Chapter 42 Whipstitch-Post Tibial Fixation for Anterior Cruciate Ligament Reconstruction
Biomechanics
Elongation and Stiffness
The purpose of fixation is to hold the graft without allowing elongation from the fixation site until biological healing has occurred. Elongation can occur from slippage of the fixation device relative to the bone or slippage of the graft relative to the fixation device. Although stiffness has been much considered as an important attribute of ACL graft fixation devices, it is less important than elongation because it only represents the elasticity of the graft–fixation construct prior to the healing of the graft in the tunnel. For BPTB this is roughly 6 weeks. For soft tissue it is 8 to 10 weeks. After this period the stiffness of the fixation device or the extraarticular portion of the graft is no longer part of the load-bearing portion of the structure, which consists only of the intraarticular portion of the graft. In fact, a high-stiffness construct will tend to concentrate mechanical force on the graft–bone interface before graft incorporation has occurred, whereas a low-stiffness construct will dissipate graft strain through elastic deformation of the graft–fixation construct and potentially offer some protection to slippage or elongation at the fixation–bone interface. The WSP method relies on extratunnel cortical fixation and would be a lower-stiffness construct than an aperture-fixated construct because it is longer, if all else were equal. However, To et al1 have shown that the increase in stiffness produced by the use of cortical fixation is much greater than the reduction in stiffness from the greater length of the construct.
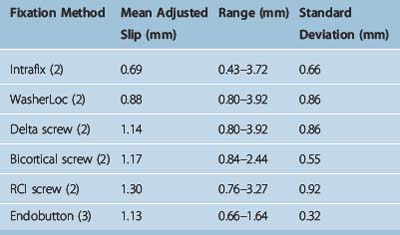
Clinically, grafts usually elongate as a result of cyclical loading, not catastrophic failure. Some of the lowest elongations yet recorded from cyclical loading were published in a recent study of six commonly used devices by Coleridge and Amis2 and are in the range of 1 mm after 1000 cycles. In a recent study we found elongation using WSP fixation to be unsurpassed by any of these fixation devices3,4 (Table 42-1). The standard deviation was also very low, indicating high consistency of the fixation results.
Indirect Versus Direct Fixation
Direct fixation holds direct purchase on the graft. Examples are interference screws and spiked ligament screw washers. Indirect fixation holds purchase through an intermediary substance. Tibial WSP fixation is in the indirect category, as is the fabric loop of Endobutton fixation. Both methods can be used effectively. However, indirect fixation has the added advantage of being able to accommodate a shorter graft. There is evidence that 15 mm5 or less6 is sufficient graft length in the tunnel to allow satisfactory healing. This is all that is needed for indirect fixation such as the WSP described here. Greater length is required for interference screw fixation to allow sufficient length of graft along the interference screw. Even more length is required if a spiked ligament screw washer is used on the tibial cortex because the graft must be long enough to extend out of the tibial tunnel.
Clinical Results
A recent meta-analysis of all HS and BPTB clinical series7 subdivided HS grafts into subgroups by fixation type. The subgroup with the highest stability rates used an Endobutton on the femur and primarily WSP tibial fixation. Of the six high-stability series with no graft failures, four used WSP fixation.8–11 Finally, the study with the overall highest stability rate also used WSP.8 Recently presented data from a series of five-strand hamstring grafts12,13 that used WSP fixation on both the tibia and femur with mean 8-year follow-up had the highest stability rates yet reported for a semitendinosus/gracilis (ST/Gr) graft.8 It should also be pointed out that these stability rates exceeded those found using BPTB from this same meta-analysis.
Morbidity, if the screw is carefully placed, is almost nonexistent. A 0% rate of screw removal due to patient irritation from the cortical screw post has been recently reported in a large series with 2- to 8-year follow-up.11
Surgical Technique
Suitable Tibial Screws
Many suitable products are available (Fig. 42-1). We use the Smith & Nephew 4.5-mm screw, which does not require a washer. The screw is best inserted with a 2.7-mm drill bit rather than the 2.4-mm bit supplied by the company. It should always be tapped. Most screws are 25 to 35 mm in length. Linvatec makes an excellent 6.5-mm screw that we used for years, which does require a washer. Arthrex makes a bioabsorbable screw that we would not recommend (see later discussion). Arthrex also makes a 4.5-mm screw for use without a washer and a 6.5-mm cancellous screw, which is used with a washer. This last screw, however, is used with a small, 2.5-mm, hexagonal screwdriver. In the past we had problems with screwdriver head breakage due to the smaller hexagonal size relative to the larger screw.
