CHAPTER 6 With What Other Disciplines Should We Work?
Cooperation among specialties, especially between anesthesiology and surgery, is the stuff of legend. Of note, a legend is defined as “a story coming down from the past; one popularly regarded as historical although not verifiable.”
And, of course, he could hear them too.
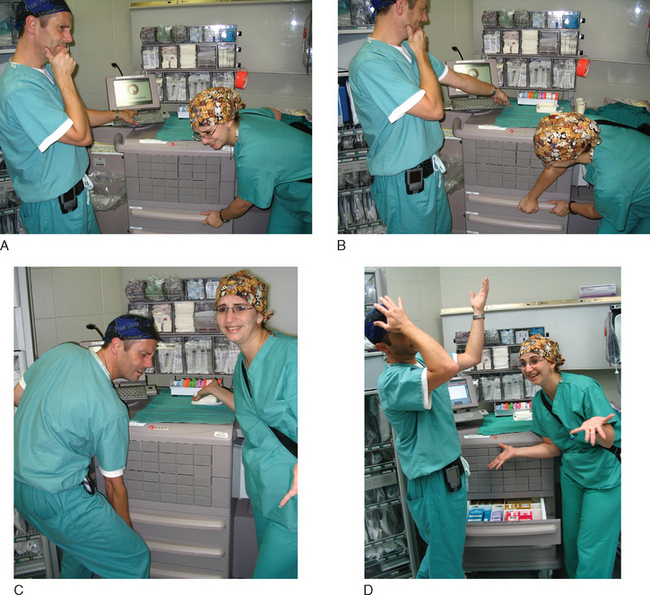
Good things happen when you throw people together.
Scheduling hassles with this multidisciplinary love-fest? Yes.
As detailed in the previous chapter, moving the meat around is the biggest headache of “Simulato-land.” So getting people there and, trickiest of all, getting different disciplines there at the same time is tough.
Oh, what about the money? Oh, that.
Friday is a slow day in the ORs, a good day for anesthesia.
But Friday is the clinic day for surgery, bad day for them. How about Thursday?
But on Tuesdays, the medical people have Grand Rounds and that’s their busiest day, so … Monday?
How about next week? Oh, that’s right, everyone’s out of town for the conference?
How about Wednesday, May 5, 2097 from 1 a.m. to 2 a.m., that’s the one time that everyone can. …
(Running a Simulator center, you have to be part pitchman.)
Same goes for running a multidisciplinary simulation center.
NEW DRUG-DISPENSING SYSTEM
Pharmacy and the information technology people have put together a new system for dispensing drugs. This system uses a log-in and fingerprint recognition system. The pharmacy and IT people gather round as a senior resident starts a simulated case. This resident uses the old system of getting drugs—a cart with all the drugs just sitting in drawers.
“Now he is for implantation of an AICD. He has external pads on and is ready for induction.”
“Shock! Defib!” the anesthesia resident shouts.
Shocking is the most crucial thing, but after three shocks it’s time to go to the next step. The anesthesia resident intubates, CPR starts (a medical student does chest compressions), and then it’s time to get the drugs.
So at the end of the simulation, everyone’s learned something.
And all these lessons at no risk to a patient.
At the end of this simulation, people have still learned good lessons.