Chapter 543 Vulvovaginitis
Etiology
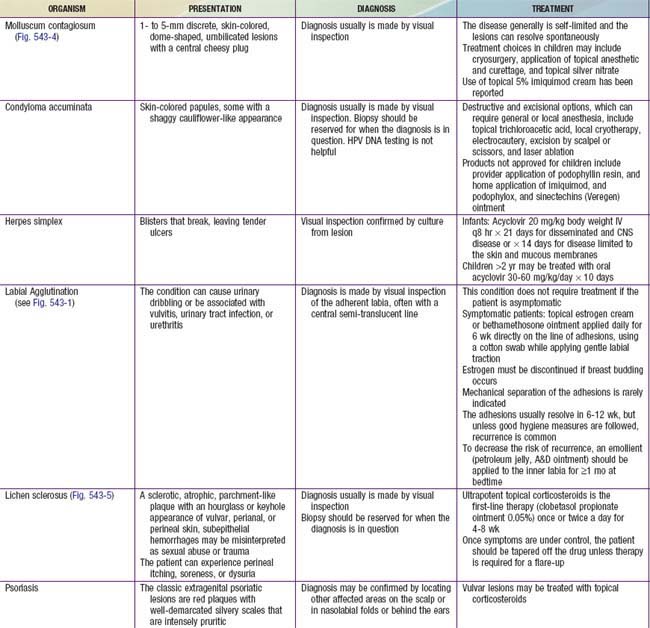
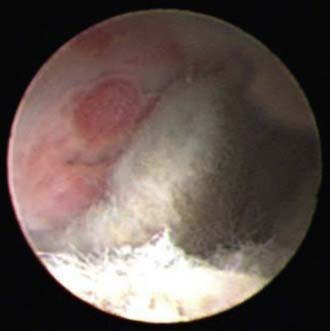
Vulvitis refers to external genital pruritus, burning, redness, or rash. Vaginitis implies inflammation of the vagina, which manifests as a discharge with or without an odor or bleeding. Vaginitis can cause vulvitis. When a child presents with vulvovaginitis, the history should include questions on hygiene (wiping from front to back) and information about possible chemical irritants (bath soaps, laundry detergents, swimming pools, or hot tubs). The caregiver can be asked about a history of diarrhea, perianal itching, or nighttime itching. The possibility of foreign objects being placed into the vagina should also be asked, although the young child is unlikely to remember or recall. Children are especially prone to nonspecific vulvovaginitis for a variety of reasons, including their nonestrogenized state, poor perianal hygiene, and the proximity of the anus to the vagina, which is without geographic barriers given the flattened labia and lack of pubic hair. Labial adhesions occur under similar conditions (Fig. 543-1 and Table 543-1).
Epidemiology
Infectious vulvovaginitis, where a specific pathogen is isolated as the cause of symptoms, may be caused by fecal or respiratory pathogens, and cultures might reveal Escherichia coli (Chapter 192), Streptococcus pyogenes, Staphylococcus aureus (Chapter 174), Haemophilus influenzae (Chapter 186), and, rarely, Candida spp. (Chapter 226). These organisms may be transmitted by the child using improper toilet hygiene and manually from the nasopharynx to the vagina. The children present with perianal redness, an inflamed introitus, and often a yellow-green or mildly bloody discharge. They may be observed to be grabbing their genital area or “digging” in their underwear, which is usually stained with yellow-brown discharge. Attempts to treat these bacterial etiologies with antifungal medication will fail; Table 543-2 gives specific recommendations.
Table 543-2 ANTIBIOTIC RECOMMENDATIONS FOR SPECIFIC VULVOVAGINAL INFECTIONS
| ETIOLOGY | TREATMENT |
|---|---|
TMP-SMX, trimethoprim-sulfamethoxazole; MRSA, methicillin-resistant Staphylococcus aureus.
Neisseria gonorrhoeae or Chlamydia trachomatis also are causes of specific infectious vulvovaginitis (Chapter 114). Management of children who have sexually transmitted infections (STIs) requires close cooperation between clinicians and child-protection authorities. Official investigations for sexual abuse, when indicated, should be initiated promptly (Chapter 371). If acquired after the neonatal period, some diseases (e.g., gonorrhea, syphilis, chlamydia) are 100% indicative of sexual contact. For other diseases (e.g., HPV infection and HSV), the association with sexual contact is not as clear. Although Trichomonas vaginalis can be transmitted vertically and can be seen in the newborn, it is an uncommon cause of specific infectious vulvovaginitis in the unestrogenized prepubertal girl.
Clinical Manifestations
Genital Ulcers
Aphthous ulceration of the vulva (Fig. 543-2) in children and adolescents who are not sexually active is well described and can occur in association with oral aphthous ulcers or Epstein-Barr virus infection (Chapter 246). These lesions usually appear in the vestibule and begin as a painful red area that evolves into a sharply demarcated red-rimmed ulcer with a necrotic or eschar-like base. The time course is generally 7-14 days until remission occurs. The lesions are often so painful that urinary diversion with a Foley catheter is necessary. The only way to confirm this clinical diagnosis is to rule other conditions, including herpes, chancroid lesion, Crohn’s disease, and syphilitic chancres. Treatment includes good hygiene, topical lidocaine, oral antibiotics to prevent superinfection, and short-term systemic steroids. The lesions can recur, and evaluation for Behçet’s disease (Chapter 155) using the International Study Group diagnostic guidelines should be considered. See Table 543-1 for other common etiologies.
