http://evolve.elsevier.com/McCuistion/pharmacology
Vitamins and minerals are needed in the correct portions for normal body function. Most vitamin and mineral nutrients can be safely obtained through the diet. Overuse of vitamins and minerals occurs easily, especially if the nutrients are coming from pills instead of food. It is important to check all supplements with the patient’s provider.
Vitamins
Vitamins are organic substances that are necessary for normal metabolic functions and for tissue growth and healing. The body needs only a small amount of vitamins daily, which can be obtained through the diet. A well-balanced diet has all of the vitamins and minerals needed for body functioning. The intake of vitamins should be increased by people experiencing periods of rapid body growth; those who are pregnant or breastfeeding; patients with debilitating illnesses; those with malabsorptive issues, such as Crohn disease; and those with inadequate diets, which includes alcoholics and some geriatric patients. Children who have poor nutrient intake and are malnourished may need vitamin replacement. People on “fad” or restrictive diets may have vitamin deficiencies, as may those who are unable to afford or do not select a wide variety of foods.
The sale of vitamins in the United States is a multibillion-dollar business. About 73% of the population uses a variety of nutritional supplements. Older women and people with higher education are typical users of nutritional supplements. Numerous vitamins and herbal medications are available for specialized needs such as cholesterol, memory, menopause, and prostate support. Before purchasing these agents, the patient should discuss with their health care provider the use and health benefits of multiple vitamins and herbal medications. Vitamin supplements are not necessary if the individual is healthy and consumes a well-balanced daily diet on a regular basis.
The Food and Nutrition Board of the Institute of Medicine (IOM) has established the Dietary Reference Intakes (DRIs).
The DRI nutrient recommendations include these components:
1. Adequate intake (AI) is the consumption and absorption of sufficient food, vitamins, and essential minerals necessary to maintain health.
TABLE 13.1
Deficiencies That Require Use of Vitamin Supplements
| Categories | Deficiencies |
| Inability to metabolize and absorb vitamins | Diarrhea, infectious and inflammatory diseases (e.g., Crohn disease, celiac disease) |
| Inability to use vitamins | Liver disease (cirrhosis, hepatitis), renal disease, certain hereditary deficiencies |
| Increased vitamin losses | Fever from infectious processes, hyperthyroidism, hemodialysis, cancer, starvation, crash diets |
| Increased vitamin requirements | Early childhood, pregnancy, debilitating disease (cancer, alcoholism), gastrointestinal surgery, special diets |
3. Recommended dietary allowance (RDA) is the amount of vitamins, minerals, or other essential nutrients that should be ingested every day by a normal person engaged in average activities. RDAs are increased for patients who are experiencing increased activity, children who are growing, and women who are pregnant and lactating. RDAs assume a state of wellness and are of little use in patients who are ill.
4. Tolerable upper intake level (UL) is the maximum level of continuing daily nutrient intake that is likely to pose no risk to the health of most of those in the age group for which it has been established.
Vitamin deficiencies can cause cellular and organ dysfunction that may result in slow recovery from illness. Vitamin supplements are necessary for the vitamin deficiencies described in Table 13.1, but vitamins are frequently taken prophylactically rather than therapeutically.
