal surfaces of the lunate and triquetrum.73,77 The dorsal radiocarpal ligament reinforces the posterior side of the radiocarpal joint and helps guide the natural arthrokinematics, especially of the bones in the proximal row.77 The fibers that attach to the lunate provide an especially important restraint against anterior (volar) dislocation of this inherently unstable bone.86

FIGURE 7-9. The primary dorsal ligaments of the right wrist.
Taleisnik originally described the thickening of the external surface of the lateral-palmer part of the capsule of the wrist as the radial collateral ligament (Figure 7-10).80 More recent anatomic descriptions, however, typically do not include the radial collateral ligament as a distinct anatomic entity.6 This connective tissue, regardless of its name, likely provides little lateral stability to the wrist. Extrinsic muscles, such as the abductor pollicis longus and the extensor pollicis brevis, perform most of this function.
Deep and separate from the palmar capsule of the wrist are several stout and extensive ligaments known collectively as the palmar radiocarpal ligaments. Three ligaments are typically described within this set: the radioscaphocapitate, the radiolunate, and, in a deeper plane, the radioscapholunate (see Figure 7-10).78 The palmar radiocarpal ligaments are much stronger and thicker than their dorsal counterparts.80 In general, each ligament arises from a roughened area on the distal radius, travels distally in a generally ulnar direction, and attaches to the palmar surface of several carpal bones. The radioscaphocapitate—the most lateral ligament of this set—often partially blends with the radial collateral ligament.
The palmar radiocarpal ligaments become maximally taut at full wrist extension.44 Passive tension exists in these ligaments even in the relaxed neutral wrist position.88 An example of the role these ligaments play in guiding the arthrokinematics of the wrist will be provided later in this chapter.
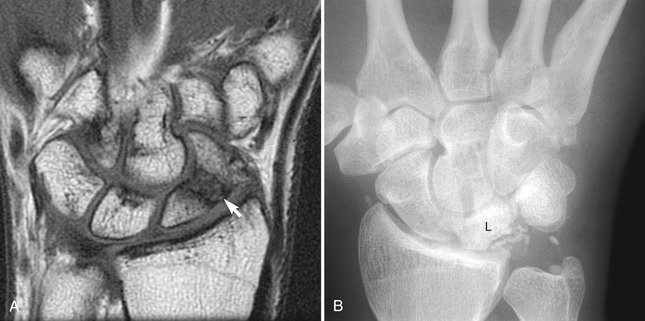
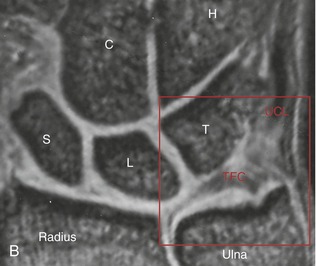
Although the ulnocarpal space appears empty on a standard radiograph (Figure 7-11, A), it is actually filled with at least five interconnected tissues, known collectively as the triangular fibrocartilage complex (TFCC) (see Box 7-1). The primary component of the TFCC is the triangular fibrocartilage—the previously described articular disc located within both the distal radio-ulnar and the radiocarpal joints (see Figure 7-11, B).
The primary global function of the TFCC is to securely bind the distal ends of the radius and ulna while simultaneously permitting the radius, with attached carpus, to freely rotate (pronate and supinate) around a fixed ulna. A summary of the more specific functions of the TFCC is included in Box 7-2. Anatomic details of the components of the TFCC are described in the following paragraphs.
The triangular fibrocartilage (TFC) attaches directly or indirectly to all components of the TFCC and therefore forms the structural backbone of the entire complex. The TFC is a biconcave articular disc, composed chiefly of fibrocartilage.78 The name “triangular” refers to the shape of the disc: its base attaches along the ulnar notch of the radius, and its apex attaches near the styloid process of the ulna (see Figure 6-26, A). The sides of the “triangle” are formed by the palmar and dorsal capsular ligaments of the distal radio-ulnar joint.25 The disc’s proximal surface accepts the head of the ulna at the distal radio-ulnar joint, and its distal surface accepts the convex surfaces of part of the lunate and the triquetrum at the radiocarpal joint (see Figures 6-26, 7-7, and 7-8, A). The central 80% of the disc is avascular with little or no healing potential.13
The palmar ulnocarpal ligament originates from the palmar edge of the articular disc and adjacent palmar aspect of the distal radio-ulnar joint capsule (see Figure 7-10).31 From this common proximal attachment the tissue splits into two distinct ligaments: ulnolunate and ulnotriquetral.
The ulnar collateral ligament represents a thickening of the medial aspect of the capsule of the wrist31,80 (see Figure 7-10). (According to the British edition of Gray’s Anatomy, the ulnar collateral ligament and the juxtaposed ulnotriquetral ligament are part of the same structure.78) Along with the flexor and extensor carpi ulnaris muscles, the palmar ulnocarpal and ulnar collateral ligaments reinforce the ulnar side of the wrist. These ligaments must be sufficiently flexible, however, to allow the radius and hand to rotate freely around the fixed ulna during pronation and supination.
The final component yet to be described within the TFCC is a poorly organized and defined connective tissue substance known as the meniscus homologue.31 This tissue likely represents the vestige of a more primitive embryonic connective tissue within the ulnar side of the wrist.78 Referred to as a “cartilaginous filler,”80 the meniscus homologue fills gaps within and immediately medial to the prestyloid recess of the ulnocarpal space (see Figure 7-7). The synovial lining within this recess often becomes distended and painful with rheumatoid arthritis. Tears in the articular disc may permit synovial fluid to spread from the radiocarpal joint to the distal radio-ulnar joint.
Intrinsic Ligaments: The primary intrinsic ligaments of the wrist can be classified into three sets: short, intermediate, or long (see Box 7-1).80 Short ligaments connect the bones of the distal row by their palmar, dorsal, or interosseous surfaces (see Figures 7-9 and 7-10). The short ligaments firmly stabilize and unite the distal row of bones, permitting them to function essentially as a single mechanical unit.
Three intermediate ligaments exist within the wrist. The lunotriquetral ligament is a fibrous continuation of the palmar radiolunate ligament (see Figure 7-10). The scapholunate ligament is a broad collection of fibers that forms the primary bond between the scaphoid and the lunate (see Figure 7-8, A).76 Several scaphotrapezial ligaments reinforce the articulation between the scaphoid and the trapezium (see Figure 7-9).
Two relatively long ligaments are present within the wrist. The palmar intercarpal ligament firmly attaches to the palmar surface of the capitate bone (see Figure 7-10). From this common attachment the ligament bifurcates proximally, forming two discrete fiber groups that resemble the shape of an inverted V. The lateral leg of the inverted V attaches to the scaphoid, and the medial leg to the triquetrum. These ligaments help guide the arthrokinematics of the wrist.
Lastly, a thin dorsal intercarpal ligament provides transverse stability to the wrist by interconnecting the trapezium, scaphoid, lunate, and triquetrum (see Figure 7-9).46,85
Kinematics of Wrist Motion
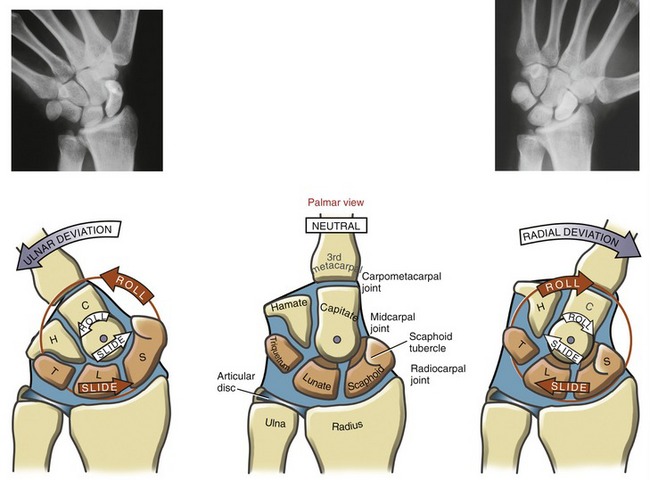
The osteokinematics of the wrist are defined for 2 degrees of freedom: flexion-extension and ulnar-radial deviation (Figure 7-12). Wrist circumduction—a full circular motion made by the wrist—is a combination of the aforementioned movements, not a distinct third degree of freedom.