Diagnosis and Differential Diagnosis
If pinworms (Chapter 286) are suspected, transparent adhesive tape or an anal swab should be applied to the anal region in the morning before defecation or bathing and then placed on a slide. Eggs seen on microscopic examination confirm the diagnosis, and sometimes the pinworms can be seen at the anal verge. Several samples may be required to detect the eggs, and false negative results still can occur.
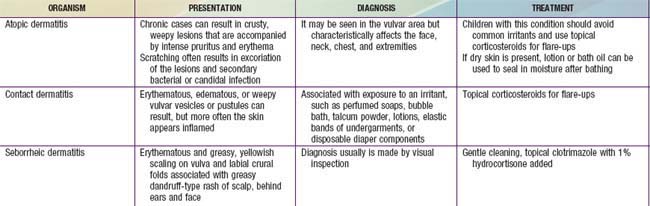
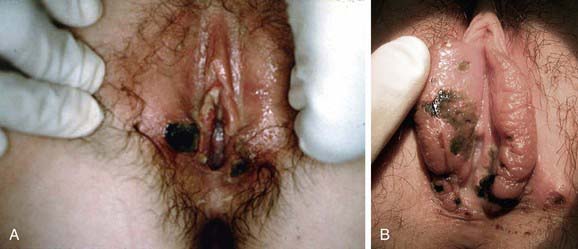
If the vaginal discharge is serosanguineous, if a foul odor is present, or if the discharge fails to respond to hygiene measures, consider presence of a vaginal foreign body (Fig. 543-3). If inspection suggests presence of a foreign body, the vagina can be irrigated, or an examination under anesthesia may reveal the foreign body. Vaginoscopy is an excellent diagnostic tool and can be performed in an unsedated cooperative patient in an outpatient setting or under general anesthesia if necessary. Using a cystoscope with saline or water irrigation to gravity, insert the endoscopic device into the vagina, gently oppose the labia, the vagina will distend and the entire vaginal cavity and cervix may be easily assessed.
Treatment and Prevention
The treatment of specific vulvovaginitis should be directed at the organism causing the symptoms (see Table 543-1). Treatment of nonspecific vulvovaginitis includes sitz baths and avoidance of irritating or harsh soaps and chemicals and tight clothing that abrades the perineum. External application of bland emollient barriers such as over-the-counter diaper rash medications and petroleum jelly may be helpful. Proper perineal hygiene is critical for long-term improvement. Younger children need supervised perineal hygiene, and caregivers should be advised to wipe the genital area from front to back. Use of a warm moistened washcloth or diaper wipe is helpful after initial wiping with toilet tissue. Little girls should wear cotton-only underwear and limit time spent in tights, leotards, and wet swimsuits. Soaking in warm clean bathwater for 15-minute intervals (no shampoo or bubble bath) is soothing and helps with cleaning the area. The parents should be counseled to avoid all scented, antiseptic and deodorant-based soaps and eliminate the use of fabric softeners or dryer sheets when laundering undergarments.
Fleischer ABJr. Diagnosis and management of common dermatoses in children: atopic, seborrheic, and contact dermatitis. Clin Pediatr. 2008;47:332-346.
Huppert JS, Geerber MA, Deitch HR, et al. Vulvar ulcers in young females: a manifestation of apthosis. J Pediatr Adolesc Gynecol. 2006;19:195-204.
Morrell DS, Nelson KC. Spreading bumps: molluscum contagiosum in the pediatric population. Pediatr Ann. 2007;36(814):816-818.
Lewin LC. Sexually transmitted infections in preadolescent children. J Pediatr Health Care. 2007;21:153-161.
Merritt DF. Genital trauma in the pediatric and adolescent female. Obstet Gynecol Clinics N Amer. 2009;36:85-98.
Myers JB, Sorensen CM, Wisner BP, et al. Bethamethosone cream for the treatment of pre-pubertal labial adhesions. J Pediatr Adolesc Gynecol. 2006;19:407-411.
Poindexter G, Morrell DS. Anogenital pruritus: lichen sclerosus in children. Pediatr Ann. 2007;36:785-791.
Schober J, Dulabon L, Martin-Alguacil N, et al. Significance of topical estrogens to labial fusion and vaginal introital integrity. J Pediatr Adolesc Gynecol. 2006;19:337-339.
Smolinski KN, Yan AC. How and when to treat molluscum contagiosus in children with imiquimod 5% cream. Br J Dermatol. 2003;149(Suppl 66):25-29.
Sukhatme SV, Gottlieb AB. Pediatric psoriasis: updates in biologic therapies. Dermatol Ther. 2009;22:34-39.