Chapter 11 Why Synthetic Grafts Failed
History of Synthetic Grafts for Anterior Cruciate Ligament Reconstruction
Synthetic grafts for anterior cruciate ligament (ACL) reconstruction had a brief period of popularity in the mid-1980s. At this time the routine operation was an open patellar tendon graft with 6 weeks of postoperative immobilization. The concept of implanting a sterile, off-the-shelf synthetic ligament with no postoperative immobilization was very appealing. There was no harvest site morbidity, and the rehabilitation was very quick. In a very short period, it was recognized that there was a higher rate of failure compared with autogenous grafts, an increased rate of late infection, considerable bone tunnel enlargement, and significant sterile effusions; in addition, the grafts were expensive. In a 2005 article reviewing the choices of graft for ACL reconstruction, West and Harner1 stated that there is no indication for synthetic ligaments.
Causes of Failure of Synthetic Grafts
The most common cause of failure of synthetic grafts was the fiber abrasion due to bending forces over the edge of the bony tunnels (Fig. 11-1). In order to avoid this problem, the Gore-Tex graft was placed over the top of the femur. This nonanatomical position eventually led to graft failure. Carson et al2 have stated that approximately 50% of the failures of ACL reconstruction are due to technical error, and the anterior femoral tunnel placement is one of the most common errors. It is likely that many of the failures of synthetic grafts were due to the same causes. The literature has numerous articles reporting the unacceptable failure rate after synthetic ACL reconstruction. Kumar and Maffuli3 reported on the stress shielding caused by the use of the LAD. Riel4 reported numerous complications following the use of the LAD and concluded that there was no indication for its use. Muren et al5 published results that showed no advantage to augmenting the patellar tendon graft with the LAD device. Guidoin et al6 reviewed 69 failed synthetic fiber ligament grafts and found that they all failed by fiber abrasion of the textile fiber around the bony tunnel edge. Kock et al7 stated that the Trevira ligament failed due to fiber abrasion and the nonanatomical position of the graft. Wredmark and Engstrom8 reviewed the results of the Stryker Dacron graft and found an 80% failure rate. Engstrom et al9 also compared the Leeds-Keio with an autogenous patellar tendon graft and found the failure rate of the synthetic to be unacceptable. Andersen et al10 reported unsatisfactory results with the Dacron synthetic graft. Bowyer and Matthews11 reported an unacceptable failure rate with the Gore-Tex ligament graft. Indelicato et al12 reported on the sterile effusions that were foreign body reactions to the synthetic graft. Woods et al13 published the deteriorating results of the Gore-Tex graft with longer follow-up from 2 to 3 years. Barrett et al14 also reported on the high failure rate (47%) with the Dacron synthetic ligament. This ligament had been placed in a nonanatomical, over-the-top position. Paulos et al15 reported 13% fair and 42% poor results with the Gore-Tex graft. Looseness and failure of the graft occurred in 30% of the cases with this graft placed in the over-the-top position. The 2.7% infection rate was higher than that reported with autogenous grafts.
Other Problems with Synthetic Grafts
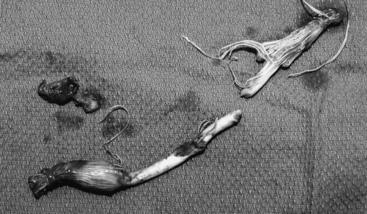
The problem of synthetic grafts is not only that they failed, but that there were other significant issues such as biocompatibility. The carbon fiber grafts produced a black synovitis in the joint. The regional lymph nodes also became enlarged with the carbon fiber debris. The Gore-Tex ligament often produced a very severe sterile synovitis that resembled a septic arthritis (Fig. 11-2). This prompted many patients to undergo a repeat arthroscopy to irrigate the joint. Biopsy of the synovium showed a foreign body reaction. The Gore-Tex ligament would occasionally produce a ganglion-type reaction at the tibial tunnel that required excision (Fig. 11-3). The bony tunnels would often become extremely large, requiring removal of the graft and bony grafting of the tunnels (Fig. 11-4). The revision ACL reconstruction would be staged some months later, when the bony tunnels had healed.
