CHAPTER 14 Volar Rim and Barton’s Fracture
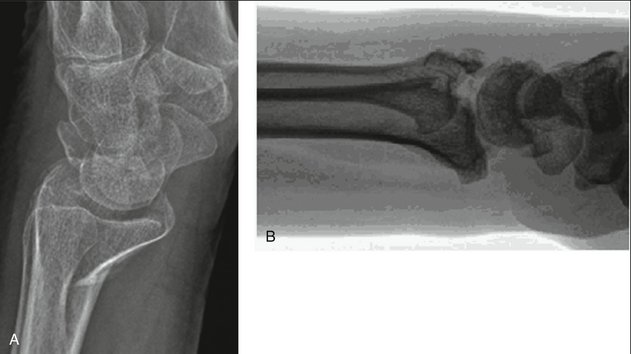
In 1838 John Rhea Barton described a specific fracture pattern of the distal radius characterized by a shearing injury to a portion of the articular and metaphyseal surface and subluxation of the carpus: “The fragment may be, and usually is, quite small, and is broken from the end of the radius … and through the cartilaginous face of it, and necessarily into the joint.”1 Although some disagreement has existed about whether Barton’s original article limited the fracture to a dorsal or a volar displacement, it is now well accepted that the volar articular marginal shearing pattern is more common.2 Therefore, to avoid confusion we will describe Barton’s fractures as either volar or dorsal (Fig. 14-1).
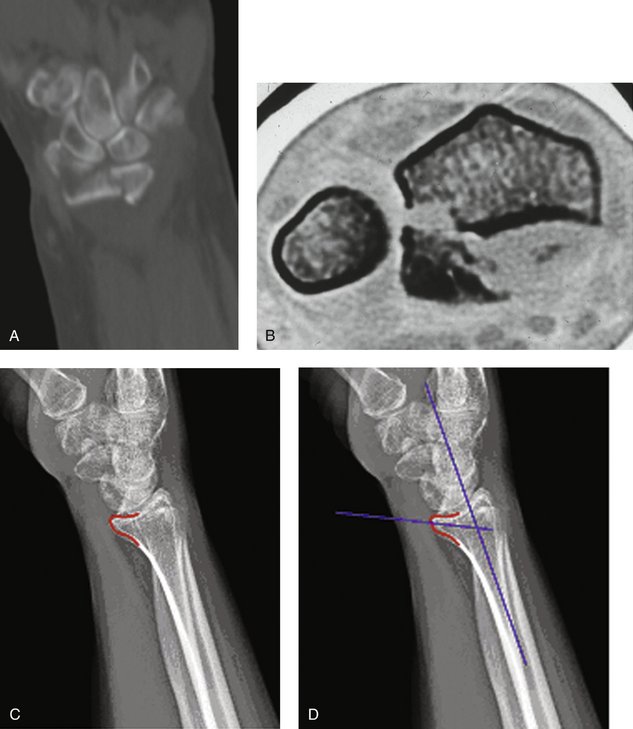
Volar rim and volar or dorsal Barton’s fractures are considered among marginal articular shearing type fractures. In the case of these marginal fractures, the shearing mechanism and obliquity of the fracture line result in volar and proximal subluxation of the carpus. The volar surface of the distal radius is relatively flat. However, the very distal margin slopes volarly in the form of a ridge from which the volar radiocarpal ligaments take origin. It is also important to understand that when viewed in cross section, the distal radial cortical margin slopes volarly from radial to ulnar and, in fact, has a slight dorsal turn just before terminating in the volar edge of the semilunar notch, giving it a somewhat convex appearance. The ulnar volar margin of the lunate facet slopes volarly from a proximal to distal direction. Thus, the volar lunate facet extends more distally than expected and effective support of this area with a plate can be challenging (Fig. 14-2).3–5 In addition, anatomical studies demonstrate that the short radiolunate ligament originates from the volar margin of the lunate facet and attaches to the volar surface of the lunate. It is proposed that this ligament may play a vital role in the stability of the radiocarpal articulation.6 Radiographic assessment of the volar lunate facet is best accomplished with a lateral projection inclined 10 degrees proximally, thereby providing a distinct profile of the articular surface and assessment of the “teardrop,” or U-shaped, outline of the volar rim of the lunate facet (see Fig. 14-2C).7 Normally, a line drawn down the central axis of the teardrop creates an angle of 70 degrees to the central axis of the radial shaft (see Fig. 14-2D). 7 A volar lunate facet fragment that is displaced or rotated can be identified by displacement of the teardrop and disruption of the teardrop angle. This will create a functional incompetence of the short radiolunate ligament, leading to radiocarpal instability.