Most natural dynamic movements of the wrist combine elements of both frontal and sagittal planes: extension tends to occur with radial deviation, and flexion with ulnar deviation.41 The resulting natural path of motion for the wrist follows a slightly oblique path, similar to a dart thrower’s motion.50 This natural combination of movements occurs with other functions, such as tying shoelaces or combing hair. These natural kinematics should be considered during rehabilitation of the wrist after injury.
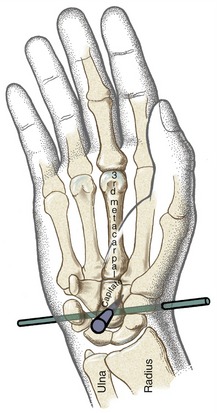
The axis of rotation for wrist movements is reported to pass through the head of the capitate (Figure 7-13).94 Generally, the axis runs in a near medial-lateral direction for flexion and extension and near anterior-posterior direction for radial and ulnar deviation. Although the axes are depicted as stationary, in reality they migrate slightly throughout the full range of motion.60 The firm articulation between the capitate and the base of the third metacarpal bone causes the rotation of the capitate to direct the osteokinematic path of the entire hand.
The wrist rotates in the sagittal plane about 130 to 160 degrees (see Figure 7-12, A). On average, the wrist flexes from 0 degrees to about 70 to 85 degrees and extends from 0 degrees to about 60 to 75 degrees.67,69 As with any diarthrodial joint, wrist range of motion varies with age and health and whether the motion is performed actively or passively. Total flexion normally exceeds extension by about 10 to 15 degrees. End-range extension is naturally limited by stiffness in the thick palmar radiocarpal ligaments. In some persons, a greater than average palmar tilt of the distal radius may also limit extension range (see Figure 7-4, B).
The wrist rotates in the frontal plane approximately 50 to 60 degrees (see Figure 7-12, B).67,94 Radial and ulnar deviation of the wrist is measured as the angle between the radius and the shaft of the third metacarpal. Ulnar deviation occurs from 0 degrees to about 35 to 40 degrees. Radial deviation occurs from 0 degrees to about 15 to 20 degrees. Primarily because of the ulnar tilt of the distal radius (see Figure 7-4, A), maximum ulnar deviation normally is double the maximum amount of radial deviation.
Ryu and colleagues tested 40 healthy subjects using a biaxial electrogoniometer to determine the range of wrist motion needed to perform 24 activities of daily living (ADLs).67 The ADLs included personal care, hygiene, food preparation, writing, and using various tools or utensils. The researchers concluded that these ADLs could be comfortably performed using 40 degrees of flexion, 40 degrees of extension, 10 degrees of radial deviation, and 30 degrees of ulnar deviation. These functional ranges were 50% to 80% of the subjects’ maximal range of wrist motion.
Medical management of a severely painful or unstable wrist may require surgical fusion.14 To minimize the functional impairment associated with this procedure, the wrist is often fused in an “average” position of function: about 10 to 15 degrees of extension and 10 degrees of ulnar deviation.68 Although permanently fusing a wrist (even partially) may seem like a radical option, the procedure may be the only treatment that can achieve stability and relieve pain.
ARTHROKINEMATICS
Many different methodologies have been used to study the kinematics of the wrist; these include in vitro and, more recently, in vivo techniques.47,51 These techniques include the following:
Even with these sophisticated techniques, the resulting data describing the kinematics across the regions of the wrist are inconsistent. Precise and repeatable descriptions of the kinematics are hampered by the complexity of the anatomy and the movement (up to eight small bones experiencing multiplanar rotations and translations) and by natural human variation. Although much has been learned over the last two decades, the study of carpal kinematics continues to evolve.*
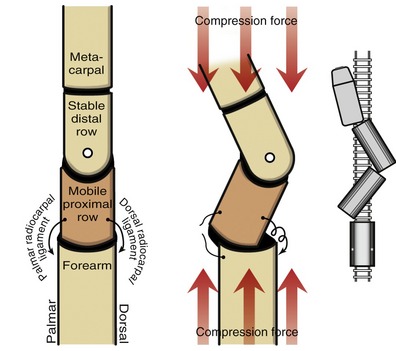
Wrist Extension and Flexion: The essential kinematics of sagittal plane motion at the wrist can be appreciated by visualizing the wrist as an articulated central column, formed by the linkages between the distal radius, lunate, capitate, and third metacarpal (Figure 7-14). Within this column, the radiocarpal joint is represented by the articulation between the radius and lunate, and the medial compartment of the midcarpal joint is represented by the articulation between the lunate and capitate. The carpometacarpal joint is a semirigid articulation formed between the capitate and the base of the third metacarpal.
Dynamic Interaction within the Joints of the Central Column of the Wrist: The arthrokinematics of extension and flexion are based on synchronous convex-on-concave rotations at both the radiocarpal and the midcarpal joints. At the radiocarpal joint depicted in red in Figure 7-15, extension occurs as the convex surface of the lunate rolls dorsally on the radius and simultaneously slides palmarly. The rolling motion directs the lunate’s distal surface dorsally, toward the direction of extension. At the midcarpal joint, illustrated in white in Figure 7-15, the head of the capitate rolls dorsally on the lunate and simultaneously slides in a palmar direction. Combining the arthrokinematics over both joints produces full wrist extension. This two-joint system has the advantage of yielding a significant total range of motion by requiring only moderate amounts of rotation at the individual joints. Mechanically, therefore, each joint moves within a relatively limited—and therefore more stable—arc of motion.
Full wrist extension elongates the palmar radiocarpal ligaments and all muscles that cross on the palmar side of the wrist. Tension within these stretched structures helps stabilize the wrist in its close-packed position of full extension.43,44 Stability in full wrist extension is useful when weight is borne through the upper extremity during activities such as crawling on the hands and knees and transferring one’s own body from a wheelchair to a bed.
The arthrokinematics of wrist flexion are similar to those described for extension but occur in a reverse fashion (see Figure 7-15).
Studies quantifying the individual angular contributions of the radiocarpal and midcarpal joints to the total sagittal plane motion of the wrist cite inconsistent data.* With few exceptions, however, most studies report synchronous and roughly equal—or at least significant—contributions from both joints.
Using the simplified central column model to describe flexion and extension of the wrist offers an excellent conceptualization of a rather complex event. A limitation of the model, however, is that it does not account for all the carpal bones that participate in the motion. For instance, the model ignores the kinematics of the scaphoid bone at the radiocarpal joint. In brief, the arthrokinematics of the scaphoid on the radius are similar to those of the lunate during flexion and extension, except for one feature. Based on the different size and curvature of the two bones, the scaphoid rolls on the radius at a different speed than the lunate.66 This difference causes a slight displacement between the scaphoid and lunate by the end of full motion. Normally, in the healthy wrist, the amount of displacement is minimized by the restraining action of ligaments, especially the scapholunate ligament (see Figure 7-8, A). Rupture of this important ligament occurs relatively frequently and can significantly alter the arthrokinematics and transfer of force within the proximal row of carpal bones.81,91 Damage to this ligament can occur through trauma, chronic synovitis from rheumatoid arthritis,5 or even surgical removal of a ganglion cyst.
