CHAPTER 13 Volar Plate Fixation
Fractures of the distal end of the radius have been estimated to account for nearly 20% of all fractures seen routinely in an emergency department.1 Despite this, until very recently the distal radius fracture was not treated as aggressively as other less common periarticular fractures. Perhaps Abraham Colles’ perception that this fracture had good outcomes no matter what was done had permeated our thinking. The reality is that frequent poor outcomes in wrist injury fueled a gradual, albeit delayed, pursuit of a better treatment option.2
Rationale and Basic Biomechanics
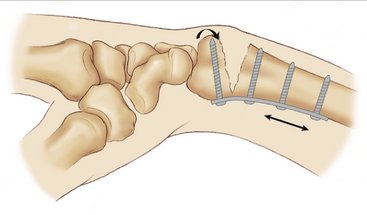
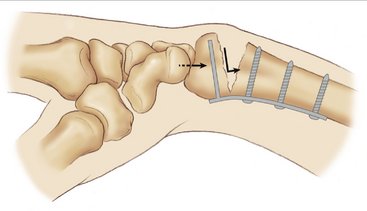
Although the concept of volar plating could be initially attributed to Lanz and Kron3 back in 1976 for plate fixation after osteotomy of malunited distal radius fractures, the volar approach remained restricted to fixation of volar rim fractures in the acute setting only.4 Volar plating was first recommended for fixation of both typical and atypical distal radius fractures by Georguoulis and associates in 1992.5 This was published in a little-known journal and was not widely accepted for dorsally displaced fractures until the landmark paper by Orbay and Fernandez in 2002.6 Volar plating offers many advantages when used in dorsally displaced fractures. The key to its success is to ensure that this was a locking plate, hence creating a fixed-angle device that would maintain the reduction and eliminate screw toggle (Fig. 13-1). Volar plating also provides the opportunity to release the pronator quadratus muscle, which is often trapped in the fracture and can be a cause of pronation contracture. A nonlocking plate when used in buttress mode can resist only moderate axial and bending forces. Thus, a simple nonlocking volar plate used in a dorsally displaced fracture without any bony contact in the opposite cortex is subject to much higher axial and bending loads, leading to failure. Therefore, a stable and strong volar fixation of a dorsally displaced fracture is only possible with a fixed-angle locking plate that can resist such high forces. Fixed-angle implants transfer load stress from the fixed distal fragment to the intact radial shaft, thus enhancing peg/plate/bone construct stability (Fig. 13-2), unlike rigid internal fixation devices that rely mainly on the frictional force between plate and bone to achieve fixation.7
The ideal volar implant should have a design compatible with the volar articular surface of the radius and should provide concomitant angular and axial stability while stabilizing the dorsal surface.8 The distal volar plate (DVR Hand Innovations, Depuy Orthopedics, Warsaw, Indiana) has two parallel rows, and the orientation planes of their respective pegs specifically match the complex three-dimensional shape of the radial articular surface. The primary row pegs are directed obliquely from proximal to distal to support the dorsal aspect of the articular surface. They are angled accurately to provide support for the radial styloid and the dorsal ulnar fragment. These pegs are most effective in supporting the dorsal aspect of the subchondral plate and hence avoid the re-displacement of the dorsally displaced fractures. Concurrently, their action induces a volar force that tends to displace the fragments in a volar direction, an effect that must be opposed by a properly configured volar buttressing surface. To enhance fracture fixation in cases of severe comminution, volar instability, or osteoporosis, an additional row of pegs originating from a more distal position on the plate and having an opposite inclination to the proximal row was conceived. The distal row is directed in a relatively proximal direction and crosses the proximal row at its midline and is intended to support the more volar and central part of the subchondral bone. It prevents the dorsal rotation of a volar marginal fragment and volar rotation of severely osteoporotic or unstable distal fragments with central articular comminution, thus neutralizing volar displacing forces of the pegs in the proximal row.
Indications and Contraindications
An unstable distal radius fracture has been defined as a fracture that, after an attempt at closed reduction, demonstrates radiographic evidence of more than 15 degrees of angulation in any plane, articular step-off of more than 2 mm, and/or radial shortening of more than 2 mm.6 However, fractures with severe comminution or pronounced initial articular displacement or that are simply osteoporotic are also termed “unstable” despite possible initial good alignment.