In comparison to its volar counterpart, dorsal Barton’s fractures are less common injuries and are often included in the spectrum of radiocarpal dislocations or complex articular fractures. The mechanism of injury is similar to volar injuries but with a dorsally directed shearing force, resulting in dorsal cortical compromise and proximal migration of the carpus. The definition of a Barton’s fracture is a shearing marginal articular fragment and requires maintenance of an intact opposite cortex.8 Confusion between a true dorsal Barton’s fracture versus either a radiocarpal fracture-dislocation or a complex articular fracture can be clarified by reviewing the AO classification of distal radius fractures (Table 14-1).9 Type B fractures are partial articular fractures of the distal radius and encompass dorsal Barton’s (type B2) and volar Barton’s (type B3) fractures and include maintenance of an intact opposite cortex. In comparison, the AO type C fracture patterns are complete articular fractures of the distal radius with multiple articular and metaphyseal fragments and therefore are not shear fractures and should not be considered a Barton fracture.
TABLE 14-1 AO Classification of Distal Radius Fractures
| Type A | Extra-articular |
| A1 | Extra-articular ulna fracture with radius intact |
| A2 | Extra-articular radius fracture with ulna intact |
| A3 | Extra-articular multifragmented radius fracture |
| Type B | Partial articular |
| B1 | Sagittal plane fracture of radius |
| B2 | Dorsal rim (Barton’s) fracture of radius |
| B3 | Volar rim (Barton’s) fracture of radius |
| Type C | Complete articular |
| C1 | Simple articular and metaphyseal fracture of radius |
| C2 | Simple articular fracture with multifragmented metaphysis |
| C3 | Multifragmented articular fracture |
Indications
The traditional variables of instability (age >60, extent of initial deformity, dorsal comminution, and associated ulna fracture) cannot be applied readily to these fractures.10 Our indications for open reduction and internal fixation of marginal fractures of the distal radius include:
Surgical Technique
In addition, to approach more ulnar fragments such as the volar lunate facet fragment, the volar ulnar approach is utilized. This interval lies between the ulnar nerve and artery and the flexor tendons of the fingers. To help visualization and mobilization of the interval, the approach is extended distally with release of the carpal tunnel.8
Volar Barton’s Fracture
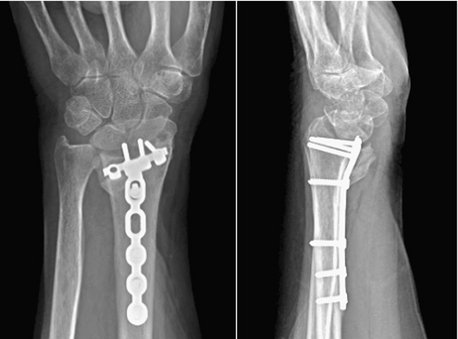
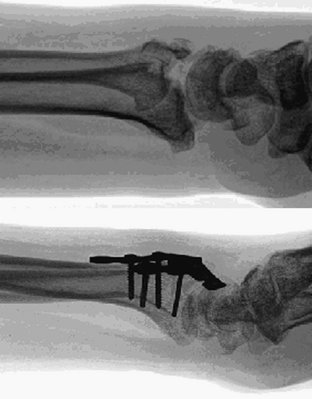
The vast majority of volar Barton’s fractures can be reduced with a combination of dorsiflexion over a bolster, manual digital traction applied by an assistant, and manipulation under direct vision with a Freer elevator. Should there be any articular depression, then this can be elevated by working through the fractured surface. A T-shaped volar plate of sufficient length is applied to ensure fixation of two bicortical screws proximal to the fracture in the radius. The plate is undercontoured and applied so that on tightening the proximal screws the plate assists in reducing the fracture by pushing it distal and buttressing it. Reduction of the articular surface is confirmed with the wrist imaged in the lateral view and the x-ray beam inclined 10 degrees from distal to proximal.7 Although placement of distal screws is not always necessary, we routinely use them because we see no disadvantage to their careful placement (Fig. 14-3). In closure, the pronator quadratus is carefully closed over the plate if possible. Postoperatively the wrist is placed in a splint for 5 to 10 days, after which sutures are removed and active wrist motion is initiated.