Ulnar and Radial Deviation of the Wrist:
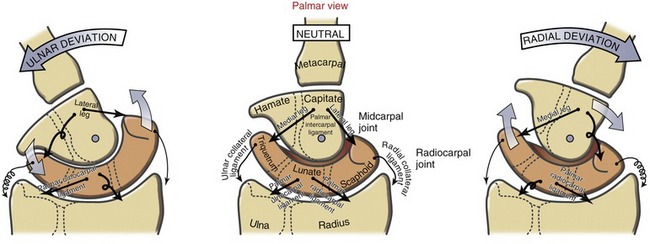
Dynamic Interaction between the Radiocarpal and Midcarpal Joints: Like flexion and extension, ulnar and radial deviation occurs through synchronous convex-on-concave rotations at both radiocarpal and midcarpal joints. During ulnar deviation, the midcarpal joint and, to a lesser extent, the radiocarpal joint contribute to overall wrist motion (Figure 7-16).35 At the radiocarpal joint shown in red in Figure 7-16, the scaphoid, lunate, and triquetrum roll ulnarly and slide a significant distance radially. The extent of this radial slide is apparent by the final position of the lunate relative to the radius at full ulnar deviation. Ulnar deviation at the midcarpal joint occurs primarily from the capitate rolling ulnarly and sliding slightly radially.
Radial deviation at the wrist occurs through similar arthrokinematics as described for ulnar deviation (see Figure 7-16). The amount of radial deviation at the radiocarpal joint is limited as the radial side of the carpus impinges against the styloid process of the radius. Consequently, a greater amount of the radial deviation occurs at the midcarpal joint.35
Using magnetic resonance imaging, Moritomo and colleagues specifically measured the three-dimensional movement at the midcarpal joint during radial and ulnar deviation.51 They reported a kinematic association between radial deviation and slight extension, and ulnar deviation and slight flexion. This “dart-throwing” movement pattern observed at the midcarpal joint is similar to that observed during many natural wrist movements.
Additional Arthrokinematics Involving the Proximal Row of Carpal Bones: Careful observation of ulnar and radial deviation using cineradiography or serial static radiographs reveals more complicated arthrokinematics than previously described. During these frontal plane movements, the proximal row of carpal bones “rock” slightly into flexion and extension and, to a much lesser extent, “twist.” The rocking motion is most noticeable in the scaphoid and, to a lesser extent, the lunate. During radial deviation the proximal row flexes slightly; during ulnar deviation the proximal row extends slightly.35,37 Note in Figure 7-16, especially on the radiograph, the change in position of the scaphoid tubercle between the extremes of ulnar and radial deviation. According to Moojen and co-workers, at 20 degrees of ulnar deviation the scaphoid is rotated about 20 degrees into extension, relative to the radius.47 The scaphoid appears to “stand up” or to lengthen, which projects its tubercle distally. At 20 degrees of radial deviation, the scaphoid flexes beyond neutral about 15 degrees, taking on a shortened stature with its tubercle having approached the radius. A functional shortening of the scaphoid allows a few more degrees of radial deviation before complete blockage against the styloid process of the radius. The exact mechanism responsible for the flexion and extension of the proximal carpal row during ulnar and radial deviation is not fully understood, but many explanations have been offered.66 Most likely, the mechanism is driven by passive forces in ligaments and compressions between adjacent carpal bones.
Carpal Instability
An unstable wrist demonstrates malalignment of one or more carpal bones, typically associated with abnormal and painful kinematics. The primary cause of carpal instability is laxity or rupture of specific ligaments. Although the intrinsic ligaments can tolerate greater relative stretch before rupture than can the extrinsic ligaments, they are more frequently injured.55 The clinical manifestation of carpal instability depends on the injured ligament (or ligaments) and the severity of the damage. Carpal instability may be static (demonstrated at rest) or dynamic (demonstrated only during free or resisted movement).
The following examples describe two of many forms of carpal instability. More detail on this subject is contained in other sources.18
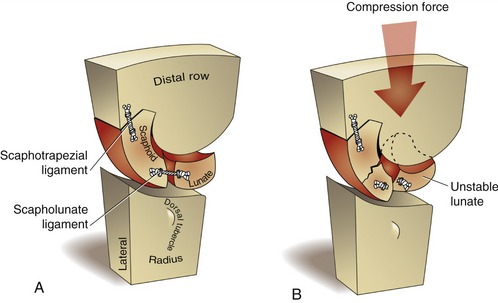
ROTATIONAL COLLAPSE OF THE WRIST
Mechanically, the wrist consists of a mobile proximal row of carpal bones intercalated or interposed between two rigid structures: the forearm and the distal row of carpal bones. Like cars of a freight train that are subject to derailment, the proximal row of carpal bones is susceptible to a rotational collapse in a “zigzag” fashion when compressed from both ends (Figure 7-18). The compression forces that cross the wrist arise from muscle activation and contact with the surrounding environment. In most healthy persons the wrist remains stable throughout life. Collapse and subsequent joint dislocation are prevented primarily by resistance from ligaments and from forces in tendons and the shapes of the adjoining carpal bones.
The lunate is the most frequently dislocated carpal bone.65 Normally its stability is provided by ligaments and articular contact with adjacent bones of the proximal row, most notably the scaphoid (Figure 7-19, A). By virtue of its two poles, the scaphoid forms an important mechanical link between the lunate and the more stable, distal row of carpal bones. The continuity of this link requires that the scaphoid and adjoining ligaments be intact.46,76,81 Consider, as an example, a fall over an outstretched hand with a resulting fracture in the waist region of the scaphoid, and tearing of the scapholunate ligament (see Figure 7-19, B). Disruption of the mechanical link between the two bones can result in scapholunate dissociation and subsequent malalignment of either or both bones.39 As shown in Figure 7-19, B, the more unstable lunate most often dislocates, or subluxes, so its distal articular surface faces dorsally. This condition is referred to clinically as dorsal intercalated segment instability (DISI) (Figure 7-20). Injury to other ligaments, such as the lunotriquetral ligament, may cause the lunate to dislocate such that its distal articular surface faces volarly (palmarly). This condition is referred to as volar (palmar) intercalated segment instability (VISI).75 Regardless of the type of rotational collapse, the consequences can be painful and disabling. Changes in the natural arthrokinematics may create regions of high stress, eventually leading to joint destruction, chronic inflammation, and changes in the shapes of the bones. A painful and unstable wrist may fail to provide a stable platform for the hand. A collapsed wrist may also alter the length-tension relationship and moment arms of the muscles that cross the region.81
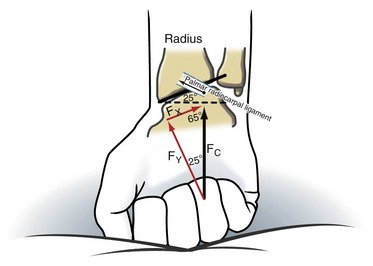
ULNAR TRANSLOCATION OF THE CARPUS
As pointed out earlier, the distal end of the radius is angled from side to side so that its articular surface is sloped ulnarly about 25 degrees (see Figure 7-4, A). This ulnar tilt of the radius creates a natural tendency for the carpus to slide (translate) in an ulnar direction.3 Figure 7-21 shows that a wrist with an ulnar tilt of 25 degrees has an ulnar translation force of 42% of the total compression force that crosses the wrist. This translational force is naturally resisted by passive tension from various extrinsic ligaments, such as palmar radiocarpal ligament. A disease such as rheumatoid arthritis may weaken the ligaments of the wrist. Over time, the carpus may migrate ulnarly. An excessive ulnar translocation can significantly alter the biomechanics of the entire wrist and hand.