Whipstitch Implantation
Tubularization
Conceptually the suture tubularizes the graft. If the graft can be thought of as a sheet (Fig. 42-2), the suture sews the two ends together so that it is essentially folded longitudinally (Fig. 42-3) and then retraces backward, folding it longitudinally again. It is key that the surgeon understands and sees where the suture is going so that he or she does not damage prior placed suture throws with the needle. As previously mentioned, it is imperative that a dyed or striped suture be used. A white suture is difficult to distinguish from the white tendon.
Tensioning
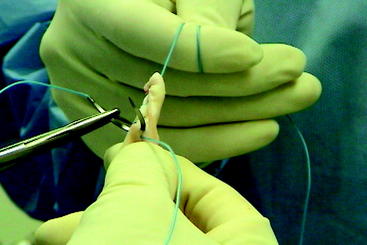
Of equal importance is that the sutures be maximally tightened after roughly every two throws (Fig. 42-4) so that no further tightening takes place after implantation. This requires the assistant to wrap the free suture end twice around his or her finger so that it will not slip while the surgeon wraps the other end around his or her own finger. They are then pulled in opposite directions, maximally tightening the weave. The force required is great, and if the suture is not wrapped properly it is possible to cut one’s finger on the suture (without cutting the glove). This should not happen in practice if care is taken. When the tightening of the weave is complete, the surgeon and assistant will have a sense of transmitting force directly to each other via the suture because no tightening is occurring within the graft.
Techniques for Specific Grafts
Screw Insertion
Unicortical Implantation
The screw should be inserted unicortically and not bicortically for four reasons, as follows:
Troubleshooting
Conclusions
1 To JT, Howell SM, Hull ML. Contributions of femoral fixation methods to the stiffness of anterior cruciate ligament replacements at implantation. Arthroscopy. 1999;15:379-387.
2 Coleridge SD, Amis AA. A comparison of five tibial-fixation systems in hamstring-graft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12:391-397.
3 Prodromos CC, Hecker A. Unpublished data
4 Harvey AR, Thomas NP, Amis AA. The effect of screw length and position on fixation of four-stranded hamstring grafts for anterior cruciate ligament reconstruction. Knee. 2003;10:92-102.
5 Zantop T, Brucker P, Bell K, et al. The effect of tunnel-graft length on the primary and secondary stability in ACL reconstruction: a study in a goat model. Presented at the 2006 meeting of the European Society of Sports Traumatology, Knee Surgery, and Arthroscopy, Innsbruck, Australia, May, 2006. 2006.
6 Yamazaki S, Yasuda K, Tomita F, et al. The effect of intraosseous graft length on tendon-bone healing in anterior cruciate ligament reconstruction using flexor tendon. Knee Surg Sports Traumatol Arthrosc. 2006;14:1086-1093.
7 Prodromos CC, Joyce BT, Shi K, et al. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar-tendon graft and fixation type. Arthroscopy. 2005;21:1202-1208.
8 Cooley VJ, Deffner KT, Rosenberg TD. Quadrupled semitendinosus anterior cruciate ligament reconstruction: 5-year results in patients without meniscus loss. Arthroscopy. 2001;17:795-800.
9 Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:564-573.
10 Hamada M, Shino K, Horibe S, et al. Preoperative anterior knee laxity did not influence postoperative stability restored by anterior cruciate ligament reconstruction. Arthroscopy. 2000;16:477-482.
11 Prodromos CC, Han YS, Keller BL, et al. Stability results of hamstring anterior cruciate ligament reconstruction at two- to eight-year follow-up. Arthroscopy. 2005;21:138-146.
12 Prodromos CC, Joyce BT. Five-strand hamstring ACL reconstruction: a new technique with better long-term stability than four-strand. Presented at the 2006 meeting of the Arthroscopy Association of North America, Hollywood, FL, May, 2006. 2006.
13 Prodromos CC, Fu F, Howell S, et al. Controversies in soft tissue anterior cruciate ligament reconstruction. Presented at symposium at the 2006 of the American Academy of Orthopaedic Surgeons, Chicago, March, 2006. 2006.
15 Post WR, King SS. Neurovascular risk of bicortical tibial drilling for screw and spiked washer fixation of soft-tissue anterior cruciate ligament graft. Arthroscopy. 2001;17:244-247.
16 Curran TA, Sekiya JK, Gibbs AE, et al. Two techniques for anterior cruciate ligament tibial fixation with a bicortical screw: an in vitro study of neurovascular risk. Am J Orthop. 2006;35:261-264.