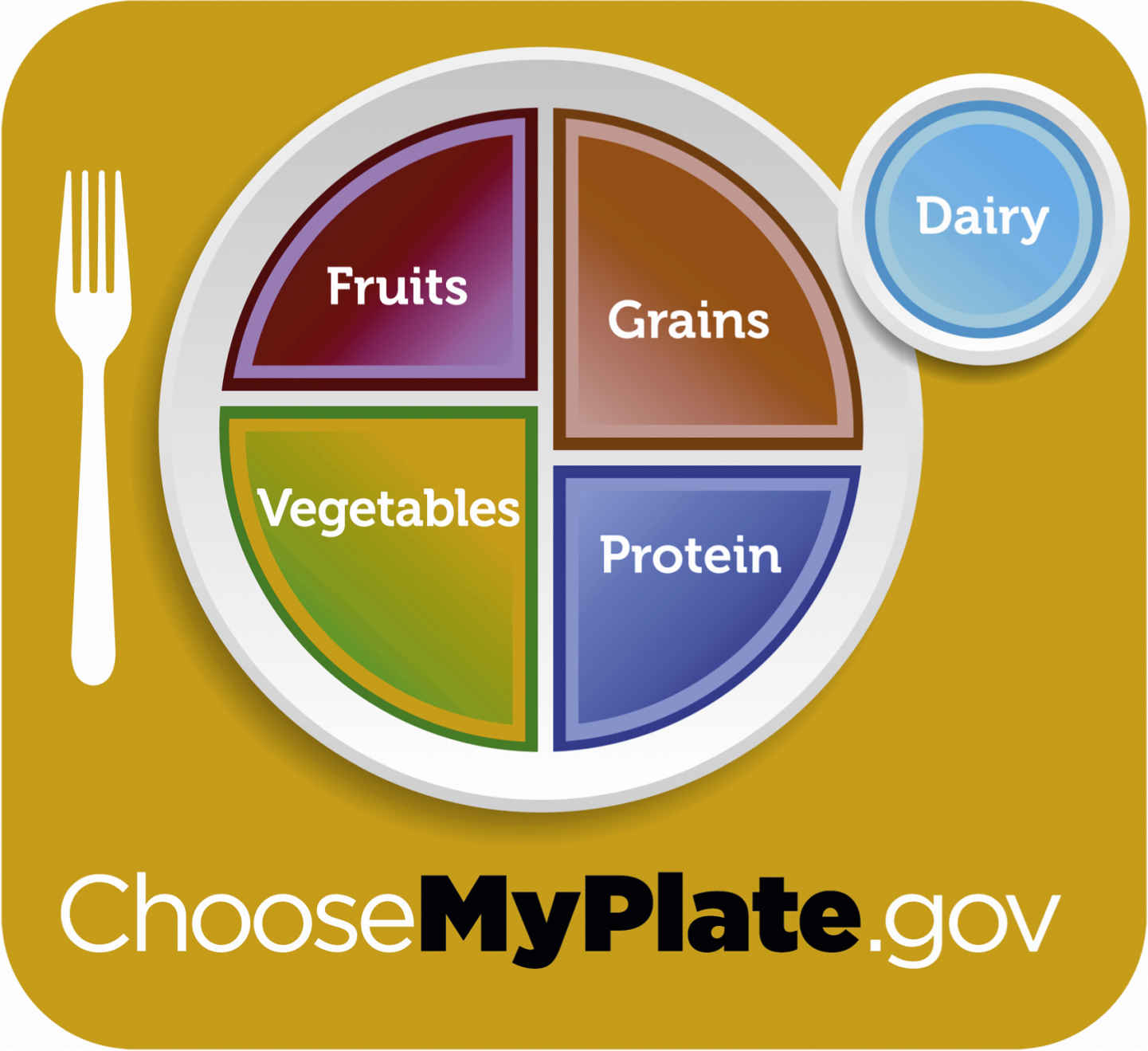
With the goal of facilitating better nutrition, the U.S. Department of Agriculture (USDA) has developed Choose My Plate, part of a communications initiative based on its 2010 Dietary Guidelines for Americans. Available at www.ChooseMyPlate.gov, Choose My Plate is an interactive tool that helps Americans to eat more healthfully (Fig. 13.1). This website offers a variety of features, including both consumer and professional information.
The Food and Nutrition Board at the IOM publishes the U.S. RDA for daily dose requirements of each vitamin. The U.S. Food and Drug Administration (FDA) requires that all vitamin products be labeled according to the vitamin content and the proportion of the RDA provided by the vitamin product. Individuals should be encouraged to check the RDA listed on the vitamin label to determine whether the product provides the RDA dose requirements. The RDA may need to be modified for patients who are ill.