MUSCLE AND JOINT INTERACTION
Innervation of the Wrist Muscles and Joints
INNERVATION OF MUSCLE
The radial nerve innervates all the muscles that cross the dorsal side of the wrist (see Figure 6-32, B). The primary wrist extensors are the extensor carpi radialis longus, extensor carpi radialis brevis, and extensor carpi ulnaris. The median and ulnar nerves innervate all muscles that cross the palmar side of the wrist, including the primary wrist flexors (see Figure 6-32, C and D). The flexor carpi radialis and palmaris longus are innervated by the median nerve; the flexor carpi ulnaris is innervated by the ulnar nerve. As a reference, the primary spinal nerve roots that supply the muscles of the upper extremity are listed in Appendix II, Part A. In addition, Appendix II, Parts B to D include additional reference items to help guide the clinical assessment of the functional status of the C5 to T1 spinal nerve roots and several major peripheral nerves of the upper limb.
SENSORY INNERVATION OF THE JOINTS
The radiocarpal and midcarpal joints receive sensory fibers from the C6 and C7 spinal nerve roots carried in the median and radial nerves.19,26,30 (This terminal sensory branch of the radial nerve often develops a painful neuroma within the wrists’ dorsal capsule.) The midcarpal joint is also innervated by sensory nerves traveling to the C8 spinal nerve root via the deep branch of the ulnar nerve.
Function of the Muscles at the Wrist
The wrist is controlled by a primary and a secondary set of muscles. The tendons of the muscles within the primary set attach distally within the carpus, or the adjacent proximal end of the metacarpals; these muscles act essentially on the wrist only. The tendons of the muscles within the secondary set cross the carpus as they continue distally to attach to the digits. The secondary muscles therefore act on the wrist and the hand. This chapter focuses more on the muscles of the primary set. The anatomy and kinesiology of the muscles of the secondary set—such as the extensor pollicis longus and the flexor digitorum superficialis—are considered in detail in Chapter 8. The proximal and distal attachments and nerve supply of the muscles of the wrist are listed in Appendix II, Part E.
As depicted in Figure 7-13, the medial-lateral and anterior-posterior axes of rotation of the wrist intersect within the head of the capitate bone. With the possible exception of the palmaris longus, no muscle has a line of force that passes precisely through either axis of rotation. At least from the anatomic position, essentially all wrist muscles therefore are equipped with moment arms to produce torques in both sagittal and frontal planes. The extensor carpi radialis longus, for example, passes dorsally to the medial-lateral axis of rotation and laterally to the anterior-posterior axis of rotation. Contraction of only this muscle would produce a combination of wrist extension and radial deviation. Using the extensor carpi radialis longus to produce a pure radial deviation motion, for example, would necessitate the activation of other muscles to neutralize the undesired wrist extension potential of the aforementioned muscle. Muscles of the wrist and hand rarely act in isolation when producing a meaningful movement. This theme of intermuscular cooperation will be further developed in this chapter and Chapter 8.
FUNCTION OF THE WRIST EXTENSORS
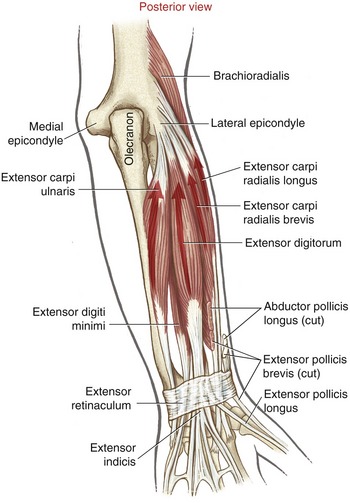
Muscular Anatomy: The primary wrist extensors are the extensor carpi radialis longus, the extensor carpi radialis brevis, and the extensor carpi ulnaris (Figure 7-22). The extensor digitorum is also capable of generating significant wrist extension torque but is mainly involved with extension of the fingers. Other secondary wrist extensors are the extensor indicis, extensor digiti minimi, and extensor pollicis longus.
The proximal attachments of the primary wrist extensors are located on and near the lateral (“extensor-supinator”) epicondyle of the humerus and dorsal border of the ulna (see Figures 6-2 and 6-6). Distally, the extensor carpi radialis longus and brevis attach side by side to the dorsal bases of the second and third metacarpals, respectively; the extensor carpi ulnaris attaches to the dorsal base of the fifth metacarpal.
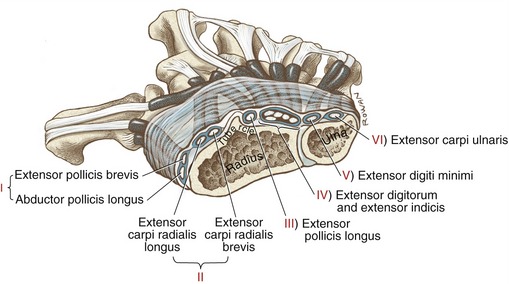
The tendons of the muscles that cross the dorsal and dorsal-radial side of the wrist are secured in place by the extensor retinaculum (Figure 7-23). Ulnarly, the extensor retinaculum wraps around the styloid process of the ulna to attach palmarly to the tendon of the flexor carpi ulnaris, pisiform bone, and pisometacarpal ligament. Radially, the retinaculum attaches to the styloid process of the radius and the radial collateral ligament. The extensor retinaculum prevents the underlying tendons from “bowstringing” up and away from the radiocarpal joint during active movements of the wrist.
Between the extensor retinaculum and the underlying bones are six fibro-osseus compartments that house the tendons along with their synovial sheaths.32 Clinicians frequently refer to these compartments by Roman numerals I to VI (see Figure 7-23). Each compartment houses a specific set of tendons. Tenosynovitis frequently occurs within one or more of these compartments, often from repetitive or forceful activities that increase tension on the associated tendons. The tendons and surrounding synovial membranes within compartment I are particularly susceptible to inflammation, a condition called de Quervain’s tenosynovitis. Activities that frequently cause this painful condition include repetitively pressing the trigger switch on a power tool, gripping tools while simultaneously supinating and pronating the forearm, or wringing out clothes. De Quervain’s tenosynovitis is typically treated conservatively by phonophoresis or iontophoresis, cortisone injections, ice, wearing a hand-wrist–based thumb splint, and modifying the activity that caused the inflammation. If conservative therapy fails to reduce the inflammation, surgical release of the first compartment may be indicated.
Biomechanical Assessment of Wrist Muscles’ Action and Torque Potential: Data are available on the relative position, cross-sectional area, and length of the internal moment arms of most muscles that cross the wrist.40,83 By knowing the approximate location of the axes of rotation of the wrist, these data provide a useful method for estimating the action and relative torque potential of the wrist muscles (Figure 7-24). Consider, for instance, the extensor carpi ulnaris and the flexor carpi ulnaris. By noting the location of each tendon from the axis of rotation, it is evident that the extensor carpi ulnaris is an extensor and ulnar deviator and the flexor carpi ulnaris is a flexor and ulnar deviator. Because both muscles have similar cross-sectional areas, they likely produce comparable levels of maximal force. In order to estimate the relative torque production of the two muscles, however, each muscle’s cross-sectional area must be multiplied by each muscle’s specific moment arm length. The extensor carpi ulnaris therefore is considered a more potent ulnar deviator than an extensor; the flexor carpi ulnaris is considered both a potent flexor and a potent ulnar deviator.
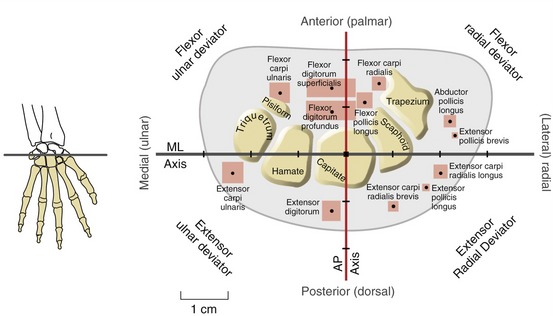
FIGURE 7-24. A cross-sectional view looking distally through the right carpal tunnel, similar to the perspective shown in Figure 7-5. The plot depicts the cross-sectional area, position, and length of the internal moment arms for most muscles that cross the wrist at the level of the head of the capitate. The area within the red boxes on the grid is proportional to the cross-sectional area of the muscle’s belly and therefore indicative of the maximal force production. The small black dot within each red box indicates the position of the muscle’s tendon. The wrist’s medial-lateral (ML) axis of rotation (dark gray) and anterior-posterior (AP) axis of rotation (red) intersect within the head of the capitate bone. Each muscle’s moment arm for a particular action is equal to the perpendicular distance between either axis and the position of the muscle’s tendon. The length of each moment arm (expressed in centimeters) is indicated by the major tick marks. Assume that the wrist is held in a neutral position.