Volar Shearing Fracture with a Volar Lunate Facet Fragment
Before approaching volar shearing fractures, obtaining a preoperative computed tomographic (CT) scan is prudent to specifically look for a volar lunate facet fragment (see Fig. 14-2A, B). Jupiter and associates demonstrated that a significant number of volar marginal shearing fractures have two or more such articular fragments.11 Intraoperatively, every effort is made to confirm the presence or absence of these fragments. If required, the surgical approach is directed ulnar, through the interval between the flexor tendons and the ulnar neurovascular structures, so as to adequately visualize this area because it may not always be visible or accessible through a standard volar approach. Extension of the incision distally with release of the carpal tunnel will aid in visualization and soft tissue mobilization. Implants are placed to achieve stable buttressing of the volar lunate facet/corner. If a single implant does not span the entire width of the radius, then the surgeon should support this fragment with an additional small plate. In situations in which the fragment is extremely small, a Kirschner wire (K-wire) is passed through the fragment to exit dorsally. Alternatively, a suture passed through the volar short radiolunate ligament and through drill holes in the volar distal radial metaphysis in the form of a figure of eight can provide fixation of this fragment.12 Reduction of the volar lunate facet fragment is checked with the wrist imaged in the lateral view and the x-ray beam inclined 10 degrees from distal to proximal and thereby confirming reconstitution of the “teardrop” or the volar rim of the lunate facet.7 Stable fixation of this fragment is critical in prevention of its displacement during the rehabilitation phase. Displacement of this fragment is usually associated with volar subluxation of the carpus, a reduction in ultimate range of motion in the wrist, and degenerative changes in the radiocarpal articulation (Fig. 14-4).
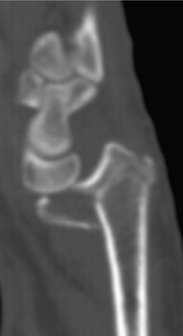
Volar Marginal Shearing Fracture with a Dorsal Cortical Fracture
This particular subset of volar shearing fractures of the distal radius is usually seen in older women and includes a portion of the distal radial articular surface with an oblique metaphyseal fracture line extending dorsally (Fig. 14-5). The articular fragment tends to displace volarly and in doing so takes the carpus with it, subluxing volarly and proximally. Plate fixation with an undercontoured volar buttress plate is to be avoided in the treatment of this injury because it leads to displacement of the entire juxta-articular portion of the distal radius in a dorsal direction, such that the articular surface may be angulated dorsally.13 It is therefore critical to be aware of this possibility. In the preoperative assessment of these patients, we recommend radiographs taken in standard planes without any plaster splints that may obscure an occult fracture line. Furthermore, if concern still exists, then a CT scan to rule out or confirm an occult dorsal cortical fracture is highly recommended (Fig. 14-6). In situations in which a dorsal cortical fracture line is identified, a fully contoured volar plate is applied. The distal screw holes are utilized, and no attempt is made to undercontour the plate. The volar fragment is provisionally fixed to the radius with a K-wire, and this construct is neutralized with a volar locking plate. This allows anatomical reduction of the articular fracture and prevents dorsal angulation of the entire articular surface (Fig. 14-7).