Megadoses of vitamins are available and are advertised for specific health conditions, but high doses of some vitamins can be toxic. Patients should be advised to contact their health care provider before taking these products. Megadoses of fat-soluble vitamins (A, D, E, and K) may cause toxic effects, whereas megadoses of water-soluble vitamins are eliminated via the urine and thus are generally not toxic. Adverse reactions—kidney stones and nerve damage, respectively—have been reported from vitamin C and vitamin B6. However, it is also claimed that B vitamins may positively influence metabolism in older adults.
Table 13.2 lists fat- and water-soluble vitamins, their functions, suggested food sources, and related deficiency conditions.
Fat-Soluble Vitamins
Vitamins fall into two general categories: fat-soluble and water-soluble. The fat-soluble vitamins are A, D, E, and K. They are metabolized slowly; can be stored in fatty tissue, liver, and muscle in significant amounts; and are excreted in the urine at a slow rate. Vitamins A and D are toxic if taken in excessive amounts over time. Current research shows that vitamin D toxicity is quite rare, and its symptoms are fairly nonspecific. Given that many people are found to be vitamin D deficient, it is not uncommon to see high-dose vitamin D therapy (e.g., 50,000 units/week).
Foods rich in vitamins A, D, E, and K are shown in Table 13.2.
Vitamin A
Vitamin A (retinol and beta-carotene) are essential for bone growth and for maintenance of epithelial tissues, skin, eyes, and hair. Vitamin A has antioxidant properties. Studies show that women who take vitamin A have a 20% decrease in breast cancer as opposed to those who do not take vitamin A. However, excessive doses can be toxic. During pregnancy, excessive amounts of vitamin A (>6000 IU) might have a teratogenic effect (i.e., it can cause birth defects) on the fetus. Prototype Drug Chart 13.1 describes the pharmacologic data on vitamin A. Intramuscular administration is used in acutely ill patients.
Pharmacokinetics
Vitamin A is absorbed in the gastrointestinal (GI) tract, and 90% is stored in the liver; however, this function can be inhibited with liver disease. Massive doses of vitamin A can cause hypervitaminosis. Signs and symptoms include hair loss, peeling skin, anorexia, abdominal pain, lethargy, nausea, and vomiting.
Pharmacodynamics
Vitamin A is necessary for many biochemical processes. It aids in the formation of the visual pigment needed for night vision. This vitamin is needed in bone growth and development, and it promotes the integrity of the mucosal and epithelial tissues. An early sign of vitamin A deficiency (hypovitaminosis A) is night blindness. This may progress to dryness and ulceration of the cornea and cause blindness.
Vitamin A taken orally is readily absorbed from the GI tract and peaks in 3 to 5 hours. Its duration of action is unknown. Because vitamin A is stored in the liver, the vitamin may be available to the body for days, weeks, or months.
Vitamin D
Vitamin D has a major role in regulating calcium and phosphorus metabolism, and it is needed for calcium absorption from the intestines. Dietary vitamin D is absorbed in the small intestine and requires bile salts for absorption. There are two compounds of vitamin D: vitamin D2, ergocalciferol, a synthetic fortified vitamin D, and vitamin D3, cholecalciferol, a natural form of vitamin D influenced by ultraviolet sunlight on the skin. Over-the-counter (OTC) vitamin D supplements usually contain vitamin D3. Once absorbed, vitamin D is converted to calcifediol (also known as 25-hydroxycholecalciferol) in the liver. Calcifediol is then converted to an active form, calcitriol, in the kidneys. Studies have suggested that vitamin D taken with calcium can reduce the incidence of fractures.
Calcitriol, the active form of vitamin D, functions as a hormone, and along with parathyroid hormone (PTH) and calcitonin, it regulates calcium and phosphorus metabolism. Calcitriol and PTH stimulate bone reabsorption of calcium and phosphorus. Excretion of vitamin D is primarily in bile; only a small amount is excreted in the urine. If serum calcium levels are low, more vitamin D is activated; when serum calcium levels are normal, activation of vitamin D is decreased. The normal adult RDA of vitamin D is 1000 mg daily (600 IU/day).
Excess vitamin D ingestion (>4000 IU/day) results in hypervitaminosis D and may cause hypercalcemia (an elevated serum calcium level). Anorexia, nausea, and vomiting are early symptoms of vitamin D toxicity.
