28 Visual pathways
Introduction
The visual system comprises the retinas, the visual pathways from the retinas to the brainstem and visual cortex, and the cortical areas devoted to higher visual functions. The retinas and visual pathways are described in this chapter. Higher visual functions are described in Chapter 29.
Retina
The retina and the optic nerves are part of the central nervous system. In the embryo, the retina is formed by an outgrowth from the diencephalon called the optic vesicle (Ch. 1). The optic vesicle is invaginated by the lens and becomes the two-layered optic cup.
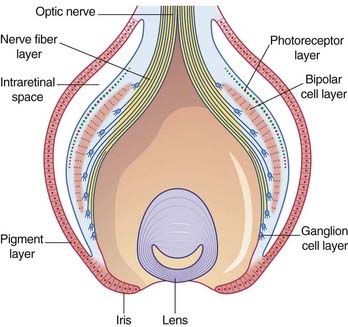
Figure 28.1 shows the general relationships in the developing retina. The nervous layer contains three principal layers of neurons: photoreceptors, which become applied to the pigment layer when the intraretinal space is resorbed; bipolar neurons; and ganglion cells which give rise to the optic nerve and project to the thalamus and midbrain.
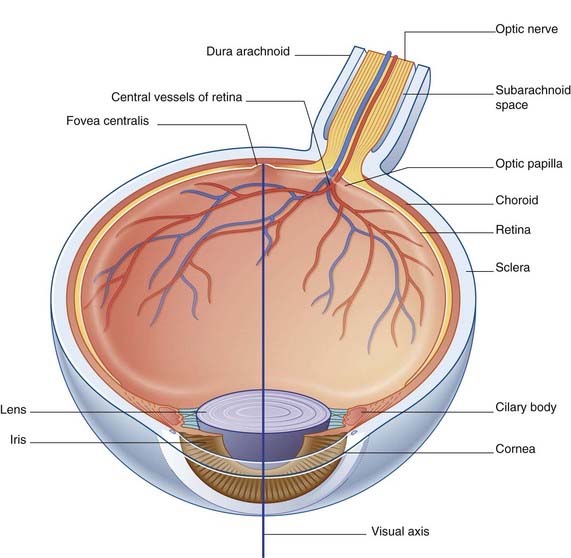
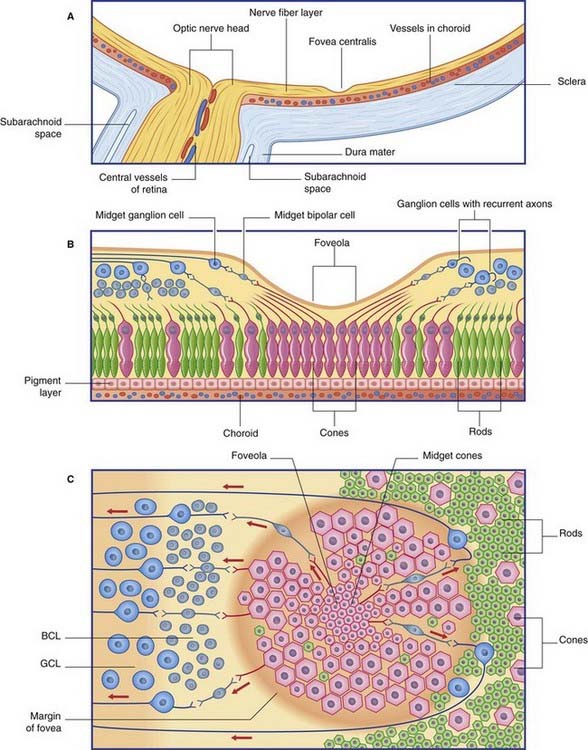
Note that the retina is inverted: light must pass through the layers of optic nerve fibers, ganglion cells, and bipolar neurons to reach the photoreceptors. However, at the point of most acute vision, the fovea centralis, the bipolar and ganglion cell layers lean away all around a central pit (fovea), and light strikes the photoreceptors directly (see Foveal Specialization, later). In the mature eye, the fovea is about 1.5 mm in diameter and occupies the center of the 5 mm wide macula lutea (‘yellow spot’) where many of the photoreceptor cells contain yellow pigment. The fovea is the point of most acute vision and lies in the visual axis – a line passing from the center of the visual field of the eye, through the center of the lens, to the fovea (Figure 28.2). To fixate or foveate an object is to gaze directly at it so that light reflected from its center registers on the fovea.