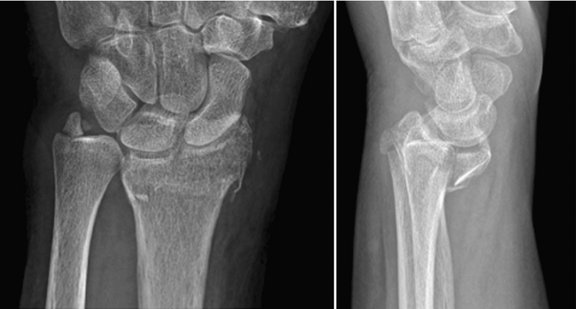
FIGURE 14-5 Radiographs of volar shearing fracture of the distal radius with dorsal cortical extension.
Dorsal Barton’s Fracture
Before approaching dorsal Barton’s fractures, a preoperative CT scan is prudent to evaluate the number of dorsal fragments, evaluate for the presence of volar avulsion fragments, and assess for a possible radial styloid fracture. The dorsal surface is approached through the floor of the third dorsal compartment. Dorsal comminution is the rule, and marginal fragments are mobilized along with the dorsal capsule so that they could be reflected distally. With in-line traction and a slight flexion moment being performed by the assistant, the fracture can be readily reduced. Metaphyseal defects can be filled with bone graft or substitutes of the surgeon’s preference. A dorsal plate is applied as a buttress plate. In cases of comminution or severe subchondral bone loss a locking dorsal plate is preferred to support the articular surface (Fig. 14-8). Reduction of the articular surface is confirmed with the wrist imaged in the lateral view with the x-ray beam inclined 20 degrees from distal to proximal.
Radiocarpal Fracture-Dislocations
Radiocarpal fracture-dislocations can result in either a volar or a dorsal dislocation of the carpus, but the dorsal pattern is most common. Fixation of these injuries requires a four-stage approach (Fig. 14-9). First, the standard volar approach is utilized and the radiocarpal joint is examined through the capsular violation. The joint is irrigated and débrided of any entrapped osteochondral fragments. Avulsion fractures, most commonly of the radial styloid, are then internally fixed with either a radial or volar plate or, alternatively, with lag screws placed through the styloid into the proximal ulnar cortex of the radius. Second, volar capsular violations are repaired with the aid of suture anchors and any remaining avulsed marginal fractures are also fixed and may require utilization of the volar ulnar approach. Third, when the dorsal rim of the distal radius is involved a second dorsal incision is made and the radiocarpal joint is approached through the floor of the third dorsal compartment. Impacted articular rim fragments are elevated, defects are bone grafted, and a dorsal buttress plate can be applied. Last, the fourth stage involves fixation of the ulnar styloid, if fractured and if intraoperative examination of the distal radioulnar joint suggests instability.
Results
Review of the literature finds that operative fixation of these fractures is effective. But the use of the Barton eponym has made critical study of the morphology of articular margin fractures of the distal radius imprecise. Jupiter and colleagues studied 49 volar intra-articular fractures in patients who underwent T-plating; there were 31 excellent, 10 good, and 8 fair results by Gartland and Werley scoring.11 Interestingly, these authors reported the high incidence of at least two or more fragments of the volar articular surface and stressed the importance of recognizing this preoperatively to aid in planning of the approach and appropriate type of fixation.
Harness and coworkers examined outcomes in 7 patients who had loss of fixation of the volar lunate facet after volar plating of a distal radius fracture.3 Five of these patients elected to undergo revision fixation. In this subgroup, there were 2 excellent, 2 fair, and 1 poor outcome. Both patients who elected not to undergo revision fixation were classified as having a good outcome. When the two groups were compared, there was no significant difference in the range of motion, but patients who had revision fixation were noted to demonstrate decreased grip strength. Whereas articular restoration appears paramount, and revision fixation would seem intuitive, the results of this study appear to suggest otherwise. However, the small sample size in this study precludes drawing any firm conclusions from these data.