Vitamin E
Vitamin E has antioxidant properties that protect cellular components from being oxidized and protect red blood cells (RBCs) from hemolysis. Vitamin E depends on bile salts, pancreatic secretion, and fat for its absorption. Vitamin E is stored in all tissues, especially the liver, muscle, and fatty tissue. About 75% of vitamin E is excreted in bile.
Although early evidence had suggested the potential for vitamin E to reduce cardiovascular disease (CVD), more recent outcome studies have not shown benefits with vitamin E. Currently, the American Heart Association guidelines do not recommend vitamin E therapy for women as a preventative measure for CVD. Vitamin E has been of interest for its antioxidant properties, and it has been used off label for various conditions, including Alzheimer disease.
The RDA of vitamin E in adults is 30 IU daily and should not exceed the upper limit (UL) of 1000 mg/day in oral intake. The dosage is determined by nutritional intake or degree of deficiency by the health care provider. Side effects of large doses of vitamin E may include fatigue, weakness, nausea, GI upset, headache, bleeding, and breast tenderness. Vitamin E may prolong the prothrombin time (PT), and patients taking warfarin should have their PT monitored closely. Iron and vitamin E should not be taken together because iron can interfere with the body’s absorption and use of vitamin E.
Vitamin K
Vitamin K occurs in three forms. Vitamin K1 (phytonadione) is the most active form and is a synthetic type of vitamin K made by plants, and it represents the bulk of dietary vitamin K. Vitamin K2 (menaquinone) is synthesized by probiotic bacteria in the digestive tract. Vitamin K3 (menadione) is another synthetic form of vitamin K. After vitamin K is absorbed, it is stored primarily in the liver and in other tissues. Half of vitamin K comes from the intestinal flora, and the remaining portion comes from the diet. The RDA for an adult male is 120 mcg/day, and for an adult female the RDA is 90 mcg/day. The IOM has not been able to determine a tolerable upper level for vitamin K, so always speak to the health care provider prior to increasing the dose of vitamin K.
Vitamin K is needed for synthesis of prothrombin and clotting factors VII, IX, and X. For oral anticoagulant overdose, vitamin K1 (phytonadione) is the only vitamin K form available for therapeutic use and is most effective in preventing hemorrhage. Vitamin K is used for two purposes: as an antidote for oral anticoagulant overdose and to prevent and treat the hypoprothrombinemia of vitamin K deficiency. Spontaneous hemorrhage may occur with vitamin K deficiency due to lack of bile salts and malabsorption syndromes that interfere with vitamin K uptake (e.g., celiac disease). Newborns are vitamin K deficient, thus a single dose of phytonadione is recommended immediately after delivery. This practice is common in the United States but is controversial in other countries because it can elevate the bilirubin level and can cause hyperbilirubinemia with a risk of kernicterus. Oral and parenteral forms of phytonadione are available; intravenous (IV) administration is dangerous and may cause death.
Water-Soluble Vitamins
Water-soluble vitamins are the B-complex vitamins and vitamin C. This group of vitamins is not usually toxic unless taken in extremely excessive amounts. Water-soluble vitamins are not stored by the body, so consistent, steady supplementation is required. Water-soluble vitamins are readily excreted in the urine. Protein binding of water-soluble vitamins is minimal. Foods that are high in vitamin B are grains, cereals, breads, and meats. There are reports that B vitamins may promote a sense of well-being and increased energy as well as decreased anger, tension, and irritability. Citrus fruits and green vegetables are high in vitamin C. If the fruits and vegetables are cut or cooked, a large amount of vitamin C is lost.
Vitamin B Complex
Vitamin B1 (thiamine), vitamin B2 (riboflavin), vitamin B3 (nicotinic acid, or niacin), and vitamin B6 (pyridoxine) are four vitamins in the vitamin B–complex group that are water soluble. This is a common group of vitamins administered in the clinical setting, especially to patients with alcoholism.