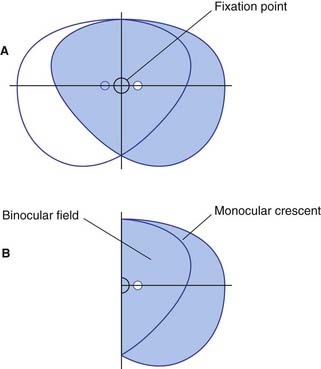
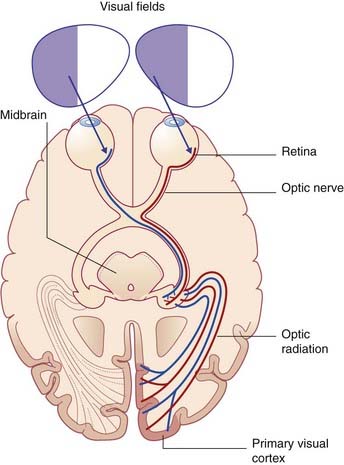
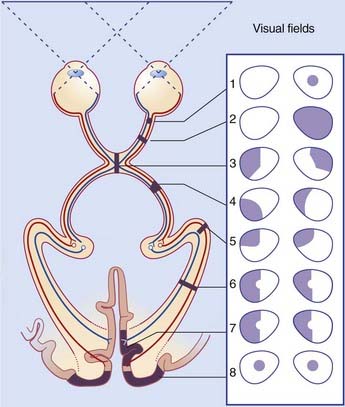
The visual fields of the two eyes overlap across two-thirds of the total visual field. Outside this binocular field is a monocular crescent on each side (Figure 28.3). During passage through the lens, the image of the visual field is reversed, with the result that, e.g., objects in the left part of the binocular visual field register on the right half of each retina, and objects in the upper part of the visual field register on the lower half. This arrangement is preserved all the way to the visual cortex in the occipital lobe.
Structure of the retina
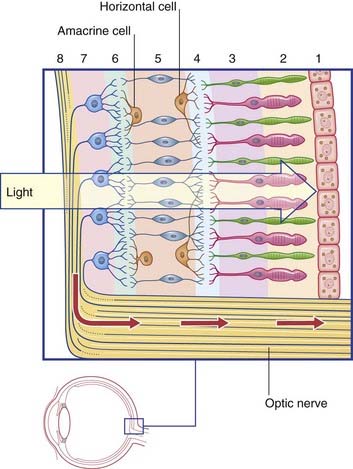
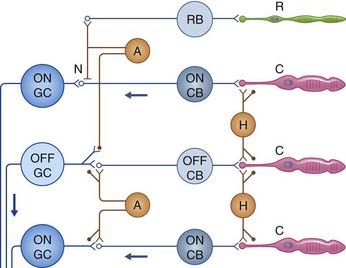
In addition to the serially arranged photoreceptors, bipolar cells, and ganglion cells shown in Figure 28.1, the retina contains two sets of neurons arranged transversely: horizontal cells and amacrine cells (Figure 28.4). A total of eight layers are described for the retina as a whole.
Cone and rod bipolar neurons
Ganglion cells
Foveal specialization
The relative density of cones increases progressively, and their size diminishes progressively, from the edge of the fovea inwards (Figure 28.6). The central one-third of the fovea, little more than 100 µm wide and known as the foveola, contains only midget cones. Two special anatomical features assist the foveal cones in general, and the midget cones in particular, in transducing the maximum amount of information concerning the form and color values of an object under direct scrutiny. First, the more superficial layers of the retina lean outward from the center, and their neurites are exceptionally long, with the result that the outer two-thirds of the foveola are little overlapped by bipolar cell bodies and the inner third is not overlapped at all; light reflected from the object strikes the cones of the foveola without any diffraction. Second, fidelity of central transmission is enhanced by one-to-one synaptic contact between the midget cones and midget bipolar neurons, and between these and midget ganglion cells. Outside the foveola, the amount of cone-to-bipolar-to-ganglion cell convergence increases progressively.