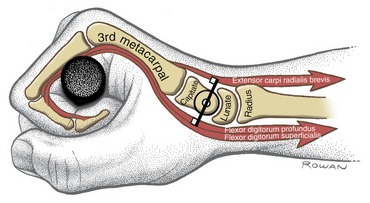
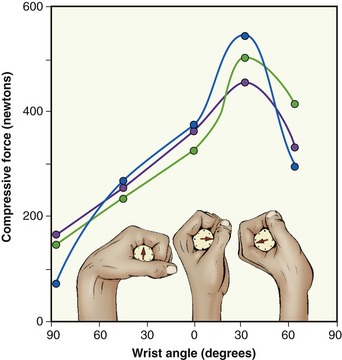
Wrist Extensor Activity while Making a Fist: The main function of the wrist extensors is to position and stabilize the wrist during activities involving active flexion of the fingers. Of particular importance is the role of the wrist extensor muscles in making a fist or producing a strong grip. To demonstrate this, rapidly tighten and release the fist and note the strong synchronous activity from the wrist extensors. The extrinsic finger flexor muscles, namely the flexor digitorum profundus and flexor digitorum superficialis, possess a significant internal moment arm as wrist flexors. The leverage of these muscles for wrist flexion is evident in Figure 7-24. The wrist extensor muscles must counterbalance the significant wrist flexion torque produced by the finger flexor muscles (Figure 7-25). As a strong grip is applied to an object, the wrist extensors typically hold the wrist in about 30 to 35 degrees of extension and about 5 degrees of ulnar deviation.56 This position optimizes the length-tension relationship of the extrinsic finger flexors, thereby facilitating maximal grip strength (Figure 7-26).
As evident in Figure 7-26, grip strength is significantly reduced when the wrist is fully flexed. The decreased grip strength is caused by a combination of two factors. First, and likely foremost, the finger flexors cannot generate adequate force because they are functioning at an extremely shortened length respective to their length-tension curve. Second, the overstretched finger extensors, particularly the extensor digitorum, create a passive extensor torque at the fingers, which further reduces effective grip force. This combination of physiologic and biomechanic events explains why a person with paralyzed wrist extensor muscles has difficulty producing an effective grip, even though the finger flexor muscles remain fully innervated. Trying to produce a maximal-effort grip when the wrist extensors are paralyzed results in an abnormal posture of finger flexion and wrist flexion (Figure 7-27, A). Stabilizing the wrist in greater extension enables the finger flexor muscles to nearly triple their grip force (see Figure 7-27, B). Manually or orthotically preventing the wrist from flexing maintains the extrinsic finger flexors at an elongated length more conducive to a higher force production.
Ordinarily the person depicted in Figure 7-27 wears a splint that holds the wrist in 10 to 20 degrees of extension. If the radial nerve fails to reinnervate the wrist extensor muscles, a tendon from another muscle is often surgically transferred to provide wrist extension torque. For example, the pronator teres muscle, innervated by the median nerve, is connected to the tendon of the extensor carpi radialis brevis. Of the three primary wrist extensors, the extensor carpi radialis brevis is located most centrally at the wrist and has the greatest moment arm for wrist extension (see Figure 7-24).
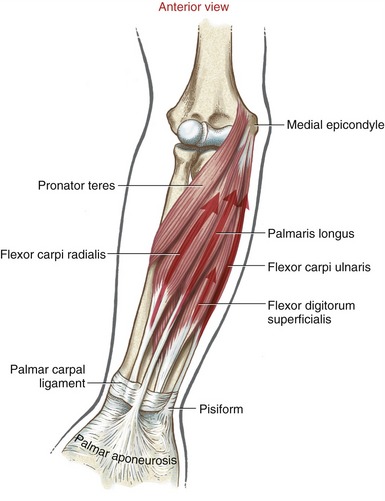
FUNCTION OF THE WRIST FLEXORS
Muscular Anatomy: The three primary wrist flexors are the flexor carpi radialis, the flexor carpi ulnaris, and the palmaris longus (Figure 7-28). The palmaris longus is absent in about 10% to 15% of people.82 Even when present, the muscle often exhibits variation in shape and number of tendons. The tendon of this muscle is often used as a donor in tendon grafting surgery.
Other secondary muscles capable of flexing the wrist are the extrinsic flexors of the digits: the flexor digitorum profundus, flexor digitorum superficialis, and flexor pollicis longus. (The classification of these muscles as “secondary” wrist flexors should not imply they have a limited potential to perform this task. Actually, based on the muscles’ cross-sectional areas and wrist flexor moment arms [see Figure 7-24], the wrist flexion torque potential of extrinsic flexors of the digits may exceed that of the primary wrist flexors.) With the wrist in a neutral position, the abductor pollicis longus and extensor pollicis brevis have a small moment arm for wrist flexion (see Figure 7-24).
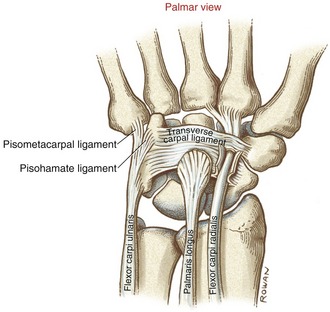
The proximal attachments of the primary wrist flexors are located on and near the medial (“flexor-pronator”) epicondyle of the humerus and dorsal border of the ulna (see Figures 6-2 and 6-6). Technically, the tendon of the flexor carpi radialis does not cross the wrist through the carpal tunnel; rather, the tendon passes in a separate tunnel formed by a groove in the trapezium and fascia from the adjacent transverse carpal ligament (Figure 7-29). The tendon of the flexor carpi radialis attaches distally to the palmar base of the second and sometimes the third metacarpal. The palmaris longus has a distal attachment primarily to the thick aponeurosis of the palm. The tendon of the flexor carpi ulnaris courses distally to attach to the pisiform bone and, in a plane superficial to the transverse carpal ligament, into the pisohamate and pisometacarpal ligaments and the base of the fifth metacarpal bone.
Functional Considerations: Based on moment arm and cross-sectional area (see Figure 7-24), the flexor carpi ulnaris produces the greatest wrist flexion torque potential of the three primary wrist flexor muscles. During active wrist flexion, the flexor carpi radialis and flexor carpi ulnaris act together as synergists while simultaneously opposing each other’s radial and ulnar deviation ability.
As indicated in Table 7-1, data indicate that the wrist flexor muscles produce about 70% greater isometric torque than the wrist extensor muscles—12.2 Nm versus 7.1 Nm, respectively.17 The greater total cross-sectional area of the wrist flexor muscles as a group can account for much of this disparity.29 It is noteworthy that the extrinsic finger flexors (flexors digitorum superficialis and profundus) account for about two thirds of the total cross-sectional area of the wrist flexors.40 Activities such as lifting or pulling heavy objects normally demand strength in both the wrist flexor and finger flexor musculature. Strong coactivation of the wrist extensor muscles is required during these activities to prevent a relatively ineffective position of combined wrist and finger flexion.
TABLE 7-1.
Magnitude and Wrist Joint Position of Peak Isometric Torque Produced by Healthy Males
| Wrist Muscle Group | Mean Peak Torque (Nm) | Joint Angle of Peak Torque |
| Flexors | 12.2 (3.7) | 40 degrees of flexion |
| Extensors | 7.1 (2.1) | From 30 degrees of flexion to 70 degrees of extension |
| Radial deviators | 11.0 (2.0) | 0 degrees (neutral) |
| Ulnar deviators | 9.5 (2.2) | 0 degrees (neutral) |
Standard deviations in parentheses.