Surgical Technique
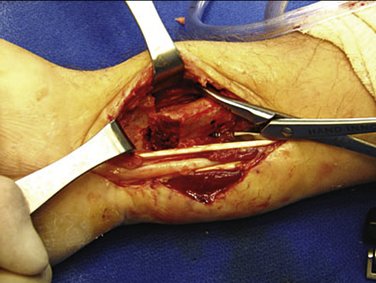
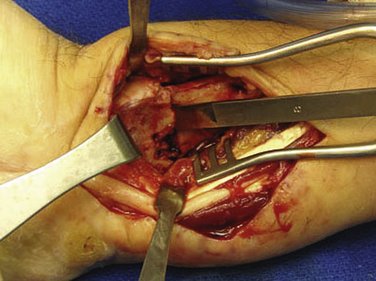
The patient is placed in the supine position with the arm extended on the hand table. A simple fracture less than 7 to 14 days old can be managed through a standard flexor carpi radialis (FCR) approach (distal Henry) (Fig. 13-3). On the other hand, complex intra-articular fractures, nascent malunions, and 2- to 3-week old fractures require a more extensile exposure, facilitated via the extended FCR approach.9 This approach allows an intrafocal reduction by using the fracture plane itself to reduce the articular major fragments. The radial shaft (proximal fragment) is rotated into pronation (Fig. 13-4), allowing fracture reduction, and the shaft is then supinated back into anatomical position. The first step is to release the sheath of the FCR and identify the pronator quadratus between the FCR sheath floor and radial artery, which seats deep to the flexor pollicis longus and flexor digitorum superficialis muscle bellies. An L-shaped incision is made in the fascia of the pronator quadratus to allow proximal and ulnar reflection to expose the fracture site and distal shaft of the radius. A more thorough exposure of the volar surface of the radius, including the volar rim of the lunate fossa, is then performed. At this point, the brachioradialis must be released subperiosteally to improve exposure and allow reduction of the radial column. Specifically, the sheath of the first dorsal compartment is opened starting proximally, the abductor pollicis longus is retracted, and the insertion of the brachioradialis on the radial styloid is identified. A step-cut tenotomy can alternatively be performed to facilitate later repair if desired. Releasing this radial septum eliminates the major deforming forces on the radial column, and reduction can be achieved much more easily. Reduction of less complex fractures is now done by longitudinal traction on the fingers by the assistant and volar flexion of the wrist; the plate is applied manually once bony length and volar tilt is restored. Insertion of a Freer elevator or narrow osteotome into the fracture site and levering the metaphysis dorsally and distally may be helpful to restore length and critical volar tilt (Fig. 13-5). The longitudinal slot in most plates is used for the initial diaphyseal screw so that later plate adjustment can be easily made if needed. While traction and wrist flexion is maintained, the distal locking screw/peg is now inserted. With most fractures, this will suffice to hold the reduction transiently while plate placement/reduction is checked on fluoroscopy. If this is satisfactory, the remainders of the locking screws distally are placed, followed by the shaft fixation for further strength. Gross examination of the plate placement also is necessary to ensure there is not impingement of the distal radioulnar joint or the radial soft tissues, which can cause postoperative discomfort (Fig. 13-6). Fractures with die-punch components or reduction difficulty due to early healing may require the extended FCR approach. This requires that the proximal radius is mobilized, elevated, and pronated out of the field to access the dorsal and articular aspect of the fracture. This facilitates proper débridement of the fracture hematoma or callus and hence reduction of the complex articular injuries. The dorsal periosteum and any organized hematoma/early callus is then excised with a rongeur. The same technique is used in cases of osteoporotic bone, whereas malunions or nonunions require a modified technique that incorporates a dorsal opening wedge osteotomy by a volar approach. In these cases, it is imperative to use the extended FCR approach to expose the dorsal aspect of the distal radius, allowing release of the dorsal periosteum and soft tissues, achieving of the required correction, and application of the cancellous autografts. The fixed-angle plate is fixed first to the proximal fragment and the distal fragment is reduced to it with traction and direct manipulation of the distal fragment to obtain the necessary volar tilt. Our preferred strategy is to attach the plate to the distal fragment first and then lever the distal fragment into correction by relying on the variable-angle peg fixation. This allows restoration of volar tilt in a much more controlled manner.