Thiamine deficiency can lead to the polyneuritis and cardiac pathology seen in beriberi or to Wernicke encephalopathy that progresses to Korsakoff syndrome, conditions most commonly associated with alcohol abuse. Wernicke-Korsakoff syndrome is a significant central nervous system (CNS) disorder characterized by confusion, nystagmus, diplopia, ataxia, and loss of recent memory. If not treated, it can cause irreversible brain damage. IV administration of thiamine is recommended for treatment of Wernicke-Korsakoff syndrome. Thiamine must be given before giving any glucose to avoid aggravation of symptoms.
Riboflavin may be given to manage dermatologic problems such as scaly dermatitis, cracked corners of the mouth, and inflammation of the skin and tongue. To treat migraine headache, riboflavin is given in larger doses than for dermatologic concerns.
Niacin is given to alleviate pellagra and hyperlipidemia, for which large doses are required. Chapter 41 offers a discussion of niacin use to reduce cholesterol levels. However, large doses may cause GI irritation and vasodilation, resulting in a flushing sensation.
Pyridoxine is administered to correct vitamin B6 deficiency. It may also help alleviate the symptoms of neuritis caused by isoniazid (INH) therapy for tuberculosis. Vitamin B6 is essential as a building block of nucleic acids, in RBC formation, and in synthesis of hemoglobin. Pyridoxine is used to treat vitamin B6 deficiency caused by lack of adequate diet, inborn errors of metabolism, or drug-induced deficiencies secondary to INH, penicillamine, or cyclosporine (or hydralazine) therapy. It is also used to treat neonates with seizures refractive to traditional therapy. Vitamin B6 deficiencies may occur in alcoholics along with deficiencies of other B-complex vitamins. Patients with diabetes or alcoholism may benefit from daily supplementation. Pyridoxine is readily absorbed in the jejunum and is stored in the liver, muscle, and brain. It is metabolized in the liver and excreted in the urine.
Vitamin C
Vitamin C (ascorbic acid) is absorbed from the small intestine. Vitamin C aids in the absorption of iron and in the conversion of folic acid. Vitamin C is not stored in the body and is excreted readily in the urine. A high serum vitamin C level that results from excessive dosing of vitamin C is excreted by the kidneys unchanged. Vitamin C is used in the treatment of scurvy, which is rare in developed countries but seen in individuals who consume few fruits and vegetables. Also, scurvy is seen in people who are on restricted diets or who abuse alcohol or drugs.
The recommended daily allowance of vitamin C (adult dose) is 75 mg/day for women and 90 mg/day for men to prevent deficiency. Some individuals take greater amounts. Massive doses of vitamin C can cause GI upset. Prototype Drug Chart 13.2 details pharmacologic data on vitamin C.
Pharmacokinetics
Vitamin C is absorbed readily through the GI tract and is distributed throughout the body fluids. The kidneys completely excrete vitamin C mostly unchanged.
Pharmacodynamics
Vitamin C is needed for carbohydrate metabolism and protein and lipid synthesis. Collagen synthesis also requires vitamin C because it is part of the intercellular matrix that binds cells together and aids in wound healing. Smoking decreases serum vitamin C levels. Vitamin C in doses greater than 500 mg aids iron absorption; however, it can decrease the effect of oral anticoagulants.
The use of large doses of vitamin C is questionable. Large doses of any vitamin can cause toxicity. Most authorities believe that vitamin C does not prevent the common cold, cure advanced cancer, or treat schizophrenia. Moreover, large doses of vitamin C can cause nausea, abdominal cramps, and diarrhea. If taken with aspirin or sulfonamides, it may cause crystal formation in the urine. Vitamin C directly irritates the intestinal mucosa in the GI tract. This is why the Food and Nutrition Board has set 2 g/day as the adult UL for vitamin C. Large doses of vitamin C can decrease the effect of oral anticoagulants. If large doses of any vitamin are to be discontinued, a gradual reduction of the dosage is necessary to avoid vitamin deficiency.
Folic Acid (Folate)
Folic acid is absorbed from the small intestine, and the active form of folic acid—folate—is circulated to all tissues. One third of folate is stored in the liver, and the rest is stored in tissues. It is excreted 80% in bile and 20% in urine.