Data from Delp SL, Grierson AE, Buchanan TS: Maximum isometric moments generated by the wrist muscles in flexion-extension and radial-ulnar deviation, J Biomech 29:1371, 1996.
FUNCTION OF THE RADIAL AND ULNAR DEVIATORS
Muscles capable of producing radial deviation of the wrist are the extensor carpi radialis brevis and longus, extensor pollicis longus and brevis, flexor carpi radialis, abductor pollicis longus, and flexor pollicis longus (review Figure 7-24). In the neutral wrist position, the extensor carpi radialis longus and abductor pollicis longus possess the largest product of cross-sectional area and moment arm for radial deviation torque. The extensor pollicis brevis has the greatest moment arm of all radial deviators; however, because of a relatively small cross-sectional area, this muscle’s torque production is relatively small. The abductor pollicis longus and extensor pollicis brevis provide important stability to the radial side of the wrist, augmenting that produced passively by the radial collateral ligament. As shown in Table 7-1, the radial deviator muscles generate about 15% greater isometric torque than the ulnar deviator muscles—11.0 Nm versus 9.5 Nm, respectively.17
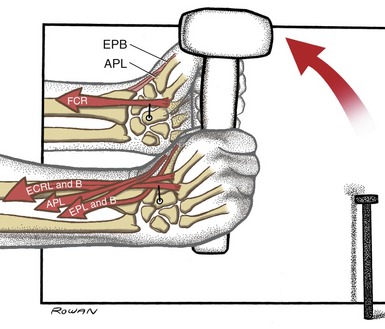
Figure 7-30 shows the radial deviator muscles contracting during use of a hammer. All these muscles pass laterally to the wrist’s anterior-posterior axis of rotation. The action of the extensor carpi radialis longus and the flexor carpi radialis, shown with moment arms, illustrates a fine example of two muscles cooperating as synergists for one motion but as antagonists for another. The net effect of this muscular cooperation produces a radially deviated wrist, well stabilized in slight extension for optimal grasp of the hammer.
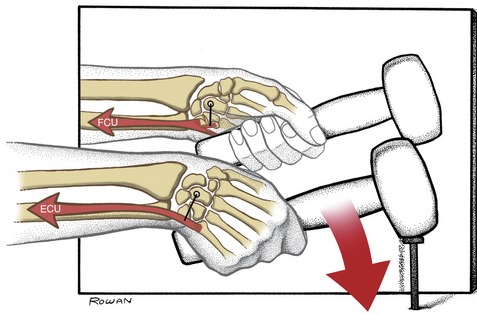
Muscles capable of ulnar deviation of the wrist are the extensor carpi ulnaris, flexor carpi ulnaris, flexor digitorum profundus and superficalis, and extensor digitorum (see Figure 7-24). Because of moment arm length, however, the muscles most capable of this action, by far, are the extensor carpi ulnaris and flexor carpi radialis. Figure 7-31 shows this strong pair of ulnar deviator muscles contracting as a nail is struck with a hammer. Both the flexor and extensor carpi ulnaris contract synergistically to perform the ulnar deviation but also stabilize the wrist in a slightly extended position. Because of the strong functional association between the flexor and extensor carpi ulnaris muscles, injury to either muscle can incapacitate the overall kinetics of ulnar deviation. For example, rheumatoid arthritis often causes inflammation and pain in the extensor carpi ulnaris tendon near its distal attachment. Attempts at active ulnar deviation with minimal to no activation in the painful extensor carpi ulnaris cause the action of the flexor carpi ulnaris to go unopposed. The resulting flexed posture of the wrist is thereby not suitable for an effective grasp.
REFERENCES
1. Alfredson, H, Ljung, BO, Thorsen, K, Lorentzon, R. In vivo investigation of ECRB tendons with microdialysis technique—no signs of inflammation but high amounts of glutamate in tennis elbow. Acta Orthop Scand. 2000;71:475–479.
2. Allan, CH, Joshi, A, Lichtman, DM. Kienböck’s disease: diagnosis and treatment. J Am Acad Orthop Surg. 2001;9:128–136.
3. Arimitsu, S, Murase, T, Hashimoto, J, et al. A three-dimensional quantitative analysis of carpal deformity in rheumatoid wrists. J Bone Joint Surg [Br]. 2007;89:490–494.
4. Ashe, MC, McCauley, T, Khan, KM. Tendinopathies in the upper extremity: A paradigm shift. J Hand Ther. 2004;17:329–334.
5. Bathala, EA, Murray, PM. Long-term follow-up of an undiagnosed trans-scaphoid perilunate dislocation demonstrating articular remodeling and functional adaptation. J Hand Surg [Am]. 2007;32:1020–1023.
6. Berger, RA. The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop Relat Res. 2001;383:32–40.
7. Berger, RA. The anatomy of the scaphoid. Hand Clin. 2001;17:525–532.
8. Blackwell, JR, Cole, KJ. Wrist kinematics differ in expert and novice tennis players performing the backhand stroke: Implications for tennis elbow. J Biomech. 1994;27:509–516.
9. Blankenhorn, BD, Pfaeffle, HJ, Tang, P, et al. Carpal kinematics after proximal row carpectomy. J Hand Surg [Am]. 2007;32:37–46.
10. Bunata, RE, Brown, DS, Capelo, R. Anatomic factors related to the cause of tennis elbow. J Hand Surg [Am]. 2007;89:1955–1963.
11. Carter, PB, Stuart, PR. The Sauve-Kapandji procedure for post-traumatic disorders of the distal radio-ulnar joint. J Bone Joint Surg [Br]. 2000;82:1013–1018.
12. Cavaliere, CM, Chung, KC. A systematic review of total wrist arthroplasty compared with total wrist arthrodesis for rheumatoid arthritis. Plast Reconstr Surg. 2008;122:813–825.
13. Chidgey, LK, Dell, PC, Bittar, ES, Spanier, SS. Histologic anatomy of the triangular fibrocartilage. J Hand Surg [Am]. 1991;16:1084–1100.
14. Dacho, AK, Baumeister, S, Germann, G, Sauerbier, M. Comparison of proximal row carpectomy and midcarpal arthrodesis for the treatment of scaphoid nonunion advanced collapse (SNAC-wrist) and scapholunate advanced collapse (SLAC-wrist) in stage II. J Plast Reconstr Aesthet Surg. 2008;61:1210–1218.
15. de Lange, A, Kauer, JM, Huiskes, R. Kinematic behavior of the human wrist joint: A roentgen-stereophotogrammetric analysis. J Orthop Res. 1985;3:56–64.
16. DeFrate, LE, Li, G, Zayontz, SJ, Herndon, JH. A minimally invasive method for the determination of force in the interosseous ligament. Clin Biomech (Bristol, Avon). 2001;16:895–900.
17. Delp, SL, Grierson, AE, Buchanan, TS. Maximum isometric moments generated by the wrist muscles in flexion-extension and radial-ulnar deviation. J Biomech. 1996;29:1371–1375.
18. Dobyns, JH, Cooney, WP. Classification of carpal instability. In: Cooney WP, Linscheid R, Dobyns JH, eds. The Wrist. St Louis: Mosby, 1998.
19. Ferreres, A, Suso, S, Ordi, J, et al. Wrist denervation. Anatomical considerations. J Hand Surg [Br]. 1995;20:761–768.
20. Friedman, SL, Palmer, AK, Short, WH, et al. The change in ulnar variance with grip. J Hand Surg [Am]. 1993;18:713–716.
21. Frykman, GK, Kroop, WE. Fractures and traumatic conditions of the wrist. In Hunter JM, Mackin EJ, Callahan AD, eds.: Rehabilitation of the hand: surgery and therapy, ed 4, St Louis: Mosby, 1995.