We believe that the median nerve should be decompressed due to swelling from both the fracture itself and the operative procedure. Routine endoscopic carpal tunnel release using an Agee10 endoscopic blade is performed (Fig. 13-7). In grossly displaced fractures, the carpal tunnel release is done after reduction of the fracture so to normalize carpal anatomy and prevent iatrogenic injury to the median nerve.11 However, the majority of endoscopic releases in the fracture scenario are performed before reduction to get the endoscopic equipment away from the field. The concept of releasing the carpal tunnel and decompressing the nerve has two advantages: (1) the nerve release obviously helps relieve current median nerve symptoms and prevent the development of late post-traumatic carpal tunnel syndrome and (2) decompressing the carpal canal allows one to free the nine tendons constrained within the tunnel, worse so because of trauma. Consequently, the flexion/extension of the fingers is much easier, and less painful, in the immediate recovery phase. We are convinced this helps minimize the development of sympathetic-mediated pain syndromes.
Volar plating can also be combined with arthroscopic débridement to accurately assess the reduction and perhaps improve on it. Die-punch fractures can be elevated and reduced just before volar plate placement if necessary. The concept of arthroscopic-assisted fixation has been used by a few surgeons and offers the advantage of more accurate articular reduction and improved joint débridement.12,13 An added benefit is that concomitant soft tissue injuries, such as triangular fibrocartilage complex or intercarpal ligament injuries, can be diagnosed and managed at the time of internal fixation of the distal radius. This arthroscopic assistance is usually reserved for younger patients with high-energy injuries or the most severe fracture patterns with articular comminution. The typical elderly patient is not indicated for arthroscopy because underlying degenerative changes are present and the wrist demands are not as great.
Results and Complications
Harness and colleagues14 noted that volar plating, however, was unable to control a very distal volar lunate facet fragment, regardless of the type of implant. They reported on a cohort of patients with a volar shearing fracture of the distal end of the radius in whom the unique anatomy of the distal cortical rim of the radius led to failure of support of a volar ulnar lunate facet fracture fragment.
Brief Literature Review
Rozental and Blazar15 studied 41 patients with a mean age of 53 years with an average follow-up of 17 months. All fractures were stabilized with volar locking plates. Radiographs in the immediate postoperative period showed a mean radial height of 11 mm, mean radial inclination of 21 degrees, and mean volar tilt of 4 degrees. At fracture healing the mean radial height was 11 mm, mean radial inclination was 21 degrees, and mean volar tilt was 5 degrees. The average score on the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire was 14, and all patients achieved excellent and good results on the Gartland and Werley scoring system, indicating minimal impairment in activities of daily living. Nine patients experienced postoperative complications. There were four instances of loss of reduction with fracture collapse, 3 patients required hardware removal for tendon irritation, 1 patient developed a wound dehiscence, and 1 patient had metacarpophalangeal joint stiffness.
Orbay and Fernandez,16 using a volar approach, treated a consecutive series of 29 patients with 31 dorsally displaced, unstable distal radial fractures with a new fixed-angle internal fixation device. At a minimal follow-up time of 12 months the fractures had healed with highly satisfactory radiographic and functional results. The final volar tilt averaged 5 degrees; radial inclination, 21 degrees; radial shortening, 1 mm; and articular incongruity, 0 mm. Wrist motion at final follow-up examination averaged 59 degrees of extension, 57 degrees of flexion, 27 degrees of ulnar deviation, 17 degrees of radial deviation, 80 degrees of pronation, and 78 degrees of supination. Grip strength was 79% of the contralateral side. The overall outcome according to the Gartland and Werley scales showed 19 excellent and 12 good results.6
Case Examples
Case 1
A C2 type fracture in a young female (Fig. 13-8) was managed by volar plating (Fig. 13-9). The patient demonstrated excellent range of motion at the final follow-up visit (Fig. 13-10).