Folic acid is essential for body growth. It is needed for DNA synthesis, and without folic acid, cellular division is disrupted. Chronic alcoholism, poor nutritional intake, malabsorption syndromes, pregnancy, and drugs that cause inadequate absorption (phenytoin, barbiturates) or folic acid antagonism (methotrexate, triamterene, trimethoprim) are causes of folic acid deficiencies. Symptoms of folic acid deficiencies include anorexia, nausea, stomatitis, diarrhea, fatigue, alopecia, and blood dyscrasias (megaloblastic anemia, leukopenia, thrombocytopenia). These symptoms are usually not noted until 2 to 4 months after folic acid storage is depleted.
Folic acid deficiency during the first trimester of pregnancy can affect the development of the CNS of the fetus. This may cause neural tube defects (NTDs) such as spina bifida, defective closure of the bony structure of the spinal cord, or anencephaly, lack of brain mass formation. The U.S. Public Health Services recommends that all women who may become pregnant consume 400 mcg of supplemental folic acid each day in addition to the folate they get with food. Synthetic folate is more stable than folic acid obtained from food: bioavailability is greater than 85% with synthetic folate and less than 59% for food-sourced folic acid. Some evidence suggests that 400 to 500 mcg (0.4 to 0.5 mg) of folic acid per day can decrease the incidence of coronary artery disease (CAD). It is thought that folic acid decreases the amino acid homocysteine in the blood, which may contribute to heart disease.
Excessive doses of folic acid may mask signs of vitamin B12 deficiency, which is a risk in older adults. Patients taking phenytoin to control seizures should be cautious about taking folic acid. This vitamin can lower the serum phenytoin level, which could increase the risk of seizures; the phenytoin dose would need to be adjusted in such patients. This is a complex interaction that is not fully understood, but it is thought that 1 mg or less per day of folic acid is safe in patients with controlled epilepsy.
Vitamin B12
Vitamin B12, like folic acid, is essential for DNA synthesis. Vitamin B12 aids in the conversion of folic acid to its active form. With active folic acid, vitamin B12 promotes cellular division. It is also needed for normal hematopoiesis (development of RBCs in bone marrow) and to maintain nervous system integrity, especially of the myelin.
The gastric parietal cells produce an intrinsic factor that is necessary for the absorption of vitamin B12 through the intestinal wall. Without the intrinsic factor, little or no vitamin B12 is absorbed. After absorption, vitamin B12 binds to the protein transcobalamin II and is transferred to the tissues. Most vitamin B12 is stored in the liver and is slowly excreted, and it can take 2 to 3 years for stored vitamin B12 to be depleted and for a deficit to be noticed.
Vitamin B12 deficiency is uncommon unless there is a disturbance of the intrinsic factor and intestinal absorption. Pernicious anemia (lack of the intrinsic factor) is the major cause of vitamin B12 deficiency, but deficiency can also develop in strict vegetarians who do not consume meat, fish, or dairy products. Other possible causes of vitamin B12 deficiency include malabsorption syndromes (cancer, celiac disease, and certain drugs), gastrectomy, Crohn disease, and liver and kidney diseases. Vitamin B12 deficiency is commonly seen with the use of metformin and proton pump inhibitors (e.g., omeprazole). Symptoms may include numbness and tingling in the lower extremities, weakness, fatigue, anorexia, loss of taste, diarrhea, memory loss, mood changes, dementia, psychosis, megaloblastic anemia with macrocytes (overenlarged erythrocytes [RBCs]) in the blood, and megaloblasts (overenlarged erythroblasts) in the bone marrow.
To correct vitamin B12 deficiency, cyanocobalamin in crystalline form can be given intramuscularly for severe deficits. It cannot be given intravenously because of possible hypersensitive reactions. Cyanocobalamin can be given orally and is commonly found in multivitamin preparations. It can also be given as a subcutaneous injection.