22. Garcia-Elias, M. Soft-tissue anatomy and relationships about the distal ulna. Hand Clin. 1998;14:165–176.
23. Gardner, MJ, Crisco, JJ, Wolfe, SW. Carpal kinematics. Hand Clin. 2006;22:413–420.
24. Gelberman, RH, Gross, MS. The vascularity of the wrist. Identification of arterial patterns at risk. Clin Orthop Relat Res. 1986;202:40–49.
25. Gofton, WT, Gordon, KD, Dunning, CE, et al. Soft-tissue stabilizers of the distal radioulnar joint: an in vitro kinematic study. J Hand Surg [Am]. 2004;29:423–431.
26. Gray, DJ, Gardner, E. The innervation of the joints of the wrist and hand. Anat Rec. 1965;151:261–266.
27. Gupta, A, Moosawi, NA. How much can carpus rotate axially? An in vivo study. Clin Biomech (Bristol, Avon). 2005;20:172–176.
28. Hagert, E, Ljung, BO, Forsgren, S. General innervation pattern and sensory corpuscles in the scapholunate interosseous ligament. Cells Tissues Organs. 2004;177:47–54.
29. Holzbaur, KR, Delp, SL, Gold, GE, Murray, WM. Moment-generating capacity of upper limb muscles in healthy adults. J Biomech. 2007;40:2442–2449.
30. Inman, VT, Saunders, JB. Referred pain from skeletal structures. J Nerv Ment Dis. 1944;99:660–667.
31. Ishii, S, Palmer, AK, Werner, FW, et al. An anatomic study of the ligamentous structure of the triangular fibrocartilage complex. J Hand Surg [Am]. 1998;23:977–985.
32. Iwamoto, A, Morris, RP, Andersen, C, et al. An anatomic and biomechanic study of the wrist extensor retinaculum septa and tendon compartments. J Hand Surg [Am]. 2006;31:896–903.
33. Jung, JM, Baek, GH, Kim, JH, et al. Changes in ulnar variance in relation to forearm rotation and grip. J Bone Joint Surg Br. 2001;83:1029–1033.
34. Kauer, JM. The mechanism of the carpal joint. Clin Orthop Relat Res. 1986;202:16–26.
35. Kaufmann, R, Pfaeffle, J, Blankenhorn, B, et al. Kinematics of the midcarpal and radiocarpal joints in radioulnar deviation: an in vitro study. J Hand Surg [Am]. 2005;30:937–942.
36. Kihara, H, Palmer, AK, Werner, FW, et al. The effect of dorsally angulated distal radius fractures on distal radioulnar joint congruency and forearm rotation. J Hand Surg [Am]. 1996;21:40–47.
37. Kobayashi, M, Berger, RA, Nagy, L, et al. Normal kinematics of carpal bones: A three-dimensional analysis of carpal bone motion relative to the radius. J Biomech. 1997;30:787–793.
38. Kraushaar, BS, Nirschl, RP. Tendinosis of the elbow (tennis elbow). Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg [Am]. 1999;81:259–278.
39. Kuo, CE, Wolfe, SW. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg [Am]. 2008;33:998–1013.
40. Lehmkuhl, LD, Smith, LK. Brunnstrom’s clinical kinesiology, ed 4. Philadelphia: FA Davis; 1983.
41. Li, ZM, Kuxhaus, L, Fisk, JA, Christophel, TH. Coupling between wrist flexion-extension and radial-ulnar deviation. Clin Biomech (Bristol, Avon). 2005;20:177–183.
42. Linscheid, RL. Kinematic considerations of the wrist. Clin Orthop Relat Res. 1986;202:27–39.
43. MacConaill, MA, Basmajian, JV. Muscles and movements: a basis for human kinesiology. New York: Robert E. Krieger; 1977.
44. Majima, M, Horii, E, Matsuki, H, et al. Load transmission through the wrist in the extended position. J Hand Surg [Am]. 2008;33:182–188.
45. Minami, A, Kato, H, Iwasaki, N. Modification of the Sauve-Kapandji procedure with extensor carpi ulnaris tenodesis. J Hand Surg [Am]. 2000;25:1080–1084.
46. Mitsuyasu, H, Patterson, RM, Shah, MA, et al. The role of the dorsal intercarpal ligament in dynamic and static scapholunate instability. J Hand Surg [Am]. 2004;29:279–288.
47. Moojen, TM, Snel, JG, Ritt, MJ, et al. In vivo analysis of carpal kinematics and comparative review of the literature. J Hand Surg [Am]. 2003;28:81–87.
48. Moojen, TM, Snel, JG, Ritt, MJ, et al. Three-dimensional carpal kinematics in vivo. Clin Biomech (Bristol, Avon). 2002;17:506–514.
49. Moore, DC, Crisco, JJ, Trafton, TG, Leventhal, EL. A digital database of wrist bone anatomy and carpal kinematics. J Biomech. 2007;40:2537–2542.
50. Moritomo, H, Apergis, EP, Herzberg, G, et al. IFSSH committee report of wrist biomechanics committee: biomechanics of the so-called dart-throwing motion of the wrist. J Hand Surg [Am]. 2007;32:1447–1453.
51. Moritomo, H, Murase, T, Goto, A, et al. Capitate-based kinematics of the midcarpal joint during wrist radioulnar deviation: an in vivo three-dimensional motion analysis. J Hand Surg [Am]. 2004;29:668–675.
52. Neumann DA: Observations from cineradiography analysis, 2000, unpublished work.
53. Nirschl, RP, Pettrone, FA. Tennis elbow. The surgical treatment of lateral epicondylitis. J Bone Joint Surg [Am]. 1979;61:832–839.
54. Nishiwaki, M, Nakamura, T, Nagura, T, et al. Ulnar-shortening effect on distal radioulnar joint pressure: A biomechanical study. J Hand Surg [Am]. 2008;33:198–205.
55. Nowalk, MD, Logan, SE. Distinguishing biomechanical properties of intrinsic and extrinsic human wrist ligaments. J Biomech Eng. 1991;113:85–93.
56. O’Driscoll, SW, Horii, E, Ness, R, et al. The relationship between wrist position, grasp size, and grip strength. J Hand Surg [Am]. 1992;17:169–177.
57. Palmer, AK, Glisson, RR, Werner, FW. Ulnar variance determination. J Hand Surg [Am]. 1982;7:376–379.
58. Palmer, AK, Werner, FW. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984;187:26–35.
59. Park, MJ, Cooney, WP, 3rd., Hahn, ME, et al. The effects of dorsally angulated distal radius fractures on carpal kinematics. J Hand Surg [Am]. 2002;27:223–232.
60. Patterson, RM, Nicodemus, CL, Viegas, SF, et al. High-speed, three-dimensional kinematic analysis of the normal wrist. J Hand Surg [Am]. 1998;23:446–453.
61. Peltier, LF. The classic. Concerning traumatic malacia of the lunate and its consequences: degeneration and compression fractures. Translation of 1910 article. Privatdozent Dr. Robert Kienbock. Clin Orthop Relat Res. 1980;150:4–8.
62. Potter, HG, Hannafin, JA, Morwessel, RM, et al. Lateral epicondylitis: Correlation of MR imaging, surgical, and histopathologic findings. Radiology. 1995;196:43–46.
63. Radonjic, D, Long, C. Kinesiology of the wrist. Am J Phys Med. 1971;50:57–71.
64. Ritt, MJ, Stuart, PR, Berglund, LJ, et al. Rotational stability of the carpus relative to the forearm. J Hand Surg [Am]. 1995;20:305–311.
65. Ruby, LK, Fractures and dislocations of the carpus, ed 2. Browner, BD, Jupiter, JB, Levine, AM, eds., Skeletal trauma: fractures, dislocations, ligamentous injuries, vol 2. Philadelphia: Saunders, 1998.