The Future
There is still considerable interest and investigation into some form of synthetic bioabsorbable scaffold to implant into the stump of the ACL after injury to the ligament.16 In fact, a type of scaffold that is augmented with growth factors holds the most promise for the future. This minimally invasive approach to ACL repair would be an improvement over the relatively barbaric procedure of harvesting of the hamstring tendons to reconstruct the ACL.
1 West RV, Harner CD. Graft selection in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2005;13:197-207.
2 Carson EW, Anisko EM, Restrepo C, et al. Revision anterior cruciate ligament reconstruction: etiology of failures and clinical results. J Knee Surg. 2004;17:127-132.
3 Kumar K, Maffullli N. The ligament augmentation device: an historical perspective. Arthroscopy. 1999;15:422-432.
4 Riel KA. [Augmented anterior cruciate ligament replacement with the Kennedy-LAD (ligament augmentation device)—long term outcome]. Zentralbl Chir. 1998;123:1014-1018.
5 Muren O, Dahlstedt L, Dalen N. Reconstruction of acute anterior cruciate ligament injuries: a prospective, randomised study of 40 patients with 7-year follow-up. No advantage of synthetic augmentation compared to a traditional patellar tendon graft. Arch Orthop Trauma Surg. 2003;123:144-147.
6 Guidoin MF, Marois Y, Bejui J, et al. Analysis of retrieved polymer fiber based replacements for the ACL. Biomaterials. 2000;21:2461-2474.
7 Kock HJ, Sturmer KM, Letsch R, et al. Interface and biocompatibility of polyethylene terephthalate knee ligament prostheses. A histological and ultrastructural device retrieval analysis in failed synthetic implants used for surgical repair of anterior cruciate ligaments. Arch Orthop Trauma Surg. 1994;114:1-7.
8 Wredmark T, Engstrom B. Five-year results of anterior cruciate ligament reconstruction with the Stryker Dacron high-strength ligament. Knee Surg Sports Traumatol Arthrosc. 1993;1:71-75.
9 Engstrom B, Wredmark T, Westblad P. Patellar tendon or Leeds-Keio graft in the surgical treatment of anterior cruciate ligament ruptures. Intermediate results. Clin Orthop Relat Res. 1993;6:190-197.
10 Andersen HN, Bruun C, Sondergard-Petersen PE. Reconstruction of chronic insufficient anterior cruciate ligament in the knee using a synthetic Dacron prosthesis. A prospective study of 57 cases. Am J Sports Med. 1992;20:20-23.
11 Bowyer GW, Matthews SJ. Anterior cruciate ligament reconstruction using the Gore-Tex ligament. J R Army Med Corps. 1991;137:69-75.
12 Indelicato PA, Pascale MS, Huegel MO. Early experience with the GORE-TEX polytetrafluoroethylene anterior cruciate ligament prosthesis. Am J Sports Med. 1989;17:55-62.
13 Woods GA, Indelicato PA, Prevot TJ. The Gore-Tex anterior cruciate ligament prosthesis. Two versus three year results. Am J Sports Med. 1991;19:48-55.
14 Barrett GR, Line LLJr, Shelton WR, et al. The Dacron ligament prosthesis in anterior cruciate ligament reconstruction. A four-year review. Am J Sports Med. 1993;21:367-373.
15 Paulos LE, Rosenberg TD, Grewe SR, et al. The GORE-TEX anterior cruciate ligament prosthesis. A long-term followup. Am J Sports Med. 1992;20:246-252.
16 Bourke SL, Kohn J, Dunn MG. Preliminary development of a novel resorbable synthetic polymer fiber scaffold for anterior cruciate ligament reconstruction. Tissue Eng. 2004;10:43-52.