Harness and coworkers also examined volar rim fractures with unrecognized extension of the dorsal cortex of the distal radius in 5 patients. The use of an undercontoured plate resulted in a loss of normal volar tilt and an average dorsal tilt of 6 degrees.13 They stressed the importance of identifying compromise of the dorsal cortex and recommended the use of a contoured volar locking plate in those circumstances.
Lozano-Calderón and colleagues studied dorsal articular margin fractures in 20 patients, 7 of whom needed combined dorsal and volar fixation. There were 6 excellent, 12 good, and 2 fair results based on the modified Gartland and Werley scoring system.14 These researchers warned of the inherent instability of dorsal articular margin fractures owing to their predilection toward dorsal radiocarpal subluxation or dislocation and also of associated volar ligament injuries, volar avulsion fractures, or articular impaction. A combined dorsal and volar exposure is often necessary for these injuries to treat the central articular impaction and the radiocarpal instability.
Mudgal and colleagues reviewed their series of radiocarpal fracture-dislocations and illustrated the rarity of these injuries but their predilection toward dorsal dislocation, a high-energy mechanism, and sensory impairment.15 Using volar and dorsal fixation they achieved 5 excellent and good, 2 fair, and 2 poor results in patients free of any associated intercarpal injuries. In the 2 patients with associated intercarpal injuries, the results were 1 fair and 1 poor, indicating that these fractures when associated with intercarpal injuries may have significantly compromised outcomes.
1. Barton JR. Views and treatment of an important injury of the wrist. Med Exam. 1838;1:365-368.
2. Thompson GH, Grant TT. Barton’s fractures–reverse Barton’s fractures: confusing eponyms. Clin Orthop Relat Res. 1977;122:210-221.
3. Harness NG, Jupiter JB, Orbay JL, et al. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Joint Surg [Am]. 2004;86:1900-1908.
4. Mekhail AO, Ebraheim NA, McCreath WA, et al. Anatomic and x-ray film studies of the distal articular surface of the radius. J Hand Surg [Am]. 1996;21:567-573.
5. Andermahr J, Lozano-Calderon S, Trafton T, et al. The volar extension of the lunate facet of the distal radius: a quantitative anatomic study. J Hand Surg [Am]. 2006;31:892-895.
6. Berger RA, Landsmeer JM. The palmar radiocarpal ligaments: a study of adult and fetal human wrist joints. J Hand Surg [Am]. 1990;15:847-854.
7. Medoff RJ. Essential radiographic evaluation for distal radius fractures. Hand Clin. 2005;21:279-288.
8. Fernandez DL, Jupiter JB, editors. Fractures of the Distal Radius: A Practical Approach to Management. New York: Springer, 2002.
9. Cohen MS, McMurtry RY, Jupiter JB. Fractures of the distal radius. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal Trauma. 2nd ed. Philadelphia: WB Saunders; 1998:1385.
10. LaFontaine M, Hardy D, Delince PH. Stability assessment of distal radius fractures. Injury. 1989;20:208-210.
11. Jupiter JB, Fernandez DL, Toh CL, et al. The operative management of volar articular fractures of the distal end of the radius. J Bone Joint Surg Am. 1996;78:1817-1828.
12. Chin KR, Jupiter JB. Wire-loop fixation of volar displaced osteochondral fractures of the distal radius. J Hand Surg [Am]. 1999;24:525-533.
13. Harness N, Ring D, Jupiter JB. Volar Barton’s fractures with concomitant dorsal fracture in older patients. J Hand Surg. 2004;29:439-445.
14. Lozano-Calderón SA, Doornberg J, Ring D. Fractures of the dorsal articular margin of the distal part of the radius with dorsal radiocarpal subluxation. J Bone Joint Surg Am. 2006;88(7):1486-1493.
15. Mudgal CS, Psenica J, Jupiter JB. Radiocarpal fracture-dislocation. J Hand Surg [Br]. 1999;24:92-98.