Central Visual Pathways
Optic nerve, optic tract
The retinal ganglion cells are homologous with the sensory projection neurons of the spinal cord. The optic nerve is homologous with spinal cord white matter, and is not a peripheral nerve. As explained in Chapter 9, true peripheral nerves, whether cranial or spinal, contain Schwann cells and collagenous sheaths, and are capable of regeneration. The optic nerve contains neuroglial cells of central type (astrocytes and oligodendrocytes) and is not capable of regeneration in mammals. In addition, the nerve is invested with meninges containing an extension of the subarachnoid space – a feature largely responsible for the changed appearance of the fundus oculi when the intracranial pressure is raised (papilledema, Ch. 4).
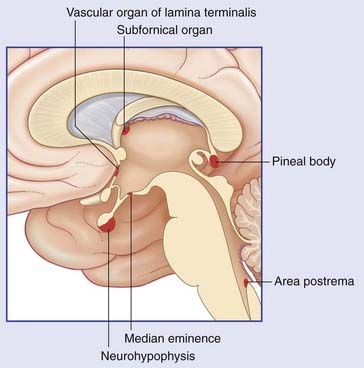
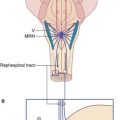
As already noted in Chapter 26, some optic nerve fibers enter the suprachiasmatic nucleus of the hypothalamus. This connection has been invoked to account for the beneficial effect of bright artificial light, for several hours per day, in the treatment of wintertime depression.
Each optic tract winds around the midbrain and divides into a medial and a lateral root.
Medial root of optic tract
Lateral root of the optic tract and lateral geniculate body
The circuitry of the LGB resembles that of other thalamic relay nuclei, and includes inhibitory (GABA) terminals derived from internuncial neurons and from the thalamic reticular nucleus. (The portion of the reticular nucleus serving the LGB is called the perigeniculate nucleus.) Corticogeniculate axons arise in the primary visual cortex and synapse upon distal dendrites of relay cells as well as upon inhibitory internuncials. Cortical synapses on relay cells are twice as numerous as those derived from retinal ganglion cells. Cortical stimulation usually enhances the response of relay cells to a given retinal input. A likely, but unproven, function could be that of selective enhancement of particular features of the visual scene, e.g. when searching for an object of known shape or color. Functional magnetic resonance imaging (fMRI, Ch. 29) is capable of detecting areas of increased neuronal activity in the brain. fMRI has shown that when volunteers expect to see an object of interest onscreen, metabolic activity in the LGB increases before the stimulus is presented.
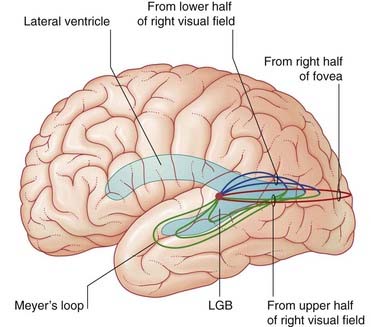
Geniculocalcarine tract and primary visual cortex
The anatomy of the optic radiation is shown in Figures 28.7–28.10. Fibers destined for the lower half of the primary visual cortex sweep forward into the temporal lobe, as Meyer’s loop, before turning back to accompany those traveling to the upper half. The tract enters the retrolentiform part of the internal capsule and continues in the white matter underlying the lateral temporal cortex. It runs alongside the posterior horn of the lateral ventricle before turning medially to enter the occipital cortex.
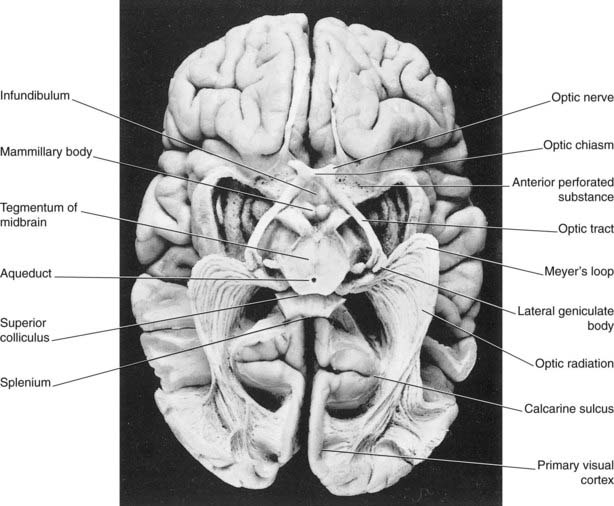
Figure 28.8 A dissection of the visual pathways, viewed from below.
(Photograph reproduced from Gluhbegovic, N. and Williams, T. W. (1980) The Human Brain, by kind permission of the authors and of J.B. Lippincott, Inc.)