 Cultural Considerations
Cultural Considerations• Food and food choices have strong cultural roots. Determine the patient’s preferred and culturally meaningful foods, and incorporate them into the food and supplement plan.
• Use interpreters as appropriate.
• Glucose-6-phosphate dehydrogenase (G-6-PD) deficiency is common among people of Arabic and Chinese heritage.
Evaluation
• Evaluate the patient’s understanding of the purpose of vitamins and their correct use.
• Evaluate the effectiveness of the patient’s diet for inclusion of appropriate amounts and types of food. Have the patient periodically keep a diet chart for a full week to determine typical nutrition.
• Determine whether the patient with malnutrition is receiving appropriate vitamin therapy.
Minerals
Various minerals—such as iron, copper, zinc, chromium, and selenium—are needed for body function.
Iron
Iron (ferrous sulfate, gluconate, or fumarate) is vital for hemoglobin regeneration. Sixty percent of the iron in the body is found in hemoglobin, and one of the causes of anemia is iron deficiency. A normal diet contains 5 to 20 mg of iron per day. Foods rich in iron include liver, lean meats, egg yolks, dried beans, green vegetables like spinach, and fruit. Food and antacids slow the absorption of iron, and vitamin C increases iron absorption.
During pregnancy, iron requirements increase due to the expansion of maternal blood volume and production of RBCs by the fetus. The iron needs of pregnant women are too great to be met through their diet, therefore supplementation is needed. About 27 mg/day are recommended during pregnancy and for 2 to 3 months after delivery.
The dose of iron for infants up to 12 months old is 11 mg/day, and for children from 1 to 8 years of age, it is 7 to 10 mg/day. Males from 9 to 50 years of age require 8 to 11 mg/day. Females 9 to 13 years of age require 8 mg/day; 14 to 18 years of age, 15 mg/day; 19 to 50 years of age, 18 mg/day; and women over 50 years of age require 8 mg/day. Prototype Drug Chart 13.3 describes the pharmacologic data on iron.
Pharmacokinetics
Iron is absorbed by the intestines and enters the plasma as heme, or it may be stored as ferritin. Although food decreases absorption by 25% to 50%, it may be necessary to take iron preparations with food to avoid GI discomfort. Vitamin C at doses greater than 500 mg may slightly increase iron absorption, whereas tetracycline, quinolone antibiotics (ciprofloxacin, levofloxacin, etc.), and antacids can decrease absorption (Complementary and Alternative Therapies 13.1).
Pharmacodynamics
Iron replacement is given primarily to correct or control iron-deficiency anemia, which is diagnosed by a laboratory blood smear. Positive findings for this anemia are microcytic (small), hypochromic (pale) erythrocytes (RBCs). Clinical signs and symptoms include fatigue, weakness, shortness of breath, pallor, and, in cases of severe anemia, increased GI bleeding. The dosage of ferrous sulfate for prophylactic use is 300 to 324 mg/day.
The onset of action for iron therapy takes days, and its peak action does not occur for days or weeks; therefore the patient’s symptoms are slow to improve. Increased hemoglobin and hematocrit levels occur within 3 to 7 days.
About 30% to 50% of adults on parenteral nutrition have been shown to have iron deficiency. Pediatric patients are at a 40% to 84% risk of developing an iron deficiency.
Iron toxicity is a serious cause of poisoning in children. As few as 10 tablets of ferrous sulfate (3 g) taken at one time can be fatal within 12 to 48 hours; hemorrhage from the ulcerogenic effects of unbound iron leads to shock, therefore parents should be strongly cautioned against leaving iron tablets that look like candy (M&Ms) within a child’s reach. (Most iron products are distributed in bubble packs.) There is also danger of children overdosing on adult or children’s multivitamins that contain iron.
Copper
Copper is needed for the formation of RBCs and connective tissues. Copper is a cofactor of many enzymes, and its function is in the production of the neurotransmitters norepinephrine and dopamine. Excess serum copper levels may be associated with Wilson disease, an inborn error of metabolism that allows for large amounts of copper to accumulate in the liver, kidneys, brain, and cornea (brown or green Kayser-Fleischer rings).