66. Ruby, LK, Cooney, WP, 3rd., An, KN, et al. Relative motion of selected carpal bones: a kinematic analysis of the normal wrist. J Hand Surg [Am]. 1988;13:1–10.
67. Ryu, JY, Cooney, WP, 3rd., Askew, LJ, et al. Functional ranges of motion of the wrist joint. J Hand Surg [Am]. 1991;16:409–419.
68. Safaee-Rad, R, Shwedyk, E, Quanbury, AO, Cooper, JE. Normal functional range of motion of upper limb joints during performance of three feeding activities. Arch Phys Med Rehabil. 1990;71:505–509.
69. Sarrafian, SK, Melamed, JL, Goshgarian, GM. Study of wrist motion in flexion and extension. Clin Orthop Relat Res. 1977;Jul-126:153–159.
70. Savelberg, HH, Kooloos, JG, de Lange, A, et al. Human carpal ligament recruitment and three-dimensional carpal motion. J Orthop Res. 1991;9:693–704.
71. Schuind, F, Eslami, S, Ledoux, P. Kienböck’s disease. J Bone Joint Surg Br. 2008;90:133–139.
72. Schuind, FA, Linscheid, RL, An, KN, Chao, EY. A normal data base of posteroanterior roentgenographic measurements of the wrist. J Bone Joint Surg Am. 1992;74:1418–1429.
73. Shaaban, H, Giakas, G, Bolton, M, et al. Contact area inside the distal radioulnar joint: effect of axial loading and position of the forearm. Clin Biomech (Bristol, Avon). 2007;22:313–318.
74. Shepherd, DE, Johnstone, A. A new design concept for wrist arthroplasty. Proceedings of the Institution of Mechanical Engineers. 2005; Part H. J Eng Med. 2005;219:43–52.
75. Shin, AY, Battaglia, MJ, Bishop, AT. Lunotriquetral instability: diagnosis and treatment. J Am Acad Orthop Surg. 2000;8:170–179.
76. Short, WH, Werner, FW, Green, JK, Masaoka, S. Biomechanical evaluation of ligamentous stabilizers of the scaphoid and lunate. J Hand Surg [Am]. 2002;27:991–1002.
77. Short, WH, Werner, FW, Green, JK, et al. The effect of sectioning the dorsal radiocarpal ligament and insertion of a pressure sensor into the radiocarpal joint on scaphoid and lunate kinematics. J Hand Surg [Am]. 2002;27:68–76.
78. Standring, S. Gray’s anatomy: The anatomical basis of clinical practice, ed 40. St Louis: Elsevier; 2009.
79. Sun, JS, Shih, TT, Ko, CM, et al. In vivo kinematic study of normal wrist motion: an ultrafast computed tomographic study. Clin Biomech (Bristol, Avon). 2000;15:212–216.
80. Taleisnik, J. The ligaments of the wrist. In: Taleisnik J, ed. The wrist. New York: Churchill Livingstone, 1985.
81. Tang, JB, Ryu, J, Omokawa, S, Wearden, S. Wrist kinetics after scapholunate dissociation: the effect of scapholunate interosseous ligament injury and persistent scapholunate gaps. J Orthop Res. 2002;20:215–221.
82. Thompson, NW, Mockford, BJ, Rasheed, T, Herbert, KJ. Functional absence of flexor digitorum superficialis to the little finger and absence of palmaris longus—is there a link? J Hand Surg [Br]. 2002;27:433–434.
83. Tolbert, JR, Blair, WF, Andrews, JG, Crowninshield, RD. The kinetics of normal and prosthetic wrists. J Biomech. 1985;18:887–897.
84. Trudel, D, Duley, J, Zastrow, I, et al. Rehabilitation for patients with lateral epicondylitis: A systematic review. J Hand Ther. 2004;17:243–266.
85. Viegas, SF. The dorsal ligaments of the wrist. Hand Clin. 2001;17:65–75.
86. Viegas, SF, Yamaguchi, S, Boyd, NL, Patterson, RM. The dorsal ligaments of the wrist: anatomy, mechanical properties, and function. J Hand Surg [Am]. 1999;24:456–468.
87. Waugh, EJ. Lateral epicondylalgia or epicondylitis: What’s in a name? J Orthop Sports Phys Ther. 2005;35:200–202.
88. Weaver, L, Tencer, AF, Trumble, TE. Tensions in the palmar ligaments of the wrist. I. The normal wrist. J Hand Surg [Am]. 1994;19:464–474.
89. Werner, FW, Palmer, AK, Fortino, MD, Short, WH. Force transmission through the distal ulna: effect of ulnar variance, lunate fossa angulation, and radial and palmar tilt of the distal radius. J Hand Surg [Am]. 1992;17:423–428.
90. Werner, FW, Short, WH, Fortino, MD, Palmer, AK. The relative contribution of selected carpal bones to global wrist motion during simulated planar and out-of-plane wrist motion. J Hand Surg [Am]. 1997;22:708–713.
91. Werner, FW, Short, WH, Green, JK, et al. Severity of scapholunate instability is related to joint anatomy and congruency. J Hand Surg [Am]. 2007;32:55–60.
92. Wolfe, SW, Crisco, JJ, Katz, LD. A non-invasive method for studying in vivo carpal kinematics. J Hand Surg [Br]. 1997;22:147–152.
93. Yoshioka, H, Tanaka, T, Ueno, T, et al. Study of ulnar variance with high-resolution MRI: correlation with triangular fibrocartilage complex and cartilage of ulnar side of wrist. J Magn Reson Imaging. 2007;26:714–719.
94. Youm, Y, McMurthy, RY, Flatt, AE, Gillespie, TE. Kinematics of the wrist. I. An experimental study of radial-ulnar deviation and flexion-extension. J Bone Joint Surg Am. 1978;60:423–431.
STUDY QUESTIONS
1. How does the tendon of the flexor carpi radialis reach the base of the metacarpal bones without actually entering the carpal tunnel?
2. Cite factors that justify the greater range of ulnar deviation as compared with radial deviation of the wrist.
3. Assume that trauma associated with a fractured distal radius created a permanent 25 degree dorsal tilt of the distal radius (review Figure 7-4, B). What are some probable functional impairments that may result from this malalignment?
4. Describe the arthrokinematic pattern for flexion and extension at the radiocarpal joint.
5. Justify the importance of the capitate bone with regard to the osteokinematics of the entire wrist and hand.
6. The following questions are based on the data presented in Figure 7-24.
a. Which muscle would produce the greatest flexion torque at the wrist, the flexor carpi radialis, or the flexor digitorum superficialis?
b. Which muscle has the longest moment arm for ulnar deviation torque?
c. Which muscle is the most direct antagonist to the flexor carpi ulnaris?
7. Which two tendons of the thumb share the same fibrous tunnel within the extensor reticulum of the wrist?
8. What is the role of the scaphoid in providing mechanical stability to the lunate?
9. How would you maximally stretch the extensor carpi radialis longus muscle?
10. Which extrinsic ligaments naturally resist an ulnar translocation of the carpus?
11. A patient had severe trauma to the proximal radius and adjacent interosseous membrane that necessitated a partial resection of the radial head. Describe possible functional impairments or pathologies that might result from a subsequent 6- to 7-mm proximal migration of the radius.
12. Which carpal bones normally do not contact the capitate bone?
13. Compare the convex-concave joint relationships that exist within the medial and lateral compartments of the midcarpal joint of the wrist. Describe how these relationships affect the arthrokinematics of the joint during flexion and extension.
14. List all muscles that have a full or partial proximal attachment to the lateral epicondyle of the humerus. Which nerve innervates all these muscles?
15. Describe the muscular interaction between the flexor carpi ulnaris and flexor carpi radialis during active flexion of the wrist?
 Answers to the study questions can be found on the Evolve website.
Answers to the study questions can be found on the Evolve website.