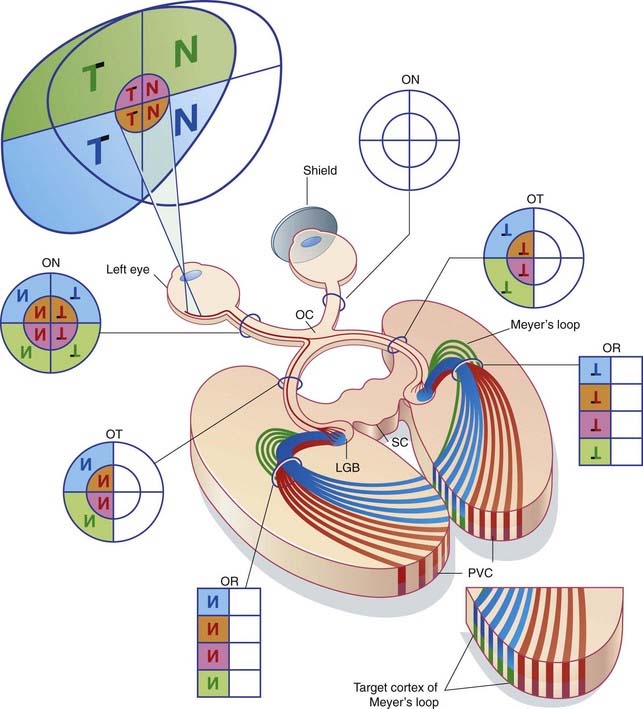
The optic radiations (OR) are fan-like (cf. Figure 28.7), with the axons carrying the foveal input initially in the middle of the fan.
The primary visual cortex occupies the walls of the calcarine sulcus along its entire length (the sulcus is 10 mm deep). It emerges onto the medial surface of the hemisphere for 5 mm both above and below the sulcus, and onto the occipital pole of the brain for 10 mm. Its total area is about 28 cm2. In the freshly cut brain, it is easily identified by a thin band of white matter (the visual stria of Gennari) within the gray matter – hence an alternative term, striate cortex. The left and right eyes are represented in the cortex in alternating stripes called ocular dominance columns (Figure 28.9).
Retinotopic map
The contralateral visual field is represented upside down. The plane of the calcarine sulcus represents the horizontal meridian. Retinal representation is posteroanterior, with a greatly magnified foveal representation in the posterior half of the calcarine cortex (Figure 28.10).
The clinical effects of various lesions of the visual pathway are described in Clinical Panel 28.1.
Clinical Panel 28.1 Lesions of the visual pathways
The following points arise in testing the visual pathways:
| Lesions | Field defects |
|---|---|
| 1 Partial optic nerve | Ipsilateral scotomaa |
| 2 Complete optic nerve | Blindness in that eye |
| 3 Optic chiasm | Bitemporal hemianopia |
| 4 Optic tract | Homonymousb hemianopia |
| 5 Meyer’s loop | Homonymous upper quadrantanopia |
| 6 Optic radiation | Homonymous hemianopia |
| 7 Visual cortex | Homonymous hemianopia |
| 8 Bilateral macular cortex | Bilateral central scotomas |
Notes on the numbered lesions
Karten HJ, Keyser KT, Brecha NC. Biochemical and morphological heterogeneity of retinal ganglion cells. In: Cohen B, Bodis-Wollner I, editors. Vision and the brain. New York: Raven Press; 1990:19-33.
Massey SC, Redburn DA. Transmitter circuits in the vertebral retina. Prog Neurobiol. 1987;28:55-96.
Rees G. The anatomy of blindsight. Brain. 2008;131:1414-1415.
Sadun AA, Glaser JS, Bose S. Anatomy of the visual sensory system. In: Tasman W, editor. Duane’s clinical ophthalmology (vol 2). Philadelphia: Lippincott, Williams and Wilkins; 2005:1-23.
Selhorst JB, Chen Y. The optic nerve. Semin Neurol. 2009;29:29-35.
Treue S. Visual attention: the where, what, how and why of saliency. Curr Opin Neurobiol. 2003;13:428-432.
Wilhelm H. The pupil. Curr Opin Neurol. 2008;21:36-42.
Zou Q, Long X, Zuo X, et al. Functional connectivity between the thalamus and visual cortex under eyes closed and eyes open conditions: a resting-state fMRI study. Hum brain mapp. 2009;30:3066-3078.