Case 2
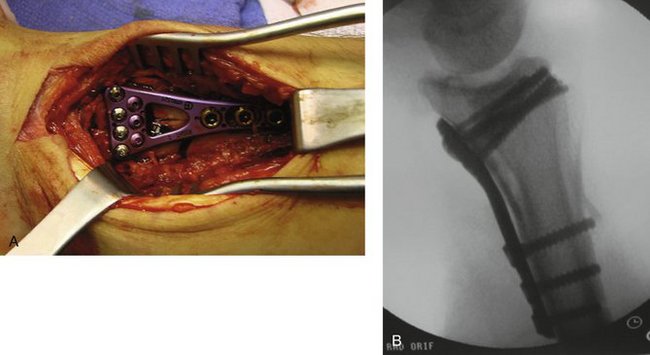
A motorcycle injury in a young active individual resulted in grossly comminuted fractures of the distal radius and ulna (Fig. 13-11). The injury was treated by an external fixator elsewhere (Fig. 13-12). The external fixator was removed and fixation was achieved using an extended flexor carpi ulnaris approach and a DVR plate (Fig. 13-13A). A good fixation of the fracture was achieved, and the distal end of the ulna was excised (Fig. 13-13B, C). At final follow-up 2 years later, the fracture had healed well and the patient had functional range of motion, despite not having been compliant with the physical therapy. He returned to work as a contractor but did not purchase a new motorcycle.

FIGURE 13-12 Radiograph of the fracture in Figure 13-11 managed by an external fixator elsewhere. Note the deformity is not corrected nor is the fracture reduced, but the fixator did improve length and facilitate later definitive surgery.

FIGURE 13-13 A, Intraoperative photograph during open reduction of fracture in Figure 13-11 showing multiple fracture fragments and soft tissue disruption, a characteristic of high-speed injury. B and C, Intraoperative fluoroscopy demonstrating good fixation of the severely displaced radius. The distal end of the ulna was excised owing to such severe comminution, and an extensor carpi ulnaris tenodesis was performed.
1. Jupiter JB. Current concepts review: fractures of the distal end radius. J Bone Joint Surg. 1991;73:461-469.
2. Cooney WP, Dobyns JH, Linscheid RL. Complications of Colles fractures. J Bone Joint Surg. 1980;62:613-619.
3. Lanz U, Kron W. A new technic for the correction of malunited distal radius fractures. Handchirurgie. 1976;8:203-206.
4. Smith RS, Crick JC, Alonso J, Horowitz M. Open reduction and internal fixation of volar lip fractures of the distal radius. J Orthop Trauma. 1988;2:181-187.
5. Georgoulis A, Lais E, Bernard M, Hertel P. Volar plate osteosynthesis in typical and atypical distal radius fractures. Akt Traumatol. 1992;22:9-14.
6. Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg [Am]. 2002;27:205-215.
7. Egol KA, Kubiak EN, Fulkerson E, et al. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18:488-493.
8. Badia A, Touhami A. Volar plating of distal radial fractures. Atlas Hand Clin. 2006;11:137-148.
9. Orbay JL, Badia A, Indriago IR, et al. The extended flexor carpi radialis approach: a new perspective for the distal radius fracture. Tech Hand Upper Extrem Surg. 2001;5:204-211.
10. Agee JM, McCarroll HRJr, Tortosa RD, et al. Endoscopic release of the carpal tunnel: a randomized prospective multicenter study. J Hand Surg [Am]. 1992;17:987-995.
11. Badia A. Median nerve compression secondary to fractures of distal radius. In: Luchetti R, Amadeo P, editors. Carpal Tunnel Syndrome. New York: Springer; 2006:247-252.
12. Geissler WB, Freeland AE. Arthroscopically assisted reduction of intraarticular distal radius fractures. Clin Orthop Relat Res. 1996;327:125-134.
13. Osterman AL, Vanduzer ST. Arthroscopy in the treatment of distal radial fractures with assessment and treatment of associated injuries. Atlas Hand Clin. 2006;1:231-241.
14. Harness NG, Jupiter JB, Orbay JL, et al. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Joint Surg [Am]. 2004;86:1900-1908.
15. Rozental TD, Blazar PE. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg [Am]. 2006;31:359-365.
16. Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg [Am]. 2004;29:96-102.