A prolonged copper deficiency may result in anemia that cannot be corrected by taking iron supplements. Abnormal blood and skin changes caused by a copper deficiency include a decrease in white blood cell count, glucose intolerance, and a decrease in skin and hair pigmentation. Mental retardation may also occur in the young. Copper deficiency in patients receiving parenteral nutrition ranges from 30% to 56% and includes both adults and children.
The RDA for copper is 900 mcg/day. Most adults consume about 1 mg/day. Foods rich in copper are shellfish (crab, oysters), liver, nuts, seeds (sunflower, sesame), legumes, and cocoa.
Zinc
Zinc is important to many enzymatic reactions, and it is essential for normal growth and tissue repair, wound healing, and taste and smell. The use of zinc has greatly increased in the past few years; some believe zinc can alleviate symptoms of the common cold and shorten its duration, although studies have disputed this claim. Large amounts of zinc can be toxic. Zinc in lozenge form can cause nausea and can leave an unpleasant taste, and zinc in nasal sprays has caused patients to lose their sense of smell. Patients should always check with a health care provider prior to taking zinc. The adult RDA is 8 to 11 mg/day. Foods rich in zinc include beef, lamb, eggs, and leafy and root vegetables.
Large doses, more than 150 mg, may cause a copper deficiency, a decrease in high-density lipoprotein (HDL) cholesterol (“good” cholesterol), and a weakened immune response. Zinc can inhibit tetracycline absorption. Patients taking zinc and an antibiotic should not take them together; zinc should be taken at least 2 hours after taking an antibiotic. About 10% of adults on long-term parenteral nutrition develop a zinc deficiency. Infants and children have a much higher rate of deficiency (20% to 30%). Zinc is the most common deficiency likely to occur in parenteral nutrition because zinc is lost in the patient’s stool.
Chromium
Chromium is said to be helpful in the control of type 2 diabetes (non–insulin-dependent diabetes). It is thought that this mineral helps to normalize blood glucose by increasing the effects of insulin on the cells. If a patient is taking large doses of chromium and an oral hypoglycemic agent or insulin, the glucose level should be monitored closely for a hypoglycemic reaction. The dose of an oral hypoglycemic drug or insulin may need to be decreased. Some patients with impaired glucose tolerance and those who do not have diabetes may benefit by taking chromium. In addition, chromium claims to promote weight loss and muscle building. Multivitamin and mineral preparations contain chloride salt of chromium.
There is no RDA for chromium; however, 25 to 35 mcg/day is considered within the normal range for adults and children older than 9 years of age. Foods rich in chromium include meats, whole-grain cereals, and brewer’s yeast.
Selenium
Selenium acts as a cofactor for an antioxidant enzyme that protects protein and nucleic acids from oxidative damage. Selenium works with vitamin E. It is thought that selenium has an anticarcinogenic effect, and doses lower than 200 mcg may reduce the risk of lung, prostate, and colorectal cancer. Excess doses of more than 200 mcg might cause weakness, hair loss, dermatitis, nausea, diarrhea, and abdominal pain. Also, there may be a garlic-like odor from the skin and breath.
The RDA for selenium is 40 to 75 mcg (the lower dose is recommended for women, higher dose for men). Foods rich in selenium include meats, especially liver; seafood; eggs; and dairy products.
 Cultural Considerations
Cultural Considerations• Ask about cultural practices and incorporate them as appropriate.
• Use an interpreter as needed.
Evaluation
• Evaluate the effectiveness of iron therapy by determining that the patient is not fatigued or short of breath and that the hemoglobin level is within the desired range.
Critical Thinking Case Study
CB is pregnant and is taking two 325-mg tablets of ferrous sulfate daily. She has a 2-year-old daughter.
1. What precautions should CB take in regard to the container of ferrous sulfate? Explain your answer.
2. CB asks if she can take iron in the morning before breakfast. How should the nurse respond?
3. CB asks the nurse if any side effects are associated with taking iron. What would be an appropriate response?
4. CB asks if she should include foods high in iron in her daily diet. How should the nurse respond?